Abstract
Background
Hypovitaminosis D is a common health problem. The purpose of this study was to investigate the inter-relationship between serum 25(OH)D levels and paternal and maternal vitamin D status in a sample of snoring children.
Methods
We selected 137 participants for whom serum 25(OH)D had been measured and underwent overnight polysomnography evaluation. Serum glucose, lipids, liver enzymes, parathyroid hormone, insulin, and glycated hemoglobin were also measured. Glucose and insulin levels were used to estimate insulin resistance with the homeostasis model assessment (HOMA-IR).
Results
Vitamin D insufficiency (<30 ng/mL) and deficiency (<20 ng/mL) were found in 40.9 and 17.5% of children, respectively. After adjustments for age, BMI z-score and seasonality, the odds ratio for risk of vitamin D insufficiency according to the vitamin D status of parents were: OR (95% CI): paternal insufficiency 15.1 (2.7–35.7), p = 0.002; maternal insufficiency 7.2 (2.4–22), p = 0.001. When children with vitamin D deficiency were analyzed separately, serum 25(OH)D concentration was found to be associated with the apnea–hypopnea index (r = −0.647, p = 0.009) and respiratory arousal index (r = −0.669, p = 0.034).
Conclusions
Family patterns of vitamin D could be helpful for the early identification of children at risk of metabolic and/or sleep disturbances and when considering strategies to improve vitamin D status.
Impact
-
Family patterns of vitamin D could be helpful for the early identification of snoring children at risk of metabolic and/or sleep disturbances.
-
Significant associations were found between serum 25-hydroxyvitamin D (25(OH)D) concentrations in children and their parents.
-
An inverse association between 25(OH)D levels and OSA severity was detected in deficient vitamin D children.
-
Children with insufficient and deficient vitamin D status tended to have a worse metabolic profile, so strategies are needed to improve vitamin D status.
Similar content being viewed by others
Introduction
The vitamin D endocrine system regulates a very large number of genes in many cells and tissues not related to calcium homeostasis, and increasing evidence is accumulating that this vitamin also has important extra-skeletal effects.1 Vitamin D is essential for an appropriately responsive immune system, and low 25-hydroxyvitamin D (25(OH)D) levels increase the risk of diabetes, cancer, and cardiovascular diseases.2,3,4 Additionally, vitamin D has been suggested to play a potential role in brain development and sleep–wake cycle modulation.3
Hypovitaminosis D in childhood is a re-emerging public health problem in the developed countries.4,5 There is evidence for the role of obesity as a risk factor for vitamin D insufficiency. Furthermore, previous studies conducted with children suggested a relationship between low levels of 25(OH)D and a range of medical conditions, including an increased risk of metabolic complications and sleep disturbances.6,7
Lifestyle habits and genetic determinants, in a variable combination, affect vitamin D status and the risk of hypovitaminosis D in children.4 In this context, it has been suggested that the vitamin D status of family members may be correlated, due to shared genetics and environmental factors.8,9
The identification of vitamin D status as a multidimensional biomarker of health among the pediatric population could contribute to the establishment of early nutritional and therapeutic strategies. The aim of the present study was to investigate the inter-relationship between serum 25(OH)D levels and (1) metabolic profiles, (2) sleep parameters, and (3) paternal and maternal vitamin D status in a sample of snoring children referred to a sleep unit.
Methods
This study was conducted from January 2015 to December 2018 as part of the Familial Longitudinal Obstructive Sleep Apnea study.
For the present investigation, we selected children aged from 3 to 14 years and their parents for whom serum 25(OH)D had been measured.
Children with a chronic disease (except for asthma or well-controlled rhinitis) and genetic syndromes, as well as those under medications potentially affecting sleep or vitamin D metabolism or who were using vitamin D supplements, were excluded, along with patients with missing data. Parents signed the informed consent, completed a demographic and medical questionnaire for their child, and were invited to participate in the study. In adulthood, exclusion criteria were the presence of chronic disease, taking medications that would affect sleep or nocturnal respiration, or using vitamin D supplements. The study was evaluated and approved by the Ethics Committee of our institution (IB 2136/13).
Parents completed a demographic questionnaire for their child, which included age, sex, and ethnicity. Anthropometric data were recorded for each participant: height and weight were measured and body mass index (BMI) was calculated. Children’s BMI z-score was calculated using sex-specific growth references.10
Sleep study
All children underwent overnight polysomnography evaluation (Grael, Compumedics, Abbotsford, Australia) at the multidisciplinary Sleep Unit in our hospital, following the American Academy of Sleep Medicine guidelines. Up to six encephalogram channels were studied, as well as chin and anterior tibial electromyogram, bilateral electro-oculogram, heart rate by electrocardiogram, airflow monitoring by nasal pressure transducer and oronasal thermistor, and chest and abdominal wall movement by respiratory inductance plethysmography. Transcutaneous measurement of arterial oxygen saturation was performed by pulse oximetry. All sleep studies were analyzed by the same two experts, according to pediatric-age validated criteria. Apnea was defined as a decrease in nasal flow ≥90% in at least two respiratory cycles. Hypopnea was defined as a decrease ≥30% followed by an arousal in electroencephalogram or oxygen desaturation >3%. The apnea–hypopnea index (AHI) was calculated by adding the number of apneas and hypopneas, divided by hours of sleep. An AHI ≥1 was classified as obstructive sleep apnea (OSA).11,12
Metabolic measurements
A fasting blood sample was collected from each family member.
Serum levels of glucose, lipids (triglycerides, total cholesterol, and high-density lipoprotein cholesterol (HDL)) and liver enzymes (gamma glutamyl transferase (GGT), alanine transaminase (ALT), and aspartate transaminase (AST)) were measured using the Architect c16000 platform (Abbott Diagnostics, Lake Forest, IL). The intra- and inter-assay coefficients of variation (CVs) were: glucose, 1.2 and 1.6%; triglycerides, 1 and 1.3%; total cholesterol, 0.8 and 1.2%; HDL, 1.4 and 2%; GGT, 1.5 and 1.6%, ALT, 3.1 and 3.3%; and AST, 2.2 and 2.4%, respectively. Low-density lipoprotein cholesterol was calculated using the Friedewald equation. Serum parathyroid hormone (PTH) and insulin levels were measured by electro-chemiluminescence on the Cobas e411 platform (Roche Diagnostics, Germany). The intra- and inter-assay CVs were: PTH, 1.8 and 3%; insulin, 2.2 and 4.1%, respectively. Glucose and insulin levels were used to estimate insulin resistance with the homeostasis model assessment (HOMA-IR).13
25(OH)D levels were measured by the Architect chemiluminescence immunoassay (Abbott Diagnostics, Lake Forest, IL) with an intra- and inter-assay CVs of 3.2 and 4.6 %, respectively.
Serum vitamin D status was categorized as follows according to the Endocrine Society definition: deficiency (serum 25(OH)D <20 ng/mL); insufficiency (serum 25(OH)D between 20 and 29 ng/mL), and sufficiency (serum 25(OH)D ≥30 ng/mL).14
The date of the 25(OH)D measurement served to classify seasonality: winter, December 21 to March 21; spring, March 21 to June 21; summer, June 21 to September 21; fall, September 21 to December 21.
Statistical analysis
A descriptive analysis was performed by calculating absolute and relative frequencies for qualitative variables. Mean and standard deviation or median and interquartile range were used for the quantitative parameters. Variable normality was assessed using Kolmogorov–Smirnov test. For mean comparison, variables that were normally distributed were compared between the three groups using analysis of variance. A Student’s t test was used when appropriate. Otherwise, non-parametric tests were applied. Chi-squared analyses were used to compare categorical variables. Spearman’s correlation analyses were conducted to examine potential associations between serum concentrations of 25(OH)D and anthropometric data, metabolic profiles, and sleep parameters. Correlations of serum concentrations of 25(OH)D were estimated between mothers and children, between fathers and children, and between mothers and fathers. Multivariate regression models were used to assess significant associations in bivariate analysis adjusting for age, sex, BMI z-score, and seasonality. A p value <0.05 was considered statistically significant. All data were processed and analyzed using SPSS v. 20.0 (IBM, NY).
Results
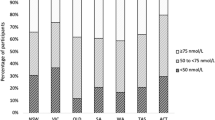
Serum 25(OH)D was measured in a total of 137 Caucasian families (children and their parents). Table 1 illustrates the distribution of the children’s characteristics according to vitamin D status. Vitamin D insufficiency and deficiency were found in 40.9 and 17.5% of study subjects, respectively. There were no significant differences in age, sex, BMI, or BMI z-score between groups. Compared with 25(OH)D sufficient children, those with 25(OH)D deficiency showed significantly higher insulin, HOMA-IR, GGT, and PTH levels. In addition, arousal index and triglyceride levels in the deficient group were significantly higher than in the insufficient group.
Table 2 provides the paternal and maternal characteristics among the children studied. The prevalence of vitamin D insufficiency varied significantly by vitamin D status of children and was greater in parents whose children had vitamin D insufficiency: overall in 64.9% of fathers and 63.2% of mothers. A significant association was found between serum 25(OH)D levels in parents and in their children (Fig. 1).
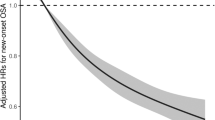
The lowest levels of 25(OH)D were observed during the winter months: children (winter: 24 ± 6 ng/mL, spring: 28 ± 9 ng/mL, summer: 35 ± 12 ng/mL, autumn: 29 ± 8 ng/mL, p = 0.003); parents (winter: 23 ± 6 ng/mL, spring: 27 ± 6, summer: 30 ± 10 ng/mL, autumn: 25 ± 9 ng/mL, p = 0.03). The odds ratios for the presence of vitamin D insufficiency in children according to parental vitamin D status are presented in Table 3. In addition, a positive association was observed between fathers and mothers (r = 0.402, p = 0.02). Table 4 summarizes the bivariate associations of 25(OH)D with anthropometric data, metabolic profiles, and sleep parameters. An inverse correlation was observed between 25(OH)D levels and HOMA index and GGT levels in the total sample of children. However, in stepwise linear multivariate regression, these associations did not remain significant after adjusting for covariates (age, BMI z-score, and seasonality). When children with vitamin D deficiency were analyzed separately, serum 25(OH)D concentration was found to be associated with AHI and respiratory arousal index (Table 5).
Discussion
This study shows significant associations between serum 25(OH)D concentrations in snoring children and their parents. Children with insufficient and deficient vitamin D status tend to have a worse metabolic profile, and an inverse association between serum levels of 25OH)D and the AHI and respiratory arousal index was observed in children with vitamin D deficiency. Overall, our results suggest that hypovitaminosis D is associated with an increase in the number of metabolic and sleep disturbances among children and their parents. Familial status of vitamin D could be used as an indicator for the early identification of children at risk of unhealthy sleep and/or metabolic complications.
The problem of hypovitaminosis D and its adequate supply represents an important issue in public health, and investigations on the association between vitamin D status and clinical conditions are rapidly emerging.15 Vitamin D is a key determinant of bone health during childhood and adolescence.16 Moreover, the role of vitamin D in the development of other non-skeletal diseases has reinforced the interest in the promotion of an adequate vitamin D status during pediatric age.4,17,18,19 It has been suggested that family-related factors may affect serum 25(OH)D levels.8 Although it is not fully clear, the underlying mechanisms could be genetic background and similarities in lifestyle factors in family members.20,21,22
In this study, we examined the impact of the familial relationship on vitamin D status in snoring children. Vitamin D insufficiency and deficiency were prevalent and a strong familial association of vitamin D status was found between children and parents. Children with insufficient or deficient vitamin D parents had significantly higher risk of suboptimal serum levels of 25(OH)D. Indeed, a significant relationship was detected between paternal and maternal vitamin D status. Children within a family are likely to share similar habits, hence variables related to overall health status such as type of diet, physical activity, and sunlight exposure could in part explain the familial relationship in vitamin D status.23 On the other hand, multiple processes of change and adaptation can be related to vitamin D status. Some previous studies showed an association between vitamin D status and age in both children and adults, whereas others did not.8,24 In the present study, no differences were observed in age and sex between groups. It is likely that the association between hypovitaminosis D in children and their parents may be related to a particular risk phenotype rather than one particular risk factor. In this regard, knowledge of vitamin D status within families would be helpful when considering interventions to prevent the burden of hypovitaminosis D.
Evidence has shown the mediating role of vitamin D in the glucose metabolism.25 Additionally, pediatric overweight and obesity are also linked to hypovitaminosis D and insulin resistance.26 Consistent with previous studies, we found that children with insufficient and deficient vitamin D had a significantly higher HOMA index when compared to sufficient children. However, the association between 25(OH)D levels and HOMA index did not remain significant after adjusting for covariates. Recent investigations suggest that vitamin D deficiency impairs insulin synthesis, regardless of the presence of obesity.6 Nonetheless, there is poor evidence of direct causality, and the biological mechanisms by which vitamin D influences insulin resistance in children and adolescents remains to be unraveled.27 PTH analysis allows us to exclude the fact that adiposity might be the only cause of hypovitaminosis D. PTH is involved in calcium and phosphorus metabolism together with vitamin D. We observed a negative trend between the PTH and 25(OH)D groups, suggesting that higher PTH levels were due to compensating for the deficiency in vitamin D.17,28,29
On the other hand, vitamin D may impact the liver through an effect on insulin resistance and the metabolic syndrome, both negatively associated with vitamin D status.30 In the current study, GGT levels were higher among the insufficient and deficient vitamin D groups. GGT is considered an indicator of metabolic liver injury and elevated GGT levels have been found to be associated with the metabolic syndrome or its components in children and adolescents. Our findings contribute to support the hypothesis that this metabolic dysregulation may be augmented in children with hypovitaminosis D and that vitamin D status could be a useful measure for identifying children with worse metabolic profiles.
An inverse correlation between the AHI and respiratory arousal index and 25(OH)D concentrations was observed in children with deficient vitamin D. These results are consistent with some previous studies.31 The relationship between low levels 25(OH)D and sleep apnea could be partly explained by common risk factors, such as obesity and impaired glucose tolerance.7,32 Alternatively, it is also possible that OSA-related hypoxia might interfere with the pathways related to 25(OH)D metabolism.29 Meanwhile, several studies reported that vitamin D receptors were expressed in the brain regions that regulate the sleep–wake cycle, and emerging lines of evidence suggest a role for inadequate vitamin D in the development of symptoms of wake impairment associated with sleep disorders.33,34 Adequate sleepers tend to have a healthier lifestyle, and vitamin D could be a mediator of the extended range of associations between sleep and health outcomes.34
Overall, our results suggest that familial vitamin D status may serve as an informative, practical approach to a generally healthy lifestyle. Evidence suggests that optimal vitamin D status may be tissue dependent, with distinct thresholds for different physiological systems and clinical outcomes. A further problem is that it is not yet known how much vitamin D is required or what dosing frequency ensures an adequate circulating concentration of 25(OH)D in order to achieve a significant reduction in the different clinical outcomes. Moreover, parental characteristics have an important influence on developing the lifestyle of children, and it is estimated that about a third of the variability in serum 25(OH)D concentrations is explained by family membership.22 In this sense, previous studies suggest that it may be effective to target families rather than individuals, so as to implement interventions designed to improve vitamin D status.
Taken together, the findings of this study indicate that vitamin D status could be an effective screening method, to identify snoring children at risk of OSA and metabolic complications. According to our findings, parental vitamin D status may help to establish a more informative typology of families and to identify groups of snoring children at higher risk of OSA and may help researchers to design more effective intervention strategies and with lower cost.
Limitations
This study had some limitations. First, the sample size was relatively small, and our results need to be interpreted in the context of testing multiple hypotheses. The study design does not allow any inference about causality between vitamin D deficiency and OSA severity, so further studies are needed to determine whether snoring children in risk of developing OSA and their parents should be screened for vitamin D deficiency for preventive purposes. Second, although 25(OH)D measurements were made using standardized methods, the single measurement may have attenuated our ability to detect associations between 25(OH)D and several outcomes. Low 25(OH)D is associated with poor health behaviors and with a large number of disorders. The causative role of low 25(OH)D in many of these conditions remains unclear, and several studies suggested that free and bioavailable 25(OH)D could reflect vitamin D metabolism better than total 25(OH)D.35 Moreover, 25(OH)D was not detected by the gold standard metabolite test (liquid chromatography tandem mass spectrometry). Although our method was standardized and calibrated against the international reference material of the National Institute of Standards and Technology, a potential bias due to this reason is possible. Third, given that children were recruited from a sleep center, our findings cannot be generalized to other populations. Fourth, we did not assess the effects of dietary habits and neither did we investigate the influence of sleep-related interventions on serum 25(OH)D levels. Moreover, although we adjusted for seasonality, measures of within-participant seasonal variation in 25(OH)D concentrations were not included in our analysis, which may have influenced the outcome of this study.
Conclusions
More than a half of the snoring children tested had vitamin D insufficiency. In addition, significant associations were found between serum 25(OH)D concentrations in children and their parents. Children with insufficient and deficient vitamin D status tended to have a worse metabolic profile, and an inverse association between 25(OH)D levels and OSA severity was detected in deficient children. In summary, family patterns of vitamin D could be helpful for the early identification of snoring children at risk of metabolic and/or sleep disturbances and when considering strategies to improve vitamin D status.
References
Bouillon, R. et al. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr. Rev. https://doi.org/10.1210/er.2018-00126 (2019).
Saponaro, F., Marcocci, C. & Zucchi, R. Vitamin D status and cardiovascular outcome. J. Endocrinol. Invest. https://doi.org/10.1007/s40618-019-01057-y (2019).
McCarty, D. E., Chesson, A. L., Jain, S. K. & Marino, A. A. The link between vitamin D metabolism and sleep medicine. Sleep Med. Rev. https://doi.org/10.1016/j.smrv.2013.07.001 (2014).
Antonucci, R., Locci, C., Clemente, M. G., Chicconi, E. & Antonucci, L. Vitamin D deficiency in childhood: old lessons and current challenges. J. Pediatr. Endocrinol. Metab. https://doi.org/10.1515/jpem-2017-0391 (2018).
Chang, S. W. & Lee, H. C. Vitamin D and health - the missing vitamin in humans. Pediatr. Neonatol. https://doi.org/10.1016/j.pedneo.2019.04.007 (2019).
Moschonis, G. et al. Vitamin D insufficiency is associated with insulin resistance independently of obesity in primary schoolchildren. The healthy growth study. Pediatr. Diabetes https://doi.org/10.1111/pedi.12678 (2018).
Kheirandish-Gozal, L., Peris, E. & Gozal, D. Vitamin D levels and obstructive sleep apnoea in children. Sleep Med. https://doi.org/10.1016/j.sleep.2013.12.009 (2014).
Clemente, M. G. et al. Family-related factors may affect serum vitamin D levels. Acta Paediatr. https://doi.org/10.1111/apa.14978 (2019).
Madsen, K. H. et al. Vitamin D status and its determinants in children and adults among families in late summer in Denmark. Br. J. Nutr. https://doi.org/10.1017/S0007114514001263 (2014).
Must, A. & Anderson, S. E. Body mass index in children and adolescents: considerations for population-based applications. Int. J. Obes. https://doi.org/10.1038/sj.ijo.0803300 (2006).
Montgomery-Downs, H. E., O’Brien, L. M., Gulliver, T. E. & Gozal, D. Polysomnographic characteristics in normal preschool and early school-aged children. Pediatrics https://doi.org/10.1542/peds.2005-1067 (2006).
Iber, C., Ancoli-Israel, S., Chesson, A. & Quan, S. F. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specification (AASM, 2007).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia https://doi.org/10.1007/BF00280883 (1985).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. https://doi.org/10.1210/jc.2011-0385 (2011).
Holick, M. F. The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev. Endocr. Metab. Disord. https://doi.org/10.1007/s11154-017-9424-1 (2017).
Carpenter, T. O. et al. Rickets. Nat. Rev. Dis. Prim. https://doi.org/10.1038/nrdp.2017.101 (2017).
Cediel, G., Corvalan, C., Lopez Romaña, D., Mericq, V. & Uauy, R. Prepubertal adiposity, Vitamin D status, and insulin resistance. Pediatrics https://doi.org/10.1542/peds.2016-0076 (2016).
Denova-Gutiérrez, E. et al. Low serum vitamin D concentrations are associated with insulin resistance in Mexican children and adolescents. Nutrients https://doi.org/10.3390/nu11092109 (2019).
Wang, M. et al. Association between vitamin D status and asthma control: a meta-analysis of randomized trials. Respir Med. https://doi.org/10.1016/j.rmed.2019.02.016 (2019).
Livshits, G., Karasik, D. & Seibel, M. J. Statistical genetic analysis of plasma levels of vitamin D: familial study. Ann. Hum. Genet. https://doi.org/10.1017/S0003480099007733 (1999).
Hong, N., Lee, Y. K. & Rhee, Y. Familial clustering of vitamin D deficiency via shared environment: The Korean National Health and Nutrition Examination Survey 2008–2012. Eur. J. Clin. Nutr. https://doi.org/10.1038/s41430-018-0157-3 (2018).
Robinson, S. L., Ramirez-Zea, M., Roman, A. V. & Villamor, E. Correlates and family aggregation of Vitamin D concentrations in school-aged children and their parents in nine Mesoamerican countries. Public Health Nutr. https://doi.org/10.1017/S1368980017001616 (2017).
Yao, S. et al. Demographic, lifestyle, and genetic determinants of circulating concentrations of 25-hydroxyvitamin D and Vitamin D-binding protein in African American and European American women. Am. J. Clin. Nutr. https://doi.org/10.3945/ajcn.116.143248 (2017).
Caristia, S. et al. Vitamin D as a biomarker of ill health among the over-50s: a systematic review of cohort studies. Nutrients https://doi.org/10.3390/nu11102384 (2019).
Mayer, O. et al. Serum vitamin D status, vitamin D receptor polymorphism, and glucose homeostasis in healthy subjects. Horm. Metab. Res. https://doi.org/10.1055/s-0043-122144 (2018).
Olson, M. L., Maalouf, N. M., Oden, J. D., White, P. C. & Hutchison, M. R. Vitamin D deficiency in obese children and its relationship to glucose homeostasis. J. Clin. Endocrinol. Metab. https://doi.org/10.1210/jc.2011-1507 (2012).
Yaribeygi, H. et al. The molecular mechanisms by which vitamin D improve glucose homeostasis: a mechanistic review. Life Sci. https://doi.org/10.1016/j.lfs.2020.117305 (2020).
Asghari, G. et al. The relation between circulating levels of Vitamin D and parathyroid hormone in children and adolescents with overweight or obesity: quest for a threshold. PLoS ONE https://doi.org/10.1371/journal.pone.0225717 (2019).
Zhang, Z., Thorne, J. L. & Moore, J. B. Vitamin D and nonalcoholic fatty liver disease. Curr. Opin. Clin. Nutr. Metab. Care https://doi.org/10.1097/MCO.0000000000000605 (2019).
Salepçi, B. M. et al. The association between obstructive sleep apnea syndrome and vitamin D deficiency. Eur. Respir. J. https://doi.org/10.1183/13993003.congress-2016.pa2332 (2016).
Van Eyck, A., Eelen, Y., Van Hoorenbeeck, K. & Verhulst, S. L. Obstructive sleep apnea syndrome and vitamin D levels in obese children and adolescents. Am. J. Respir. Crit. Care Med. https://doi.org/10.1016/j.sleep.2013.12.009 (2015).
Fan, Z. et al. Independent association of vitamin D and insulin resistance in obstructive sleep apnea. Ann. Endocrinol. https://doi.org/10.1016/j.ando.2019.09.004 (2019).
Al-Shawwa, B., Ehsan, Z. & Ingram, D. G. Vitamin D and sleep in children. Sleep https://doi.org/10.1093/sleep/zsaa056.952 (2020).
Dogan-Sander, E. et al. Association of serum 25-hydroxyvitamin D concentrations with sleep phenotypes in a German community sample. PLoS ONE https://doi.org/10.1371/journal.pone.0219318 (2019).
Wang, D. et al. Distribution of free 25OHD in elderly population based on LC-MS/MS. J. Steroid Biochem. Mol. Biol. https://doi.org/10.1016/j.jsbmb.2020.105672 (2020).
Acknowledgements
This work was supported by Fondo de Investigación Sanitaria [Grant: FIS PI1302120].
Author information
Authors and Affiliations
Contributions
A.B. and J.P. conceived and designed the study. A.B., D.M.-G., J.P., M.d.l.P., A.A.-F., C.R., and J.A.P.-Z. supervised the data collection and managed the data, including quality control. M.d.l.P. and A.B. provided statistical advice on study design and analyzed the data; A.B. and A.A.-F. chaired the data oversight committee. A.B. and D.M.-G. drafted the manuscript, and all authors contributed substantially to its revision. A.B. and J.P. take responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient statement
Parents signed the informed consent of all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barceló, A., Morell-Garcia, D., Ribot, C. et al. Vitamin D as a biomarker of health in snoring children: a familial aggregation study. Pediatr Res 91, 1176–1181 (2022). https://doi.org/10.1038/s41390-021-01612-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01612-5