Abstract
Background
Previous studies showed that preterm birth increased the risk for hospital admissions in infancy and childhood due to some acute diseases. However, the risk of preterm children developing Kawasaki disease remains unknown. In the present study, we investigate whether preterm birth increased the morbidity of Kawasaki disease.
Methods
We included 36,885 (34,880 term and 2005 preterm) children born in 2010 in Japan. We examined the association between preterm birth and hospitalization due to Kawasaki disease using a large nationwide survey in Japan.
Results
In log-linear regression models that were adjusted for children’s characteristics (sex, singleton birth, and parity), parental characteristics (maternal age, maternal smoking, paternal smoking, maternal education, and paternal income), and residential area, preterm infants were more likely to be hospitalized due to Kawasaki disease (adjusted risk ratio: 1·55, 95% confidence interval: 1.01–2.39). We then examined whether breastfeeding status modified the potential adverse effects of preterm birth on health outcome. Preterm infants with partial breastfeeding or formula feeding had a significantly higher risk of hospitalization due to Kawasaki disease compared with term infants with exclusive breastfeeding.
Conclusions
Preterm infants were at a high risk for Kawasaki disease, and exclusive breastfeeding might prevent this disease among preterm infants.
Impact
-
Previous studies showed that preterm birth increased the risk for hospital admissions in infancy and childhood due to some acute diseases, however, the risk of preterm children developing Kawasaki disease remains unknown.
-
This Japanese large population-based study showed that preterm infants were at a high risk for Kawasaki disease for the first time.
-
Furthermore, this study suggested that exclusively breastfeeding might prevent Kawasaki disease among preterm infants.
Similar content being viewed by others
Introduction
Although the cause of Kawasaki disease (KD) remains unknown, the risk factors for KD have been studied and discussed for a long time and several risk factors were previously reported. As the host factor, a higher incidence of KD in specific Asian countries1 and racial differences in the incidence of KD2 have been reported. These findings suggested that there is a relationship between susceptibility to KD and a patient’s genetic background, and some susceptibility genes that may be related to KD,3,4,5,6,7,8 such as ITPKC3 have been reported. Another previous study also proposed a relationship between a defect in the innate immune system and KD.9
A pathogen is also suspected to be involved in the development of KD based on previous periodic epidemics and regional epidemic areas of KD,10 although no specific pathogen has been identified.11,12 Currently, KD is generally thought to be systemic vasculitis in childhood due to an immunological response that is evoked by an infectious agent and an environmental agent in genetically and immunologically susceptible individuals.13
It should be noted that preterm birth is a major public health concern worldwide, and it can have a negative impact on child health and development.14 Previous studies showed that preterm birth increases the risk for hospital admissions in infancy and childhood due to acute disease such as respiratory infections, enterocolitis, and asthma.14,15 Thus, preterm birth may also be related to the development of KD, similar to other major acute childhood illness. However, the relationship between preterm birth and the development of KD has not previously been elucidated. In the present study, we used the national data of population-based longitudinal cohort study to investigate whether preterm birth increased KD morbidity and how breastfeeding affects KD morbidity in preterm infants.
Methods
Study participants
The Japanese Ministry of Health, Labour and Welfare implemented a nationally representative longitudinal survey between May 10 and 24, 2010, which was called the Longitudinal Survey of Newborns in the 21st Century (2010 cohort),16,17 to follow infants who were born throughout the country. Baseline questionnaires were sent to all families when infants who were born during the study period were 6 months old. Among the 43,767 questionnaires that were mailed, 38,554 were completed and returned (88.1% response rate). Follow-up questionnaires were sent to all participants who initially responded each year (at 18, 30, 42, 54, and 66 months). The sixth survey was completed in 2014. Birth record data such as birth weight, gestational age, singleton or multiple births, sex, parity, and parental age at delivery were obtained from the Vital Statistics system for each child who was included in this survey. The Vital Statistics is basic statistics conducted by the Japanese Ministry of Health, Labor and Welfare that record information on births, deaths, stillbirths, marriages, and divorces which occurred in Japan within the survey year.
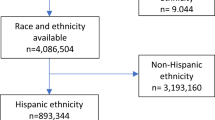
Children were excluded if they did not have information on their gestational age (n = 7). In the present study, to assess the effect of preterm birth on KD morbidity compared to term birth, we excluded children who were born after 42 weeks gestation (n = 127). We also excluded children whose at least one parent did not have Japanese nationality to reduce the impact of racial differences (n = 1535), and thus, 36,885 children were included in the analysis (Fig. 1).
Gestational age
We determined each infant’s gestational age from their birth records and categorized them into two groups, which were term infants (37–41 weeks) and preterm infants (22–36 weeks). In Japan, the gestational age is routinely estimated by the date of the onset of the mother’s last menstrual period and then corrected by the first-trimester ultrasound in almost all pregnancy cases.
Morbidity of Kawasaki disease
The survey obtained information on whether the child had been hospitalized during the previous 12 months for any reason and asked respondents to provide further details if the hospitalization resulted from one of several common diseases including KD. The same question was asked in each survey from age 18 to 66 months. To assess KD morbidity, we used the results of the question “hospitalizations due to KD” in early childhood (up to 66 months of age).
Statistical analysis
We compared the baseline characteristics of eligible term and preterm infants. To investigate the association between preterm birth and KD morbidity between 6 and 66 months of age, we used log-linear regression models and estimated risk ratios (RRs) and 95% confidence intervals (CIs) for the hospitalization due to KD using the “term infants” as the reference category. A generalized estimating equation analysis was conducted to account for the longitudinal nature of the surveys. To evaluate the shape of the association of gestational age with the risk of hospitalization due to KD, we conducted a restricted cubic spline analysis, which was a method to flexibly model non-linear relationships in regression models.18
We selected the potential confounders based on the previous studies.16,17,19 The child factors included sex (dichotomous), singleton or multiple births (dichotomous), and parity (0 or more than 1, dichotomous). The parental factors included maternal age at delivery (continuous), maternal smoking status (non-smoker or smoker, dichotomous), maternal educational level (categorical), paternal income (categorical), and residential area. Data regarding infant sex, singleton or multiple births, parity, and maternal age at delivery were obtained from the birth record. Maternal smoking status was ascertained from the first survey (at infant age of 6 months). Paternal income was obtained from the questionnaires of the Longitudinal Survey of Newborns in the 21st Century. The type of municipality was obtained from the 2010 national census. We obtained the parental educational level from the second survey questionnaire, and we classified the original eight categories of educational level into three categories as follows: high school or less, junior college (2 years) or vocational school, and university (4 years) or higher.
Furthermore, because a previous study reported that breastfeeding could reduce the risk of developing KD,17 we evaluated how breastfeeding could modify the potential adverse effects of preterm birth on KD morbidity. We ascertained the infants’ feeding status according to the first survey (6–7 months of age), which included questions on infant-feeding practices to specify whether the children had been breastfed, only colostrum-fed, or formula-fed.16 We created “exclusive breastfeeding” and “non-exclusive breastfeeding” categories using the information on breast- and formula feeding. We categorized “exclusive breastfeeding” as when parents answered that they had breastfed their babies and never formula-fed. However, we categorized “non-exclusive breastfeeding” as when parents had given formula. There were 306 cases with missing information about infant-feeding practices. We created four new categories by combining birth status with breastfeeding status: i.e., term infants with exclusive breastfeeding; term infants with non-exclusive breastfeeding; preterm infants with exclusive breastfeeding; and preterm infants with non-exclusive breastfeeding. We evaluated the association between the new categories and hospitalization due to KD using “term infants with exclusive breastfeeding” as the reference category. We estimated the RRs and 95% CIs adjusting for the same set of confounding variables.
Stata SE version 16 statistical software (StataCorp., College Station, TX) was used for all analyses. This study was approved by the Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences Institutional Review Board (No. 1506-073).
Results
The baseline characteristics of the eligible infants separated into term and preterm infant groups are summarized in Table 1. Preterm infants tended to be male and had multiple births compared with term infants. Compared to term infants, the proportion of breastfed infants is lower for preterm infants, especially exclusively breastfed infants (Table 1).
The follow-up percent and percent of hospital admissions due to KD in each period for the term or preterm births are shown in Table 2. The follow-up rate for term infants and preterm infants at survey six was 69.9% and 67.6%, respectively.
The RRs and 95% CIs for the association between preterm birth and hospitalization due to KD between 6 and 66 months of age are presented in Table 3. Preterm infants were more likely to be hospitalized than term infants due to KD between six and 66 months after controlling for potentially confounding variables (aRR: 1.55, 95% CI: 1·01–2.39). The restricted cubic spline analysis showed the tendency toward an increase in the RR of KD as gestational age decreased, although the 95% CI was wide (Fig. 2).
The restricted cubic spline analysis showed a tendency toward an increase in the risk ratio of Kawasaki disease as the gestational age decreased, although the 95% confidential interval was wide. The solid line indicates point estimates of the risk ratio and dashed lines indicate upper and lower bounds of 95% confidential interval.
When we used the combined categories for birth status and breastfeeding status (Table 4), preterm infants with partial breastfeeding or formula feeding had a significantly higher risk of hospitalization due to KD compared with term infants with exclusive breastfeeding (aRR: 1.80, 95% CI: 1.09–2.98).
Discussion
In the present study, we examined the association between preterm birth and the development of KD from 6 to 66 months of age using data from a nationwide, population-based, longitudinal survey in Japan. We observed the increased risk for the development of KD in preterm children. Taking into account the breastfeeding status, only preterm infants with non-exclusive breastfeeding had a significantly increased risk for KD compared with exclusively breastfed term infants.
To the best of our knowledge, this is the first study that investigated the relationship between preterm birth and KD. First, we would like to consider this association based on the hypothesis that a pathogen triggers the development of KD.13 Transplacental active transport of IgG to the fetus occurs during pregnancy, and fetal IgG concentration increase sharply during the third trimester.20 Thus, preterm infants are born with low levels of immunoglobulin. Including this reason, there could be a potentially increased susceptibility to infection in preterm infants, which may persist throughout infancy.16,21 This susceptibility to infection might be associated with an increased risk of KD. However, the altered gut microbiota is receiving much attention as a possible pathogenesis mechanism for KD.22 Chen et al. recently reported a significant reduction in fecal microbial diversity in acute KD children using 16S rRNA gene sequencing.23 Kinumaki et al. also found a markedly increased amount of Streptococcus spp. in the gut microbiota of acute-phase KD patients and a relative increase in the number of Ruminococcus bacteria in a non-acute phase of KD using metagenomic analysis.24 Considering that the difference in gut microbiota between preterm infants and full-term infants persisted until 4 years of age,25 altered gut microbiota in preterm infants may be associated with the development of KD during the present study.
For the protective effect of breastfeeding on the development of KD, gut microbiota and regulatory T cells (Tregs) might have important roles. Tregs are a type of T cell that secretes transforming growth factor (TGF)-β and interleukin (IL)-10 and functions in an anti-inflammatory manner. However, Tregs have been reported to be predominantly decreased in the acute phase of KD.26 Additionally, the effects of breast milk on the microbiota and Tregs have been reported, and are described below. Breast milk stimulates the proliferation of a well-balanced and diverse microbiota, which initially influences a switch from an intrauterine Th2 predominant to a Th1/Th2 balanced response and with activation of Tregs.27 The anti-infective effect of secreted IgA, lactoferrin, and defensin in breast milk inhibits pathogens and further contributes to microbiota composition.27,28 Furthermore, short-chain fatty acids in breast milk and those produced by the gut microbiota activate receptors on Tregs,27 and microRNAs (miRNAs) including miR-155, which are abundant in human breast milk, might play an important role in regulating thymic Treg development.29 Anti-infective effects and positive effects on the gut microbiota of breast milk have also been observed clinically in preterm infants.16,30 In the present study, both non-exclusively breastfed term infants and exclusively breastfed preterm infants had a somewhat elevated risk of developing KD, but these increases were not significant. When preterm birth and non-exclusive breastfeeding overlapped, however, the risk of KD was significantly increased. The above-mentioned items might be associated with the highest risk of developing KD in the preterm and non-exclusive breastfeeding group.
In addition to breastfeeding, mode of delivery (vaginal birth vs. cesarean section),31 maternal antibiotic use during pregnancy,32 and antibiotic use for infant33 could also affect the gut microbiota. Unfortunately, information on the mode of delivery was not available in this study, so it could not be examined. The effect of the mode of delivery, which may be related to preterm birth, is a subject for future research. Furthermore, the relationship between prior antibiotic use and morbidity of KD was recently reported by Fukazawa et al. and that is very interesting, including the relationship with gut microbiota.34 Though the present study did not provide information on the use of antibiotics in mothers and infants, these are also important issues for future research, given that preterm infants are often exposed to antibiotics.
The main strength of this study is that we used a large, nationally representative cohort of Japanese children. Thus, the number of KD cases was relatively high, and we were able to examine the association between preterm birth and the development of KD stratified by feeding status. The response rate for the baseline survey was high at 88.1%, with a high follow-up rate of nearly 70% for survey six. We were also able to adjust for a wide range of potential confounding factors due to child and parental factors. The breastfeeding information was also accurate because the parents were asked about feeding practices when their infant was 6–7 months of age, and almost all parents kept a record of breastfeeding in the Maternal and Child Health Handbook, which is distributed under Japanese law.16,35 However, the effects of continued breastfeeding beyond 6–7 months of age have not been evaluated.
Conversely, we cannot exclude the possibility of misclassification of hospital admission for KD because of the subjective nature of the questions that are used to assess this outcome. We could not directly confirm the admission by direct communication with hospitals because the data set that was obtained from the Ministry was anonymized. However, the diagnostic criteria for KD in Japan have not changed from 2002 to 2019,36 so the diagnostic methods that were used by physicians during the study period are likely to be similar across the country. It is also likely that most KD patients were hospitalized under the Japanese health insurance system.
In conclusion, we found that preterm birth was a significant risk for the development of KD from 6 to 66 months of age in children, using data from a nationwide longitudinal study in Japan, where KD is prevalent. Preterm infants without exclusive breastfeeding had a greater risk of developing KD compared to term infants with exclusive breastfeeding. There are positive effects of breastfeeding on child health and development, and exclusive breastfeeding is also highly recommended for preterm infants from the perspective of preventing KD. Further studies are required to determine the association between gut microbiota and the risk of KD, especially in preterm infants.
References
Uehara, R. & Belay, E. D. Epidemiology of Kawasaki disease in Asia, Europe, and the United States. J. Epidemiol. 22, 79–85 (2012).
Holman, R. C. et al. Racial/ethnic differences in the incidence of Kawasaki syndrome among children in Hawaii. Hawaii Med. J. 69, 194–197 (2010).
Onouchi, Y. et al. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nat. Genet. 40, 35–42 (2008).
Onouchi, Y. et al. Common variants in CASP3 confer susceptibility to Kawasaki disease. Hum. Mol. Genet. 19, 2898–2906 (2010).
Khor, C. C. et al. Genome-wide association study identifies FCGR2A as a susceptibility locus for Kawasaki disease. Nat. Genet. 43, 1241–1246 (2011).
Onouchi, Y. et al. A genome-wide association study identifies three new risk loci for Kawasaki disease. Nat. Genet. 44, 517–521 (2012).
Lee, Y.-C. et al. Two new susceptibility loci for Kawasaki disease identified through genome-wide association analysis. Nat. Genet. 44, 522–525 (2012).
Onouchi, Y. et al. Variations in ORAI1 gene associated with Kawasaki disease. PLoS ONE 11, e0145486 (2016).
Hara, T. et al. Kawasaki disease: a matter of innate immunity. Clin. Exp. Immunol. 186, 134–143 (2016).
Nagao, Y., Urabe, C., Nakamura, H. & Hatano, N. Predicting the characteristics of the aetiological agent for Kawasaki disease from other paediatric infectious diseases in Japan. Epidemiol. Infect. 144, 478–492 (2016).
Rowley, A. H. et al. Search for highly conserved viral and bacterial nucleic acid sequences corresponding to an etiologic agent of Kawasaki disease. Pediatr. Res. 36, 567–571 (1994).
Principi, N., Rigante, D. & Esposito, S. The role of infection in Kawasaki syndrome. J. Infect. 67, 1–10 (2013).
Galeotti, C. et al. Predisposing factors, pathogenesis and therapeutic intervention of Kawasaki disease. Drug Discov. Today 21, 1850–1857 (2016).
Kato, T. et al. Associations of preterm births with child health and development: Japanese population-based study. J. Pediatr. 163, 1578–1584.e4 (2013).
Jaakkola, J. J. K. et al. Preterm delivery and asthma: a systematic review and meta-analysis. J. Allergy Clin. Immunol. 118, 823–830 (2006).
Nakamura, K. et al. Exclusively breastfeeding modifies the adverse association of late preterm birth and gastrointestinal infection: a nationwide birth cohort study. Breastfeed. Med. 15, 509–515 (2020).
Yorifuji, T., Tsukahara, H. & Doi, H. Breastfeeding and risk of kawasaki disease: a nationwide longitudinal survey in Japan. Pediatrics. 137, e20153919 (2016).
Lusa, L. & Ahlin, Č. Restricted cubic splines for modelling periodic data. PLoS ONE 15, 1–17 (2020).
Tamai, K. et al. Associations of birth weight for gestational age with child health and neurodevelopment among term infants: a nationwide Japanese population-based study. J. Pediatr. https://doi.org/10.1016/j.jpeds.2020.06.075 (2020).
van den Berg, J. P. et al. Transplacental transport of IgG antibodies to preterm infants: a review of the literature. Early Hum. Dev. 87, 67–72 (2011).
Isayama, T. et al. Health services use by late preterm and term infants from infancy to adulthood: a meta-analysis. Pediatrics 140, e20170266 (2017).
Kaneko, K. et al. Our evolving understanding of Kawasaki disease pathogenesis: role of the gut microbiota. Front. Immunol. 11, 1616 (2020).
Chen, J. et al. Altered gut microbiota correlated with systemic inflammation in children with Kawasaki disease. Sci. Rep. 10, 14525 (2020).
Kinumaki, A. et al. Characterization of the gut microbiota of Kawasaki disease patients by metagenomic analysis. Front. Microbiol. 6, 824 (2015).
Fouhy, F. et al. Perinatal factors affect the gut microbiota up to four years after birth. Nat. Commun. 10, 1517 (2019).
Jia, S. et al. The T helper type 17/regulatory T cell imbalance in patients with acute Kawasaki disease. Clin. Exp. Immunol. 162, 131–137 (2010).
Walker, W. A. & Iyengar, R. S. Breast milk, microbiota, and intestinal immune homeostasis. Pediatr. Res. 77, 220–228 (2015).
Victora, C. G. et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 387, 475–490 (2016).
Hsu, P. S. & Nanan, R. Does breast milk nurture T lymphocytes in their cradle? Front. Pediatr. 6, 268 (2018).
Wang, Z. et al. Comparing gut microbiome in mothers’ own breast milk- and formula-fed moderate-late preterm infants. Front. Microbiol 11, 268 (2020).
Hoang, D. M., Levy, E. I. & Vandenplas, Y. The impact of caesarean section on the infant gut microbiome. Acta Paediatr. 110, 60–67 (2021).
Qu, W., Liu, L. & Miao, L. Exposure to antibiotics during pregnancy alters offspring outcomes. Expert Opin. Drug Metab. Toxicol. 6, 1–10 (2021).
Uzan-Yulzari, A. et al. Neonatal antibiotic exposure impairs child growth during the first six years of life by perturbing intestinal microbial colonization. Nat. Commun. 12, 443 (2021).
Fukazawa, M. J. et al. Previous antibiotic use and the development of Kawasaki disease: a matched pair case-control study. Pediatr. Int. 62, 1044–1048 (2020).
Yamakawa, M. et al. Long-term effects of breastfeeding on children’s hospitalization for respiratory tract infections and diarrhea in early childhood in Japan. Matern. Child Health J. 19, 1956–1965 (2015).
Committee for the Revision of the Guideline for Diagnosis of Kawasaki Disease Japanese Society of Kawasaki Disease. Guideline for Diagnosis of Kawasaki Disease 6th edn (in Japanese). http://www.jskd.jp/info/pdf/tebiki201906.pdf (2019).
Acknowledgements
This work was supported in part by a Grant for Strategies for Efficient Operation of Okayama University (grant number 2007030201). We thank Saori Irie for her help in data collection. We also thank Chris Rowthorn from eibunkousei.net (http://www.eibunkousei.net/) for editing a draft of this article.
Funding
This work was supported in part by a Grant for Strategies for Efficient Operation of Okayama University (grant number 2007030201). The sponsor had no involvement in the study design; the collection, analysis, or interpretation of the data; the writing of the report; or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
A.T. conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. N.M. conceptualized and designed the study, carried out the initial analyses, and reviewed and revised the manuscript. T.N., K.T., M.N., K.N., M.K., T.K., and H.T. conceptualized and designed the study and reviewed and revised the manuscript. T.Y. conceptualized and designed the study and critically reviewed and revised the manuscript for important intellectual content. All authors had full access to all the data in this study and accepted the responsibility to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takeuchi, A., Namba, T., Matsumoto, N. et al. Preterm birth and Kawasaki disease: a nationwide Japanese population-based study. Pediatr Res 92, 557–562 (2022). https://doi.org/10.1038/s41390-021-01780-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01780-4
This article is cited by
-
Multisystem inflammatory syndrome in 1.2 million children: longitudinal cohort study of risk factors
Pediatric Research (2024)
-
Epigenetic insights into the pathogenesis of Kawasaki disease
Pediatric Research (2022)
-
Long-term infant feeding roles in triggering uncontrolled inflammatory responses
Pediatric Research (2022)
-
Neonatal sepsis and Kawasaki disease
European Journal of Pediatrics (2022)