Abstract
Background
Brain injury is a serious and common complication of critical congenital heart disease (CHD). Impaired autonomic development (assessed by heart rate variability (HRV)) is associated with brain injury in other high-risk neonatal populations.
Objective
To determine whether impaired early neonatal HRV is associated with pre-operative brain injury in CHD.
Methods
In infants with critical CHD, we evaluated HRV during the first 24 h of cardiac ICU (CICU) admission using time-domain (RMS 1, RMS 2, and alpha 1) and frequency-domain metrics (LF, nLF, HF, nHF). Pre-operative brain magnetic resonance imaging (MRI) was scored for injury using an established system. Spearman’s correlation coefficient was used to determine the association between HRV and pre-operative brain injury.
Results
We enrolled 34 infants with median birth gestational age of 38.8 weeks (IQR 38.1–39.1). Median postnatal age at pre-operative brain MRI was 2 days (IQR 1–3 days). Thirteen infants had MRI evidence of brain injury. RMS 1 and RMS 2 were inversely correlated with pre-operative brain injury.
Conclusions
Time-domain metrics of autonomic function measured within the first 24 h of admission to the CICU are associated with pre-operative brain injury, and may perform better than frequency-domain metrics under non-stationary conditions such as critical illness.
Impact
-
Autonomic dysfunction, measured by heart rate variability (HRV), in early transition is associated with pre-operative brain injury in neonates with critical congenital heart disease.
-
These data extend our earlier findings by providing further evidence for (i) autonomic dysfunction in infants with CHD, and (ii) an association between autonomic dysfunction and brain injury in critically ill neonates.
-
These data support the notion that further investigation of HRV as a biomarker for brain injury risk is warranted in infants with critical CHD.
Similar content being viewed by others
Introduction
Congenital heart disease (CHD) is the most common form of congenital malformation, affecting 4–12/1000 live births.1,2 Neurologic disability is a common complication of CHD and its management, with the potential for lifelong debilitating consequences.3,4,5,6,7 The mechanisms underlying brain injury and neurologic morbidity in these infants are likely multifactorial and probably cumulative, starting in the fetal period and extending from birth to the intraoperative period and beyond.8,9,10,11
Neonates with CHD are particularly vulnerable to brain injury due to a unique combination of immature brain development and impaired cerebral perfusion and/or oxygenation. White matter injury (WMI), including periventricular leukomalacia, is commonly found both pre- and post-operatively.12,13 Metabolic and structural brain development are impaired in critical CHD, with term neonates displaying decreased N-acetylaspartate-to-choline ratios, increased lactate, delayed cerebral maturation, and decreased cerebral volumes compared with control term neonates.5,6,14 Microstructural and metabolic brain development appear to be strongly related to pre-operative brain injury in CHD,14 and may be related to differences in the cerebral circulation.15 Impaired brain perfusion and oxygenation are likely contributors to both impaired cerebral maturation and brain injury in CHD.16,17
Currently, brain imaging studies, with magnetic resonance imaging (MRI) as the gold standard, are used to detect brain injury in critically ill infants. However, clinical instability in such patients may preclude leaving the intensive care unit (ICU) for brain imaging studies. In addition, imaging studies may only detect brain injury after the threshold of reversibility has passed.
We have previously shown that autonomic function is associated with brain injury patterns in other high-risk neonates.18 The ANS plays a critical role in neurogenic control of the cardiopulmonary and cerebral circulation and is one system responsible for intrinsic neuroprotection. ANS dysfunction may lead to impairment of critical intrinsic neuroprotective reflexes (e.g., cerebral pressure autoregulation (CAR)), leaving the infant vulnerable to irreversible brain injury from insults such as hypoperfusion and hypoxemia that commonly occur in CHD.19,20,21,22,23 We have previously described significant autonomic dysfunction in newborns with hypoplastic left heart syndrome (HLHS) and transposition of the great arteries (TGA), two forms of critical CHD.24 Impaired ANS development may lead to an adverse neurologic outcome in several ways. Immature cardiorespiratory control may predispose to cerebral hypoxia-ischemia and brain injury. The brainstem ANS plays an important activity-based role in the development of higher cortical and subcortical centers; impaired maturation of the ANS might, therefore, lead to long-term neurodevelopmental and psycho-affective dysfunction in later life.25
Autonomic function may be measured using signals such as heart rate, blood pressure, and respiratory rate.26 Heart rate variability (HRV), which measures variation in beat-to-beat intervals between successive R-waves on electrocardiography (ECG) recordings, is the most widely used measure of autonomic function in neonates, given the non-invasive nature of the measurement (by ECG). We use HRV in this study as a metric of ANS function in neonates with CHD. HRV can be calculated using standard ICU continuous ECG monitoring and analyzed by both time- and frequency-domain approaches. Time-domain analysis (metrics include root mean square (RMS) 1, RMS 2, alpha 1, and alpha 2) determines both long-term (RMS 2, alpha 2) and short-term (RMS 1, alpha 1) HRV. Long-term HRV metrics (RMS 2, alpha 2) reflect both sympathetic and baroreceptor-mediated parasympathetic function, while short-term HRV metrics (RMS 1, alpha 1) reflect predominantly parasympathetic function. RMS metrics indicate the variability between R-R intervals on ECG, while alpha metrics indicate the autocorrection in the R-R intervals. Among frequency-domain metrics, low-frequency (LF, 0.05–0.25 Hz) HRV characterizes sympathetic and parasympathetic tone and changes related to baroreflex function,27,28 while high-frequency (HF, 0.3–1 Hz) HRV reflects the parasympathetic tone and is impacted by the respiratory rate.28 Frequency-domain approaches may be less reliable in non-stationary conditions.29 Lower metrics of HRV indicate immature or impaired autonomic function.
In this study, we sought to extend our earlier studies of HRV in critically ill infants including those with CHD.24,29,30 We tested the hypothesis that HRV over the first 24 h of cardiac ICU (CICU) admission would be associated with pre-operative brain injury (by MRI) in a cohort of infants with critical CHD. These data may help elucidate mechanisms of brain injury in infants with CHD as well as set the stage for the development of supplemental neuromonitoring strategies in infants who are too unstable to tolerate brain imaging.
Methods
Participants
All subjects in this single-center study were part of a prospective, observational MRI study in which pregnant women with a fetal diagnosis of critical CHD, i.e., infants expected to require cardiac surgery within the first 30 postnatal days31,32 of age, were recruited. Subjects underwent fetal MRI and postnatal, pre-operative brain MRI. The Institutional Review Board of Children’s National Hospital approved this study and written informed consent was obtained from each participant. Inclusion criteria were infants with critical CHD (i) admitted to the Children’s National Hospital Cardiac ICU (CICU) within 72 h of birth, (ii) with postnatal, pre-operative MRI studies, and (iii) archived ECG data for the first 24 h after CICU admission. Exclusion criteria included documented (i) genetic or chromosomal abnormalities, (ii) congenital infection, or (iii) multiple gestations.
Given that our population consisted of a heterogeneous group of infants with CHD, we categorized them as (i) two ventricle without aortic obstruction (2V–AO; n = 14), (ii) two ventricle with aortic obstruction (2V+AO; n = 1) (iii) single ventricle without aortic obstruction (SV–AO; n = 5), or (iv) single ventricle with aortic obstruction (SV+AO; n = 14). For the purposes of this study, we compared either SV (n = 19) vs. 2 V (n = 15) or AO (n = 15) vs. no AO (n = 19).
Continuous physiologic signals were retrospectively obtained from a large central archive. Relevant clinical data were abstracted from the medical record. A total of 34 infants had both postnatal, pre-operative brain MRI and continuous ECG data of sufficient quality to calculate time- and frequency-domain metrics of HRV.
Conventional MRI studies
MR imaging was performed preoperatively on a 3T magnet (General Electric, Milwaukee, WI). Sequences obtained included conventional T1- and T2-weighted imaging, diffusion-tensor imaging, and gradient-echo sequences, as well as MR spectroscopy of the basal ganglia. Our neuroradiologist (JM) reviewed postnatal, pre-operative brain MRI and scored MRIs according to the Magnetic Resonance Imaging Abnormality Scoring System used by Andropoulos et al.33 This scoring system categorizes brain MRI abnormalities as (i) WMI, (ii) infarction (INF), (iii) intraparenchymal hemorrhage (IPH), (iv) punctate lesions (PL), (v) lactate peak on MRS (lactate), (vi) intraventricular hemorrhage (IVH), (vii) subdural hemorrhage (SDH), or (viii) deep venous sinus thrombosis (DVST). Abnormalities in each category are given a score of 0–3 (0 = none, 1 = mild, 2 = moderate, 3 = severe) and weighted by a significance multiplier.33 For WMI, INF, and IPH the significance multiplier is 3, for PL and lactate the significance multiplier is 2, and for IVH, SDH, and DVST the significance multiplier is 1. Scores used in the analysis are derived from summated scores of all categories after the application of the significance multiplier.
Physiologic signal collection
We retrospectively retrieved ECG data from the Phillips Data Warehouse System (DWS) (IntelliVue MP-70, Philips, MA) or the RDE system (IntelliVue Information Center; Philips Healthcare). We retrieved ECG over the course of the first 24 h of admission to Children’s National CICU. The sampling rate of the ECG retrieved from DWS and the RDE was 250 and 125 Hz, respectively. We processed all data offline using computer programs developed in MATLAB 2018 (Mathworks, Inc, Natick, MA).
Heart rate variability analysis
We bandpass filtered the ECG signals between 0.5 and 60 Hz.34,35 After identifying R-waves, we calculated beat-to-beat interval (RRi).29,35,36 After partitioning RRi into 10-min end-to-end epochs, we calculated HRV metrics (LF, HF, nLF, nHF, alpha 1, alpha 2, RMS 1, RMS 2) for RRi in each epoch. We averaged every metric over the entire recording period and obtained one representative value for the metric per study.
To calculate frequency-domain metrics (LF, nLF, HF, nHF), we used the Welch periodogram approach with a frequency resolution of 0.016 Hz to estimate a power spectrum of RRi in every 10-min epoch. LF was calculated as the median of the logarithm of the power in 0.05–0.25 Hz, and HF was calculated as the median of the logarithm of the power in 0.3–1 Hz. Normalized low-frequency (nLF) and normalized high-frequency (nHF) were calculated as the ratio of the sum of the powers in low- and high-frequency bands to the total power. Total power was defined as the sum of the powers in the frequency band between 0.05 and 2 Hz.
We used detrended fluctuation analysis (DFA), a modified RMS analysis, to calculate the time-domain metrics.37,38 DFA involves five steps. First, the profile function, the mean value of the RRi is subtracted from the RRi series and the cumulative sum is calculated. Then, we partition the profile into end-to-end windows containing “s” number of beats and use a fourth-degree polynomial to fit the profile in each window. Next, we calculate the local fluctuation function as the RMS of the difference between the profile and best fits. Last, we use the median of the local fluctuation function from all the windows to calculate the fluctuation function. We repeat steps 1–3 for different window sizes.39 The window size is varied from six beats to one-fourth of the number of RRi samples in the 10-min epoch. We calculated the time-domain metrics RMS 1 (s) and RMS 2 (s) as the maximum value of the fluctuation function for “s” between 15 and 50 beats and 100 and 150 beats, respectively. Alpha 1 and alpha 2 were calculated as the slope of the fluctuation and “s” in a double logarithmic plot from 15 to 30 beats and 35 to 150 beats, respectively. Autocorrelation in the RRi is characterized by the alpha metrics.40 RMS (s) metrics characterize the variability in the RRi.40
Statistical analysis
We calculated Spearman’s rank correlation coefficient to determine the correlation between brain injury scores and HRV metrics. We used SAS (ver. 9.3, Cary, NC) to conduct all analyses with statistical significance considered for p < 0.05. Two-sided significance testing was used, with no adjustment for multiple comparisons. We present data as median (Q1–Q3) or frequency and percent. Group comparisons were made using either t-tests or Fisher’s exact test, where appropriate.
Results
Patient population
Thirty-four infants met the inclusion criteria. The clinical and demographic characteristics of our cohort are outlined in Table 1. There was no significant difference in demographic characteristics between groups no matter the CHD classification (Table 1). Overall, the median maternal age was 30.0 years (IQR 26.2–35.0), 19 (55.9%) infants were delivered via caesarean section, and median GA at birth was 38.9 weeks (IQR 38.1–39.1). As part of the original prospective study, a total of 33/34 infants underwent at least one fetal MRI prior to birth (Table 2). On the first fetal MRI, one fetus was found to have a single abnormal appearing sulcus. One fetus had pontine and vermian hypoplasia vs. dysplasia and was found to have Blake’s pouch cyst and small pontine measurements on the second fetal MRI. One fetus had mild ventriculomegaly on the second fetal MRI. There was no evidence of brain injury on fetal MRI in any fetus included in our cohort.
HRV and brain injury scores
As outlined in Table 3, our cohort had a median gestational age of 39.1 weeks at the time of the postnatal, pre-operative brain MRI. A total of 13 (38.2%) infants had brain injury on pre-operative MRI. Among infants with pre-operative brain injury, six (46.2%) had mild brain injury, five (38.5%) had moderate brain injury, and two (5.9%) had severe brain injury. A total of nine infants had WMI, one infant had IPH, two infants had PL, five infants had IVH, and four infants had SDH. Of the four infants with SDH, three had SDH including the interhemispheric fissure (subscore of 2) and one had a small supratentorial SDH. No infants in our cohort had cerebral INF, lactate peak on MRS, or DVST on pre-operative MRI. Among infants with SDH, three of four had hemorrhage or injury in at least one category in addition to SDH (one with SDH+IVH+WMI+IPH, one with SDH+IVH+PL, one with SDH+IVH). All five infants with IVH had at least one other category of injury (one with SDH+IVH+WMI+IPH, one with SDH+IVH+PL, one with SDH+IVH, two with IVH+WMI).
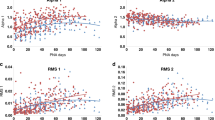
We found that time-domain metrics RMS 1 and RMS 2 significantly negatively correlated (p < 0.01) with total brain injury score. This inverse correlation seemed to be driven predominantly by scores for IVH and SDH, which were also significantly inversely correlated with RMS 1 and RMS 2 values of HRV (Table 4). While we did not find a significant correlation between total brain injury scores and other metrics of HRV, there was a significant negative correlation between time-domain metric Alpha 1 and brain injury subscores for PL and IVH. All significant correlations between total brain injury scores or subscores and HRV metrics occurred between time-domain metrics of HRV. No infants in our cohort had a cerebral INF, DVST, or lactate peak on MRS on pre-operative brain MRI. We found no correlation between frequency-domain metrics of HRV (LF, HF, nLF, and nHF) and pre-operative brain injury scores in our cohort.
Pregnancy conditions and illness severity
Pregnancy conditions and markers of illness severity prior to pre-operative MRI within our cohort are described in Table 5. No infant in our study had cardiac arrest or required ECMO prior to MRI. A total of 12 neonates underwent balloon atrial septostomy, 5 (24%) with no pre-op brain injury and 7 (54%) with brain injury. There was no significant difference in the rates of maternal or gestational diabetes, pregnancy-induced hypertension/pre-eclampsia, or chorioamnionitis between the brain-injured vs. non-brain-injured groups. We also found no significant difference between brain-injured vs. non-brain-injured groups with regard to lowest pH, highest pCO2, need for balloon atrial septostomy, or need for other cardiac intervention prior to MRI.
Discussion
In the current study of newborn infants with critical CHD, we show that lower autonomic tone, as measured by three time-domain metrics of HRV (RMS 1, RMS 2, and alpha 1), is associated with higher total brain injury scores on pre-operative brain MRI. The ANS controls the cardiovascular system via interaction between its sympathetic and parasympathetic branches that modulate heart rate and peripheral vascular resistance. ANS function is associated with cardiovascular, behavioral, and neurodevelopmental outcomes later in life.25,41,42,43,44,45,46 Impaired or immature sympathetic function is associated with brain injury in other populations, and this may be due to the effects of altered sympathetic-parasympathetic balance on CAR, cardiac output, and baroreflex function.47 A functional and appropriately mature autonomic nervous system is known to play a key role in neuroprotection, but there is much left to study regarding the interplay between these systems in the critically ill neonate and in CHD, specifically.
ANS development is prolonged, spanning the fetal period and continuing after birth.48,49 The sympathetic division of the ANS begins to develop early in gestation and continues to mature steadily throughout the fetal period. The myelinated vagus nerve develops during the third trimester and begins to exert parasympathetic influence,50,51 resulting in a steep increase in parasympathetic tone near term.24,43,52
In an earlier report, we showed that autonomic tone, as measured by HRV, is depressed in infants with HLHS or transposition of TGA in the early transitional, pre-operative period, suggesting that ANS development is delayed in the CHD population.24 Fetal HRV is lower in fetuses with HLHS than controls in the third trimester, and similar trends have been noted in fetuses with tetralogy of Fallot and transposition of TGA.53
Understanding the interplay between brain injury, brain maturity, and ANS function may help elucidate mechanisms of brain injury in CHD. Mechanisms underlying delayed ANS development in CHD remain poorly understood. CHD may result in chronic cerebral hypoxia, hypoperfusion, or both, beginning in the fetal period. There is considerable evidence to support delayed brain growth and development in infants with critical CHD,54,55,56 which may, in turn, result in delayed development of the ANS. We hypothesize, based upon this study and others, that chronic fetal cerebral hypoxia or hypoperfusion contributes to delayed structural brain maturation and delayed ANS maturation, leaving survivors of CHD more vulnerable to brain injury.
With regard to brain injury, it may be that intrinsic autoregulatory mechanisms controlled by the ANS play some role in cerebral blood flow and perfusion by participating in the regulation of vasoconstriction and vasodilation of the cerebral vessels in response to changes in blood pressure, oxygenation, and CO2 levels.47,57 Human and animal studies suggest that sympathetic inputs to the cerebral vasculature in fetuses and neonates may play a more important role in cerebrovascular tone in infants than in adults.58,59 In one study of infants with birth asphyxia, cerebral blood flow varied significantly with variations in blood pressure, suggesting that CAR is impaired in distressed infants.60 We hypothesize that this may be one mechanism by which ANS function and brain injury may be linked. Further studies will be needed to investigate this possibility.
Our findings suggest that impaired ANS function correlates with total pre-operative brain injury score in infants with critical CHD. We found no difference in rates of common prenatal conditions, including gestational diabetes, pregnancy-induced hypertension/pre-eclampsia, and chorioamnionitis between brain-injured vs. non-brain-injured neonates with CHD, but our cohort had relatively low rates of high-risk pregnancy conditions. Future studies with a larger cohort will be necessary to better evaluate the relationship between prenatal conditions, brain injury, and autonomic function in CHD. We also found no difference in markers of postnatal illness severity, such as lowest pH, highest pCO2, and need for cardiac interventions prior to surgery, between CHD neonates with pre-operative brain injury vs. those without. However, our population was relatively homogeneous with respect to illness severity markers, and no infant in our cohort experienced cardiac arrest or required ECMO prior to MRI. Relationships between illness severity, brain injury, and ANS function should be investigated in larger studies.
It is notable that we found no association between brain injury scores and frequency-domain metrics of HRV in the CHD population. We have reported this phenomenon previously in a study of premature infants.29 Our data suggest that time-domain metrics may more accurately reflect HRV under non-stationary conditions such as critical illness.
In this study, we used the brain injury scoring system developed by Andropoulos et al. that includes WMI, INF, IPH, PL, lactate on MRS, IVH, SDH, and DVST.33 This scoring system has been utilized previously in the CHD population by our group and others.61,62,63 While we did find a significant negative/inverse correlation between RMS 1 and RMS 2 and total brain injury score, we only found a trend toward significance between RMS 1 and RMS 2 and subscores for WMI, which is one of the most commonly noted types of brain injury in CHD. The lack of correlation with subscores for WMI may be related to the relatively low levels of injury in our cohort and the fact that the majority of injury we did see was relatively mild. This will need to be addressed in larger studies.
We found that RMS 1 and RMS 2 were inversely correlated with subscores for IVH and SDH. The Andropoulos scoring system includes points for SDH, although some authors have questioned the relevance for the long-term outcome of small SDH in neonates.64 Notably, small posterior fossa SDH are considered “normal” by the Andropoulos scoring system, in that they contribute zero points to the injury score. Only supratentorial SDH contribute to the injury score, and even then, they have a significance multiplier of 1, so they contribute far less to the total score than WMI or IPH, which have a significance multiplier of 3. Others have shown that infants with supratentorial SDH (the type of SDH in our cohort) have normal developmental outcomes at 24 months.64 In our cohort, three of four infants with SDH had at least one other type of brain injury subcategory as scored by the Andropoulos system, and 5/5 infants with IVH had a brain injury in at least one other subcategory. Our findings of an inverse correlation between HRV metrics and SDH and IVH may reflect the fact that SDH and IVH appear to be associated with other types of injury resulting in an overall higher burden of injury among infants with SDH and IVH, rather reflecting a correlation between HRV and isolated SDH or IVH. We cannot assess the clinical impact of SDH on our cohort with the available data, but this finding warrants further study.
While our study has many strengths, it is limited by its relatively small size. Within our cohort of 34 infants with critical CHD, only 13 had brain injury on pre-operative MRI, and only 2 of those had a severe brain injury. Our study was performed in a stand-alone children’s hospital in which all patients are outborn. While the majority of the participants in this study were transferred within the first 24 h of birth (and all were transferred within the first 72 h), we were not able to obtain HRV data immediately following birth. This study included neonates with a variety of CHD lesions that have different circulatory pathophysiologies. We consider the fact that our data show a significant inverse correlation between time-domain metrics of HRV (indicating impaired ANS function or delayed ANS maturation) and brain injury scores despite this heterogeneity to be a strength, but the more precise understanding of the interplay between autonomic function and brain injury in CHD may be gained by studying larger populations with similar heart defects and physiology. Our study was insufficiently powered to evaluate the influence of specific cardiac defects on brain injury due to the heterogeneity of cardiac defects in our population. Although we show a significant association between HRV metrics and brain injury, we are unable to determine the causal direction of this association, i.e., whether alterations in autonomic function measured by HRV preceded brain injury or whether brain injury influenced autonomic function (HRV), as previously described by us in otherwise healthy term infants with perinatal hypoxic-ischemic encephalopathy.65,66,67 While the subjects in our study had fetal brain MRI studies without brain injury in the third trimester, we are not able to able to exclude perinatal brain injury between the fetal MRI studies and the onset of our HRV recordings.
In the future, larger studies may determine the precise mechanisms and interplay between autonomic function, as measured by HRV, and brain injury in CHD. Future studies using serial HRV measures and brain MRI in fetuses and infants with critical CHD may help to clarify the temporal and causal relationships between autonomic function and brain injury in this vulnerable population. Future studies using real-time and simultaneous monitoring of cerebral oxygenation, blood pressure, and HRV in critically ill infants may better elucidate any connections between cerebral autoregulation, autonomic function, and brain injury in this vulnerable population. While much remains to be learned, understanding HRV and whether it may serve as a marker for brain injury or brain maturation may set the stage for the development of novel methods of neuromonitoring in the CICU using HRV. Such novel neuromonitoring techniques may prove clinically valuable given that many infants with critical CHD may be too unstable to risk transport from the ICU to the MRI scanner. For now, we show a significant negative correlation between early postnatal time-domain metrics of HRV and total pre-operative brain injury score in infants with critical CHD.
References
Grech, V. & Gatt, M. Syndromes and malformations associated with congenital heart disease in a population-based study. Int. J. Cardiol. 68, 151–156 (1999).
Tennstedt, C., Chaoui, R., Korner, H. & Dietel, M. Spectrum of congenital heart defects and extracardiac malformations associated with chromosomal abnormalities: results of a seven year necropsy study. Heart 82, 34–39 (1999).
Donofrio, M. T., Duplessis, A. J. & Limperopoulos, C. Impact of congenital heart disease on fetal brain development and injury. Curr. Opin. Pediatr. 23, 502–511 (2011).
Shillingford, A. J. et al. Aortic morphometry and microcephaly in hypoplastic left heart syndrome. Cardiol. Young. 17, 189–195 (2007).
Licht, D. J. et al. Brain maturation is delayed in infants with complex congenital heart defects. J. Thorac. Cardiovasc Surg. 137, 529–536 (2009). Discussion 536–527.
Miller, S. P. et al. Abnormal brain development in newborns with congenital heart disease. N. Engl. J. Med. 357, 1928–1938 (2007).
Sarajuuri, A. et al. Neurodevelopmental burden at age 5 years in patients with univentricular heart. Pediatrics 130, e1636–e1646 (2012).
Mulkey, S. B. et al. Multi-tiered analysis of brain injury in neonates with congenital heart disease. Pediatr. Cardiol. 34, 1772–1784 (2013).
Limperopoulos, C. et al. Neurodevelopmental status of newborns and infants with congenital heart defects before and after open heart surgery. J. Pediatr. 137, 638–645 (2000).
Limperopoulos, C. et al. Neurologic status of newborns with congenital heart defects before open heart surgery. Pediatrics 103, 402–408 (1999).
Donofrio, M. T. & Massaro, A. N. Impact of congenital heart disease on brain development and neurodevelopmental outcome. Int. J. Pediatr. 2010, 359390 (2010).
Mahle, W. T. et al. An MRI study of neurological injury before and after congenital heart surgery. Circulation 106, I109–I114 (2002).
Beca, J. et al. New white matter brain injury after infant heart surgery is associated with diagnostic group and the use of circulatory arrest. Circulation 127, 971–979 (2013).
Dimitropoulos, A. et al. Brain injury and development in newborns with critical congenital heart disease. Neurology 81, 241–248 (2013).
Ortinau, C. et al. Regional alterations in cerebral growth exist preoperatively in infants with congenital heart disease. J. Thorac. Cardiovasc. Surg. 143, 1264–1270 (2012).
Sethi, V. et al. Single-ventricle anatomy predicts delayed microstructural brain development. Pediatr. Res. 73, 661–667 (2013).
Petit, C. J. et al. Preoperative brain injury in transposition of the great arteries is associated with oxygenation and time to surgery, not balloon atrial septostomy. Circulation 119, 709–716 (2009).
Heart Rate Variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur. Heart J. 17, 354–381 (1996).
Al-Shargabi, T. et al. Changes in autonomic tone in premature infants developing necrotizing enterocolitis. Am. J. Perinatol. 35, 1079–1086 (2018).
Doheny, K. K. et al. Diminished vagal tone is a predictive biomarker of necrotizing enterocolitis-risk in preterm infants. Neurogastroenterol. Motil. 26, 832–840 (2014).
Vergales, B. D. et al. Depressed heart rate variability is associated with abnormal EEG, MRI, and death in neonates with hypoxic ischemic encephalopathy. Am. J. Perinatol. 31, 855–862 (2014).
Stone, M. L. et al. Abnormal heart rate characteristics before clinical diagnosis of necrotizing enterocolitis. J. Perinatol. 33, 847–850 (2013).
Fairchild, K. D. & Aschner, J. L. Hero monitoring to reduce mortality in NICU patients. Res. Rep. Neonatol. 2, 65–76 (2012).
Mulkey, S. B. et al. Heart rate variability is depressed in the early transitional period for newborns with complex congenital heart disease. Clin. Auton. Res. 30, 165–172 (2020).
Porges, S. W. & Furman, S. A. The early development of the autonomic nervous system provides a neural platform for social behavior: a polyvagal perspective. Infant Child Dev. 20, 106–118 (2011).
Schlatterer, S. D. & du Plessis, A. J. Exposures influencing the developing central autonomic nervous system. Birth Defects Res. 113, 845–863 (2021).
Malliani, A., Lombardi, F. & Pagani, M. Power spectrum analysis of heart rate variability: a tool to explore neural regulatory mechanisms. Br. Heart J. 71, 1–2 (1994).
Valenza, G., Citi, L., Saul, J. P. & Barbieri, R. Measures of sympathetic and parasympathetic autonomic outflow from heartbeat dynamics. J. Appl. Physiol. 125, 19–39 (2018).
Schlatterer, S. D. et al. Autonomic development in preterm infants is associated with morbidity of prematurity. Pediatr. Res. 2, 1–7 (2021). https://doi.org/10.1038/s41390-021-01420-x. Epub ahead of print.
Mulkey, S. B. et al. Autonomic nervous system maturation in the premature extrauterine milieu. Pediatr. Res. 89, 863–868 (2021).
Zun, Z. & Limperopoulos, C. Placental perfusion imaging using velocity-selective arterial spin labeling. Magn. Reson. Med. 80, 1036–1047 (2018).
De Asis-Cruz, J., Donofrio, M. T., Vezina, G. & Limperopoulos, C. Aberrant brain functional connectivity in newborns with congenital heart disease before cardiac surgery. Neuroimage. Clin. 17, 31–42 (2018).
Andropoulos, D. B. et al. Brain immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J. Thorac. Cardiovasc. Surg. 139, 543–556 (2010).
Ulusar, U. D. et al. Adaptive rule based fetal QRS complex detection using Hilbert transform. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2009, 4666–4669 (2009).
Kota, S. et al. Identification of QRS complex in non-stationary electrocardiogram of sick infants. Computers Biol. Med. 87, 211–216 (2017).
Ulusar, U. D. et al. Adaptive rule based fetal QRS complex detection using Hilbert transform. Conf. Proc. IEEE Eng. Med Biol. Soc. 1, 4666–4669 (2009).
Govindan, R. B. Detrended fluctuation analysis using orthogonal polynomials. Phys. Rev. E 101, 010201 (2020).
Govindan, R. B., Preissl, H., Eswaran, H., Campbell, J. Q. & Lowery, C. L. Detrended fluctuation analysis of short data sets: ANA pplication to fetal cardiac. PhysD: Nonlinear Phenom. 226, 23–31 (2007).
Govindan, R. B. et al. Detrended fluctuation analysis of non-stationary cardiac beat-to-beat interval of sick infants. EPL 108, 40005–p40001–p40006 (2014).
Mulkey, S. B. et al. The effect of labor and delivery mode on electrocortical and brainstem autonomic function during neonatal transition. Sci. Rep. 9, 11020 (2019).
Montagna, A. & Nosarti, C. Socio-emotional development following very preterm birth: pathways to psychopathology. Front Psychol. 7, 80 (2016).
Hack, M., Schluchter, M., Cartar, L. & Rahman, M. Blood pressure among very low birth weight (<1.5 kg) young adults. Pediatr. Res. 58, 677–684 (2005).
Mulkey, S. B. & du Plessis, A. J. Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatr. Res. 85, 120–126 (2019).
Siddiqui, S., Fifer, W. P., Ordonez-Retamar, M., Nugent, J. D. & Williams, I. A. An antenatal marker of neurodevelopmental outcomes in infants with congenital heart disease. J. Perinatol. 37, 953–957 (2017).
Haraldsdottir, K. et al. Heart rate recovery after maximal exercise is impaired in healthy young adults born preterm. Eur. J. Appl. Physiol. 119, 857–866 (2019).
Thiriez, G. et al. Altered autonomic control in preterm newborns with impaired neurological outcomes. Clin. Auton. Res. 25, 233–242 (2015).
Fyfe, K. L., Yiallourou, S. R., Wong, F. Y. & Horne, R. S. The development of cardiovascular and cerebral vascular control in preterm infants. Sleep. Med. Rev. 18, 299–310 (2014).
Fyfe, K. L. et al. The effect of gestational age at birth on post-term maturation of heart rate variability. Sleep 38, 1635–1644 (2015).
Karin, J., Hirsch, M. & Akselrod, S. An estimate of fetal autonomic state by spectral analysis of fetal heart rate fluctuations. Pediatr. Res. 34, 134–138 (1993).
Porges, S. W. in The Polyvagal Theory (WW Norton & Company, 2011).
Longin, E., Gerstner, T., Schaible, T., Lenz, T. & Konig, S. Maturation of the autonomic nervous system: differences in heart rate variability in premature vs. term infants. J. Perinat. Med. 34, 303–308 (2006).
Clairambault, J., Curzi-Dascalova, L., Kauffmann, F., Medigue, C. & Leffler, C. Heart rate variability in normal sleeping full-term and preterm neonates. Early Hum. Dev. 28, 169–183 (1992).
Siddiqui, S. et al. Autonomic regulation in fetuses with congenital heart disease. Early Hum. Dev. 91, 195–198 (2015).
Limperopoulos, C. et al. Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation 121, 26–33 (2010).
Clouchoux, C. et al. Delayed cortical development in fetuses with complex congenital heart disease. Cereb. Cortex 23, 2932–2943 (2013).
McQuillen, P. S., Goff, D. A. & Licht, D. J. Effects of congenital heart disease on brain development. Prog. Pediatr. Cardiol. 29, 79–85 (2010).
Segar, J. L. Fetal and Neonatal Cardiovascular Physiology in Fetal and Neonatal Physiology (eds Polin, R. A., Fox, W. W. & Abman, S. H.) 789–793 (Elsevier, 2011).
Bevan, R. et al. Responsiveness of human infant cerebral arteries to sympathetic nerve stimulation and vasoactive agents. Pediatr. Res. 44, 730–739 (1998).
Hayashi, S., Park, M. K. & Kuehl, T. J. Higher sensitivity of cerebral arteries isolated from premature and newborn baboons to adrenergic and cholinergic stimulation. Life Sci. 35, 253–260 (1984).
Lou, H. C., Lassen, N. A. & Friis-Hansen, B. Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J. Pediatr. 94, 118–121 (1979).
Kosiorek, A. et al. Predictors of neurological outcome following infant cardiac surgery without deep hypothermic circulatory arrest. Pediatr. Cardiol. (2021). Epub ahead of print.
Schlatterer, S. D. et al. Placental pathology and neuroimaging correlates in neonates with congenital heart disease. Sci. Rep. 9, 4137 (2019).
Andropoulos, D. B. et al. The association between brain injury, perioperative anesthetic exposure, and 12-month neurodevelopmental outcomes after neonatal cardiac surgery: a retrospective cohort study. Paediatr. Anaesth. 24, 266–274 (2014).
Rooks, V. J. et al. Prevalence and evolution of intracranial hemorrhage in asymptomatic term infants. AJNR Am. J. Neuroradiol. 29, 1082–1089 (2008).
Schneebaum Sender, N. et al. Effects of regional brain injury on the newborn autonomic nervous system. Early Hum. Dev. 90, 893–896 (2014).
Metzler, M. et al. Pattern of brain injury and depressed heart rate variability in newborns with hypoxic ischemic encephalopathy. Pediatr. Res. 82, 438–443 (2017).
Schneebaum Sender, N. et al. Cerebral modulation of the autonomic nervous system in term infants. J. Perinatol. 37, 558–562 (2017).
Funding
Grant support for this project is from the Canadian Institute of Health Research, MOP-8111 and National Institutes of Health: NHLBI R01 HL116585-01.
Author information
Authors and Affiliations
Contributions
S.D.S. designed the study, interpreted the data, and wrote the manuscript. R.B.G. performed HRV analysis for the study population and provided a critical review of the manuscript. J.M. interpreted and scored brain MRIs for brain injury and provided a critical review of the manuscript. S.D.B. performed statistical analyses for the study, interpreted the data, and provided a critical review of the manuscript. C.L. coordinated patient enrollment and clinical data acquisition and provided a critical review of the manuscript. M.T.D. interpreted patient echocardiograms, aided in study recruitment, and provided a critical review of the manuscript. S.B.M. provided a critical review of the manuscript and provided HRV data on subjects. C.L. designed the study with S.D.S. and A.J.d.P., provided MRI data on study subjects, and provided a critical review of the manuscript. A.J.d.P. designed the study and provided a critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Institutional Review Board of Children’s National Hospital approved this study and written informed consent was obtained from each participant.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schlatterer, S.D., Govindan, R.B., Murnick, J. et al. In infants with congenital heart disease autonomic dysfunction is associated with pre-operative brain injury. Pediatr Res 91, 1723–1729 (2022). https://doi.org/10.1038/s41390-021-01931-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01931-7