Abstract
Child abuse is common in the United States but is often undetected. The incidence of this form of abuse is difficult to quantify, but children with a history of abuse are at risk of chronic health conditions. Medical providers are in the unique position of triaging trauma patients and differentiating unintentional from abusive trauma, as well as having the important position of being a mandated reporter of abuse in all states. Obtaining a detailed history and screening for risk factors can help identify children at risk of abuse. Certain orthopedic injuries may be related to abuse, which may trigger clinical suspicion and lead to further workup or intervention. By increasing awareness, through medical provider education and increased screening, earlier detection of abuse may prevent more serious injuries and consequences. This review evaluates current literature regarding the orthopedic manifestations of child abuse in hopes of increasing medical provider awareness.
Impact
-
Child abuse is common in the United States but often remains undetected.
-
Medical professionals are in the unique position of evaluating trauma patients and identifying concerns for abusive injuries.
-
Certain orthopedic injuries may raise concern for abuse triggering clinical suspicion and further workup or intervention.
Similar content being viewed by others
Introduction
Child abuse is common in the United States but is often undetected.1 The definition of child abuse in the United States varies per state but is universally defined in the Federal Child Abuse Prevention and Treatment Act as “any recent act or failure to act on the part of a parent or caretaker which results in death, serious physical or emotional harm, sexual abuse or exploitation” or “an act or failure to act which presents an imminent risk of serious harm.”2 The incidence of child abuse has been estimated to be approximately 10.3 per 1000 children.1 Child abuse is a public health issue with lifelong implications.2 Adolescents who suffered from abuse during childhood have high rates of depression, conduct disorder, drug abuse, and cigarette smoking.3,4 Adults with a history of physical abuse when they were children are more likely to report chronic physical and mental health conditions.5
Medical professionals are in the unique position of triaging trauma patients and differentiating accidental and abusive trauma. This is an invaluable skill developed through clinical reasoning and recognition of presenting patterns that can have long-lasting effects on a patient’s well-being. This process begins by taking a comprehensive medical history and can be initiated by emergency providers, medical physicians, and surgeons alike, making recognition of signs of child abuse an important skill for all providers to possess. Certain orthopedic injuries, in particular, may be related to abuse, which may trigger clinical suspicion and lead to further workup or intervention. This review evaluates current literature regarding the orthopedic presentations of child abuse in hopes of increasing provider awareness.
Articles were identified through biomedical search engines including PubMed and Google Scholar, identified for relevance and applicability to the topic of orthopedic manifestations of abuse. Emphasis was placed on more recent studies and meta-analyses that have influenced or have the potential to influence provider practice.
Presentation
History
Children younger than 4 years old are at the greatest risk of serious abuse and are the least able to explain or convey what caused their injuries,6 and children under 1 year of age are at particularly elevated risk, especially when presenting with orthopedic injuries.7 History taking is therefore often done with a caregiver who may or may not be knowledgeable of possible abuse. In any case, involving suspected child abuse, it is recommended that parents be allowed to provide full histories without interruption to minimize provider influence on the conversation, with multiple caregivers interviewed separately when possible.2 Documentation is key during history taking, including all possible means of trauma. Although there is immense value in interviewing an adolescent patient alone, victims may be unwilling to disclose abuse due to fear or out of loyalty to an abuser, and denial is not enough to exclude potential abuse.1 Patients may also change their history or have one that differs from that of the parent or guardian. Younger children may also be unable to communicate the abuse that took place and may only communicate their abuse with nonverbal cues.8 Medical history with an emphasis on prior traumatic injuries is imperative, as recurrent admissions are frequently the catalyst for clinical suspicion.1 Evidence exists suggesting that systematic screening of all pediatric emergency department admissions can increase detection of child abuse.9 Chan et al. developed a tool to evaluate caregiver abuse risk when they questioned parents of children in the community. Pandya et al. and Baldwin et al. developed diagnostic algorithms to calculate the abuse likelihood of a child presenting with a fracture in the emergency room, based on various factors including age, hospitalization history, and significant historical elements.10,11 Imperative to these risk factor assessments and in general when evaluating a patient’s history, history provided by the family can provide additional information to help make an assessment.
Caregivers’ explanations for an injury in the setting of child abuse can vary greatly, with a fall often stated as the means for a traumatic fracture.12 Nevertheless, certain details of a patient presentation can warrant further investigation and can be particularly telling in the setting of provider suspicion. Explicit denial of trauma in conflict with clinical symptoms, particularly when given by the patient, can be a particularly sensitive sign. Explanations that are inconsistent with the observed trauma should also raise suspicions and explanations inconsistent with the developmental abilities of the patient can be similarly concerning for abuse; for instance, a purported fall in a nonambulatory infant or child presenting with a high-energy fracture.13,14 Any changes or inconsistencies in caregiver histories should raise concern, especially when discussing major aspects of the injury, although speculation about patient or caregivers’ demeanor while being interviewed should be avoided due to the significant potential for implicit bias and subjective nature of such interviewing. Lastly, any inexplicable delay in seeking care should amplify clinical suspicions of abuse.2,15
Although beyond the scope of this review, it is imperative to recognize that provider bias has been identified in the literature as impacting the reporting and workup of suspected pediatric abuse.16,17,18 Child abuse clinical pathways have been identified to improve odds of identifying cases concerning child maltreatment and ensuring that those children receive an appropriate workup and consultation with a child abuse pediatrician while also mitigating the effects of healthcare bias,19 suggesting that standardization of practice is a valuable means of improving equitable management of suspected abuse. This remains an area of ongoing study.
Fracture properties
After soft tissue injuries, such as bruising, fractures are the second most common medical presentation of child abuse and can be present in 30–50% of abuse cases.20 Although fractures are common injuries in pediatric patients, some fracture patterns and locations are more suggestive of abuse compared to others.12 Multiple fractures in varying stages of healing are considered one of the signs of potential abusive trauma (Fig. 1).21 Spiral fractures of any bone with even minor clinical suspicion were once considered pathognomonic for nonaccidental trauma, as the twisting force required for fracture is classically observed when limbs are forcibly rotated by another person.21 However, evidence in the literature now suggests that spiral fractures can occur frequently in cases of observed accidental trauma and the finding is neither sensitive nor specific for abuse;20,22 the actual evaluation of fractures in suspected trauma is far more complicated than distillation into pathognomonic fracture types. In a review of pediatric long bone fractures, Pierce et al. discuss the importance of connecting patient history with fracture biomechanics. For example, transverse fractures, in which the fracture line is perpendicular to the shaft, require high-energy bending loads that could be in conflict with a caregiver history of a low-energy fall.23 A spiral lower extremity long bone fracture in a nonambulatory patient would be an injury inconsistent with a patient’s stage of motor development.24 Fracture morphology should be considered in association with the patient’s time until presentation, as a non-displaced buckle fracture would have minimal symptoms compared to a spiral femur fracture, with time to presentation understandably different regardless of injury etiology.23,25 The fracture type is not itself diagnostic of the origin of injury but can be crucially reflective of the nature of the injury, and discrepancies between this nature and other components of a patient’s history and the presentation should elevate suspicion of potential abuse.
The location of the fracture can also identify patients for whom abuse is a concern. Rib fractures, specifically posterior rib fractures (Fig. 2), are conventionally considered suspicious for abuse, as this is an atypical accidental injury that suggests a squeezing compressive force around the trunk.15,20,26,27 In one study, posterior rib fractures were found to be due to abuse in 70% of cases.28 Humerus fractures were found to have a 50% probability of being due to abuse in children under 3 years old when otherwise obvious trauma was excluded; however, with a very wide confidence interval of 6–94%,28 suggesting that fracture type alone is not specific for abuse.21,29 Atypical injuries without obvious cause are rarely reported, but should immediately raise concern for abusive trauma, such as metaphyseal corner fractures,20 cervical vertebral fractures,30 and femoral neck fractures.31 In these cases, a central tenet is that infants simply cannot generate the force required to sustain such fractures. Swischuk et al. note that it is very unlikely for normal infants to sustain metaphyseal corner fractures (Fig. 3) with normal daily activity or mild falls unless the bone appears abnormal due to demineralization and osteoporosis, signifying an underlying bone disorder.32 Loder et al. found in their review that 15% of femur fractures in children under the age of two were due to abuse, with falls accounting for the majority of femoral fractures.33
Physical exam
In the setting of traumatic fractures, other physical examination findings may be highly significant and assist in identifying cases of physical abuse. Bruising in children of all ages is the most common injury from physical abuse and can be crucial in differentiating accidental and nonaccidental trauma.34,35,36,37,38 In a 2021 study, Pierce et al. validated a refined bruising clinical decision rule, the TEN-4-FACESp, for use in children under 4 years of age. The rule would raise concerns for abuse in young children with bruising to the torso, ear, neck, frenulum, angle of the jaw, fleshy facial cheeks, eyelids, and subconjunctival hemorrhages. The study also identifies concern for abuse when there is patterned bruising to a child or when there is any bruise on a patient <4.99 months old (TEN-4).37 This rule was performed with high sensitivity (96%) as well as high specificity when screening bruised patients for abuse, with any bruise of the TEN regions alone correctly identifying abuse in 81% of the identified patients. The upcoming implementation of this standardized rule, which effectively utilizes and encompasses up-to-date knowledge on bruising patterns, will be a crucial tool in identifying nonaccidental trauma while helping to minimize stress in accidental trauma cases.
Nearly one-third of young children found to have abusive fractures had signs and symptoms suggestive of trauma previously missed during healthcare interactions.39 These signs primarily involved swelling or bruising, particularly in unusual areas such as the ears or neck, but also included symptoms such as unexplainable irritability, fever, and vomiting.14 Exam findings concerning traumatic injury may include bruises, burns, edema, other bony abnormalities, or signs of head or abdominal trauma. Any signs of injury in a preambulatory child should also raise immediate concern for physical abuse and trigger a more thorough evaluation.2
When a child presents with a nonspecific fracture, a thorough skin examination may reveal concerning bruises or other injuries which should raise concerns of physical abuse and trigger a further workup.
Imaging
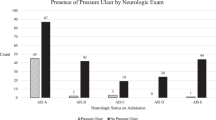
The use of imaging modalities in conjunction with the physical exam is crucial in evaluating suspicions of abuse. Given the minor but inherent risk of imaging in young patients, the American College of Radiology (ACR) has guidelines for imaging suspected physical abuse.40 Per ACR recommendation, X-ray skeletal surveys are the primary tool for evaluation of skeletal trauma in young children and should consist of frontal and lateral views of the skull, lateral views of the cervical spine and thoracolumbosacral spine, and single frontal views of the long bones, hands, feet, chest, and abdomen.24 Repeat skeletal surveys can exclude pelvis, spine, and skull radiographs if no injury was seen on primary evaluation, to limit unnecessary radiation exposure. These radiographs should be repeated when there are concerns for abuse and a fracture was identified on the initial skeletal survey, as well as in the case of an ambiguous or negative primary survey with high clinical suspicion for abuse.40 Since 80% of abused children with fractures are <18 months of age, the ACR recommends a primary skeletal survey in all children <2 years old when abuse is suspected.25 ACR recommendation of skeletal survey decreases if the child is >24 months since children older than 24 months can often verbalize, so initial imaging may be targeted to a specific area of their body.25 Noncontrast computed tomography scans should be used for patients with suspected abusive head trauma, which includes any suspected abuse patients with clear head trauma, such as neurologic changes, facial injuries, or hemorrhagic retinopathy, as well as any child under the age of 6 months in which there are concerns for abuse.24,41 Occult head injury was found by Boehnke et al. in 19.7% of children under 2 years of age being evaluated for suspected abuse without signs of head injury,42 and Henry et al. identified occult head injury in 6.5% of evaluated children under 12 months old,43 both suggestive of a low threshold for neuroimaging utilization in the setting of suspected abuse. Magnetic resonance imaging of the head can be useful for children with suspected abusive head trauma, but it is not usually utilized in the emergent setting because it often requires sedation.
Imaging is inherently warranted in cases of pediatric fracture but is also valuable in cases of suspected abuse without obvious skeletal injury. Rib fractures and metaphyseal corner injuries of long bones are often not clinically obvious, particularly in infants, with observable indications like bruising not commonly present.2,20 A 2011 study by Duffy et al. found occult orthopedic trauma through a skeletal survey in 11% of patients, which proved to be a crucial component in confirming abuse in over half of those cases.44 Repeated skeletal surveys per ACR guidelines have been found to increase the number of diagnosed fractures by more than 25% in abused patients.45 There is evidence suggesting a benefit to performing skeletal surveys on siblings of abused children, with a study by Lindberg et al. finding evidence of fractures on over 11% of surveyed siblings.46
Treatment/management
If a physician suspects child abuse, most states require them to report their suspicion to the police or appropriate authority. Forty-seven states designate physicians as “mandated reporters,” while Indiana, New Jersey, and Wyoming do not specify specific professional groups as mandated reporters, but nevertheless require all individuals who suspect abuse to report it.47 In addition, 18 states require reporting of suspected child abuse by any person who suspects it, not just healthcare professionals.47 While states may mandate that certain people report abuse, anyone can voluntarily report suspected abuse; these people are referred to as “permissive reporters.”47 Reports are required when the reporter suspects or has reason to believe that abuse is occurring; however, they do not need to have proof that mistreatment has occurred.47 Mandatory and voluntary reporters are protected in all states from liability when reporting suspected child abuse under “good faith” laws.48 Many states also provide additional immunity for specific actions medical practitioners take to evaluate suspected child abuse, such as imaging studies or lab tests, performing a medical exam, or disclosing medical records in the court of law.48
Medical professionals can provide treatment for an injury resulting from abuse as is appropriate for the specific injury or injuries (e.g., splint or casting of fracture) and should fulfill their reporting requirements as soon as possible without delaying treatment. Depending on the severity of injuries, patients may be hospitalized or discharged and scheduled for follow-up care.2 In cases of child abuse, medical or mental health treatment for family members may also be necessary since domestic violence, drug abuse, and other stressors can co-occur with child abuse.2
When evaluating pediatric fractures, especially when the fracture type appears to require a higher force mechanism than described by caregivers, an evaluation for genetic and metabolic causes of bone fragility may be necessary for the differential diagnosis of fractures.49 The possibility of a metabolic cause of fractures may be raised in legal proceedings and therefore should be considered and excluded if appropriate.
The most common metabolic bone disease resulting in fractures is osteogenesis imperfect (OI).50 Leventhal et al. estimated that each year OI is responsible for roughly 0.85% of 15,000 fractures in children under the age of 36 months.51 Rickets, which results from vitamin D and calcium deficiency, is the most common metabolic bone disease in the pediatric population.52 Rickets is a rare but possible etiology of fractures in children, with poor skeletal mineralization putting these patients at increased risk of atypical or major fractures from low-energy trauma.53,54 In clinical practice, it is important to differentiate rickets from low vitamin D status, which is common in children and does not result in increased fracture risk.55,56,57 Some reports have also suggested that children with Ehlers–Danlos syndrome (EDS) may have an increased risk of fractures.58,59,60 However, controversy exists surrounding this topic and the previous studies which suggest that EDS is associated with an increased risk of fractures in infants. More recently, a population-based case–control study by Rolfes et al. found that individuals with EDS were more likely to have one or more fractures during childhood; however, none had fractures during the first year of life.61
In addition to genetic causes of pathological fractures, it is also important to consider other effects on bone health such as inflammatory diseases, oncological diseases, chronic total parenteral nutrition, older children who are not weight bearing, extreme prematurity, etc.62
When there is a concern for fractures resulting from abuse, it is important to complete a comprehensive medical evaluation to rule out other possible causes such as underlying bone disease. However, it is also important to note that while having an underlying bone disease may predispose a child to fractures, it does not rule out simultaneous abuse as a cause of fractures. Consultation with child abuse pediatricians can therefore aid in evaluating patients with complex presentations and underlying diseases.
Future directions
Prevention of future incidents of abuse is important although challenging. By increasing medical provider awareness of child abuse through education and increased screening, abuse may be identified earlier, preventing continued or worsening abuse. Pediatricians or other providers of pediatric care can play an important role in preventing child abuse by recognizing risk factors, providing support for families, and advocating for prevention programs in their communities.2 By increasing availability and access to resources regarding child abuse, more people may recognize and report suspected abuse. Therefore, it is important to continue to compile and disseminate materials with clear and concise language regarding abuse that both medical and non-medical professionals can understand.63
Summary
Child abuse often remains undetected in the United States despite the frequency at which it occurs. The literature on the presentation and screening of child abuse is constantly evolving, with an emphasis on recognizing and managing such injuries. Child victims of physical abuse may present to a number of physicians and allied healthcare professionals including family practice and emergency medicine physicians, pediatricians, and orthopedists, underscoring the need for a multidisciplinary approach to the management of this problem. Awareness and vigilance practiced by all medical professionals who evaluate pediatric patients can help improve the detection of child abuse. By doing so, we can continually improve care for this vulnerable population.
References
ACF. Child maltreatment. ACF Archive https://www.acf.hhs.gov/cb/resource/child-maltreatment-2018 (2018).
Christian, C. W. Committee on Child Abuse and Neglect, American Academy of Pediatrics. evaluation suspected child Phys. Abus. Pediatrics 135, e1337–e1354 (2015).
Kaplan, S. J. et al. Adolescent physical abuse: risk for adolescent psychiatric disorders. Am. J. Psychiatry 155, 954–959 (1998).
Hussey, J. M., Chang, J. J. & Kotch, J. B. Child maltreatment in the United States: prevalence, risk factors, and adolescent health consequences. Pediatrics 118, 933–942 (2006).
Shaw, B. A. & Krause, N. Exposure to physical violence during childhood, aging, and health. J. Aging Health 14, 467–494 (2002).
Gross, R. H. & Stranger, M. Causative factors responsible for femoral fractures in infants and young children. J. Pediatr. Orthop. 3, 341–343 (1983).
Rivara, F. P., Kamitsuka, M. D. & Quan, L. Injuries to children younger than 1 year of age. Pediatrics. 81, 93–97 (1988).
Katz, C. et al. Non-verbal behavior of children who disclose or do not disclose child abuse in investigative interviews. Child Abuse Negl. 36, 12–20 (2012).
Louwers, E. et al. Effects of systematic screening and detection of child abuse in emergency departments. Pediatrics 130, 457–464 (2012).
Pandya, N. K., Baldwin, K. D., Wolfgruber, H., Drummond, D. S. & Hosalkar, H. S. Humerus fractures in the pediatric population: an algorithm to identify abuse. J. Pediatr. Orthop. B 19, 535–541 (2010).
Baldwin, K. D. et al. Femur fractures in the pediatric population: abuse or accidental trauma? Clin. Orthop. Relat. Res. 469, 798–804 (2011).
Leventhal, J. M., Thomas, S. A., Rosenfield, N. S. & Markowitz, R. I. Fractures in young children: distinguishing child abuse from unintentional injuries. Am. J. Dis. Child. 147, 87–92 (1993).
Preer, G., Sorrentino, D. & Newton, A. W. Child abuse pediatrics: prevention, evaluation, and treatment. Curr. Opin. Pediatr. 24, 266–273 (2012).
Sink, E. L. et al. Child abuse. The role of the orthopaedic surgeon in nonaccidental trauma. Clin. Orthop. Relat. Res. 469, 790–797 (2011).
Kleinman, P. K., Marks, S. C., Nimkin, K., Rayder, S. M. & Kessler, S. C. Rib fractures in 31 abused infants: postmortem radiologic- histopathologic study. Radiology 200, 807–810 (1996).
Wood, J. N. et al. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics 126, 408–414 (2010).
Lane, W. G., Rubin, D. M., Monteith, R. & Christian, C. W. Racial differences in the evaluation of pediatric fractures for physical abuse. J. Am. Med. Assoc. 288, 1603–1609 (2002).
Rangel, E. L., Burd, R. S. & Falcone, R. A. Socioeconomic disparities in infant mortality after nonaccidental trauma: a multicenter study. J. Trauma 69, 20–25 (2010).
Stavas, N., Paine, C., Song, L., Shults, J. & Wood, J. Impact of child abuse clinical pathways on skeletal survey performance in high-risk infants. Acad. Pediatr. 20, 39–45 (2020).
Scherl, S. A. Orthopaedic aspects of child abuse. Curr. Orthop. Pract. 24, 625–630 (2013).
Sullivan, C. M. Child abuse and the legal system: the orthopaedic surgeon’s role in diagnosis. Clin. Orthop. Relat. Res. 469, 768–775 (2011).
Scherl, S. A. et al. Accidental and nonaccidental femur fractures in children. Clin. Orthop. Relat. Res. https://doi.org/10.1097/00003086-200007000-00014, 96–105 (2000).
Pierce, M. C., Bertocci, G. E., Vogeley, E. & Moreland, M. S. Evaluating long bone fractures in children: a biomechanical approach with illustrative cases. Child Abuse Negl. 28, 505–524 (2004).
Strait, R. T., Siegel, R. M. & Shapiro, R. A. Humeral fractures without obvious etiologies in children less than 3 years of age: When is it abuse? Pediatrics 96, 667–671 (1995).
Rex, C. & Kay, P. R. Features of femoral fractures in nonaccidental injury. J. Pediatr. Orthop. 20, 411–413 (2000).
Barsness, K. A. et al. The positive predictive value of rib fractures as an indicator of nonaccidental trauma in children. J. Trauma 54, 1107–1110 (2003).
Flaherty, E. G. et al. Evaluating children with fractures for child physical abuse. Pediatrics 133, e477–e489 (2014).
Kemp, A. M. et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ 337, 859–862 (2008).
Taitz, J., Moran, K. & O’Meara, M. Long bone fractures in children under 3 years of age: Is abuse being missed in Emergency Department presentations? J. Paediatr. Child Health 40, 170–174 (2004).
Feldman, K. W., Avellino, A. M., Sugar, N. F. & Ellenbogen, R. G. Cervical spinal cord injury in abused children. Pediatr. Emerg. Care 24, 222–227 (2008).
Pastor, A. J., Gupta, A., Press, C. M. & Gourineni, P. Femoral neck fracture as the sentinel sign of child abuse in an infant: a case report. J. Pediatr. Orthop. B 21, 587–591 (2012).
Swischuk, L. E. Metaphyseal corner fractures in infants: a review. Emerg. Radiol. 5, 103–107 (1998).
Loder, R. T., O’Donnell, P. W. & Feinberg, J. R. Epidemiology and mechanisms of femur fractures in children. J. Pediatr. Orthop. 26, 561–566 (2006).
Ellerstein, N. S. The cutaneous manifestations of child abuse and neglect. Am. J. Dis. Child 133, 906–909 (1979).
Maguire, S. & Mann, M. Systematic reviews of bruising in relation to child abuse-what have we learnt: an overview of review updates. Evid. Based Child Health 8, 255–263 (2013).
Pierce, M. C., Kaczor, K., Aldridge, S., O’Flynn, J. & Lorenz, D. J. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics 125, 67–74 (2010).
Pierce, M. C. et al. Validation of a clinical decision rule to predict abuse in young children based on bruising characteristics. JAMA Netw. Open 4, https://doi.org/10.1001/jamanetworkopen.2021.5832 (2021).
Sugar, N. F., Taylor, J. A. & Feldman, K. W. Bruises in infants and toddlers: those who don’t cruise rarely bruise. Arch. Pediatr. Adolesc. Med. 153, 399–403 (1999).
Thorpe, E. L., Zuckerbraun, N. S., Wolford, J. E. & Berger, R. P. Missed opportunities to diagnose child physical abuse. Pediatr. Emerg. Care 30, 771–776 (2014).
Expert Panel on Pediatric Imaging: Wootton-Gorges, S. L. et al. ACR Appropriateness Criteria® suspected physical abuse-child. J. Am. Coll. Radiol. 14, S338–S349 (2017).
Bajaj, M. & Offiah, A. C. Imaging in suspected child abuse: necessity or radiation hazard? Arch. Dis. Child 100, 1163–1168 (2015).
Boehnke, M., Mirsky, D., Stence, N., Stanley, R. M. & Lindberg, D. M. Occult head injury is common in children with concern for physical abuse. Pediatr. Radiol. 48, 1123–1129 (2018).
Henry, M. K. et al. Occult head injuries in infants evaluated for physical abuse. Child Abuse Negl. 103, https://doi.org/10.1016/j.chiabu.2020.104431 (2020).
Duffy, S. O., Squires, J., Fromkin, J. B. & Berger, R. P. Use of skeletal surveys to evaluate for physical abuse: analysis of 703 consecutive skeletal surveys. Pediatrics 127, e47–e52 (2011).
Kleinman, P. K. et al. Follow-up skeletal surveys in suspected child abuse. Am. J. Roentgenol. 167, 893–896 (1996).
Lindberg, D. M. et al. Prevalence of abusive injuries in siblings and household contacts of physically abused children. Pediatrics 130, 193–201 (2012).
Child Welfare Information Gateway. Mandatory reporters of child abuse and neglect. https://www.childwelfare.gov/topics/systemwide/laws-policies/statutes/manda/ (2019).
Child Welfare Information Gateway. Immunity for reporters of child abuse and neglect. https://www.childwelfare.gov/pubPDFs/immunity.pdf (2018).
Miller, M. & Mirkin, L. D. Classical metaphyseal lesions thought to be pathognomonic of child abuse are often artifacts or indicative of metabolic bone disease. Med. Hypotheses 115, 65–71 (2018).
Pepin, M. G. & Byers, P. H. What every clinical geneticist should know about testing for osteogenesis imperfecta in suspected child abuse cases. Am. J. Med. Genet. C 169, 307–313 (2015).
Leventhal, J. M., Martin, K. D. & Asnes, A. G. Fractures and traumatic brain injuries: abuse versus accidents in a US database of hospitalized children. Pediatrics 126, https://doi.org/10.1542/PEDS.2009-1076 (2010).
Thacher, T. D. et al. Increasing incidence of nutritional rickets: a population-based study in Olmsted County, Minnesota. Mayo Clin. Proc. 88, 176–183 (2013).
Chapman, T. et al. Fractures in infants and toddlers with rickets. Pediatr. Radiol. 40, 1184–1189 (2010).
Servaes, S. et al. The etiology and significance of fractures in infants and young children: a critical multidisciplinary review. Pediatr. Radiol. 46, 591–600 (2016).
Schilling, S., Wood, J. N., Levine, M. A., Langdon, D. & Christian, C. W. Vitamin D status in abused and nonabused children younger than 2 years old with fractures. Pediatrics 127, 835–841 (2011).
Contreras, J. J., Hiestand, B., O’Neill, J. C., Schwartz, R. & Nadkarni, M. Vitamin D deficiency in children with fractures. Pediatr. Emerg. Care 30, 777–781 (2014).
Keller, K. A. & Barnes, P. D. Rickets vs. abuse: a national and international epidemic. Pediatr. Radiol. 38, 1210–1216 (2008).
Owen, S. M. & Durst, R. D. Ehlers-Danlos syndrome simulating child abuse. Arch. Dermatol. 120, 97–101 (1984).
Holick, M. F., Shirvani, A. & Charoenngam, N. Fetal fractures in an infant with maternal Ehlers-Danlos syndrome, CCDC134 pathogenic mutation and a negative genetic test for osteogenesis imperfecta. Child 8, 512 (2021).
Holick, M. F., Hossein-Nezhad, A. & Tabatabaei, F. Multiple fractures in infants who have Ehlers-Danlos/hypermobility syndrome and or vitamin D deficiency: a case series of 72 infants whose parents were accused of child abuse and neglect. Dermatoendocrinology 9, https://doi.org/10.1080/19381980.2017.1279768 (2017).
Rolfes, M. C. et al. Fracture incidence in Ehlers-Danlos syndrome—a population-based case-control study. Child Abuse Negl. 91, 95–101 (2019).
Boyce, A. M. & Gafni, R. I. Approach to the child with fractures. J. Clin. Endocrinol. Metab. 96, 1943–1952 (2011).
Child Welfare Information Gateway. Prevention Resource Guide Chapter 5: tip sheets for parents and caregivers. https://www.childwelfare.gov/topics/preventing/preventionmonth/resources/resource-guide (2019).
Author information
Authors and Affiliations
Contributions
All authors participated in the research and preparation of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Milner, J.D., Hartnett, D.A., DeFroda, S.F. et al. Orthopedic manifestations of child abuse. Pediatr Res 92, 647–652 (2022). https://doi.org/10.1038/s41390-021-01850-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01850-7