Abstract
Objectives
Patients with anorexia nervosa (AN) have autonomic nervous system (ANS) dysfunction as measured by heart rate variability (HRV). Omega-3 fatty acids may improve heart rate regulation. Our aim was to describe ANS response to a mid-day meal in adolescent females with AN in a 12-week treatment program, randomized to receive either omega-3 supplements or placebo.
Methods
This pilot study was a longitudinal, double-blind, randomized controlled trial. Each group was subdivided into an acutely ill cohort and a chronically ill cohort. Linear and non-linear measures of slope, mean, and pre/post-meal changes in HRV were measured at baseline, 6 weeks, and 12 weeks.
Results
Twenty-four women (n = 12 placebo; n = 12 omega-3) were enrolled. By program end, the acute omega-3 group alone showed no change in any pre-meal slope. Acute and chronic omega-3 groups, but not placebo groups, demonstrated physiologically expected post-meal heart rate increases at 12 weeks. For all measures at 6 and 12 weeks, the chronic placebo and omega-3 groups had smaller physiologic responses to the meal compared with the acute groups.
Conclusions
Participation in a 12-week partial hospitalization program may improve autonomic function in response to mealtime, with possible additional benefit from omega-3 PUFA, particularly in those with acute illness.
Impact
-
Autonomic function with meals improves with a 12-week partial hospitalization program in adolescent females with anorexia nervosa.
-
Omega-3 polyunsaturated fatty acids may improve autonomic function, especially in adolescent females with acute forms of anorexia nervosa.
-
Longer duration of illness in adolescent females with anorexia nervosa is associated with blunted autonomic response to meals.
Similar content being viewed by others
Introduction
Anorexia nervosa (AN) is a serious psychiatric illness characterized by intentional weight loss, restrictive eating, fear of gaining weight, and distorted body image, with or without binge eating and purging episodes.1 Eating disorders are most likely to develop during adolescence, and AN has a lifetime prevalence of 1.4% for women and 0.2% for men.2 The malnutrition associated with AN may be severe, and cardiovascular complications are common, including dysfunction of the autonomic nervous system (ANS) both at rest3,4 and in response to challenge.5,6 Altered ANS function may be either a consequence of malnutrition or a potential cause of disordered eating.7
The majority of literature reporting on ANS function in AN has shown predominance of parasympathetic activity over sympathetic activity in patients with AN compared with healthy controls.3,8,9 Some researchers have found similar autonomic function between AN and controls, but even in these studies, evidence of reduced sympathetic activity was found during postural changes10 and in at least one measure of autonomic function at rest.11 Importantly, at least some of these differences in findings may be due to failure to differentiate patients with AN by duration of illness. Individuals with chronic AN demonstrate significantly lower levels of parasympathetic activity and, thus, higher relative sympathetic activity, compared with individuals with acute AN.12,13
Eating a meal is known to increase heart rate (enhanced sympathetic activity) in healthy adults with a maximal effect 1.5–2 h post-meal.14,15,16,17 Similarly, high frequency heart rate variability (HRV) (an index of parasympathetic activity) decreases in healthy adults following a meal.14,18 Given the known anxiety experienced by individuals with AN in association with meals19 and the known dysfunctional ANS, autonomic effects of a meal in adolescents with AN needs examination.
Omega-3 polyunsaturated fatty acids (PUFA) have been shown to improve heart rate20 regulation and HRV in a number of different populations.21,22,23,24 Three primary mechanisms by which PUFAs may affect these autonomic markers have been proposed21: (1) modulation of autonomic function through increases in acetylcholine (ACh)25,26 or ACh receptors,25,27 (2) suppression of sympathetic activity through modulation of circulating catecholamine concentrations28,29 and pro-inflammatory cytokines,29,30,31,32 and (3) slowing heart rate through modulation of cardiac electrophysiology by reducing cardiac membrane electrical excitability via inhibition of the Na+ and Ca+ ion channels.33,34,35
Multiple studies have demonstrated that omega-3 PUFAs are reduced in individuals with AN compared with healthy controls,36 and that levels improve with treatment in adolescents with acute forms of AN.37 Administering PUFAs has been suggested as a treatment for AN.38 However, the few studies that have examined outcomes in AN patients treated with PUFAs have demonstrated mixed results including improved weight gain and enhanced mood39 and no differences in weight gain40,41 compared with control groups. The effect of omega-3 PUFAs on ANS function in AN has not been studied.
Although evidence for specific treatment approaches for AN is limited,42 the use of family-based therapy (FBT) has the best available evidence for children and adolescents and is frequently the initial treatment approach.43 While FBT was developed as an outpatient treatment for patients and families with more acute needs, FBT has also been shown to be effective in a partial-hospital setting.44 The aim of this longitudinal study was to describe and compare autonomic responses to a mid-day meal in adolescent females with acute and chronic AN who initiated treatment in a 12-week partial hospitalization treatment program and were randomized to receive either an omega-3 PUFA supplement or placebo.
Methods
This was a two arm, longitudinal, double-blind, randomized controlled pilot study design. The local institutional human subjects review board and the U.S. Food and Drug Administration (IND 117431) approved the protocol, and the study was conducted in accordance with the ethical standards from the 1964 Declaration of Helsinki. The trial was registered at clinicaltrials.gov (NCT01933243). All participants provided written assent or consent, depending on age, and a parent or legal guardian provided written informed consent for participation of minors.
Setting/Sample
A sample of 12–21-year-old adolescent females admitted to the eating disorders partial hospitalization FBT program at a large Midwestern children’s hospital for treatment of AN, restrictive subtype, was recruited shortly after admission. Patients meeting criteria could move from partial hospitalization program (PHP) to intensive outpatient treatment as their conditions improved. Sample size in this pilot study was determined based on the available time period and the budget of the pilot award. Potential participants were excluded if they had co-morbid medical or psychiatric conditions affecting appetite or weight, were currently taking omega-3 PUFA supplements, were unable to swallow a pill, or were unable to complete the 12-week study. Following enrollment, participants were assigned to group based on a block randomization scheme consisting of eight participants per block that was generated by the hospital’s investigational drug service pharmacy (IDS). Group assignment with an allocation ratio of 1:1 was made following consent when the study team contacted IDS for delivery of a coded container of PUFA or placebo according to the next sequential treatment group in the prepared random list. Study team and participants were both blinded to group allocation.
The intervention group received omega-3 PUFA supplements provided by Nordic Naturals® ProEPA™ Xtra (Watsonville, CA) at a dose of four capsules daily for 12 weeks. The four omega-3 PUFA capsules provided a total daily dose of 2,120 mg eicosapentaenoic acid (EPA), 600 mg DHA, and 404 mg of other omega-3 PUFA. Supplements contained lemon essential oil to mask potential fishy aftertaste. The control group received a placebo also provided by Nordic Naturals®. Placebo capsules were identical in color, size, and flavor but contained predominantly soybean oil (3960 mg total daily dose) and negligible omega-3 PUFA (40 mg total daily dose).
Measures
ANS function was measured using HRV based on electrocardiographic (ECG) recordings using Marquette Seer MC Holter Recorders (General Electric, Inc.). HRV refers to the miniscule differences in beat-to-beat intervals that are the result of a precise interaction between sympathetic and parasympathetic nervous system heart rate regulation.45 Linear and non-linear approaches to analysis were used. Linear measures were determined using frequency domain methods, which partition the variability in heart rate into underlying rhythms resulting from of a number of different physiologic processes, such as thermoregulation and baroreceptor activity.46 For this study, high-frequency HRV (hfHRV) was used as a marker for parasympathetic regulation of heart rate, which is the variability that occurs at the same frequency as respirations.45 ANS response to a stressor would be reflected by decreases in hfHRV, indicating withdrawal of parasympathetic stimulation. This withdrawal would generally be accompanied by increases in sympathetic activity. Heart rate (HR) was also recorded, providing a measure of overall arousal. Increases in HR are associated with more sympathetic activity.47 Recovery from a stressful event would be reflected in subsequent increases in hfHRV and reductions in HR. In general, relatively higher levels of baseline hfHRV, lower baseline HR, and greater magnitudes of change in response to internal or external stressors reflect healthy and responsive autonomic functioning.48
Non-linear measures of HRV add additional information about regulation of heart rate not attainable with linear measures. We measured short-term detrended fluctuation analysis (DFA1), which quantifies fractal properties of heart rate, providing information about level of organization, rather than magnitude, of changes in heart rate.49,50 In healthy adults, DFA1 decreases with challenging activities, suggesting more sympathetic activity.50,51 Non-linear measures have rarely been measured in adolescents with AN11,13 and may provide additional information about possible alterations in autonomic function.
Pre-meal was defined as 2 h immediately preceding the mid-day meal using average values of four consecutive 30-min epochs. Post-meal was defined as beginning 1 h after the meal started and continued for the subsequent 2 h using average values of four consecutive 30-min epochs. To gain a comprehensive analysis of HRV responses to the meal, four variables were used for each of the three primary HRV measures (hfHRV, DFA1, and HR): Pre-meal slopes, post-meal slopes, mean values of the four 30 min epochs pre- and post-meal, and magnitude of change in pre- and post-meal mean values, adjusting for baseline.
Procedure
Immediately following recruitment and informed consent and assent, a Holter recorder was attached to each participant. Participants recorded mealtimes for the following day in a diary supplied by the study. Participants returned to the clinic for removal of the recorder 48 h after monitor placement. This procedure was repeated at 6 weeks (mid-program) and 12 weeks (end of program). ECG data for HRV measures were calculated for pre- and post-mealtimes as described above for each data collection time.
Data analysis
To account for differences in ANS function between acute duration and chronic duration of illness, each treatment group was subdivided into an acute cohort and a chronic cohort with the following groups: acute placebo (AP), acute omega-3 (AO), chronic placebo (CP), and chronic omega-3 (CO).
Due to the small sample size, group-level analysis was not considered. Instead we opted for multiple single-subject analysis using interrupted time series, specifically regression discontinuity analysis.52 These single-subject models were then synthesized using a meta-analysis approach for assessing within- and between-group change.53 Like true-experimental studies, single-subject designs can be used to test whether a treatment is responsible for observed changes in performance. Research syntheses, using meta-analysis, focuses on integrating the single-subject empirical research in order to find generalizations in the data. Marginal means were then used to assess magnitude and direction of change between pre-meal and post-meal using regression analysis. Type 1 error rate was set at 0.10 for this pilot study in order to retain potential variables for future hypothesis-testing studies. Because of the small sample size, marginal effect sizes for magnitude of change, adjusted for baseline values, are reported rather than statistical significance.
Additional analyses were done to examine within-group comparisons over time in preparation for future, adequately powered studies. These analyses can be accessed in the Supplemental Table.
Results
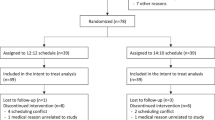
Recruitment and follow-up took place between January 2015 and February 2016. Out of 41 potential participants, 24 were enrolled, 2 did not meet criteria, and 15 declined participation. Characteristics of the sample and the CONSORT diagram have been reported elsewhere.41 The CONSORT diagram can be viewed in the Supplemental Figure. In summary, participants were on average 14.7 years of age, white, non-Hispanic with an average BMI of 19.2. Twelve participants were randomized to the placebo group, and 12 to the omega-3 group. Sixteen participants (placebo: n = 7; omega-3: n = 9) were classified as having acute illness of <12 months duration; eight (placebo: n = 5; omega-3: n = 3) were classified as having chronic illness of ≥12 months duration. Results for each of the HRV indices are presented by each HRV variable and data collection time point.
hfHRV: Baseline
Within-group slopes (see Table 1)
All groups (AP, AO, CP, and CO) had positive hfHRV slopes in the 2 h leading up to the meal. Following the meal, the AP and CO groups had flattened, stable slopes, whereas AO and CP groups demonstrated positive slopes (AO: t = 2.760, p = 0.017; CP: t = 7.859, p = 0.000).
Within- and between-cohort group comparisons of marginal means
(see Table 2) The AP group had lower mean hfHRV than the AO group at pre-meal baseline (t = 2.96, p = 0.003). There were no differences in baseline values within the chronic groups. However, the AP group had lower values than the CP group at baseline (t = 3.07, p = 0.002). Post-meal, the lower values for AP as compared with CP remained (t = 2.45, p = 0.015). There were no differences between the AO and CO groups.
hfHRV: 6 weeks
Within-group slopes (see Table 1)
Before the meal, both acute and chronic placebo groups had flattened, stable hfHRV slopes, whereas both acute and chronic omega-3 groups had positive slopes (AO: t = 4.989, p = 0.0003; CO: t = 6.546, p = 0.000). Following the meal, both acute and chronic placebo groups had positive slopes, whereas both acute and chronic omega-3 groups had flattened, stable slopes.
Within- and between-cohort group marginal means (see Table 2)
Only one significant difference was found within- or between-cohort groups at 6 weeks. The AP group had higher hfHRV than the AO group post-meal (t = −1.66, p = 0.098).
Within- and between-cohort group magnitude of change of marginal means (see Table 3 and Fig. 1)
The placebo and omega-3 groups did not differ in magnitude of change of hfHRV after the meal within either acute or chronic cohort groups. However, the magnitude of change was lower in the chronic cohort groups compared with the acute cohort groups with large effect sizes of 0.695 (placebo) and 0.721 (omega-3) (see Fig. 1).
hfHRV: 12 weeks
Within group slopes (see Table 1)
Before the meal, both acute and chronic placebo groups had positive slopes (AP: t = 3.925, p = 0.002; CP: t = 5.450, p = 0.0001) whereas both acute and chronic omega-3 groups had flattened, stable slopes. Following the meal, the AP group had increasing values (t = 16.461, p = 0.000). However, the remaining groups demonstrated steady values.
Within- and between-cohort group marginal means (see Table 2)
hfHRV did not differ by treatment condition or duration of illness (acute/chronic) at 12 weeks.
Within- and between-cohort group magnitude of change of marginal means (see Table 3 and Fig. 1)
The placebo and omega-3 groups did not differ in magnitude of change of hfHRV after the meal in either acute or chronic cohorts. However, the magnitude of change was lower in the chronic cohort compared with the acute cohort with large effect sizes of 0.866 (placebo) and 0.713 (omega-3).
DFA1: Baseline
Within-group slopes (see Table 1)
Before the meal, negative DFA1 slopes were seen in the AP (t = −10.01, p = 0.000), AO (t = −2.28, p = 0.042), and CO (t = −6.99, p = 0.000) groups. However, DFA1 was stable in the CP group (t = −1.31, p = 0.213). Following the meal, both acute and chronic placebo groups had flattened, stable slopes (AP: t = 1.577, p = 0.141; CP: t = 0.130, p = 0.900). However, both acute and chronic omega-3 groups had positive slopes (AO: t = 5.507, p = 0. 0001; CO: t = 8.366, p = 0.000).
Within- and between-cohort group marginal means (see Table 2)
Within the acute cohort, the placebo group had higher pre-meal DFA1 values than the omega-3 group (t = −2.70, p = 0.007). Within the chronic cohort, the placebo group had lower pre-meal and post-meal values than the omega-3 group (t = 1.90, p = 0.058). Similarly, between-cohort group analysis showed the AP group had higher pre-meal values than the CP group (t = −2.21, p = 0.028), yet the AO group had lower pre-meal values than the CO group (t = 2.11, p = 0.035). Post-meal, the only differences found were lower DFA1 values in the CP group compared with the CO group (t = 1.97, p = 0.050).
DFA1: 6 weeks
Within-group slopes (see Table 1)
Before the meal, the acute and chronic placebo groups exhibited negative slopes (AP: t = −2.964, p = 0.012; CP: t = −1.745, p = 0.107). However, both acute and chronic omega-3 groups exhibited flattened, stable slopes. Following the meal, the AP group showed steady values, whereas the remaining three groups showed positive slopes (AO: t = 12.939, p = 0.000; CP: t = 5.111, p = 0.0003; CO: t = 3.144, p = 0.009).
Within- and between-cohort group marginal means (see Table 2)
Pre-meal DFA1 did not differ by treatment condition or duration of illness (acute/chronic). Post-meal, the AP group had lower values than the AO group (t = 2.41, p = 0.017). The AO group levels were also higher than the CO group (t = −1.88, p = 0.061).
Within- and between-cohort group magnitude of change of marginal means (see Table 3 and Fig. 1)
The placebo and omega-3 groups did not differ in magnitude of change of DFA1 after the meal in either acute or chronic condition cohorts. However, the magnitude of change was lower in the chronic condition cohort with large effect sizes of −1.607 (placebo) and −1.673 (omega-3).
DFA1: 12 weeks
Within-group slopes (see Table 1)
Before the meal, the AP, AO, and CP groups showed flattened, stable slopes whereas the CO showed negative slopes (t = −3.172, p = 0.008). Following the meal, the AP, AO, and CO groups showed flattened, stable slopes (AP: t = −0.656, p = 0.524; AO: t = 0.637, p = 0.536; CO: t – 1.349, p = 0.202)) whereas the CP group had decreasing values (t = −2.204, p = 0.048).
Within- and between-cohort group marginal means (see Table 2)
The only difference in means between groups at 12 weeks was that the AP group had significantly lower values of DFA1 than the CP group (t = 2.17, p = 0.031).
Within- and between-cohort group magnitude of change of marginal means (see Table 3 and Fig. 1)
The placebo and omega-3 groups did not differ in magnitude of change of DFA1 after the meal in either acute or chronic condition cohorts. However, the magnitude of change was lower in the chronic cohort with large effect sizes of −1.963 (placebo) and −1.602 (omega-3).
Heart rate: Baseline
Within group slopes (see Table 1)
Before the meal, all groups showed negative slopes (AP: t = −19.34, p = 0.000; AO: t = −1.88, p = 0.085; CP: t = −38.19, p = 0.000; CO: t = −6.17, p = 0.000). Following the meal, heart rate for the AP and CO groups was steady (AP: t = −0.951, p = 0.360; CO: t = 1.082, p = 0.301), whereas heart rate decreased for AO (t = −3.179, p = 0.008) and CP (t = −13.623. p = 0.000).
Within- and between-cohort group marginal means (see Table 2)
Pre-meal, the AP group had higher heart rates than the AO group (t = −3.64, p = 0.000). However, the chronic groups did not differ by treatment condition. Both the acute placebo and omega-3 groups had higher heart rates than the chronic placebo and omega-3 groups (placebo: t = −3.75, p = 0.000; omega-3: t = −2.18, p = 0.030). Post-meal, the AP group had higher heart rates than the AO group (t = −2.64, p = 0.009) whereas the chronic groups did not differ. The AP group had higher heart rates than the CP group (t = −3.93, p = 0.000), but the acute and chronic omega-3 groups did not differ.
Heart rate: 6 weeks
Within-group slopes (see Table 1)
Before the meal, AP, AO, and CP groups demonstrated flattened, stable slopes, whereas the CO group showed negative slopes (t = −3.632, p = 0.003). Following the meal, heart rate values increased in the AP, AO, and CP groups (AP: t = 13.044, p = 0.000, AO: t = 4.725, p = 0.0005; CP: t = 13.650, p = 0.000) and was steady in the CO group (t = 1.116, p = 0.286).
Within- and between-cohort group marginal means (see Table 2)
At 6 weeks, the AP had higher pre-meal heart rates than the AO group (t = −1.65, p = 0.099). Post-meal, both the acute placebo and acute omega-3 groups had higher heart rates compared with the chronic placebo and chronic omega-3 groups (placebo: t = −2.83, p = 0.005; omega-3: t = −1.67, p = 0.096).
Within- and between-cohort group magnitude of change of marginal means (see Table 3 and Fig. 1)
The AP group had a higher magnitude of HR change post-meal than the AO group, but the effect size was small (−0.307). The CP and CO groups changed in different directions (CP decreasing and CO increasing), and this difference exhibited a moderate effect size (−0.349). Similar to the other HRV measures of change, the magnitude of change was lower in the chronic cohort compared with the acute cohort with large effect sizes of −0.925 (placebo) and −0.967 (omega-3).
Heart rate: 12 weeks
Within-group slopes (see Table 1)
Before the meal, negative heart rate slopes were observed in the AP group (t = −3.084, p = 0.010) whereas flattened, stable heart rates were observed in the remaining three groups (AO, CP, CO). Following the meal, both acute and chronic placebo groups had negative slopes (AP: t = −3.676, p = 0.003; CP: t = −2.336, p = 0.038) whereas both acute and chronic omega-3 groups had positive slopes (AO: t = 2.471, p = 0.029; CO: t = 2.371, p = 0.035).
Within- and between-cohort group marginal means (see Table 2)
At 12 weeks, differences by duration of illness were similar to those at 6 weeks wherein both the placebo and omega-3 groups in the acute cohort had higher heart rates compared with the placebo and omega-3 groups in the chronic cohort (placebo: t = −3.18, p = 0.002; omega-3: t = −2.37, p = 0.018).
Within- and between-group magnitude of change of marginal means (see Table 3 and Fig. 1)
The AP group had a higher magnitude of HR change post-meal than the AO group, but the effect size was small (−0.330). The CP and CO groups again changed in different directions (CP decreasing and CO increasing) and this difference exhibited a moderate effect size (ES = −0.380). Similar to the other HRV measures of change, the magnitude of change was lower in the chronic cohort compared with the acute cohort with large effect sizes of −1.192 (placebo) and −0.961 (omega-3).
Discussion
In this pilot study examining ANS function in adolescent females with AN who were admitted to a FBT PHP, participants were randomly assigned to receive either omega-3 PUFA or placebo for the duration of the 12-week program. Results demonstrated differences between the placebo and omega-3 groups as well as between acute and chronic cohorts. Overall, our results suggest some improvements in autonomic functioning over the course of the 12-week program with possible evidence of effectiveness of omega-3 PUFA, primarily in the acute cohort.
Slopes for HRV and heart rate
At the pre-intervention baseline, we were surprised to observe pre-meal decreases in heart rate values in all groups, having anticipated increases in heart rate because of the sympathetic effects of pre-meal anxiety. Upon closer inspection, however, we observed a concomitant increase in vagal activity (hfHRV) and a decrease in the non-linear HRV measure, DFA1. This pattern of increased vagal activity, decreased heart rate, and decreased DFA1 is known to occur in laboratory settings in which both the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS) are activated simultaneously (co-activation) and is associated with instability of heart rate.54,55 Vagal activation reduces heart rate and, when present in the face of norepinephrine, dominates the effect to produce lower heart rates.55,56 We propose that this simultaneous activation of the PNS and SNS is evidence of acute distress in this population. Indeed, co-activation may be a conditioned response to aversive stimuli,57 that is, mealtime for the adolescents in this study. In other words, presented with a challenge, co-activation of the ANS may be more likely in this population.
This interplay of these three measures of slope before the meal did not occur again in any of the groups after the start of treatment, although significant reductions in slope of heart rate continued for the chronic omega-3 cohort. This suggests that the significant emotional challenge of mealtime may have been reduced with the PHP in all but the chronic omega-3 group. Co-activation may have continued to be an issue for the chronic omega-3 group with evidence at 12 weeks of reductions in DFA1 and heart rate. Additional research with larger samples will help clarify this issue.
Slopes for hfHRV and DFA1 at 6 and 12 weeks were similar within treatment groups, i.e., both the acute and chronic placebo groups had flattened, stable slopes at 6 weeks and increased slopes at 12 weeks, whereas both the acute and chronic omega-3 groups had increased slopes at 6 weeks and flattened stable slopes at 12 weeks. Importantly, by program end at 12 weeks, the acute omega-3 group showed no change in any slope index in the 2 h preceding the meal, suggesting baseline pre-meal stress/anxiety had been diminished. In contrast, the acute placebo group and both chronic placebo and chronic omega-3 groups continued to demonstrate changes in hfHRV and HR. After the meal, our primary finding was that both the acute and chronic omega-3 groups demonstrated post-meal heart rate increases at 12 weeks, which was not observed in either the acute or chronic placebo groups. Increases in heart rate are expected following meals because of parasympathetic withdrawal with resultant increased sympathetic activity needed to facilitate blood flow to gastrointestinal organs during the digestive process.18,58
In summary, by the end of the treatment program, we observed an expected lack of pre-meal anticipatory autonomic response in the omega-3 group, but only in the acute cohort. We similarly observed expected post-meal autonomic responses of increases in heart rate in both the acute and chronic omega-3 groups and not the acute or chronic placebo groups. It is possible that the omega-3 PUFA contributed to normalizing of autonomic response to meals. We speculate that omega-3 PUFA may have influenced autonomic responses to meals differently in the participants who were acutely versus chronically ill with AN, and that these responses may have been differentially elicited due to the type of stimulus, i.e., emotional pre-meal anticipatory anxiety versus post-meal physiologic digestive processes. These findings support the need for additional research to more thoroughly evaluate the effects of omega-3 PUFA on autonomic function in this population.
Mean values
At baseline, we found differences between the acute placebo and acute omega-3 groups in pre- or post-meal mean values of all three HRV indices and differences between the chronic placebo and chronic omega-3 groups in pre-meal DFA1. We are unable to account for these baseline differences by age, hospitalization history, or medications, and suggest that small sample size may have been a factor. Unsurprisingly, the acute cohort differed at baseline from the chronic cohort in all three pre-meal indices for the placebo group and two of three indices for the omega-3 group, having lower mean hfHRV, lower or higher mean DFA1, and higher mean heart rates. Similarly, we noted differences in baseline post-meal responses, again with lower mean hfHRV and higher mean heart rates in the acute cohort.
At the program mid-point of 6 weeks, compared with the acute placebo group, the acute omega-3 group had lower mean pre-meal heart rates, suggesting less pre-meal arousal. In addition, the acute omega-3 group had lower post-meal mean hfHRV and higher post-meal mean DFA1, consistent with supportive physiologic response to eating. However, by the end of the PHP program, we found no differences in mean values between the acute placebo and acute omega-3 groups or between the chronic placebo and chronic omega-3 groups. It is possible that treatment with omega-3 PUFA improved autonomic function in the acute omega-3 group that either was not sustained or that was matched by the acute placebo group by 12 weeks as both were concurrently participating in the PHP program. More research is needed to further examine these relationships.
We did observe differences in mean values by acute/chronic condition. Most apparent were differences in mean heart rate post-meal at both 6 and 12 weeks. Both acute placebo and acute omega-3 groups had significantly higher heart rates compared with the chronic placebo and chronic omega-3 groups. These differences suggest a reduced ability in individuals with chronic AN to mount the physiologically expected autonomic response to eating14,15,16 and is consistent with the literature reporting reduced autonomic responsiveness in chronically ill AN patients.12,13
Magnitude of change
We examined magnitude of change in autonomic response between pre-meal and post-meal because magnitude of change is a marker for healthy flexibility and responsiveness of autonomic function.48 There were small differences (based on effect sizes) between placebo and omega-3 groups within the acute cohort and within the chronic cohort for hfHRV and DFA1 and more moderate differences for HR, suggesting small effects of omega-3 PUFA on magnitude of autonomic change, primarily exhibited in heart rate.
Our most interesting, but not surprising, finding was the differences in magnitude of change between the acute and chronic cohorts. For all measures at 6 and 12 weeks (controlling for baseline), the chronic cohort had smaller physiologic responses with large effect sizes. These findings are consistent with other research in which blunted autonomic responses have been demonstrated in individuals with chronic AN.12,13 These differences between acutely and chronically ill individuals with AN are important to consider when designing research in this population, as failing to analyze these groups separately may conceal real differences between groups.
Limitations
As this was an exploratory study to identify relationships for future randomized controlled trials, sample size was small, and firm conclusions cannot be drawn. Effect sizes were obtained that will support calculation of power for future studies. The placebo in this study was soybean oil, consisting largely of omega-6 fatty acids. Historically, omega-6 fatty acids (specifically, linoleic acid) have been thought to increase inflammation.59 However, a recent comprehensive review60 and a meta-analysis61 revealed no effect of soybean oil or increases in dietary intake of linoleic acid on markers of inflammation. We did not ask the participants to keep a detailed diary of activities during the time ECG recordings were obtained that could have affected ANS responses. However, these differences were likely distributed relatively equally between groups. Finally, due to budgetary constraints, we did not collect plasma levels of omega-3 fatty acids, and it is possible that some participants did not take the supplements as directed. In future studies, measurement of omega-3 fatty acids should be considered to strengthen evidence of these relationships.
Conclusion
In this exploratory study, we found evidence that participation in a 12-week PHP may improve autonomic function in response to mealtime in acute and chronically ill adolescent girls with AN. In addition, this study provides preliminary evidence that omega-3 PUFAs may add additional benefit through reducing anticipatory pre-meal autonomic responses and enhancing post-meal physiologic responses, particularly in those with shorter duration of illness. Further, we identified distinct differences between girls with acute illness and girls with chronic illness in terms of autonomic response to meals. Since dysfunctional autonomic responses have been associated with significant morbidity and mortality in individuals with AN, additional research in this area is critically important.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Association, A. P. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Galmiche, M., Déchelotte, P., Lambert, G. & Tavolacci, M. P. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am. J. Clin. Nutr. 109, 1402–1413 (2019).
Kollai, M., Bonyhay, I., Jokkel, G. & Szonyi, L. Cardiac vagal hyperactivity in adolescent anorexia nervosa. Eur. Heart J. 15, 1113–1118 (1994).
Sachs, K. V., Harnke, B., Mehler, P. S. & Krantz, M. J. Cardiovascular complications of anorexia nervosa: a systematic review. Int J. Eat. Disord. 49, 238–248 (2016).
Billeci, L. et al. Autonomic nervous system response during light physical activity in adolescents with anorexia nervosa measured by wearable devices. Sensors 19, 2820 (2019).
Monteleone, P. et al. Asymmetry of salivary cortisol and alpha-amylase responses to psychosocial stress in anorexia nervosa but not in bulimia nervosa. Psychol. Med. 41, 1963–1969 (2011).
Kaye, W. Neurobiology of anorexia and bulimia nervosa. Physiol. Behav. 94, 121–135 (2008).
Bär, K. J. et al. Changes of pain perception, autonomic function, and endocrine parameters during treatment of anorectic adolescents. J. Am. Acad. Child Adolesc. Psychiatry 45, 1068–1076 (2006).
Mazurak, N., Enck, P., Muth, E., Teufel, M. & Zipfel, S. Heart rate variability as a measure of cardiac autonomic function in anorexia nervosa: a review of the literature. Eur. Eat. Disord. Rev. 19, 87–99 (2011).
Murialdo, G. et al. Alterations in the autonomic control of heart rate variability in patients with anorexia or bulimia nervosa: correlations between sympathovagal activity, clinical features, and leptin levels. J. Endocrinol. Invest. 30, 356–362 (2007).
Vigo, D. E. et al. Nonlinear analysis of heart rate variability in patients with eating disorders. World J. Biol. Psychiatry 9, 183–189 (2008).
Nakai, Y., Fujita, M., Nin, K., Noma, S. & Teramukai, S. Relationship between duration of illness and cardiac autonomic nervous activity in anorexia nervosa. Biopsychosoc. Med. 9, 12 (2015).
Platisa, M. M., Nestorovic, Z., Damjanovic, S. & Gal, V. Linear and non-linear heart rate variability measures in chronic and acute phase of anorexia nervosa. Clin. Physiol. Funct. Imaging 26, 54–60 (2006).
Sauder, K. A., Johnston, E. R., Skulas-Ray, A. C., Campbell, T. S. & West, S. G. Effect of meal content on heart rate variability and cardiovascular reactivity to mental stress. Psychophysiology 49, 470–477 (2012).
Scott, E. M. et al. Carbohydrate ingestion, with transient endogenous insulinaemia, produces both sympathetic activation and vasodilatation in normal humans. Clin. Sci. 102, 523–529 (2002).
Täubel, J., Fernandes, S. & Ferber, G. Stability of the effect of a standardized meal on QTc. Ann Noninvasive Electrocardiol. 22, e12371 (2017).
Taubel, J., Wong, A. H., Naseem, A., Ferber, G. & Camm, A. J. Shortening of the Qt interval after food can be used to demonstrate assay sensitivity in thorough Qt studies. J. Clin. Pharmacol. 52, 1558–1565 (2012).
Lu, C. L., Zou, X., Orr, W. C. & Chen, J. D. Postprandial changes of sympathovagal balance measured by heart rate variability. Dig. Dis. Sci. 44, 857–861 (1999).
Smith, K. N., Van Huysse, J. L. & Rienecke, R. D. Changes in meal-related anxiety predict treatment outcomes in an intensive family-based treatment program for adolescents with anorexia nervosa. Eat. Disord. 29, 483–496 (2021).
Aung, T. et al. Associations of omega-3 fatty acid supplement use with cardiovascular disease risks: meta-analysis of 10 trials involving 77 917 individuals. JAMA Cardiol. 3, 225–234 (2018).
Drewery, M. L., Spedale, S. B. & Lammi-Keefe, C. J. Modulation of heart rate and heart rate variability by N-3 long chain polyunsaturated fatty acids: speculation on mechanism(S). Med Hypotheses 107, 29–34 (2017).
Colombo, J. et al. Long-chain polyunsaturated fatty acid supplementation in infancy reduces heart rate and positively affects distribution of attention. Pediatr. Res. 70, 406–410 (2011).
Mozaffarian, D. et al. Effect of fish oil on heart rate in humans: a meta-analysis of randomized controlled trials. Circulation 112, 1945–1952 (2005).
Macartney, M. J., Ghodsian, M. M., Noel-Gough, B., McLennan, P. L. & Peoples, G. E. DHA-rich fish oil increases the Omega-3 Index in healthy adults and slows resting heart rate without altering cardiac autonomic reflex modulation. J. Am. Coll. Nutr. 1–9 https://doi.org/10.1080/07315724.2021.1953417 (2021).
Nishizaki, T., Ikeuchi, Y., Matsuoka, T. & Sumikawa, K. Short-term depression and long-term enhancement of ACh-gated channel currents induced by linoleic and linolenic acid. Brain Res. 751, 253–258 (1997).
Aïd, S., Vancassel, S., Linard, A., Lavialle, M. & Guesnet, P. Dietary docosahexaenoic acid [22: 6(N-3)] as a phospholipid or a triglyceride enhances the potassium chloride-evoked release of acetylcholine in rat hippocampus. J. Nutr. 135, 1008–1013 (2005).
Kang, J. X., Xiao, Y. F. & Leaf, A. Free, long-chain, polyunsaturated fatty acids reduce membrane electrical excitability in neonatal rat cardiac myocytes. Proc. Natl Acad. Sci. USA 92, 3997–4001 (1995).
Hamazaki, K. et al. Effect of Omega-3 fatty acid-containing phospholipids on blood catecholamine concentrations in healthy volunteers: a randomized, placebo-controlled, double-blind trial. Nutrition 21, 705–710 (2005).
Bexton, R. S., Vallin, H. O. & Camm, A. J. Diurnal variation of the Qt interval–influence of the autonomic nervous system. Br. Heart J. 55, 253–258 (1986).
Das, U. N. Beneficial effect(S) of N-3 fatty acids in cardiovascular diseases: but, why and how? Prostaglandins Leukot. Essent. Fatty Acids 63, 351–362 (2000).
Pluess, T. T. et al. Intravenous fish oil blunts the physiological response to endotoxin in healthy subjects. Intensive Care Med. 33, 789–797 (2007).
Meydani, S. N. et al. Oral (N-3) fatty acid supplementation suppresses cytokine production and lymphocyte proliferation: comparison between young and older women. J. Nutr. 121, 547–555 (1991).
Leaf, A. The electrophysiologic basis for the antiarrhythmic and anticonvulsant effects of N-3 polyunsaturated fatty acids: heart and brain. Lipids 36(Suppl), S107–S110 (2001).
Xiao, Y. F., Kang, J. X., Morgan, J. P. & Leaf, A. Blocking effects of polyunsaturated fatty acids on Na+ channels of neonatal rat ventricular myocytes. Proc. Natl Acad. Sci. USA 92, 11000–11004 (1995).
Kang, J. X. Reduction of heart rate by Omega-3 fatty acids and the potential underlying mechanisms. Front. Physiol. 3, 416 (2012).
Caspar-Bauguil, S. et al. Anorexia nervosa patients display a deficit in membrane long chain poly-unsaturated fatty acids. Clin. Nutr. 31, 386–390 (2012).
Swenne, I. & Rosling, A. Omega-3 essential fatty acid status is improved during nutritional rehabilitation of adolescent girls with eating disorders and weight loss. Acta Paediatr. 101, 858–861 (2012).
Shih, P. B., Morisseau, C., Le, T., Woodside, B. & German, J. B. Personalized polyunsaturated fatty acids as a potential adjunctive treatment for anorexia nervosa. Prostaglandins Other Lipid Mediat. 133, 11–19 (2017).
Ayton, A. K., Azaz, A. & Horrobin, D. F. A pilot open case series of ethyl-epa supplementation in the treatment of anorexia nervosa. Prostaglandins Leukot. Essent. Fatty Acids 71, 205–209 (2004).
Mauler, B. et al. Hypercaloric diets differing in fat composition have similar effects on serum leptin and weight gain in female subjects with anorexia nervosa. Nutr. Res. 29, 1–7 (2009).
Manos, B. E. et al. A pilot randomized controlled trial of Omega-3 fatty acid supplementation for the treatment of anxiety in adolescents with anorexia nervosa. Int. J. Eat. Disord. 51, 1367–1372 (2018).
Fisher, C. A., Skocic, S., Rutherford, K. A. & Hetrick, S. E. Family therapy approaches for anorexia nervosa. Cochrane Database Syst. Rev. 5, Cd004780 (2019).
Lock J., L. G. D. Treatment Manual for Anorexia Nervosa: A Family-Based Approach 2nd edn (Guilford Press, 2012).
Hoste, R. R. Incorporating family-based therapy principles into a partial hospitalization programme for adolescents with anorexia nervosa: challenges and considerations. J. Fam. Ther. 37, 41–60 (2015).
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiologic interpretation, and clinical use. Eur. Heart J. 17, 354–381 (1996).
Berntson, G. G. et al. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology 34, 623–648 (1997).
Gordan, R., Gwathmey, J. K. & Xie, L. H. Autonomic and endocrine control of cardiovascular function. World J. Cardiol. 7, 204–214 (2015).
Porges, S. W. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation (W. W. Norton & Company, 2011).
Peng, C. K., Havlin, S., Stanley, H. E. & Goldberger, A. L. Quantification of scalingexponents and crossover phenomena in nonstationary heartbeat time series. Chaos 5, 82–87 (1995).
Willson, K., Francis, D. P., Wensel, R., Coats, A. J. & Parker, K. H. Relationship between detrended fluctuation analysis and spectral analysis of heart-rate variability. Physiol. Meas. 23, 385–401 (2002).
Hautala, A. J., Mäkikallio, T. H., Seppänen, T., Huikuri, H. V. & Tulppo, M. P. Short-term correlation properties of R-R interval dynamics at different exercise intensity levels. Clin. Physiol. Funct. Imaging 23, 215–223 (2003).
Kazdin, A. E. Single-Case Research Designs: Methods for Clinical and Applied Settings (Oxford University Press, 2011).
Beretvas, S. N. & Chung, H. A Review of meta-analyses of single-subject experimental designs: methodological issues and practice. Evid.-Based Commun. Assess. Intervention 2, 129–141 (2008).
Tulppo, M. P. et al. Effects of pharmacological adrenergic and vagal modulation on fractal heart rate dynamics. Clin. Physiol. 21, 515–523 (2001).
Tulppo, M. P., Makikallio, T. H., Seppanen, T., Airaksinen, J. K. E. & Huikuri, H. V. Heart rate dynamics during accentuated sympathovagal interaction. Am. J. Physiol. Heart Circulatory Physiol. 274, H810–H816 (1998).
Mourot, L. et al. Conditions of autonomic reciprocal interplay versus autonomic co-activation: effects on non-linear heart rate dynamics. Auton. Neurosci. 137, 27–36 (2007).
Berntson, G. G., Cacioppo, J. T. & Quigley, K. S. Autonomic determinism: the modes of autonomic control, the doctrine of autonomic space, and the laws of autonomic constraint. Psychol. Rev. 98, 459–487 (1991).
Ryan, S. M., Goldberger, A. L., Ruthazer, R., Mietus, J. & Lipsitz, L. A. Spectral analysis of heart rate dynamics in elderly persons with postprandial hypotension. Am. J. Cardiol. 69, 201–205 (1992).
DiNicolantonio, J. J. & O’Keefe, J. H. Importance of maintaining a low Omega-6/Omega-3 ratio for reducing inflammation. Open Heart 5, e000946 (2018).
Messino, M., Shearer, G. & Peteresen, K. Soybean oil lowers circulating cholesterol levels and coronary heart disease risk, and has no effect on markers of inflammation and oxidation. Nutrition 89, 111343 (2021).
Su, H., Liu, R., Chang, M., Huang, J. & Wang, X. Dietary linoleic acid intake and blood inflammatory markers: a systematic review and meta-analysis of randomized controlled trials. Food Funct. 8, 3091–3103 (2017).
Acknowledgements
We gratefully acknowledge the adolescents and their families who participated in this study.
Funding
Funding was provided by the Clinical and Translational Intramural Funding Program at the Research Institute at Nationwide Children’s Hospital, the Center for Integrative Health and Wellness at the Ohio State University, and The Ohio State University Center for Clinical and Translational Science, Grant no. UL1TR001070. Drug (active and placebo) was provided in kind by Nordic Naturals®.
Author information
Authors and Affiliations
Contributions
T.M.H.: substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; final approval of the version to be published. R.B.: substantial contributions to analysis and interpretation of data; drafting the article or revising it critically for important intellectual content, final approval of the version to be published. A.E.B.: substantial contributions to conception and design and acquisition of data; revising the article critically for important intellectual content; final approval of the version to be published. B.E.M.: substantial contributions to conception and design and acquisition of data; revising the article critically for important intellectual content; final approval of the version to be published. T.B.: substantial contributions to conception and design and acquisition of data; drafting the article or revising it critically for important intellectual content; final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
All participants provided written informed assent or consent, depending on age, and a parent or legal guardian provided written informed consent for participation of minors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Harrison, T.M., Brown, R., Bonny, A.E. et al. Omega-3 fatty acids and autonomic function in adolescents with anorexia: A randomized trial. Pediatr Res 92, 1042–1050 (2022). https://doi.org/10.1038/s41390-022-02058-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02058-z
This article is cited by
-
Imperative to accelerate research aligning real-time clinical demand with mental health supply
Pediatric Research (2022)