Abstract
Background
Neonatal neurocritical care (NNCC) is a rapidly advancing field with limited fellowship training available in locally developed, non-accredited programs. A standardized survey aimed to understand the training backgrounds of individuals practicing NNCC, the structure of existing clinical NNCC services/training programs, and suggested clinical competencies for new graduates.
Methods
We developed an anonymous survey electronically sent to members of societies related to NNCC. Using the survey results as a guide, we discuss a competence by design (CBD) curriculum as a complementary approach to traditional time-based training.
Results
There were 82 responses to the survey from 30 countries; 95% of respondents were physicians. Thirty-one (42%) institutions reported having an NNCC service, 24 (29%) individuals reported formal NNCC training, 81% reported “significant variability” across NNCC training programs, and 88% were both in favor of standardizing training programs and pursuing formal accreditation for NNCC in the next 5 years.
Conclusions
The survey results demonstrate international interest in standardizing NNCC training and development of an accreditation or certification process. We propose consideration of a CBD-type curriculum as a training approach to focus on the development of specific NNCC competencies, rather than assuming the acquisition of these competencies based on time as a surrogate.
Impact
-
Continued growth and development in the field of NNCC has led to increasing need for training programs suited to meet the diverse needs of trainees from varied backgrounds.
-
We present the results of an international survey that assessed the structure of existing training programs and the priority areas in which graduates must demonstrate competence, highlighting the combination of CBD and time-based training as one approach to address these recommendations.
-
The survey results support interest in translating published training competencies, existing expertise, and infrastructure across centers into a standardized curriculum for NNCC including certification opportunities.
Similar content being viewed by others
Background
The field of neonatal neurocritical care (NNCC) is a rapidly evolving subspecialty that has arisen in response to the increasingly complex care of newborns with neurological conditions. As training programs for physicians seeking to master the requisite skills necessary to care for these infants emerged, experts from major academic medical centers in the United States and Canada outlined “an initial framework for the standardization of training”.1 In this 2016 publication, core competencies were detailed, common fetal and neonatal neurological conditions were delineated, and options for clinical (1 year) versus academic (2–3 years) fellowship tracks were described. Given the substantive variability in training and experience of trainees entering NNCC programs (who are most commonly Child Neurologists or Neonatologists), the proposed training curriculum was designed to be flexible, providing learners with the opportunity to develop competencies not native to their own medical subspecialty (e.g., a neonatology trainee developing expertise in conventional electroencephalogram [EEG] interpretation).
Throughout the Canadian medical system, a similarly flexible training curriculum known as competence by design (CBD) is being implemented. CBD is a learner-focused, rather than a time-based, training model2,3 that has been employed by medical and surgical specialties since 2017. The fundamental intent of the CBD program is to ensure competency at each stage before progression to the next level—thus ensuring a graduated skill set. In a pure CBD system, there are no hard time allotments to progress between stages, and trainees advance at their own rate. However, a pure CBD approach, without time allocation, was not considered feasible in the Canadian healthcare system, where a trainee has key roles both as a learner and as part of the workforce.4 The Canadian system has therefore adopted a hybrid model of CBD and time-based curricula in which a trainee has scheduled rotations with specific time allocations, but a newly heightened focus on developing competencies that are no longer assumed using time as a surrogate. Thus, while the trainee has a set schedule of rotations, thereby helping fulfill their contributions as part of the workforce, they also have well-delineated and relevant learning goals that are assessed through frequently targeted feedback.
Here, we consider the implementation of CBD principles to NNCC training as they apply to the results of an international survey. The survey assessed the training background of individuals currently practicing NNCC, the curriculum design of existing NNCC training programs, and priority areas for the competency of graduating trainees. In the context of the growing number of clinical and training programs in this field, we also assessed views regarding the need for standardizing NNCC training and working towards certification in this expanding field.
Methods
Study participants
The goal of the survey was to collect information from an international audience of physicians and allied care professionals involved in NNCC across a wide range of backgrounds, including those who represent major academic institutions as well as clinicians from non-academic centers.
Survey development
A REDCap survey was designed (Supplementary Appendix A). The survey consisted of 26 questions, with the first question as the waiver of consent and the next asking the country of practice and institution name to permit elimination of duplicate responses for certain analyses. Also included in the general profile questions were the participant role (e.g., physician or nurse practitioner), number of level III/IV beds in the neonatal intensive care unit (NICU), and estimated frequency of common neonatal neurological issues.
Subsequent questions assessed the training background of the participant and whether the participant’s institution had either an NNCC service and/or a training program. If so, detailed questions were asked about the program structure, size, and a number of trainees. One specific question listed core competencies of an NNCC program as outlined by Smyser et al.1 and asked respondents to identify which core elements were priorities (respondents were permitted to check all that apply). There was also an option to write in other priorities not already listed. Detailed personal demographic information was not collected from respondents in order to protect anonymity. There were multiple opportunities for respondents to provide free-text responses. The focus areas of the survey were developed as areas of interest by the authors.
Survey implementation
In order to include a broad, comprehensive group of NNCC-focused providers, including trainees and program graduates, the survey was sent to all members of the Newborn Brain Society (www.newbornbrainsociety.org), the NNCC Special Interest Group listserve (www.NNCC-SIG.org), the European Society of Pediatric Neurology, British Pediatric Neurology Society, and the British Association of Perinatal Medicine, all societies in this field to which the authors had access. The survey was conducted over 1 month from June 2020 to July 2020. Reminder e-mails were sent twice to participants at weekly intervals. The Institutional Review Board at Maine Medical Center approved the study.
Analysis
We analyzed the surveys by describing the frequency of responses by country (dividing the USA and Canada apart from the other countries) and presented data about the size of the NICU and conditions treated using the median and interquartile range for non-normally distributed data. In order to eliminate duplicate entries for institution-specific analyses reported in Table 1, only one survey per institution was analyzed. Surveys were selected on the basis of having the most complete information. All responses, including duplicates from institutions, were analyzed for results presented in Table 2, which details the background of the respondents.
Results
A total of 88 individuals initiated the survey, with 82 (93%) completing all questions. Fifty percent of responses were from North American countries; 31 within the United States representing 27 institutions, 11 from Canada representing 8 institutions, and 2 from Mexico representing 2 institutions. The other half of the responses came from the following regions: Europe, Middle East, South and East Asia, South America, Australia, and Africa (Table 1). Across all respondents, the median NICU size was 40 beds (interquartile range (IQR) 16, 59). The median number of beds was larger in NICUs in the United States and Canada and, annually, there were greater numbers of patients with common neurologic conditions cared for in the United States and Canada (Table 1).
A total of 31 (42%) institutions reported having an NNCC service, most of which employ a consult service model (81%). The majority (61%) have been in place for more than 5 years (Table 1). The description of consult services varied widely, ranging from providers that regularly meet to discuss neonatal neurology cases, to named and dedicated services with defined inclusion criteria and specialized teams of nurses, nurse practitioners, physicians, and other providers in the acute and follow-up phases of care. Outside the United States and Canada, more services (42%) utilized a model of care in which an NNCC service had assigned beds on a floor with a designated physician of record as opposed to a consulting provider model.
Physicians (n = 76, 93%) comprised the majority of respondents, with additional responses from three trainees, two nurses, and one nurse practitioner (Table 2). A minority, 24 (29%), reported having formal specialized training in NNCC (defined as training beyond elective rotations), with another 4 (5%) describing informal training. Of the 24 who reported additional training in NNCC, 25% had one additional year of training, 17% had 2 years, and the remainder had wide-ranging amounts of training. Examples of additional training described by respondents in free-text included a 1-month visiting rotation, sabbaticals, completing an NNCC-related M.S. or Ph.D. degree, and “lifelong dedication to the field.” Seven (29%) of the 24 respondents with additional training indicated that they came from a Child Neurology background, 13 (54%) from a Neonatology background, and four (17%) from a combined background.
In terms of key competencies, most respondents agreed with the importance of teaching skills such as an age-appropriate neurological exam and developing skills in neuroimaging and EEG interpretation (Table 2). However, only 54% felt that research and quality improvement training were core competencies. Additional recommendations from open-ended responses highlighted the additional areas of focus; interpretation and application of near-infrared spectroscopy (NIRS), trimester-specific fetal neurology, neurodevelopmental follow-up, accessing cerebrospinal fluid reservoirs in neonates with hydrocephalus, performing and assessing head ultrasounds including additional acoustic windows, and diagnosis and treatment of molecular and metabolic diseases.
The majority of respondents (50/62, 81%) reported that there is “significant variability” across NNCC training programs and were in favor of standardizing training programs for NNCC (66/75, 88%). Sixty-six (88%) of 75 respondents indicated that pursuing formal accreditation for NNCC in the next 5 years was an important goal.
Only 14 (17%) of the 82 respondents reported having an NNCC training program. These responses reflected nine individual programs in four countries. Five (56%) of these programs have existed for <5 years, with the other four (44%) existing for >5 years. These programs are funded by a variety of mechanisms, including research monies, philanthropy, grants, endowments or foundation funds, transport funds, or were “self-funded” by the applicant. Amongst the respondents with formalized programs, they had trained a median of four trainees (IQR 2, 6) since the start of their programs, and most programs (n = 6) offer 1 year of training with a few supporting additional optional years. Scholarly activity was required by five programs (56%), with abstracts and manuscripts most often cited as the expected product. Trainees were split between Neonatology and Child Neurology backgrounds. Three programs (33%) provide a traditional time-based approach to training, while six (66%) tailor training based on trainee goals while maintaining core requirements.
Discussion
In this survey of physicians and allied health professionals with interest in NNCC from around the world, the vast majority of respondents favored standardizing NNCC training programs and supported pursuing certification for NNCC training programs in the next 5 years. Importantly, we found that less than one-third of respondents have had formal training in NNCC, an anticipated rate given the nascent state of the field. Further, there were only nine NNCC training programs captured in the survey, and the mechanisms of funding trainees across these programs appear tenuous, with the majority of positions funded in potentially non-sustainable ways (e.g., research, neonatal transport program fund, or self-funding). These findings demonstrate a need for more structured, sustainable training opportunities.
The core competencies for NNCC training proposed by Smyser et al.1 were supported by the majority of respondents, with suggestions for additional competencies including acquiring specific knowledge and technical skills (e.g., applying and interpreting NIRS, accessing cerebrospinal fluid reservoirs). Surprisingly, one area with comparatively less enthusiasm was scholarly activity, with slightly more than half of the respondents indicating that scholarly activity should be required. The differing amounts of support for this specific core competency may reflect the academic or clinical background of the individual responding or could be indicative of the need to limit training to 1 year due to competing priorities and/or limitations in funding. Alternatively, some respondents may recognize the importance of NNCC training as a mechanism to broadly improve the clinical care of neonates with neurologic complications, with the subsequent primary goal to prepare trainees to provide this new standard of clinical care to patient populations in need. Regardless, this highlights the need for innovative curriculum designs that support flexibility for a trainee to pursue different career paths (e.g., clinical, academic, or mixed).
Smyser et al.1 acknowledged this need for flexibility; a 1-year fellowship was suggested for trainees pursuing clinical training alone versus a 2- to 3-year fellowship for trainees intending to practice in an academic setting and/or who were committed to additional formal training in research, quality improvement, or other scholarly activity. Interestingly, two-thirds of the existing training programs report that they tailor their NNCC training to the specific needs of the individual trainee rather than focusing on an exclusively time-based curriculum. With the priority of achieving standardization within the next 5 years supported by more than 90% of respondents, the challenge of accomplishing certification while simultaneously achieving flexibility for individual learners will be complicated. The Canadian training experience provides an example where the CBD5, 6 model has been implemented nationally in a stepwise manner to balance this apparent tension between flexibility and standardization.
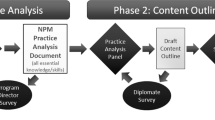
CBD curriculum development begins with experts in the field creating a consensus-based description of the scope of training requirements, similar to what was previously described by Smyser et al. for NNCC training.1 Building upon this work, training requirements are broken into a series of integrated stages beginning with the transition into a discipline followed by a foundations phase, flexible core training, and finally standardized examination and transition to autonomous practice (Fig. 1).5, 7 In order to ensure competency, trainees are provided a list of clear learning objectives known as entrustable professional activities (EPA; Table 3 outlines examples of specific skills to develop EPAs for evaluation and management of neonatal encephalopathy). The trainee is observed performing EPAs throughout their training, and these observations are documented, with constructive feedback provided in a timely fashion. A competence committee6 meets regularly to review the trainee’s online portfolio,8 and only when all the EPAs for a specific level are met, does the trainee progress to the next level of training.
Adapted from: https://www.royalcollege.ca/rcsite/documents/cbd/cbd-competence-continuum-diagram-legal-e.pdf. *Research, quality improvement, education, etc.
Implementation of this CBD model was motivated by three key issues shaping the physician role; issues that have clear application to the field of NNCC. The first was the ever-increasing complexity of medical practice and associated procedural competence within the scope of practice.5, 9 This is certainly true of NNCC, where, as an example, routine care of a neurologically compromised term neonate may include accurate identification and characterization of the infant’s neurological status and interpreting serial neurological exams, implementing therapeutic hypothermia for 72 hours, interpreting aEEG and continuous EEG monitoring, brain ultrasound, and magnetic resonance imaging (MRI) studies, and synthesizing these data for prognostication that can be clearly and empathetically communicated to traumatized parents. In many ways, the existing NNCC programs can be seen as a response to the emerging complexity of this field. As such, training and expertise may no longer be optimally achieved within the traditional, time-based curriculum of either a Child Neurology residency or Neonatology fellowship.
The second motivation for incorporation of CBD principles into NNCC training stemmed from differences in practice settings, namely academic versus non-academic. There is recognition within the Canadian system that training within a major children’s hospital may not provide all the skills needed for practice outside a quaternary-care setting.5, 9 Experts who practice outside major academic medical centers may be less likely to have routine access to the full complement of highly specialized experts across other relevant medical specialties (e.g., pediatric neurosurgery, pediatric neuroradiology, and even child neurology). An NNCC expert wishing to practice in non-quaternary settings may identify and develop competence in additional training areas, such as performing ventricular cerebrospinal fluid removal, formally reading neuroimaging studies and EEGs, or performing and interpreting cranial ultrasonography. A CBD curriculum could provide trainees with the opportunity to align their learning goals with their anticipated career path and care setting and develop skills targeted to their future work and realities of practice.
The third consideration was the societal expectation for greater physician accountability focused upon attaining a minimum standard of competence to ensure patient safety.5, 9 Currently, NNCC trainees do not have minimum subspecialty-specific competencies, and this survey indicates that the NNCC physicians around the world agree that it is time to establish these standards. These competencies are essential to this field regardless of curriculum type and may be developed from the list suggested by Smyser et al.,1 a list that was supported by the majority of survey respondents. In the immediate term, it may be feasible to incorporate NNCC CBD principles into existing child neurology or neonatology training as a way of establishing standards that will later be applicable to accredited NNCC fellowship training programs.
In addition to these relative advantages, incorporation of CBD principles into a traditional time-based model has the potential to further enrich NNCC training through its standardized incorporation of clear learning objectives (e.g., coursework for amplitude-integrated EEG, conventional EEG, head ultrasound, MRI, and Hammersmith Neonatal Neurological Examination), frequent feedback, and competence committee review. Graduates of these individualized hybrid programs would possess a clear knowledge base and focused skill set that addresses the substantial and growing field of NNCC. Trainees would also gain the requisite attitudes, ethical awareness, and communication skills critical to delivering excellent care for the neurologically compromised neonate and their family across care settings.
Strengths and limitations
While the survey was developed by a subset of authors (K.M., A.K.C., M.A.E.-D, and C.D.S.) who are experienced in NNCC, it was not a validated questionnaire. Survey respondents were generally supportive of the majority of the core competencies from the 2016 Smyser paper; however, these proposed competencies were developed by expert consensus without a formal approach. Future curricular work could benefit from a more systematic approach to developing competencies such as the modified Delphi process implemented by a group of expert psychiatrists in Canada, who developed core competencies for training in electroconvulsive therapy.10 Of note, the survey did not address the state of fetal neurology services and training opportunities as few exist. The small number of fetal neurology experts and services underscores the need for further development and consistent incorporation of fetal neurology education and training into NNCC training.
Based on the survey design, we were not able to differentiate responses from those with a Neonatology background from those with a Child Neurology or other background as fewer than 30% of respondents identified their training background in the survey. In addition, we did not collect data on the specific role of respondents; program directors may have been able to provide more detail than other respondents. While 82 of the 88 individuals who started the survey actually completed it, there is no way to know how many people may have seen the survey and decided not to initiate a response. Finally, there were only nine training programs represented in the survey, and we cannot know if these reflect the training experience and goals of other programs.
Of note, this survey aimed to assess the current state of NNCC services and training programs across an international sample of high, middle, and low-income countries in both academic and non-academic settings. A strength of this work is the international representation of responses; however, there was a greater proportion of responses from centers in North America and Europe. In this regard, the survey was limited by the fact that it was only available in English, which may have decreased international participation. Future studies could be provided in multiple languages and/or target more institutions from countries not fully represented by this survey’s responses. While beyond the scope of the survey, we also believe that it will be important to address medical inequities related to race/ethnicity, poverty, and availability of medical resources as part of future NNCC curriculum development.
Recommendations and future directions
The field of NNCC is rapidly expanding and the results of this survey suggest that further development is needed. Despite substantial clinical advances in the field, there are only limited opportunities to gain training in NNCC, and existing training programs are not standardized; a factor for which change was highly supported by respondents of the survey. Few respondents had formal training in NNCC or fetal neurology, another related field in which greater exploration of training opportunities and curriculum development could be considered. We propose CBD-based curriculum concepts as a complement to the traditional time-based teaching model used for graduate medical education in this domain. We believe the additional flexibility afforded by the CBD model is well-suited to supporting the educational needs of physicians from diverse backgrounds who choose to pursue additional training in NNCC. The survey results support the development of plans to translate the training standards proposed by Smyser and colleagues into a standardized curriculum for NNCC including certification opportunities. These future efforts should also seek to integrate NNCC within the continuum of prenatal to pediatric care in order to streamline training across specialties with the goal of improving brain health from conception through childhood.
References
Smyser, C. D. et al. Fellowship training in the emerging fields of fetal-neonatal neurology and neonatal neurocritical care. Pediatr. Neurol. 63, 39–44.e3 (2016).
Song, J. Learner-centered approaches in an international nurse training program. Contin. Educ. Nurs. J50, 183–188 (2019).
Canada TRCoPaso. Competence by Design Technical Guides and Policy (The Royal College of Physicians and Surgeons of Canada, accessed 18 November 2020); https://www.royalcollege.ca/rcsite/cbd/technical-guides-and-policy-e.
Canada TRCoPaSo C. CanMEDS Interactive Guide 2015 (The Royal College of Physicians and Surgeons of Canada, accessed 18 September 2020); http://canmeds.royalcollege.ca/guide.
Canada TRCoPaSo. What is Competence by Design? (The Royal College of Physicians and Surgeons of Canada, accessed 18 November 2020); https://www.royalcollege.ca/rcsite/cbd/what-is-cbd-e.
Canada TRCoPaSo. Competence Committees (The Royal College of Physicians and Surgeons of Canada, accessed 18 November 2020); https://www.royalcollege.ca/rcsite/cbd/assessment/competence-committees-e.
Canada TRCoPaSo. CBD Competence Continuum 2015 (The Royal College of Physicians and Surgeons of Canada, accessed 23 April 2021); https://www.royalcollege.ca/rcsite/documents/canmeds/competence-continuum-diagram-e.pdf.
Canada TRCoPaSo. ePortfolio (The Royal College of Physicians and Surgeons of Canada, accessed 18 November 2020); https://www.royalcollege.ca/rcsite/cbd/cbd-eportfolio-e.
Pinsk, M., Karpinski, J. & Carlisle, E. Introduction of competence by design to canadian nephrology postgraduate training. Can. J. Kidney Health Dis. 5, 2054358118786972 (2018).
Al-Qadhi, S. A., Chawla, T., Seabrook, J. A., Campbell, C. & Burhan, A. M. Competency by design for electroconvulsive therapy in psychiatry postgraduate training: face and content validation study. J ECT 36, 18–24 (2020).
Funding
There are no financial relationships to declare.
Author information
Authors and Affiliations
Consortia
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: A.K.C., K.M., and C.D.S. Drafting the article or revising it critically for important intellectual content: all authors. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Patient consent was not required for this study; participants consented before filling the survey.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mohammad, K., Craig, A.K., Chang, T. et al. Training in neonatal neurocritical care: a proposal for a hybrid model of competence by design and time-based methods. Pediatr Res (2021). https://doi.org/10.1038/s41390-021-01727-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-021-01727-9