Abstract
Background
The objective of this study was to describe the differences in metabolic parameters and in time to recovery from diabetes ketoacidosis (DKA), between children and adolescents with newly diagnosed diabetes compared with established type 1 diabetes (T1DM).
Methods
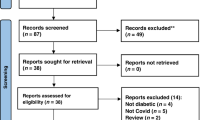
This was a single-center, retrospective study. The cohort consists of 356 children and adolescents with T1DM who had DKA during 2008–2018. Data were obtained from the patients’ medical files. Recovery of DKA was defined as the resolution of acidosis (pH >7.3 and bicarbonate >15 meq/L).
Results
The mean time to recovery from DKA was significantly longer in patients with newly diagnosed diabetes than in those with established diabetes (13± versus 8.5± h) (p < 0.001). This difference was maintained in an analysis according to DKA severity: mild, moderate, and severe. pH at presentation did not differ between the groups, but bicarbonate at presentation was significantly lower in patients with newly diagnosed diabetes than in those with established diabetes, 9.9± versus 12± mmol/L (p < 0.001). Potassium and phosphorus levels were lower, and sodium and chloride levels were higher in patients with newly diagnosed diabetes than in those with established diabetes (p < 0.001).
Conclusions
DKA is associated with a shorter recovery time in patients with established diabetes compared to newly diagnosed diabetes. This may have implications on the treatment of people with established diabetes.
Impact
-
DKA is associated with a shorter recovery time in patients with established diabetes compared with newly diagnosed diabetes.
-
Shorter recovery time in a patient with established diabetes compared with newly diagnosed diabetes was observed in any DKA severity.
-
The time to recovery from DKA did not differ significantly between patients treated with an insulin pump and those treated with multiple daily injections.
-
Triggers for DKA among patients with established diabetes were poor compliance with treatment, infection, pump dysfunction, and dehydration.
Similar content being viewed by others
Introduction
Type 1 diabetes mellitus (T1DM) is one of the most common chronic diseases in childhood. Diabetic ketoacidosis (DKA) is the leading cause of morbidity and mortality in children with T1DM1,2. DKA is characterized by the triad of hyperglycemia, acidosis, and ketosis that occurs in the presence of very low levels of effective insulin action. DKA reportedly occurs in children with established diabetes at a rate of 1–10% per patient per year3,4,5. In children and adolescents with newly diagnosed diabetes, the reported incidence has a wide range worldwide, 15–70%4,6,7,8. According to reports from different centers in Israel, the prevalence of DKA among young people with newly diagnosed T1D is 29.4–42%9,10,11. A similar prevalence of 40.6% was reported by the Israeli T1D registry12. At Schneider Children’s hospital during the last 5 years, the prevalence of DKA in new-onset diabetes was 32.–41.9%. Risk factors for DKA in individuals newly diagnosed with T1DM include younger age, delayed diagnosis, lower socioeconomic status, absence of a family history of T1DM, and residence in a country with a low prevalence of T1DM13,14,15,16. Risk factors for DKA in individuals with known diabetes include omission of insulin, females, higher glycated hemoglobin (HbA1C), lower income, limited access to medical services, unknown interruption of insulin delivery from an insulin pump, alcohol consumption, and psychiatric disorders3,4,5,17,18.
Treatment of DKA includes the administration of insulin to resolve ketosis and to reduce hyperglycemia, correction of dehydration with intravenous (IV) fluids, and correction of electrolyte abnormalities with electrolyte replacement. A range of IV fluid protocols can be safely used to rehydrate children with DKA. Neither the rate of administration nor the sodium chloride content was shown to significantly influence neurological outcomes19.
Complications of DKA include hypokalemia, hypophosphatemia, cerebral edema20, and cognitive impairment21,22. The mortality rate from DKA in children is 0.15–0.30%23,24. Cerebral edema is a possible devastating complication of DKA, carrying a 20–25% mortality rate, and remaining the leading cause of death in children with DKA25,26,27,28.
Although treatment for DKA is the same in newly diagnosed and established patients with T1DM, we hypothesized that those with established T1DM would respond faster to treatment for DKA.
Patients and methods
The current study was a single-center, retrospective study of patients who were followed at the National Center for Childhood Diabetes, Schneider Children’s Medical Center of Israel, a major tertiary hospital during the years 2008–2018. The center is the largest pediatric diabetes center in Israel and practices a holistic, multidisciplinary treatment approach. More than 1700 patients with T1DM are followed at our institute, of whom around two-thirds are treated with insulin pump therapy and the majority are using continuous glucose monitoring. We have ~130 newly diagnosed patients yearly, who were diagnosed at Schneider Children’s Medical Center or referred from other hospitals.
Patients with DKA are hospitalized in the pediatric department of the Schneider Children’s Medical Center and are treated according to a uniform protocol of DKA management. Patients with severe DKA and children younger than 2 years are hospitalized in the intensive care unit (ICU). After recovering from DKA, patients are started on subcutaneous insulin injections, as are the patients without DKA at the onset. The diabetes multidisciplinary care team (physicians, nurses, dietitians, social workers, and psychologists) deliver diabetes education to the patients and their caregivers. Patients are usually discharged within 1–3 days. The center is technology-oriented with the use of insulin pumps, continuous glucose monitoring, data uploading, and use of decision-support systems. Follow-up clinical visits are scheduled at least 4 times per year, and a physician-on-call is available 24/7 along with a multidisciplinary team.
Data for the study were obtained from patients’ medical records. The inclusion criteria were as follows: T1DM and an episode of DKA at age <18 years. Receipt of primary treatment for DKA at a different hospital was a study exclusion criterion. The diagnosis of DKA was based on pH <7.3 or bicarbonate <15 meq/L, with glucose >200 mg/dL and ketonuria24,29. The severity of DKA was defined as mild (pH <7.3–>7.2 or serum bicarbonate level >10–<15 meq/L), moderate (pH >7.1–<7.2 or serum bicarbonate level >5–<10 meq/L), or severe (pH <7.1 or serum bicarbonate level <5 meq/L). The following data were obtained from the patients’ medical files: sex, ethnic origin, age at DKA appearance, family history of diabetes, concomitant illnesses, medications, hospitalizations including in the ICU, and the results of blood tests at diagnosis of DKA. The latter included pH, bicarbonate, electrolytes, HbA1C, creatinine, and urea. In patients with known T1DM, the age at diagnosis of diabetes, type of treatment (multiple daily insulin injections or insulin pump therapy), previous episodes of DKA, and the assumed reason for DKA occurrence were also obtained.
At our center, the DKA treatment protocol is based on a clinical estimation of mild, moderate, or severe dehydration21. The fluid amount is calculated based on the daily maintenance amount plus the estimated fluid deficit, given as Nacl 0.9% over 48 h. Insulin is administered via continuous IV infusion at a rate of 0.1 U/kg/h, following an initial period of 1 h of fluid resuscitation. Potassium supplementation is added as KCl when a patient is not significantly hyperkalemic (<5 meq/L), and electrolyte levels are reassessed every 2 h. Blood gases are assessed every 4 h. Serum blood glucose is assessed hourly and dextrose is added to maintain fluids and to prevent a precipitous decline with insulin therapy (when serum levels drop <300 g/dl).
Resolution of DKA was defined as resolution of acidosis (pH >7.3 and bicarbonate >15 meq/L). In the current study, time to resolution of acidosis was defined as the time from initiation of the DKA protocol to resolution of acidosis.
Each DKA episode was analyzed separately, i.e., if a patient presented with DKA at diagnosis and then had another episode after diagnosis, it was included as two separate DKA episodes (one episode at the new-onset diabetes group and one in the group of established patients).
The study was approved by the local Institutional Review Board (0786-18-RMC).
Laboratory measurements
Standard laboratory methods were used to measure glucose and blood gases in the clinical laboratory of the Schneider Children’s Medical Centre of Israel.
Capillary HbA1C was measured using an automated immunochemical technique (DCA 2000, DCA 2000+, or DCA Vantage, utilizing the same brand of reagents, Bayer Diagnostics Inc., Tarrytown, NY; reference range: 4.3–5.8%).
Statistical analysis
The data were analyzed using the SPSS software version 2530.
Data are expressed as mean ± standard deviation (SD) for normally distributed variables and median (interquartile range) for skewed variables. Variables were compared between groups using independent t tests (for normally distributed variables), the Mann–Whitney test (for skewed variables), Pearson’s χ2 test, or Fisher’s exact test (for categorical variables). Correlations between time to recovery from acidosis and laboratory values were analyzed using Spearman’s correlation tests (all variables had a skewed distribution). Significance was set at p ≤ 0.05.
Results
A total of 356 patients met the study inclusion criteria; they experienced 405 episodes of DKA during the study period (some patients had multiple events). Of these, 243 patients were with newly diagnosed diabetes and 113 with established diabetes; 162 episodes of DKA occurred in the latter group. Patient characteristics according to the timing of DKA (at diabetes onset or during the course of diabetes) are presented in Table 1. The median age of diagnosis of T1DM was significantly lower among patients with established diabetes than among those with newly diagnosed diabetes (8.0 vs. 10.6 years, p < 0.001). The median age at the episode of DKA was significantly lower among patients with newly diagnosed diabetes than among those with established diabetes (10.6 vs. 12.8 years, p < 0.001). Statistically significant differences were not found between the groups in sex distribution and in ethnic origins (Table 1). Most of the Jewish patients were from mixed cultural background (Ashkenazi and Sephardi).
Among patients with established diabetes, 98 (60%) were treated with insulin pumps at the diagnosis of the DKA event, and the remaining patients were treated with multiple daily injections. The assumed triggers for DKA among patients with established diabetes were poor compliance with treatment, infection, pump dysfunction, and dehydration.
Sixteen (14.2%) patients with established diabetes had a family history of T1DM vs. only 11 (4.5%) of those with newly diagnosed diabetes (p < 0.001). Among those with established diabetes, the proportions with autoimmune diseases and with a family history of autoimmune diseases were higher (Table 1).
Table 2 compares the laboratory data relevant to all DKA events according to DKA timing. The median time to resolution of acidosis was significantly longer in patients with newly diagnosed diabetes: 13.0 vs. 8.5 h, p < 0.001. pH at presentation did not differ between the groups (p = 0.164, Table 2). However, compared with patients with established diabetes, among those with newly diagnosed diabetes, the median levels of bicarbonate, potassium, and phosphorus were lower, and the median levels of sodium and chloride were higher (Table 2). In addition, the urea and creatinine values were significantly higher in patients with established diabetes (p < 0.001), the statistical differences between the groups remained significant after correction for age (p < 0.001). Among the 243 patients with new-onset diabetes, 88 (36%) had mild DKA, 99 (41%) had moderate DKA, and 53 (22%) had severe DKA. Of the 162 DKA episodes among the patients with established diabetes: 79 (49%) were mild, 55 (34%) moderate, and 28 (17%) severe (p = 0.059). For each severity category, DKA recovery was shorter among those with established diabetes than with new-onset diabetes. (Fig. 1). Among patients with established diabetes, the time to recovery from DKA did not differ significantly between patients treated with an insulin pump and those treated with multiple daily injections (8.0 vs. 9.5 h, p = 0.229).
We found positive correlations of recovery time from ketosis with higher values of chloride and sodium, both in newly diagnosed diabetes patients and in patients with established diabetes. Time to recovery from ketosis was found to correlate negatively with pH at presentation, and with levels at presentation of bicarbonate, potassium, and phosphorus for both groups (Table 3).
Both pH and bicarbonate at presentation were positively correlated with lower values of phosphorus in both study groups, and with lower values of potassium among newly diagnosed patients (Table 4). Negative correlations were found of both pH and bicarbonate with higher values of chloride, sodium, and creatinine in both study groups (Table 4).
Discussion
DKA is the leading cause of increased morbidity and mortality in children with T1DM. Both patients with newly diagnosed diabetes and with established diabetes are at risk for DKA. Our study showed a longer recovery time from DKA among patients with newly diagnosed than established diabetes, even at the same level of DKA severity. This is despite the use of the same treatment protocol for the two groups. For each severity category: mild, moderate, and severe, DKA recovery was shorter among those with established than new-onset diabetes.
The occurrence of mild, moderate, and severe DKA was similar between patients with new-onset and established diabetes. pH level at DKA diagnosis did not differ as well. However, the bicarbonate level at presentation was lower among the former, probably implying a more severe dehydration. This may be explained by the lower index of suspicion in undiagnosed patients and therefore a delay in seeking healthcare. Moreover, patients with newly diagnosed diabetes in our study less often had a family history of T1DM. This could also lead to a lower index of suspicion of diabetes onset, resulting in DKA. Our patients with newly diagnosed diabetes were younger than those with established diabetes. Less developed mechanisms of metabolic compensation and lower residual beta cell function have been reported in younger patients, thus leading to more severe dehydration31,32,33. It is important to note that the mean age of DKA in patients with established diabetes is the beginning of puberty, which is a known trigger for DKA. Besides the changes in insulin sensitivity attributed to physical and hormonal changes associated with puberty, adolescence is also the time when patients start to self-manage diabetes. Adolescence is a complex period with emotional and psychological concerns that sometimes lead to unpredictable behavior with inadequate attention to diabetes care. The time of transition to self-care is an important time for the medical team to re-educate the patient in diabetes management including risks for DKA and measures to avoid it.
The shorter recovery time from DKA of patients with established diabetes may be due to a shorter duration of insulin deficiency. Patients with established T1D are aware of symptoms of DKA, which appear after a relatively short duration of insulin discontinuation, even after several hours. Furthermore, glucose and ketone measurements may lead to early detection and treatment that might lead to less severe acidosis and dehydration. In addition, people with newly diagnosed diabetes would presumably have been exposed to a longer period of insulin deficiency. Longer duration of hyperglycemia and insulin deficiency is evident from the significantly higher HbA1c among patients with newly diagnosed T1D compared with established diabetes. Prolonged hyperglycemia may cause increased insulin resistance34,35 with increased “glucose toxicity” that might in turn attribute to the longer recovery time of DKA among newly diagnosed. In addition, insulin deficiency was found to cause mitochondrial dysfunction and altered expression of mitochondrial gene transcripts, associated with impaired energy production and metabolic derangements36, which may also attribute to longer DKA recovery time after long periods of insulin deficiency. These may explain why at the same level of severity of DKA, the time to recovery was shorter among those with established diabetes.
The lower levels of phosphate and potassium at DKA in patients with newly diagnosed compared with established diabetes also imply a more severe dehydration due to osmotic diuresis27. Insulin deficiency causes potassium efflux from cells that may lead to higher potassium levels in the blood, while the cells are potassium-depleted. This effect is mediated by insulin control of the NA+/K+ ATPase regulation. On the other hand, potassium is extensively lost from the body due to osmotic diuresis and secondary hyperaldosteronism in response to intravascular volume depletion and causes increased renal potassium loss, which may be the reason for the lower potassium levels37. Another finding that concurs with the lesser dehydration among patients with established diabetes is the lack of significant correlations of pH and bicarbonate with potassium. This is because the deficit is caused by osmotic diuresis and due to aldosterone elevation.
An interesting finding of this study is the higher values of creatinine in patients with established diabetes, even after correction for age. The reasons for elevated creatinine in patients with DKA are dehydration, the presence of diabetic nephropathy, and the interference of ketoacids with the plasma creatinine assay, which can result in a falsely high plasma creatinine concentration38,39. The patients with established diabetes seemed less dehydrated (higher bicarbonate and faster recovery), so higher creatinine is more likely explained by diabetic nephropathy or falsely high creatinine. Notably, we do not have evidence for nephropathy among the included patients.
A positive correlation was found between time to recovery and a higher value of chloride during treatment. This finding is in line with other studies27, which showed that hyperchloremia may develop in children who receive a fluid replacement that contains large amounts of chloride. This can contribute to the persistent hyperchloremic metabolic acidosis and the low serum bicarbonate level.
The strengths of our study include a large number of patients and the comparison of DKA outcome in patients with new-onset diabetes and established diabetes, treated at the same center with the same protocol.
This study has a number of limitations, due in large part to the retrospective design. For example, the laboratory tests were not taken at the same point in the process of recovery from DKA.
In conclusion, we showed a shorter recovery time from DKA in patients with established diabetes compared with patients with newly diagnosed diabetes. This important finding can help clinicians plan treatment. Specifically, regardless of the severity of the DKA, clinicians can prepare for shorter IV treatment in patients with established diabetes, with the expectation of fewer complications. Children and adolescents with established T1D with any level of DKA severity are often hospitalized. The shorter recovery time might support outpatient management and avoid hospitalization in cases of uncomplicated mild-to-moderate DKA. Faster replacement with subcutaneous insulin treatment might be considered and hence avoids the need and complications that might be related to IV treatment. The next step would be to evaluate the subcutaneous treatment option in a randomized controlled study.
References
Morgan, E. et al. Mortality in type 1 diabetes diagnosed in childhood in Northern Ireland during 1989-2012: a population-based cohort study. Pediatr. Diabetes 19, 166–170 (2018).
Vicinanza, A., Messaaoui, A., Tenoutasse, S. & Dorchy, H. Diabetic ketoacidosis in children newly diagnosed with type 1 diabetes mellitus: role of demographic, clinical, and biochemical features along with genetic and immunological markers as risk factors. A 20‐year experience in a tertiary Belgian center. Pediatr. Diabetes 20, pedi.12864 (2019).
Cengiz, E. et al. Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D exchange clinic registry. Pediatr. Diabetes 14, 447–454 (2013).
Wolfsdorf, J. I. et al. Diabetic ketoacidosis and hyperglycemic hyperosmolar state: a consensus statement from the International Society for Pediatric and Adolescent Diabetes. Pediatr. Diabetes https://doi.org/10.1111/pedi.12701 (2018).
Rewers, A. et al. Predictors of acute complications in children with type 1 diabetes. JAMA 287, 2511 (2002).
Usher-Smith, J. A., Thompson, M., Ercole, A. & Walter, F. M. Variation between countries in the frequency of diabetic ketoacidosis at first presentation of type 1 diabetes in children: a systematic review. Diabetologia 55, 2878–2894 (2012).
Szypowska, A. & Skórka, A. The risk factors of ketoacidosis in children with newly diagnosed type 1 diabetes mellitus. Pediatr. Diabetes 12, 302–306 (2011).
Quinn, M., Fleischman, A., Rosner, B., Nigrin, D. J. & Wolfsdorf, J. I. Characteristics at diagnosis of type 1 diabetes in children younger than 6 years. J. Pediatr. 148, 366–371 (2006).
Eyal, O. et al. Ketoacidosis in newly diagnosed type 1 diabetes in children and adolescents in israel: prevalence and risk factors. Isr. Med. Assoc. J. 20, 100–103 (2018).
Gruber, N., Reichman, B., Lerner-Geva, L. & Pinhas-Hamiel, O. Increased risk of severe diabetic ketoacidosis among Jewish ultra-orthodox children. Acta Diabetol. 52, 365–371 (2014).
de Vries, L. et al. Decrease in frequency of ketoacidosis at diabetes onset over the past two decades - perspectives of a paediatric tertiary care centre. Diabet. Med. 29, 170–175 (2012).
Blumenfeld, O. et al. Trends in the incidence of type 1 diabetes among Jews and Arabs in Israel. Pediatr. Diabetes 15, 422–427 (2014).
Usher-Smith, J. A., Thompson, M. J., Sharp, S. J. & Walter, F. M. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ 343, d4092–d4092 (2011).
Klingensmith, G. J. et al. Diabetic ketoacidosis at diabetes onset: Still an all too common threat in youth. J. Pediatr 162, 330–4.e1 (2013).
Rewers, A. et al. Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the search for diabetes in youth study. Pediatrics 121, e1258–e1266 (2008).
Rodacki, M. et al. Ethnicity and young age influence the frequency of diabetic ketoacidosis at the onset of type 1 diabetes. Diabetes Res. Clin. Pract. 78, 259–262 (2007).
Hermann, J. M. et al. Self-reported regular alcohol consumption in adolescents and emerging adults with type 1 diabetes: a neglected risk factor for diabetic ketoacidosis? Multicenter analysis of 29 630 patients from the DPV registry. Pediatr. Diabetes 18, 817–823 (2017).
Morris, A. D. et al. Adherence to insulin treatment, glycaemic control, and ketoacidosis in insulin-dependent diabetes mellitus. The DARTS/MEMO Collaboration. Diabetes Audit and Research in Tayside Scotland. Medicines Monitoring Unit. Lancet 350, 1505–1510 (1997).
Kuppermann, N. et al. Clinical trial of fluid infusion rates for pediatric diabetic ketoacidosis. N. Engl. J. Med. 378, 2275–2287 (2018).
Glaser, N. et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N. Engl. J. Med. 344, 264–269 (2001).
Ghetti, S., Lee, J. K., Sims, C. E., Demaster, D. M. & Glaser, N. S. Diabetic ketoacidosis and memory dysfunction in children with type 1 diabetes. J. Pediatr. 156, 109–114 (2010).
Cameron, F. J. et al. Neurological consequences of diabetic ketoacidosis at initial presentation of type 1 diabetes in a prospective cohort study of children. Diabetes Care 37, 1554–1562 (2014).
Desai, D., Mehta, D., Mathias, P., Menon, G. & Schubart, U. K. Health care utilization and burden of diabetic ketoacidosis in the U.S. over the past decade: a nationwide analysis. Diabetes Care 41, 1631–1638 (2018).
Wolfsdorf, J. I. et al. Diabetic ketoacidosis and hyperglycemic hyperosmolar state: a consensus statement from the international society for pediatric and adolescent diabetes. Pediatr. Diabetes https://doi.org/10.1111/pedi.12701 (2018).
Lavoie, M. E. Management of a patient with diabetic ketoacidosis in the emergency department. Pediatr. Emerg. Care 31, 376–380 (2015).
Corwell, B., Knight, B., Olivieri, L. & Willis, G. C. Current diagnosis and treatment of hyperglycemic emergencies. Emerg. Med. Clin. N. Am. 32, 437–452 (2014).
Cashen, K. & Petersen, T. Diabetic ketoacidosis. Pediatr. Rev. 40, 412–420 (2019).
Alois, C. I. & Rizzolo, D. Diabetic ketoacidosis. J. Am. Acad. Physician Assist. 30, 20–23 (2017).
Agiostratidou, G. et al. Standardizing clinically meaningful outcome measures beyond HbA1c for type 1 diabetes: a consensus report of the American Association of Clinical Endocrinologists, the American Association of Diabetes Educators, the American Diabetes Association, the Endocrine Society, JDRF International, The Leona M. and Harry B. Helmsley Charitable Trust, the Pediatric Endocrine Society, and the T1D Exchange. Diabetes Care 40, 1622–1630 (2017).
IBM Corp. IBM SPSS Statistics for Windows, Version 25 (IBM Corp, 2017).
De Vries, L. et al. Factors associated with diabetic ketoacidosis at onset of Type 1 diabetes in children and adolescents. Diabet. Med. 30, 1360–1366 (2013).
Lee, H. J. et al. Factors associated with the presence and severity of diabetic ketoacidosis at diagnosis of type 1 diabetes in Korean children and adolescents. J. Korean Med. Sci. 32, 303–309 (2017).
Usher-Smith, J. A., Thompson, M. J., Sharp, S. J. & Walter, F. M. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ 343, p4092 (2011).
Yki-Järvinen, H., Helve, E. & Koivisto, V. A. Hyperglycemia decreases glucose uptake in type I diabetes. Diabetes 36, 892–896 (1987).
Wolosowicz, M., Lukaszuk, B. & Chabowski, A. The causes of insulin resistance in type 1 diabetes mellitus: Is there a place for quaternary prevention? Int. J. Environ. Res. Public Health 17, 1–13 (2020).
Karakelides, H. et al. Effect of insulin deprivation on muscle mitochondrial ATP production and gene transcript levels in type 1 diabetic subjects. Diabetes 56, 2683–2689 (2007).
Palmer, B. F. & Clegg, D. J. Electrolyte and acid–base disturbances in patients with diabetes mellitus. N. Engl. J. Med. 373, 548–559 (2015).
Kemperman, F. A. W. et al. The influence of ketoacids on plasma creatinine assays in diabetic ketoacidosis. J. Intern. Med. 248, 511–517 (2008).
Molitch, M. E., Rodman, E., Hirsch, C. A. & Dubinsky, E. Spurious serum creatinine elevations in ketoacidosis. Ann. Intern. Med. 93, 280–281 (1980).
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study design and methods and advised on analysis or interpretation of the data. K.S.-Z. collected the data and wrote the first draft of the manuscript. All the authors commented and revised the manuscript and approved the submitted version. M.Y.-G. performed the statistical analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The study was approved by the local Institutional Review Board (0786-18-RMC). This was a retrospective study, and no patient consent was required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smuel-Zilberberg, K., Shalitin, S., Yackobovitch-Gavan, M. et al. Diabetes ketoacidosis recovery in youth with newly diagnosed and established type 1 diabetes. Pediatr Res 91, 1272–1277 (2022). https://doi.org/10.1038/s41390-021-01618-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01618-z




 ) represent the mean.
) represent the mean.