Abstract
Background
Epidemiologic evidence documenting fracture risk as children with cerebral palsy (CP) age throughout growth is lacking to inform on when to implement fracture prevention strategies. The objective was to characterize the 5-year risk of fractures by each year of age among <1–13 year olds with CP and effects by patient-level factors.
Methods
This retrospective cohort study used commercial administrative claims from 01/01/2001 to 12/31/2018 from children <1–13 years old with ≥5 years of insurance enrollment. Fractures were examined during the 5-year follow-up. For the CP cohort, the association between 5-year fracture rate and patient-level factors was assessed using Cox regression.
Results
Children with (n = 5559) vs. without (n = 2.3 million) CP had a higher 5-year fracture risk at the vertebral column, hip, and lower extremities at almost each year of age, but lower 5-year fracture risk at the upper extremities after 6 years old (all P < 0.05). Among children with CP, the 5-year fracture rate was elevated for co-occurring neurological conditions and non-ambulatory status at the vertebral column, hip, and lower extremities (hazard ratio [HR] range, 1.44–2.39), and higher for males at the upper extremities (HR = 1.29) (all P < 0.05).
Conclusions
This study provides novel epidemiologic evidence of 5-year fracture risk for each year of age for children with CP.
Impact
-
This study provides novel epidemiologic evidence of 5-year fracture risk for each year of age across important developmental stages for children with vs. without cerebral palsy (CP).
-
Children with vs. without CP were more likely to fracture at the vertebral column, hip, lower extremities, and humerus and less likely to fracture at the forearm and hands.
-
The age-related 5-year fracture risk was associated with clinically relevant patient-level factors, but in different ways by fracture region.
-
Study findings may be used to enhance clinical detection of at-risk children and strategize when to implement fracture prevention efforts for children with CP.
Similar content being viewed by others
Introduction
Cerebral palsy (CP) is a neurological syndrome that arises around the time of birth and is clinically characterized by an array of motor dysfunction disorders, among other complications.1 Impaired neuromuscular function and an underdeveloped and weak-for-size musculoskeletal system are well-known issues associated with CP, and increases the risk for early development of bone fragility.2,3,4,5,6,7,8 A major consequence of bone fragility is sustaining a fracture, which can lead to acute (e.g., impaired bone healing, infections) and chronic (e.g., increased morbidity and mortality) health complications for individuals with CP.9,10,11,12,13 As pediatric bone health is a major determinant of bone health across the lifespan,14 implementing fracture prevention strategies early in life for individuals with CP is a high clinical priority.
To date, there is little epidemiologic evidence on fracture risk by anatomical region and age at a detailed level (e.g., each year of age) to assist in clinical monitoring and to strategize population-based prevention efforts based on the complex skeletal needs of children with CP. Studies have reported fracture rates of ~4% or less per year for children with CP, which was similar to the general population of children without CP.15,16 However, these and other epidemiologic investigations are often limited by a relatively small sample size (e.g., n < 600), not allowing for a detailed age assessment or additional analyses by fracture region, potentially masking clinically important aspects of fracture risk. For example, a recent period prevalence study found a similar 1-year fracture risk between 2 and 17 year olds with CP (n = 1699) and without CP (n = 1.2 million), but when stratified by fracture region, children with CP were ~3.3 times more likely to fracture at the lower extremities and ~51% less likely to fracture at the upper extremities.17 Differentiating by fracture region to inform prevention efforts is critical because lower extremity fractures, especially the distal femur which is a common site for CP,12,18 are especially debilitating to health and function and can be more complicated to treat and manage than upper extremity fractures.19,20
Additionally, bone development follows a complex, multi-factorial process that has unique priorities at different stages of growth.14,21 Abnormal bone development likely occurs at varying degrees and at multiple stages of growth in CP, owing in part to issues with function, biology (e.g., hormonal milieu), and iatrogenic factors (e.g., surgeries).22,23,24 Collectively, longitudinal fracture risk may compound with increasing age during growth differently for children with vs. without CP. However, this has not been well captured as fracture epidemiologic studies in CP often group children as a whole (e.g., 2–18 year olds) or broad age categories (e.g., 2–7 years). Knowledge of longitudinal fracture risk by each year of age could assist in prioritizing when to implement clinical monitoring and prevention strategies.
Accordingly, the primary objective was to characterize 5-year fracture risk (at any site, then region-specific) by each year of age among a large, nationwide sample of <1 to 13 year olds with CP and without CP for comparison. To enhance clinical interpretations, the secondary objective was to determine if clinically relevant patient-level factors influence the age-related 5-year fracture risk among children with CP, including demographics, ambulatory status, and co-occurring intellectual disabilities and epilepsy.
Methods
Design and database
This retrospective cohort study leveraged patient-level claims from 01/01/2001 to 12/31/2018 from Optum’s de-identified Clinformatics® Data Mart Database. This administrative claims database contains medical claims with representation across the United States.25 Claims data are primarily used for billing reimbursement, but medical conditions can be identified by searching for unique codes attached to patient-level claims for research purposes. The codes used to identify CP, co-occurring intellectual disabilities and epilepsy, and wheelchair use are presented in Supplemental Table S1. Data are de-identified prior to administration to researchers. As a result, the University Institutional Review Board approved this study as non-regulated and patient consent was not required.
Cohort selection
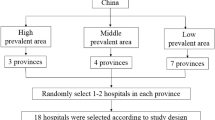
A flow chart of inclusion/exclusion is presented in Supplemental Fig. S1. Children who were <1–13 years of age by 12/31/2013 and with mostly continuous health plan enrollment for ≥5 years were eligible for analysis. Temporary drops in health plan enrollment are not uncommon for commercial health plans, and requiring full continuous enrollment for ≥5 years can lead to selection bias that can be partially avoided. Therefore, this study allowed for no more than 3 gaps in enrollment during the 5-year period, such that each gap lasted <3 months and were separated by ≥6 months of continuous health plan enrollment. This approach was meant to optimize cohort representation and sufficient time to identify fractures during the 5-year follow-up period.
The cohort with CP was identified by ≥2 claims with a pertinent code for CP, where each claim for CP was on a separate day within 12 months of one another. Using the 5-year period mitigates early detection bias for identifying children with CP, as some children may not get a diagnosis for CP until 2 or 3 years of age.26 The cohort without CP was identified by having 0 claims for CP over the 5-year period.
Fracture
The first all-cause fracture date per site was identified. This study included fracture sites that are known or suspected to significantly alter function for children with CP. Major fracture sites included the vertebral column, hip (including proximal femur), non-proximal femur, tibia/fibula, humerus, and ulna/radius. Fractures at the foot/toes were included due to the poor motor function in CP that can be worsened with an immobilized foot/ankle, such as from a cast. Fractures at the hand/fingers were included as children with CP may rely on upper extremity and hand function to use assistive mobility devices. Therefore, fractures in the hand/fingers could disproportionately impact mobility and independence for children with vs. without CP. For fractures at multiple simultaneous sites, they were grouped as occurring in the upper extremities only or other sites (i.e., vertebral column, hip, lower extremities) with or without a fracture in the upper extremities.
Patient-level characteristics
Sex, race, and U.S. region of residence was sequestered from the study entry year. The database provides the year the child was born, but not the day or month. Age was calculated as the study entry year minus the year the child was born, and interpretations should consider that the true age has a range of ±364 days of the calculated age. Co-occurring intellectual disabilities and epilepsy are relatively common for children with CP and may increase the risk of fractures.27,28 A variable was constructed to identify mutually exclusive sub-groups of co-occurring intellectual disabilities and/or epilepsy.29 Intellectual disabilities and epilepsy were identified in the same manner as CP. The type of CP was described based on available codes.
Claims data does not provide information about the severity of CP. To provide a proxy for non-ambulatory status, a 3-level variable was constructed based on claims for the presence of wheelchair use or wheelchair accessories over the 5-year period. Children with a code for “wheelchair dependence” at any point were designated as non-ambulatory. For the remainder, children with Durable Medical Equipment evidence of a wheelchair or accessories in two separate years were also designated as non-ambulatory, whereas children with evidence of a wheelchair or accessories in only one year were designated to have an unknown ambulatory status. This is because surgeries or a fracture, for example, may have led to a temporary use of a wheelchair. A single year to capture wheelchair use could therefore misclassify the non-ambulatory status of some chidlren. Children without any claims for wheelchair use or accessories over the 5-year period were designated as ambulatory.
Statistical analysis
Basic descriptive characteristics and 5-year fracture risks were summarized for the cohorts with and without CP. The crude relative risk (RR) with 95% confidence intervals (CI) was estimated for each fracture variable comparing children with vs. without CP to assess the magnitude of risk elevation (or suppression).
Age was examined at the single year unit to provide a detailed assessment of 5-year fracture risk by age. To determine whether there were differential time-varying rates by each year of age, the cumulative incidence function was plotted for each cohort separately. Given the number of outcome events, fracture outcomes in these detailed age analyses were examined as (1) any site, and then single or multiple simultaneous fractures occurring at the (2) vertebral column, hip, or lower extremities and (3) upper extremities. This regional grouping of fracture sites was determined by conceptual (i.e., to capture differential fracture region distribution between children with and without CP) and logistical (i.e., based on the available sample size to provide reasonable estimates) components.
To determine whether patient-level factors, including sex, co-occurring intellectual disabilities and/or epilepsy, and non-ambulatory status, impact the relationship between age and 5-year fracture rate, Cox proportional hazards regression models were developed and included the main effect of age, each factor, and their interaction term in separate models. These models adjusted for these patient-level factors, U.S. region of residence, and the study entry year. If the interaction was not statistically significant at P < 0.05, the interaction term was removed and the hazard ratio (HR) with 95% CI was estimated to determine the association between these factors with 5-year fracture rate. The proportional hazards assumption was visually inspected and tested for each covariate in all models based on the weighted Schoenfeld residuals.
Sensitivity analysis
To determine whether the primary fracture outcomes in children with CP were occurring mostly among those designated as non-ambulatory, children with CP without evidence of wheelchair use (ambulatory) were compared to two cohorts: (1) children with CP designated as non-ambulatory and (2) ambulatory children without CP. Children with CP with an unknown ambulatory status (i.e., evidence of wheelchair use in a single year) were excluded from this analysis to avoid biased interpretations from possible misclassification of ambulatory status.
To study outcomes over a 5-year period, this study excluded 8795 children with CP that had 1–4 years of mostly continuous health plan enrollment (Supplemental Fig. S1). To assess for possible selection bias, baseline characteristics and 1-year fracture risks in the first year of follow-up were summarized and compared between children with CP that had 1–4 years vs. ≥5 years (primary cohort) of mostly continuous health plan enrollment. Ambulatory status was excluded as this variable required more than a single year to designate the status. In a Cox regression model, the interaction between group (1–4 years vs. ≥5 years) with age was tested to determine if the age-related fracture risk patterns were consistent across cohorts.
Analyses were performed using SAS version 9.4 and P < 0.05 was considered statistically significant.
Results
There were 5559 children with CP and 2,318,476 children without CP who were eligible for the primary analysis. Baseline descriptive characteristics are presented in Table 1. For both cohorts, the majority had a study entry year in 2001 (with CP, 26.3%; without CP, 22.8%), while the proportion for the remaining 12 years ranged from 2.1 to 8.2% (data not shown). The majority of each cohort did not have any gaps in health plan enrollment for the 5-year period (with CP, 86.5%; without CP, 86.4%).
5-year fracture risk for the entire cohorts
The 5-year fracture risk and the relative risk (RR) for the entire cohort with and without CP are presented in Table 2. While there was a relatively similar 5-year risk for fracture at any site between cohorts (with CP, 13.0%; without CP, 12.3%; RR = 1.06; 95% CI = 0.99–1.13), there were differences in the distribution of where the fractures were occurring. Children with vs. without CP were more likely to sustain a fracture(s) in the vertebral column, hip, lower extremities, and humerus (RR ranged from 1.25 to 10.28, all P < 0.05), and less likely to sustain a fracture at the ulna/radius and hand/fingers (RR = 0.54 and 0.65, respectively, both P < 0.05).
5-year fracture risk by age
The 5-year risk of fracture at any site was similar between children with and without CP, and increased per older year of age until about 10 years old (Fig. 1a). However, children with vs. without CP had a higher 5-year risk of fracture at the vertebral column, hip, and lower extremities at almost each year of age, which generally increased with each year of age (Fig. 1b). Children with vs. without CP had a similar 5-year risk of fracture at the upper extremities until about 5 years of age, and then had a lower 5-year risk thereafter (Fig. 1c). To be sure the findings were not driven by fractures at the foot/toes and hand/fingers, the same analysis was conducted after separating out these fracture sites. As shown in Supplemental Fig. S2, fracture at the foot/toes was similar between cohorts, while other patterns remained similar as above.
The marker represents the point estimate (5-year fracture risk) and the vertical lines represent the 95% confidence interval. Due to the large sample size, the 95% confidence intervals for the cohort without CP are difficult to visualize. a Fracture at any site. b Fracture at the vertebrae, hip, and lower extremities. c Fracture at the upper extremities.
To visualize the time-varying rates, the cumulative incidence of fracture by each year of age was examined for fracture at any site (Fig. 2), vertebral column, hip, or lower extremities (Supplemental Fig. S3), and upper extremities (Supplemental Fig. S4). In general, the fracture rates were relatively linear across the 5-year follow-up for children with and without CP.
Patient-level factors associated with 5-year risk of fracture
Among the cohort with CP, the fully adjusted model for each fracture outcome is presented in Table 3. There was no evidence of an age interaction with the patient-level factors for any of the fracture outcomes. There was also no evidence that the proportional hazards assumption was violated for any analysis.
There was a sex difference in fracture rate only for the upper extremities, with males vs. females having a 29% higher fracture rate. There was a geographical difference, with the West having the lowest 5-year rate of fractures, especially of the upper extremities. Co-occurring intellectual disabilities with or without epilepsy and evidence of wheelchair use were associated with higher 5-year rates of fractures at the vertebral column, hip, or lower extremities, but not for the upper extremities.
Sensitivity analysis
The 5-year risk of the primary fracture outcomes for ambulatory and non-ambulatory children with CP and ambulatory children without CP are presented in Table 4. The 5-year risk of fracture at the vertebral column, hip, or lower extremities was highest for non-ambulatory children without CP (14.3%), but ambulatory children with vs. without CP still had a higher risk at these sites (RR = 1.38; 95% CI = 1.20–1.58). The 5-year fracture risk at the upper extremities was relatively similar among ambulatory and non-ambulatory children with CP and lower compared to children without CP, consistent with the primary analysis.
The baseline descriptive characteristics of children with CP with 1–4 years (n = 8795) vs. ≥5 years (n = 5559) of mostly continuous health plan enrollment were similar, except the 36.1 vs. 17.7% with missing data on race, respectively (Supplemental Table S2). The 1-year fracture risk was slightly higher for the 1–4 vs. ≥5 year cohort for fracture at any site (3.2 vs. 2.7%), vertebral column, hip, or lower extremities (2.0 vs. 1.7%), and upper extremities (1.3 vs. 1.2%). However, there was no evidence of an interaction between group (1–4 vs. ≥5 years) with age for these fracture outcomes (P for interaction ranged from 0.763 to 0.906) (data not shown). Taken together, selection bias may have led to slight underestimates of 5-year fracture risks in the primary analysis, but no appreciable impact on the age-related patterns.
Discussion
By leveraging a large, nationwide claims database, this study was able to provide novel epidemiologic evidence of 5-year fracture risks for each year of age for children with and without CP. This allowed for the documentation of nuanced changes in fracture vulnerability across important developmental stages.
As expected, the 5-year fracture risk increased with age, but the age-related patterns differed for children with vs. without CP. In general, children with vs. without CP were more likely to fracture at the vertebral column, hip, and lower extremities and less likely to fracture at the upper extremities, which is consistent with a 1-year cross-sectional study that grouped children as 2–7, 8–11, 12–14, and 15–17 years old.17 The findings from this study may be able to assist clinicians strategize at what age to implement fracture prevention efforts. For example, in this study, children <1 to 4 years old with CP had a ~10% 5-year risk of fracture, while children 5–7 years old with CP had a ~13% 5-year risk of fracture and children 8–13 years old had a ~15–20% 5-year risk of fracture, with the majority of fractures occurring at particularly debilitating sites; i.e., vertebral column, hip, and lower extremities. Thus, fracture prevention efforts should be considered early in life for children with CP and with increasing clinical prioritization throughout growth.
This study found no evidence that the age-related 5-year fracture risk patterns differed by clinically relevant patient-level factors. Thus, the HR can be interpreted as a consistent effect by that patient-level factor for each year of age among children with CP. For example, the HR for sex was 1.29 for the adjusted fracture rate at the upper extremities, suggesting that males vs. females had a ~29% higher adjusted 5-year fracture rate for each year of age.
Notably, co-occurring intellectual disabilities and evidence of wheelchair use were associated with higher 5-year adjusted rate of fractures at the vertebral column, hip, or lower extremities, but not for the upper extremities. These variables may reflect on the child’s medical complexity (co-occurring intellectual disabilities) and extent of bone fragility (wheelchair use).27 This is consistent with a study that found greater deficits in musculoskeletal mass in the lower vs. upper extremities among children with vs. without CP, but these lower extremity deficits were greater in children with CP that were non-ambulatory vs. ambulatory.30 However, it is important to note that while the adjusted 5-year rate of fracture was elevated for children with CP that had evidence of wheelchair use, bone fragility is still a problem for ambulatory children with mild forms of CP.2 The first sensitivity analysis in this study supports this notion. Even among children with CP without evidence of wheelchair use, their 5-year risk of fracture at the vertebral column, hip, or lower extremities was 38% higher compared to children without CP. Taken together, early fracture prevention efforts are needed for children with mild to severe forms of CP.
Overviews of factors driving bone fragility and fracture, and opportunities to improve bone health among individuals with CP have been discussed elsewhere (e.g., refs. 31,32,33,34,35). Briefly, low activity and fitness levels, CP characteristics (e.g., type of CP, affected body regions, severity), motor dysfunction and resultant low weight-bearing, altered body composition of high fat and low fat-free mass, altered biology and pubertal development, comorbidities, other forms of medical complexity (e.g., medications, multiple surgeries), nutritional deficiencies, and societal factors, among other factors, can influence abnormal bone development and heighten fracture risk for children with CP.2,23,35,36,37,38,39,40,41,42 Further research is needed to better understand the complex multi-factorial reasons for fracture vulnerability and the activities that lead to a fracture event for children with CP,18 ultimately to inform personalized and effective intervention design for fracture prevention.
Generalizability of study findings from this privately insured cohort to the broader pediatric population with CP is not exactly known. Population-based evidence from a nationally representative sample of U.S. children 0–17 years of age suggests that the majority (65.3%) of children with CP were covered by private insurance in the year 2016, and there were no differences in parental report of age, sex, or severity of CP between children with private vs. public insurance coverage.17 However, children with CP with private vs. public insurance had a lower proportion of Black children (6.8 vs. 35.8%). In the current study, 8.1% of children with CP were Black, but 17.7% had missing data on race, hindering attempts to make comparisons with national estimates. In addition, in this study, ~15% of children with CP had co-occurring intellectual disabilities and ~31% had co-occurring epilepsy, which is lower than the ~28% and slightly lower than the ~35–39%, respectively, reported from population-based studies in children with CP.43,44 A previous population-based study found that ~33% of children with CP have “limited or no walking” ability.44 In the current study, ~36% of children with CP in this study had evidence of wheelchair use (17% with evidence in 2 separate years), but the variables to capture ambulatory ability are different, making it difficult to compare across studies.44 Taken together, this study may represent a slightly less medically complex segment of the pediatric population with CP with possible insufficient racial representation although fracture risk does not appear to be associated with race in children with CP.15
The limitations that directly influence interpretations of this study must be discussed. The true age is ±364 days of the calculated age due to the variable provided in the database. This may have masked significant deviations in fracture risk patterns by each year of age, but this is anticipated to have a negligible impact on conclusions drawn. Claims data does not contain sufficient information about the severity of CP. Prior studies have attempted to classify the severity of CP using claims data, but the majority of individuals were unable to be classified.45,46 This study constructed a variable to indicate (non-)ambulatory status to serve as a proxy for severity of CP. However, this approach is not validated and it is unknown how well it captures ambulatory ability. Evidence of baseline co-occurring intellectual disabilities and epilepsy were determined using the full 5-year period. An assumption was made that these conditions were present prior to study entry, but some children may have developed these conditions after study entry, thus misclassifying the “baseline” status of these co-occurring conditions. This is anticipated to be rare and unlikely to bias the study findings.
This study provides novel epidemiologic evidence of 5-year fracture risk for each year of age during growth for children with CP, and the association by clinically relevant patient-level factors to enhance clinical detection and strategize population-based fracture prevention efforts.
Data availability
The data that support the findings of this study are available from the Optum's de-identified Clinformatics Data Mart Database but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are not available from the authors.
References
Appleton, R. E. & Gupta, R. Cerebral palsy: not always what it seems. Arch. Dis. Child. 104, 809–814 (2019).
Whitney, D. G. et al. Cortical bone deficit and fat infiltration of bone marrow and skeletal muscle in ambulatory children with mild spastic cerebral palsy. Bone 94, 90–97 (2017).
Modlesky, C. M., Kanoff, S. A., Johnson, D. L., Subramanian, P. & Miller, F. Evaluation of the femoral midshaft in children with cerebral palsy using magnetic resonance imaging. Osteoporos. Int. 20, 609–615 (2009).
Henderson, R. C. et al. The relationship between fractures and DXA measures of BMD in the distal femur of children and adolescents with cerebral palsy or muscular dystrophy. J. Bone Min. Res 25, 520–526 (2010).
Henderson, R. C., Kairalla, J. A., Barrington, J. W., Abbas, A. & Stevenson, R. D. Longitudinal changes in bone density in children and adolescents with moderate to severe cerebral palsy. J. Pediatr. 146, 769–775 (2005).
Walker, J. L. et al. Differences in body composition according to functional ability in preschool-aged children with cerebral palsy. Clin. Nutr. 34, 140–145 (2015).
Elder, G. C. et al. Contributing factors to muscle weakness in children with cerebral palsy. Dev. Med. Child Neurol. 45, 542–550 (2003).
Rose, J. & McGill, K. C. Neuromuscular activation and motor-unit firing characteristics in cerebral palsy. Dev. Med. Child Neurol. 47, 329–336 (2005).
Etter, J. P. et al. The respiratory disease burden of non-traumatic fractures for adults with cerebral palsy. Bone Rep. 13, 100730 (2020).
Whitney, D. G., Bell, S., Etter, J. P. & Prisby, R. D. The cardiovascular disease burden of non-traumatic fractures for adults with and without cerebral palsy. Bone 136, 115376 (2020).
Whitney, D. G. et al. The mortality burden of non-trauma fracture for adults with cerebral palsy. Bone Rep. 13, 100725 (2020).
Presedo, A., Dabney, K. W. & Miller, F. Fractures in patients with cerebral palsy. J. Pediatr. Orthop. 27, 147–153 (2007).
Leet, A. I., Shirley, E. D., Barker, C., Launay, F. & Sponseller, P. D. Treatment of femur fractures in children with cerebral palsy. J. Child Orthop. 3, 253–258 (2009).
Baxter-Jones, A. D., Faulkner, R. A., Forwood, M. R., Mirwald, R. L. & Bailey, D. A. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J. Bone Min. Res. 26, 1729–1739 (2011).
Stevenson, R. D. et al. Fracture rate in children with cerebral palsy. Pediatr. Rehabil. 9, 396–403 (2006).
Uddenfeldt Wort, U., Nordmark, E., Wagner, P., Duppe, H. & Westbom, L. Fractures in children with cerebral palsy: a total population study. Dev. Med. Child Neurol. 55, 821–826 (2013).
Whitney, D. G., Hurvitz, E. A. & Caird, M. S. Critical periods of bone health across the lifespan for individuals with cerebral palsy: informing clinical guidelines for fracture prevention and monitoring. Bone 150, 116009 (2021).
Kannikeswaran, S. et al. Fracture characteristics by age, sex, and ambulatory status among individuals with cerebral palsy: a descriptive study. Disabil. Rehabil. https://doi.org/10.1080/09638288.2021.1921860 (2021).
von Keudell, A. et al. Treatment options for distal femur fractures. J. Orthop. Trauma 30(Suppl 2), S25–S27 (2016).
Mubark, I. et al. Mortality following distal femur fractures versus proximal femur fractures in elderly population: the impact of best practice tariff. Cureus 12, e10744 (2020).
Kirmani, S. et al. Bone structure at the distal radius during adolescent growth. J. Bone Min. Res. 24, 1033–1042 (2009).
Hegazi, M. A. et al. Growth hormone/insulin-like growth factor-1 axis: a possible non-nutritional factor for growth retardation in children with cerebral palsy. J. Pediatr. 88, 267–274 (2012).
Kuperminc, M. N. et al. Puberty, statural growth, and growth hormone release in children with cerebral palsy. J. Pediatr. Rehabil. Med. 2, 131–141 (2009).
Nazif, H. et al. Bone mineral density and insulin-like growth factor-1 in children with spastic cerebral palsy. Childs Nerv. Syst. 33, 625–630 (2017).
Whitney, D., Kamdar, N., Hirth, R. A., Hurvitz, E. A. & Peterson, M. D. Economic burden of paediatric-onset disabilities among young and middle-aged adults in the USA: a cohort study of privately insured beneficiaries. BMJ Open 9, e030490 (2019).
Hubermann, L., Boychuck, Z., Shevell, M. & Majnemer, A. Age at referral of children for initial diagnosis of cerebral palsy and rehabilitation: current practices. J. Child Neurol. 31, 364–369 (2016).
Reid, S. M., Meehan, E. M., Arnup, S. J. & Reddihough, D. S. Intellectual disability in cerebral palsy: a population-based retrospective study. Dev. Med. Child Neurol. 60, 687–694 (2018).
Sellier, E. et al. Epilepsy and cerebral palsy: characteristics and trends in children born in 1976-1998. Eur. J. Paediatr. Neurol. 16, 48–55 (2012).
Whitney, D. G. et al. Timecourse of morbidity onset among adults living with cerebral palsy. Am. J. Prev. Med. 61, 37–43 (2021).
Zhang, C., Colquitt, G., Miller, F., Shen, Y. & Modlesky, C. M. Preferential deficit of fat-free soft tissue in the appendicular region of children with cerebral palsy and proposed statistical models to capture the deficit. Clin. Nutr. 39, 1541–1550 (2020).
Whitney, D. G. et al. Bone marrow fat physiology in relation to skeletal metabolism and cardiometabolic disease risk in children with cerebral palsy. Am. J. Phys. Med. Rehabil. 97, 911–919 (2018).
Gannotti, M. E., Liquori, B. M., Thorpe, D. E. & Fuchs, R. K. Designing exercise to improve bone health among individuals with cerebral palsy. Pediatr. Phys. Ther. 33, 50–56 (2021).
Modlesky, C. M. & Zhang, C. Complicated muscle-bone interactions in children with cerebral palsy. Curr. Osteoporos. Rep. 18, 47–56 (2020).
Hough, J. P., Boyd, R. N. & Keating, J. L. Systematic review of interventions for low bone mineral density in children with cerebral palsy. Pediatrics 125, e670–e678 (2010).
Jesus, A. O. & Stevenson, R. D. Optimizing nutrition and bone health in children with cerebral palsy. Phys. Med. Rehabil. Clin. N. Am. 31, 25–37 (2020).
Nooijen, C. et al. Health-related physical fitness of ambulatory adolescents and young adults with spastic cerebral palsy. J. Rehabil. Med. 46, 642–647 (2014).
Whitney, D. G., Miller, F., Pohlig, R. T. & Modlesky, C. M. BMI does not capture the high fat mass index and low fat-free mass index in children with cerebral palsy and proposed statistical models that improve this accuracy. Int. J. Obes. 43, 82–90 (2019).
Mughal, M. Z. Fractures in children with cerebral palsy. Curr. Osteoporos. Rep. 12, 313–318 (2014).
Rehbein, I. et al. Analysis of orthopedic surgical procedures in children with cerebral palsy. World J. Orthop. 11, 222–231 (2020).
Sung, K. H. et al. Differences in body composition according to gross motor function in children with cerebral palsy. Arch. Phys. Med. Rehabil. 98, 2295–2300 (2017).
Devesa, J., Casteleiro, N., Rodicio, C., Lopez, N. & Reimunde, P. Growth hormone deficiency and cerebral palsy. Ther. Clin. Risk Manag. 6, 413–418 (2010).
Worley, G. et al. Secondary sexual characteristics in children with cerebral palsy and moderate to severe motor impairment: a cross-sectional survey. Pediatrics 110, 897–902 (2002).
Hollung, S. J. et al. Comorbidities in cerebral palsy: a patient registry study. Dev. Med. Child Neurol. 62, 97–103 (2020).
Kirby, R. S. et al. Prevalence and functioning of children with cerebral palsy in four areas of the United States in 2006: a report from the autism and developmental disabilities monitoring network. Res. Dev. Disabil. 32, 462–469 (2011).
Pulgar, S. et al. Prevalence, patterns, and cost of care for children with cerebral palsy enrolled in Medicaid managed care. J. Manag. Care Spec. Pharm. 25, 817–822 (2019).
Conner, B. C., Xu, T., Kamdar, N. S., Haapala, H. & Whitney, D. G. Physical and occupational therapy utilization and associated factors among adults with cerebral palsy: longitudinal modelling to capture distinct utilization groups. Disabil. Health J. 101279 (2022).
Funding
This work was supported by the University of Michigan Office of Health Equity and Inclusion Diversity Fund.
Author information
Authors and Affiliations
Contributions
The author has met the Pediatric Research authorship requirements.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Ethics approval and consent to participate
The data were de-identified prior to administering to researchers, and patient consent is not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Whitney, D.G. 5-year fracture risk among children with cerebral palsy. Pediatr Res 93, 996–1002 (2023). https://doi.org/10.1038/s41390-022-02207-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02207-4