Abstract
Background
Despite the widespread clinical perception that hypoglycemia may drive weight gain in youth with type 1 diabetes (T1D), there is an absence of published evidence supporting this hypothesis.
Methods
We estimated the body fat percentage (eBFP) of 211 youth (HbA1c 8.0–13.0%, age 13–16) at baseline, 6, and 18 months of the Flexible Lifestyles Empowering Change trial using validated equations. Group-based trajectory modeling assigned adolescents to sex-specific eBFP groups. Using baseline 7-day blinded continuous glucose monitoring data, “more” vs. “less” percent time spent in hypoglycemia was defined by cut-points using sample median split and clinical guidelines. Adjusted logistic regression estimated the odds of membership in an increasing eBFP group comparing youth with more vs. less baseline hypoglycemia.
Results
More time spent in clinical hypoglycemia (defined by median split) was associated with 0.29 the odds of increasing eBFP in females (95% CI: 0.12, 0.69; p = 0.005), and 0.33 the odds of stable/increasing eBFP in males (95% CI: 0.14, 0.78; p = 0.01).
Conclusions
Hypoglycemia may not be a major driver of weight gain in US youth with T1D and HbA1c ≥8.0. Further studies in different sub-groups are needed to clarify for whom hypoglycemia may drive weight gain and focus future etiological studies and interventions.
Impact
-
We contribute epidemiological evidence that hypoglycemia may not be a major driver of weight gain in US youth with type 1 diabetes and HbA1c ≥8.0% and highlight the need for studies to prospectively test this hypothesis rooted in clinical perception.
-
Future research should examine the relationship between hypoglycemia and adiposity together with psychosocial, behavioral, and other clinical factors among sub-groups of youth with type 1 diabetes (i.e., who meet glycemic targets or experience a frequency/severity of hypoglycemia above a threshold) to further clarify for whom hypoglycemia may drive weight gain and progress etiological understanding of and interventions for healthy weight maintenance.
Similar content being viewed by others
Overweight and obesity compound the elevated cardiovascular disease risk faced by individuals with type 1 diabetes, underscoring the need to understand the reasons for weight gain in this population and develop strategies for healthy weight maintenance.1,2 Overweight is associated with hypertension, dyslipidemia, inflammation, oxidative stress, and further challenges to glycemic levels through disruptions in insulin sensitivity as well as fat and carbohydrate metabolism.2,3 Critically, there are data to suggest that the cardiometabolic risks associated with being overweight or obese may offset the protective effects of intensive insulin therapy for cardiovascular health.4
The added cardiovascular health risk of overweight among individuals with type 1 diabetes is of particular concern in youth. Glycemic levels are highest during adolescence than at any other point in the lifespan.5 Moreover, the prevalence of overweight among youth with type 1 diabetes has recently surpassed that of the general population.6,7 Evidence that health behaviors and overweight track into adulthood further compels the importance of identifying and intervening upon drivers of weight gain during this developmental stage.8
Weight gain in youth with type 1 diabetes is currently posited to occur both through pathways relevant to populations without type 1 diabetes as well as pathways unique to type 1 diabetes.2,9,10 In the general population, overweight is attributed to a confluence of biological, behavioral, social, and environmental factors.11 Correlates of overweight in the general population such as race, ethnicity, and socioeconomic factors are associated with overweight among youth with type 1 diabetes.12 Despite its central role in preventing micro- and macrovascular complications, intensive insulin therapy is a key type 1 diabetes-specific factor that is associated with weight gain in some individuals.4,13 Potential mediators of this association include decreased glucosuria, increased lipogenesis from hyperinsulinemia, greater flexibility in food choices and timing as compared to fixed-dose therapy, and increased energy intake in response to hypoglycemia.2,9,10,14,15,16 This last potential driver of weight gain specific to type 1 diabetes was of interest to the present analysis. We aimed to explore the clinical perception that hypoglycemia may lead to eating more food than needed to stabilize blood glucose, resulting in excess energy consumption. Specifically, fear of impending hypoglycemia, hypoglycemia-induced hunger, or errors in insulin timing or dose may result in repeated positive energy balance which, over time, may lead to weight gain.2,9,10
Most studies of weight gain in youth with type 1 diabetes use body mass index (BMI) to measure weight status despite well-known limitations of BMI to accurately characterize adiposity (e.g., overestimates adiposity in males) or capture change in adiposity over time, particularly in youth.6,7,17,18,19,20,21 SEARCH for Diabetes in Youth examined socioeconomic correlates of longitudinal estimated adiposity in a surveillance cohort of American youth with type 1 diabetes using validated equations to estimate percent body fat from anthropometric data.12,22 However, no studies have attempted to objectively examine associations between hypoglycemia and weight gain using longitudinal adiposity data and objective hypoglycemia measures derived from blinded continuous glucose monitoring (CGM) despite the widespread clinical perception that hypoglycemia is a driver of overeating and potentially weight gain in youth with type 1 diabetes. To begin to address this gap, our aim was to examine whether greater time spent in hypoglycemia was associated with greater odds of an increasing estimated adiposity trajectory.
Methods
Subjects
This study is part of a series of observational, post-hoc analyses of the 18-month Flexible Lifestyles Empowering Change (FLEX) multi-site randomized controlled trial (NCT01286350) that aim to inform the design of future interventions for youth with type 1 diabetes. FLEX tested the efficacy of a behavior change intervention to improve glycated hemoglobin (HbA1c) among 258 youth 13–16 years of age with type 1 diabetes and sub-optimal glycemic levels (baseline HbA1c 8.0–13.0%).23 Additional eligibility criteria included type 1 diabetes duration ≥1 year, literacy in English, primary caregiver willing to participate, and no other serious medical conditions or pregnancy. In brief, the design included intervention sessions delivered by Certified Diabetes Care and Education Specialists who combined motivational interviewing, family-systems therapy, and problem-solving skills training in order to help youth identify, execute, and refine personally relevant and realistic diabetes self-management goals. Written informed consent and assent were provided by parent and adolescent, respectively, at the first in-person baseline measurement visit. Institutional Review Board approval was obtained at each of the participating sites (Cincinnati Children’s Hospital Medical Center; University of Colorado Barbara Davis Center for Childhood Diabetes; University of North Carolina at Chapel Hill). The FLEX trial is described in detail elsewhere.23
Dependent variable: estimated body fat percentage (eBFP) trajectory group
Anthropometry was collected at baseline, 6, and 18 months of FLEX. Weight was measured to the nearest 0.1 kg using an electronic scale, height was measured in centimeters using a stadiometer, and waist circumference was measured using NHANES and minimum/natural waist methods.24 To create a measure of estimated adiposity for each participant at 0, 6, and 18 months, we employed age and race-specific equations that were developed from 1999 to 2006 NHANES data to predict body fat percentage (eBFP) in Americans 8 years and older using weight, height, and waist circumference measurements.22 We selected this method because it provides an improved estimate of adiposity over BMI. Though useful as an inexpensive, crude measure of population adiposity, BMI is an imperfect proxy of adiposity because it does not distinguish between lean and fat mass, is differentially accurate by sex and race/ethnicity, and is an unreliable measurement of change in adiposity over time especially when used in growing children and adolescents.19,20,21,25,26 The equations we selected were validated against DXA measurements in a representative sample of Americans, including youth the same age as those who participated in FLEX.22 DXA measurements reliably and validly monitor small changes in body composition in children and adolescents.27 To specify 18-month eBFP trajectories in our cohort, we used group-based trajectory modeling (SAS PROC TRAJ), which fit a semi-parametric model with eBFP measurements from 0, 6, and 18 months using the maximum-likelihood method.28 Modeling was sex-stratified because of well-known sex differences in body composition changes throughout adolescence.29 This stratified approach avoided generating estimated adiposity trajectory groups that obscure and mischaracterize the patterns of change in estimated adiposity among males and females (e.g., males with a slight increase in adiposity relative to other males being inappropriately grouped in a stable or even decreasing trajectory group due to larger relative increases in adiposity among females, and females with a decrease in adiposity relative to other females being inappropriately grouped in a stable or increasing adiposity group due to larger relative decreases in adiposity among males). To specify the number of trajectory groups among each cohort of males and females, we compared n-group solutions across multiple criteria: change Bayesian information criterion and log form of the Bayes factors values (change in BIC of ≥20 and log Bayes factor of ≥6 as suggestive of strong to very strong evidence in favor of the more complex model), average group posterior probabilities (≥0.70), percent of the sample in each group (≥5%), the interpretability and distinctness of each trajectory group, and the ability of the chosen solution to address the substantive research question at hand.28,30,31 Participants were assigned to their trajectory group using the maximum probability rule, which places the participants in the group where their posterior probability of membership is highest.28,30,31
Independent variable: hypoglycemia
At baseline of the FLEX trial, all 258 enrolled participants wore a 7-day blinded CGM [iPro®2 Professional CGM; Medtronic Diabetes, Northridge, CA], meaning that unless they used a personal CGM as part of their usual self-management, participants did not have the awareness to readings that might influence their behavior. Further details about the device and how participants were counseled to use it are published elsewhere.23,32 To help ensure that the blinded baseline CGM wear time data represented participants’ usual glycemic levels, the study protocol permitted continued use of any resources relied upon for routine self-management, which included simultaneous use of a personal CGM in addition to the blinded CGM worn at baseline. This protocol was selected in order to minimize disruption of usual self-management behaviors and introduction of bias to the health indicators collected as part of the study.
Consistent with international consensus guidelines, hypoglycemia was defined as <70 mg/dL, where “clinical alert hypoglycemia” was defined as 54–69 mg/dL, and “clinically serious hypoglycemia” was defined as <54 mg/dL.33 We modeled the percent time spent in hypoglycemia during the 7-day blinded CGM wear time in two ways in order to facilitate understanding the relationship between hypoglycemia and longitudinal adiposity within our sample while also facilitating comparison with other studies. In the first, we assigned participants to a “more” vs. “less” hypoglycemia category using the median percent time in hypoglycemia of our whole study sample as the cut-point (i.e., those above the median of 2.0% for <70 mg/dL, 1.5% for 54–69 mg/dL and 0.3% for <54 mg/dL were categorized as “more”, and those below were categorized as “less”). The overall median from the cohort of males and females combined (vs. sex-specific medians) was used to categorize participants by “more” or “less” categories due to nominal differences between males and females across hypoglycemia metric medians. For the second binary specification of time spent in hypoglycemia (i.e., <1% vs. ≥1% time spent <54 mg/dL and 4% vs. ≥4% time spent <70 mg/dL), we used clinical cut-points put forth by international consensus guidelines.33 Supplementary Table S1 displays the mean percent time spent in hypoglycemia within each of the groups defined by median split and clinical cut-points.
Missing data
Participants were excluded from the analysis if they were missing any eBFP measurement due to missing waist circumference measurements (n = 22). Another two participants with 10% absolute change in eBFP between 0 and 6 months, and again between 6 and 18 months were excluded as outliers (>4 SE from the mean). Twenty-one participants with missing CGM data were excluded. A participant who spent 58.3% of nighttime (12:00–06:00 AM) <70 mg/dL and a participant who spent 21.3% of overall time <54 mg/dL were excluded due to suspected measurement error. A total of 211 participants were included. Those excluded (n = 47) did not differ from those included in the analysis by age, sex, race/ethnicity, health insurance status, parental education, diabetes duration, baseline HbA1c, or any psychosocial measures, but did have lower mean BMI z-score (−0.47; p = 0.002) and percentile (−13.1; p = 0.001).
Statistical analyses
Trajectory group modeling and regression modeling were sex-stratified due to well-established differences in body composition trajectories in males and females throughout puberty.29 For each trajectory group, we graphed the 0–6-month and 6–18-month changes in eBFP for each group member and examined the direction of change between each time point in order to select trajectory group names that best characterized the change in eBFP experienced by group members (i.e., increasing, decreasing, stable). The means and frequencies of baseline demographic and clinical characteristics by trajectory group were compared using chi-square for categorical and ANOVA or Kruskal–Wallis for continuous variables. Logistic regression estimated the association between categories of percent time spent in hypoglycemia at baseline and odds of membership in increasing vs. decreasing 18-month eBFP trajectory groups (adjusted for baseline eBFP, age, Ohio/Colorado study site, and intervention/control group). All analyses were conducted in SAS (version 9.4; Cary, NC).
Results
The study sample (n = 211) was 50.7% female and 76.8% non-Hispanic White, with mean age of 14.9 ± 1.1 years, T1D duration of 6.3 ± 3.8 years and HbA1c of 9.6 ± 1.3% at baseline. The majority of participants (76.8%) used an insulin pump. Among females (n = 107), mean eBFP at baseline was 33.2 ± 5.4 and percent time below range during the 1-week blinded CGM wear time was 2.2 ± 2.6% (54–69 mg/dL) and 1.5 ± 2.5% (<54 mg/dL). Among males (n = 104), mean eBFP at baseline was 21.1 ± 4.8 and percent time below range was 2.1 ± 2.6% (54–69 mg/dL) and 1.5 ± 2.6% (<54 mg/dL).
Trajectory modeling
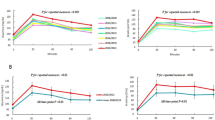
As depicted in Fig. 1, group-based trajectory modeling identified two eBFP trajectories in males and females. Approximately half of males followed a stable or increasing eBFP trajectory (“stable/increasing” trajectory group; n = 51; mean eBFP at baseline: 20.0 ± 4.5, 6 months: 20.8 ± 4.3, 18 months: 20.9 ± 4.8) vs. a decreasing eBFP trajectory (“decreasing” trajectory group; n = 53; mean eBFP at baseline: 22.3 ± 4.8, 6 months: 20.7 ± 5.1, 18 months:19.6 ± 4.8). A slight majority of females followed an increasing eBFP trajectory (“increasing” trajectory group; n = 60; mean eBFP at baseline: 31.9 ± 5.0, 6 months: 33.2 ± 5.2, 18 months: 35.0 ± 5.0) compared to a stable or decreasing eBFP trajectory (“stable/decreasing” trajectory group; n = 47; mean eBFP at baseline: 34.9 ± 5.2, 6 months: 34.6 ± 5.2, 18 months: 34.6 ± 4.9). At 0, 6, and 18 months, mean eBFP among males was lower than mean eBFP among females (Fig. 1). Figure 1 also illustrates how the slope of change in eBFP in the stable/decreasing eBFP trajectory group among females is less steep than that of the decreasing eBFP trajectory group among males (mean change in eBFP 0–6 months: −0.2 ± 0.9 vs. −1.6 ± 1.6, p ≤ 0.001; 6–18 months: −0.3 ± 1.4 vs. −2.7 ± 1.6, p ≤ 0.001), whereas the slope of change in eBFP in the increasing eBFP trajectory group among females is more steep than the stable/increasing eBFP trajectory group among males (mean change in eBFP 0–6 months: 1.3 ± 1.4 vs. 0.8 ± 1.4, p = 0.05; 6–18 months: 3.1 ± 1.3 vs. 0.9 ± 1.7, p ≤ 0.001).
Mean (SE) change in estimated body fat percentage (eBFP) in male (a) and female (b) FLEX trial participants over 18 months. Sex-stratified group-based trajectory modeling identified a stable/increasing (A1) eBFP trajectory and decreasing (A2) eBFP trajectory in males and an increasing (B1) eBFP trajectory and stable/decreasing (B2) eBFP trajectory in females.
Among males and among females, baseline eBFP differed between eBFP trajectory groups (Table 1). Males who followed a decreasing eBFP trajectory had a higher eBFP at baseline compared to those who followed a stable/increasing eBFP trajectory (22.3 ± 4.8 vs. 20.0 ± 4.5; p = 0.01). Similarly, females who followed a stable/decreasing eBFP trajectory had a higher mean baseline eBFP than females who followed an increasing eBFP trajectory (34.9 ± 5.2 vs. 31.9 ± 5.3; p = 0.01).
For both males and females, percent time spent below the range (<70 mg/dL) was greater among those in the decreasing vs. stable/increasing group (males) and stable/decreasing vs. increasing group (females). This difference in percent time below range was only statistically significant for males (males: 5.1 ± 5.9% in the decreasing eBFP trajectory group vs. 2.1 ± 2.8% in stable/increasing eBFP trajectory group; p = 0.003) and the magnitude of the difference was more pronounced than in females.(females: 4.2 ± 5.2% in the stable/decreasing group vs. 3.3 ± 4.4% in the increasing group, p = 0.16). As depicted in Table 1, this pattern was consistent across percent time spent in both clinical (54–69 mg/dL) and clinically serious (<54 mg/dL) hypoglycemia.
Additional demographic and clinical characteristics by sex and trajectory group can be found in Supplementary Table S2.
Regression modeling
Table 2 presents sex-stratified adjusted logistic regression model results, in which the odds ratios correspond to the odds of following an increasing vs. stable/decreasing 18-month eBFP trajectory (females) or stable/increasing vs. decreasing 18-month eBFP trajectory (males) comparing those with more vs. less time spent in hypoglycemia (as measured by median split and clinical cut-points) during the 7-day blinded CGM wear time at baseline.
Males who spent more time in hypoglycemia, as defined by both median split and clinical cut-points, had reduced odds of following a stable/increasing 18-month eBFP trajectory. More (vs. less) time spent in clinical hypoglycemia (defined by median split) was associated with 0.33 times the odds of following a stable/increasing eBFP trajectory (95% CI: 0.14, 0.78; p = 0.01), and spending ≥4% (vs. <4%) time above the cut-point for clinical hypoglycemia was associated with 0.27 times the odds of following a stable/increasing eBFP trajectory (95% CI: 0.10, 0.72; p = 0.009). Spending ≥1% (vs. <1%) above the cut-point for clinically serious hypoglycemia was associated with 0.40 the odds of following a stable/increasing eBFP trajectory (95% CI: 0.16, 1.0; p = 0.05). The direction of the odds ratio comparing more vs. less clinically serious hypoglycemia (defined by median split instead of clinical cut-point) was consistent with this finding, but was not statistically significant (OR: 0.60; 95% CI: 0.26, 1.36; p = 0.22).
In aggregate, the direction and statistical significance of the odds ratios among females indicate that more hypoglycemia at baseline was associated with lower odds of following an increasing eBFP trajectory (Table 2). More time spent in clinical hypoglycemia (defined by median split) was associated with 0.29 the odds of following an increasing eBFP trajectory (95% CI: 0.12, 0.69; p = 0.005). Although not statistically significant, the odds ratios for clinically serious hypoglycemia and those for which clinical cut-points were used to specify time spent in hypoglycemia (<4% clinical hypoglycemia and <1% clinically serious hypoglycemia), also suggest an association between more time spent in hypoglycemia and increased odds of following a stable/decreasing eBFP trajectory as opposed to increasing trajectory.
Discussion
We estimated sex-specific 18-month body fat percentage trajectories of 211 adolescents with HbA1c ≥8.0 in the FLEX trial and found that contrary to clinical anecdote, more time spent in hypoglycemia at baseline was associated with lower odds of membership in the group with increasing estimated percent body fat over time. This association was consistent in both males and females. Our results posit that although hypoglycemia could indeed be a driver of weight gain in specific individuals, adult or youth sub-groups with type 1 diabetes (i.e., youth who meet glycemic level targets or who experience a frequency hypoglycemia above a particular threshold), hypoglycemia is perhaps not the main driver of weight gain in the broader population of youth with HbA1c ≥8.0%.34
The eBFP trajectories we identified for males and females are consistent with what is known about sex-specific body composition changes through puberty.29 Sex-specific hormones lead to increasing fat mass in females and increasing muscle mass in males, as reflected by the eBFP trajectories among males (stable/increasing and decreasing) and females (increasing and stable/decreasing) where the slope of the decreasing trajectory in males was steeper than that of the stable/decreasing trajectory in females, and the slope of the increasing trajectory in females was steeper than that of the stable/increasing trajectory in males. Critically, 47.4% of males and females in our cohort of adolescents had obesity based on their estimated percent body fat (according to commonly used cut-points of ≥25% in males and ≥30% in females), underscoring the need to understand the drivers of weight gain and identify weight management interventions in this age group.35,36,37,38,39,40
Approximately 16% of males in our sample (n = 17) were classified as normal weight by percent body fat (<25%) but classified as overweight or obese by BMI (≥85 percentile), and approximately 32% of females (n = 34) were classified as obese by percent body fat (≥30%) but classified as normal weight by BMI (<85 percentile). These findings are consistent with the literature that shows BMI can overestimate adiposity in males and underestimate adiposity in females, highlighting the importance of using alternative measures where feasible when investigating associations between adiposity and other health factors.41
An unexpected finding was that the association between more time spent in hypoglycemia and a decreasing estimated adiposity trajectory was more marked in males (i.e., in terms of the magnitude and statistical significance of the odds ratios and consistency of observing this association across all hypoglycemia metrics modeled). These data therefore highlight a potential benefit of continuous clinical monitoring of body composition throughout puberty to calculate insulin needs, particularly in males, given that the increase in muscle and decrease in fat mass that characterize the change in male body composition during puberty might mean a greater likelihood of improper insulin calculations based on weight, and thus more hypoglycemia.
Compared to the two-group trajectory solution we identified in the present analysis, SEARCH for Diabetes in Youth used parallel modeling criteria to specify three distinct eBFP trajectories among males (n = 376) and females (n = 363) over approximately 7 years.12 Comparisons to the present analysis are limited because the SEARCH trajectories were specified for a sample with mean HbA1c below 8.0% and followed individuals from diabetes diagnosis starting from 10 years of age as well as starting after puberty (vs. ≥8.0% baseline HbA1c, 6.3 ± 3.8 years diabetes duration, and 14.9 ± 1.1 years of age in our FLEX sample). Key characteristics of the sex-specific trajectories—namely the tendency for the male trajectories to decrease and female trajectories to increase—were similar between the SEARCH analysis and the present analysis. However, a larger, more population-representative sample (n = 739) enabled the SEARCH study to identify a greater number of distinct groups and maintain sufficient group membership to analyze associations between these trajectories and other variables. We thus acknowledge that the 2-group trajectory solution that we identified as most appropriate to characterize our sample after considering both fit statistics and our study aims may have resulted in a mixing of increasing trajectories with stable trajectories among males or decreasing trajectories with stable trajectories among females, which may have obscured important insights about the relationship between hypoglycemia and estimated adiposity among our target population—youth 12–17 years of age with sub-optimal HbA1c (≥8.0%).
The present study findings are consistent with previous findings from the FLEX trial showing that BMI z-score at trial baseline was not significantly associated with time spent in clinical or clinically serious hypoglycemia, and more recently, that daily total energy intake did not differ on days with and without hypoglycemia.12,42 The average HbA1c of youth included in the FLEX trial (≥8.0%), and thus the present analysis, is representative of the average HbA1c among youth in the US and parts of Europe, which underscores the important and relevant contribution of the present analysis to the still limited knowledge about the drivers of weight gain in youth with type 1 diabetes.5,6,7
To gain further insight into the broader context of glycemic management in which we observed a relationship between more hypoglycemia and stable or decreasing eBFP, we compared other CGM-based glycemic metrics as well as behavioral and psychological metrics across the eBFP trajectory groups (Supplementary Table S2). Notably, in addition to greater mean percent time in hypoglycemia among males in the decreasing vs. stable/increasing eBFP trajectory group (5.1 ± 5.9% vs. 2.1 ± 2.8%; p = 0.003), males in the decreasing eBFP trajectory group had greater mean percent time in range, as well as lower HbA1c and percent time spent above range (Supplementary Table S2). When interpreted alongside these other metrics of glycemic level management, a greater mean percent time spent in hypoglycemia is plausibly a proxy indicator for behaviors or other factors that facilitate tighter management of glycemic levels. Unfortunately, sample size constraints precluded the inclusion of multiple social, psychological, clinical, and diabetes management behavior variables in our models that could shed further light on the unanticipated association we observed between hypoglycemia and estimated adiposity. Interestingly, despite not adjusting for factors that have been demonstrated by other studies to shape glycemic levels and weight status (e.g., diabetes self-management behaviors, disordered eating), we note that a number of these potential confounders did not statistically significantly differ by eBFP trajectory group (Supplementary Table S2), which therefore suggests adjustment for these factors would not have markedly changed our findings.2,9,10 It is also possible that other self-management indicators that were not collected as part of this analysis (e.g., treating hypoglycemia only when blood glucose <70 mg/dL vs. proactively treating before <70 mg/dL) confounded the associations observed.
We did not control for estimates of caloric intake or physical activity during the baseline blinded CGM wear time. Our previous exploratory analyses in this cohort showed that caloric intake did not differ on days with or without hypoglycemia.42 Unfortunately, physical activity data collected during the baseline blinded CGM wear time from which we assessed hypoglycemia was missing in almost half of the study participants, which precluded us from adjusting for this potentially important confounder. Future studies that examine matched physical activity, dietary intake, and hypoglycemia data over a long enough period to capture meaningful changes in adiposity will be key in untangling the relationships between hypoglycemia and weight gain.
Although we adjusted for age in our regression models and age differed only slightly between trajectory groups (Supplementary Table S2), age is an imperfect proxy for physical or behavioral maturity. We acknowledge the possibility of residual confounding by the pubertal development stage, which shapes body fat trajectory while also impacting prevention or response to hypoglycemia through behavioral and hormonal pathways.43,44 Interestingly, even assuming that the slightly older adolescents in the decreasing (males) or stable/decreasing (females) eBFP trajectories were at the tail-end or a late stage of pubertal development at the start of the FLEX trial, our results show that these individuals experienced more hypoglycemia despite potentially being more behaviorally mature and experiencing less hormonal fluctuation and insulin resistance, which runs counter to a plausible expectation of less hypoglycemia. Future studies that explore relationships between psychosocial factors, self-management behaviors, hypoglycemia, and body composition at multiple time points during adolescence will contribute insights into how adolescents can be supported to avoid hypoglycemia and maintain a healthy weight throughout puberty—a stage characterized by frequent changes in physiology, attitudes, and behavior.
There were 47 participants in the FLEX trial missing from the present analysis due to incomplete anthropometry or CGM data. As discussed previously, those missing from the analysis had lower eBFP (or where eBFP could not be calculated, lower BMI) than those included in the analysis. Given what is known about the baseline estimated adiposity of those included in the present analysis (i.e., that those with lower baseline eBFP or BMI were more likely to follow an increasing body fat trajectory), it is possible that those excluded from the analysis would have been in the increasing (females) or stable/increasing (males) trajectory groups since they also had lower eBFP and BMI at baseline. If those excluded individuals had more hypoglycemia than those included in our sample, the inclusion of these missing individuals could have shifted our results so that we did not observe more hypoglycemia to be associated with a decreasing or stable/decreasing eBFP trajectory. However, as previously discussed, because the excluded individuals did not statistically significantly differ from the included individuals by other key characteristics that could influence time in hypoglycemia or weight status (i.e., age, sex, race/ethnicity, health insurance status, parental education, diabetes duration, baseline HbA1c, nor any psychosocial measures), it is unlikely that including these missing participants would have substantially changed the main takeaways of our analysis.2,9,10,12
Other limitations of our analysis include that the FLEX trial was not designed to test the hypothesis we explored in the present analysis, which limits the strength of inferences that can be made from the observed associations. Using randomized control trial data for observational analysis can introduce bias through trial effects on the variables under study. However, we expect these effects to be nominal in the present analysis: the FLEX trial did not demonstrate differences between intervention and control groups with respect to the primary outcome (HbA1c) at 18 months, and we adjusted for intervention group membership in our models.45 Additionally, the blinded 7-day CGM wear time at baseline of the FLEX trial may not be representative of participants’ usual experiences with hypoglycemia over 18 months. Key strengths of the study include the availability of longitudinal anthropometric data, an objective measure of hypoglycemia, use of hypoglycemia cut-points put forth by clinical consensus guidelines to facilitate comparisons with future studies, and improvement upon the limitations of BMI to more accurately estimate adiposity and change in adiposity using validated equations. Data from the FLEX trial provided a unique opportunity to progress current understandings of the relationship between hypoglycemia and weight gain in youth with type 1 diabetes and HbA1c ≥8.0%.
Conclusions
In a sample of adolescents with type 1 diabetes HbA1c ≥8.0%, we found that increased time spent in hypoglycemia was not associated with increasing estimated adiposity over 18 months, but rather with decreasing or stable estimated adiposity over time. The magnitude of this association observed in males posits that ongoing monitoring of body fat percentage throughout puberty, particularly in males, may have clinical utility to calculate insulin needs, which may help reduce insulin dosing errors and subsequently hypoglycemia. Our findings further epidemiological evidence that hypoglycemia may not be a major driver of weight gain in US youth with type 1 diabetes and HbA1c ≥8.0%, and highlights the need for studies to prospectively test this hypothesis that is rooted in clinical perception. Additional studies that examine the interplay of hypoglycemia, weight, psychosocial, behavioral, and clinical factors among youth sub-groups are needed to further clarify for whom hypoglycemia may be a driver of weight gain and help focus future etiological and intervention studies.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Lind, M. et al. Glycemic control and excess mortality in type 1 diabetes. N. Engl. J. Med. 371, 1972–1982 (2014).
Corbin, K. D. et al. Obesity in type 1 diabetes: pathophysiology, clinical impact, and mechanisms. Endocr. Rev. 39, 629–663 (2018).
Polsky, S. & Ellis, S. L. Obesity, insulin resistance, and type 1 diabetes mellitus. Curr. Opin. Endocrinol. Diabetes Obes. 22, 277–282 (2015).
Purnell, J. Q., Zinman, B. & Brunzell, J. D. The effect of excess weight gain with intensive diabetes mellitus treatment on cardiovascular disease risk factors and atherosclerosis in type 1 diabetes mellitus: results from the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study (Dcct/Edic) Study. Circulation 127, 180–187 (2013).
Miller, K. M. et al. Current state of type 1 diabetes treatment in the US: updated data from the T1d Exchange Clinic Registry. Diabetes Care 38, 971–978 (2015).
Liu, L. L. et al. Prevalence of overweight and obesity in youth with diabetes in USA: the search for diabetes in youth study. Pediatr. Diabetes 11, 4–11 (2010).
DuBose, S. N. et al. Obesity in youth with type 1 diabetes in Germany, Austria, and the United States. J. Pediatr. 167, 627–632.e624 (2015) .
Craigie, A. M., Lake, A. A., Kelly, S. A., Adamson, A. J. & Mathers, J. C. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas 70, 266–284 (2011).
Driscoll, K. A. et al. Biopsychosocial aspects of weight management in type 1 diabetes: a review and next steps. Curr. Diabetes Rep. 17, 58 (2017).
Minges, K. E. et al. Correlates of overweight and obesity in 5529 adolescents with type 1 diabetes: the T1d Exchange Clinic Registry. Diabetes Res. Clin. Pract. 126, 68–78 (2017).
Hu, F. Obesity Epidemiology (Oxford University Press, 2008).
Kahkoska, A. R. et al. Sociodemographic associations of longitudinal adiposity in youth with type 1 diabetes. Pediatr. Diabetes 19, 1429–1440 (2018).
Purnell, J. Q. et al. Effect of excessive weight gain with intensive therapy of type 1 diabetes on lipid levels and blood pressure: results from the DCCT. JAMA 280, 140–146 (1998).
Jacob, A., Salinas, K., Adams‐Huet, B. & Raskin, P. Potential causes of weight gain in type 1 diabetes mellitus. Diabetes Obes. Metab. 8, 404–411 (2006).
Russell‐Jones, D. & Khan, R. Insulin‐associated weight gain in diabetes–causes, effects and coping strategies. Diabetes Obes. Metab. 9, 799–812 (2007).
Mehta, S. N. et al. Emphasis on carbohydrates may negatively influence dietary patterns in youth with type 1 diabetes. Diabetes Care 32, 2174–2176 (2009).
Ibfelt, E. et al. Association between glycaemic outcome and BMI in Danish children with type 1 diabetes in 2000–2018: a nationwide population‐based study. Diabet. Med. 38, e14401 (2020).
Nansel, T., Lipsky, L. & Iannotti, R. Cross-sectional and longitudinal relationships of body mass index with glycemic control in children and adolescents with type 1 diabetes mellitus. Diabetes Res. Clin. Pract. 100, 126–132 (2013).
Pasco, J. A. et al. Body mass index and measures of body fat for defining obesity and underweight: a cross-sectional, population-based study. BMC Obes. 1, 1–7 (2014).
Siervogel, R. M. et al. Annual changes in total body fat and fat‐free mass in children from 8 to 18 years in relation to changes in body mass index: the Fels Longitudinal Study. Ann. N. Y. Acad. Sci. 904, 420–423 (2000).
Sørensen, K. & Juul, A. BMI percentile-for-age overestimates adiposity in early compared with late maturing pubertal children. Eur. J. Endocrinol. 173, 227–235 (2015).
Stevens, J., Ou, F.-S., Cai, J., Heymsfield, S. & Truesdale, K. Prediction of percent body fat measurements in americans 8 years and older. Int. J. Obes. 40, 587–594 (2016).
Kichler, J. C. et al. The Flexible Lifestyle Empowering Change (FLEX) intervention for self-management in adolescents with type 1 diabetes: trial design and baseline characteristics. Contemp. Clin. Trials 66, 64–73 (2018).
Patry-Parisien, J., Shields, M. & Bryan, S. Comparison of waist circumference using the World Health Organization and National Institutes of Health protocols. Health Rep. 23, 53–60 (2012).
Vanderwall, C., Clark, R. R., Eickhoff, J. & Carrel, A. L. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr. 17, 1–6 (2017).
Vanderwall, C., Eickhoff, J., Clark, R. R. & Carrel, A. L. BMI Z-score in obese children is a poor predictor of adiposity changes over time. BMC Pediatr. 18, 1–6 (2018).
Bridge, P. et al. Validation of longitudinal DXA changes in body composition from pre-to mid-adolescence using MRI as reference. J. Clin. Densitom. 14, 340–347 (2011).
Nagin, D. S. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol. Methods 4, 139 (1999).
Loomba-Albrecht, L. A. & Styne, D. M. Effect of puberty on body composition. Curr. Opin. Endocrinol. Diabetes Obes. 16, 10–15 (2009).
Nagin, D. Group-based Modeling of Development. 4159, 9780674041318 (Harvard University Press, Cambridge, Mass, 2005).
Nagin, D. S. & Odgers, C. L. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 6, 109–138 (2010).
Kahkoska, A. R. et al. Dysglycemia among youth with type 1 diabetes and suboptimal glycemic control in the Flexible Lifestyle Empowering Change trial. Pediatr. Diabetes 20, 180–188 (2019).
Abraham, M. B. et al. Ispad Clinical Practice Consensus Guidelines 2018: assessment and management of hypoglycemia in children and adolescents with diabetes. Pediatr. Diabetes 19, 178–192 (2018).
Bumbu, A. et al. Non‐severe hypoglycaemia is associated with weight gain in patients with type 1 diabetes: results from the Diabetes Control and Complication Trial. Diabetes Obes. Metab. 20, 1289–1292 (2018).
Williams, D. P. et al. Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am. J. Public Health 82, 358–363 (1992).
Going, S. B. et al. Percent body fat and chronic disease risk factors in US children and youth. Am. J. Preventive Med. 41, S77–S86 (2011).
Mueller, W. H., Harrist, R. B., Doyle, S. R. & Labarthe, D. R. Percentiles of body composition from bioelectrical impedance and body measurements in US adolescents 8–17 years old: Project Heartbeat! Am. J. Hum. Biol. 16, 135–150 (2004).
Neovius, M. G., Linné, Y. M., Barkeling, B. S. & Rossner, S. O. Sensitivity and specificity of classification systems for fatness in adolescents. Am. J. Clin. Nutr. 80, 597–603 (2004).
Sardinha, L. B., Going, S. B., Teixeira, P. J. & Lohman, T. G. Receiver operating characteristic analysis of body mass index, triceps skinfold thickness, and arm girth for obesity screening in children and adolescents. Am. J. Clin. Nutr. 70, 1090–1095 (1999).
Taylor, R., Falorni, A., Jones, I. & Goulding, A. Identifying adolescents with high percentage body fat: a comparison of bmi cutoffs using age and stage of pubertal development compared with bmi cutoffs using age alone. Eur. J. Clin. Nutr. 57, 764–769 (2003).
Willett, W. Nutritional Epidemiology, Vol. 40 (Oxford University Press, 2012).
Igudesman, D. et al. Dietary intake on days with and without hypoglycemia in youth with type 1 diabetes: the Flexible Lifestyle Empowering Change Trial. Pediatr. Diabetes 21, 1475–1484 (2020).
Hanna, K. M. & Guthrie, D. Adolescents’ behavioral autonomy related to diabetes management and adolescent activities/rules. Diabetes Educator. 29, 283–291 (2003).
Amiel, S. A., Sherwin, R. S., Simonson, D. C., Lauritano, A. A. & Tamborlane, W. V. Impaired insulin action in puberty. N. Engl. J. Med. 315, 215–219 (1986).
Mayer-Davis, E. J. et al. The Flexible Lifestyles Empowering Change (FLEX) intervention for adolescents with type 1 diabetes: randomized clinical trial results for effect on metabolic status, diabetes related behaviors, and quality of life. Lancet Child Adolesc. Health 2, 635 (2018).
Acknowledgements
The FLEX trial is indebted to the many youths and their families whose participation made this study possible.
Funding
This analysis used data from the Flexible Lifestyles Empowering Change (FLEX) trial, which was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (1UC4DK101132) and the Helmsley Charitable Trust.
Author information
Authors and Affiliations
Contributions
E.M.-D., D.M.M., J.C.K., M.S., A.R.K., and A.C.S. designed the analysis. A.C.S conducted the analysis and interpreted the data. A.C.S. drafted the initial manuscript. All authors reviewed analyses and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.R.K. received financial support for travel from Novo Nordisk A/S to present work unrelated to this analysis in 2019. For work unrelated to the present analysis, D.M.M. reports research support from the NIH, JDRF, NSF, and the Helmsley Charitable Trust, and his institution has had research support from Medtronic, Dexcom, Insulet, Bigfoot Biomedical, Tandem, and Roche. D.M.M. has consulted for Abbott, Aditxt, the Helmsley Charitable Trust, Sanofi, Novo Nordisk, Eli Lilly, Medtronic, Insulet, and Dompe. All other authors have nothing to disclose. For work unrelated to the present analysis, D.Z. reports fellowship funding from ISPAD-JDRF, grants from the Helmsley Charitable Trust, and Medtronic Diabetes, Ascensia Diabetes Care, and Insulet Canada speaker bureau participation. R.P. reports consulting fees from AstraZeneca; consulting fees from Glytec, LLC; grants from Hanmi Pharmaceutical Co.; grants and consulting fees from Janssen; consulting fees from Merck; grants from Metavention; consulting fees from Mundipharma; grants, speaker fees, and consulting fees from Novo Nordisk; consulting fees from Pfizer; grants from Poxel SA; grants and consulting fees from Sanofi; consulting fees from Scohia Pharma Inc.; consulting fees from Sun Pharmaceutical Industries; personal consulting fees from Sanofi US Services, Inc. Except for consulting fees in February 2018 and June 2018 from Sanofi US Services, Inc., R.P. services were paid for directly to AdventHealth, a nonprofit organization. All other authors report no financial ties to products used in the study or perceived/potential conflicts of interest.
Consent for publication
Written informed consent and assent were provided by parent and adolescent, respectively, at the first in-person baseline measurement visit of the Flexible Lifestyles Empowering Change (FLEX) trial.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sarteau, A.C., Kahkoska, A.R., Crandell, J. et al. More hypoglycemia not associated with increasing estimated adiposity in youth with type 1 diabetes. Pediatr Res 93, 708–714 (2023). https://doi.org/10.1038/s41390-022-02129-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02129-1