Abstract
Background
Afghanistan has one of the highest under-five mortality rates in South Asia, 70.4 per 1000 live births. Determinants need to be identified to reduce this rate. Knowledge of the existence of familial and community frailty will also assist in the reduction of under-five mortality.
Methods
The 2015 Afghanistan Demographic Health Survey, including 32,712 live births, was analysed. Under-five mortality was disaggregated into neonatal, post-neonatal and child mortality and piecewise traditional Cox proportional hazard, variance-corrected and frailty models were developed. All the models identified determinants and the two frailty models examined the existence of familial and community frailty for each age group.
Results
There was statistically significant evidence of community frailty. Breastfeeding status was a highly significant determinant under univariable and multivariable analysis for neonatal and post-neonatal mortality. Post-neonates of employed mothers also experienced increased mortality, particularly those whose mother worked in agriculture where the hazard ratio was 2.77 (95% CI 2.10, 3.65). Birth order 5+ was associated with increased mortality for all three age groups.
Conclusion
The Afghanistan Ministry of Public Health should identify frail communities. Support, such as daycare facilities, should be provided and early initiation of breastfeeding and breastfeeding throughout the post-neonatal period should also be encouraged.
Impact
-
The study identified determinants of neonatal, post-neonatal and child mortality.
-
The study also established the presence of community frailty with respect to under-five mortality in Afghanistan.
-
The study shows that the association of not breastfeeding and mortality is more acute in the early neonatal age group and it extends into the post-neonatal age group.
-
The study identified the association of high birth order and mortality in the neonatal, post-neonatal and child age groups in Afghanistan.
-
Policies should be implemented that encourage early initiation of breastfeeding to continue throughout the post-neonatal period and support for vulnerable families should be provided.
Similar content being viewed by others
Introduction
A global study estimated under-five deaths at 5.4 million in 2017.1 This is a huge number given that the United Nations and World Health Organization have been working on the reduction of under-five deaths for over 30 years. A number of countries in South Asia have recorded some of the highest under-five mortality rates in the world. In an effort to reduce these rates, a couple of studies conducted in the region attempted to identify determinants. Chowdhury2 identified breastfeeding status, place of residence, region of residence and previous death of a sibling as determinants in Bangladesh. Sohail and Neupane3 identified maternal age, employment status of mothers and father’s education as determinants in India and Pakistan. Identifying frail sub-groups may also aid in the reduction of under-five mortality and at least one study had this focus where community and maternal frailty were identified in Bangladesh.4
Afghanistan, a South Asian country, has some of the highest under-five mortality rates in the region. In 2015, under-five mortality and neonatal mortality were 70.4 per 1000 and 40.5 per 1000, respectively.5 The aim of the present study is to identify determinants of neonatal, post-neonatal and child mortality in Afghanistan. The determinants identified by an earlier study in Afghanistan are for neonatal mortality and included multiple gestation, larger and smaller than average birth sizes, maternal age ≤18, maternal age ≥35, and birth interval <2 years.6 Determinants of the other sub-age groups of under-five mortality, namely, post-neonatal and child mortality, also need to be identified. The study also aims to determine if there are familial and community frailty with respect to the named sub-groups. Frailty has not been previously investigated in Afghanistan.
The study is also new in investigating time-dependent variables as possible determinants of under-five mortality in Afghanistan. Knowledge of time-dependent determinants will identify the time period where the problem is most acute and provide for focused, effective and efficient use of resources in reducing under-five mortality. This investigation will therefore assist and guide healthcare planners, as they institute policies and allocate scarce resources, in their efforts to reduce under-five mortality.
Methods
Data
The 2015 Afghanistan Demographic Health Survey (AfDHS) data were analysed. The data were collected from a nationally representative sample of 25,650 households. The AfDHS involved administering a woman’s questionnaire to ever-married women, aged 15–49 years, in selected households in each province. Ever-married women who were permanent residents of the household or those who stayed over the night before were interviewed. The number of ever-married women actually interviewed was 29,461. The data were cleaned using the Stata software, where mislabeled and out of range values were identified and deleted. After cleaning, the data consisted of information on 32,712 children born during the five years before the interview.7 The final data set had missing values of less than 4% for any of the variables analysed. All analyses were done using the Stata SE 15 (Stata Corp., College Station, TX) and R.8
Independent variables
The potential determinants were identified after reviewing the literature and included breastfeeding status (not breastfed or breastfed), sex of the child (male or female), maternal age at first birth (<20, 20–29 or ≥30 years), mother’s current age group (<20, 20–29, 30–39 or 40 years+), number of births in the past 1 year (no births or one birth or more births), mother’s age at birth of child (<20, 20–29, or ≥30 years), birth order (1, 2, 3, 4 or 5+), size of child at birth (very small and small, average or very large and large), source of drinking water (piped/well/protected or open source/unprotected/others), place of delivery (institutional or non-institutional), delivery by caesarean (yes or no), mother’s education level (no education or primary and higher), father’s education (no education or primary and higher), mother’s occupation (unemployed, professional/technical/managerial/clerical, agricultural/self-employed or service/manual skilled and unskilled), father’s occupation (professional/technical/managerial/clerical, agricultural/self-employed or service/sales/manual skilled and unskilled), household wealth (poorest, poorer, middle, richer and richest), place of residence (rural or urban) and region of residence. The provinces were grouped into eight regions. Balkh, Faryab, Jawzjan, Samangan and Sar-E-Pul as the Northern region; Badakhshan, Baghlan, Kunduz and Takhar as the North Eastern region; Badghis, Farah, Ghor and Herat as the Western region; Bamyan and Daykundi as the Central Highland region; Kabul, Kapisa, Logar, Panjsher, Parwan and Wardak as the Capital region; Ghazni, Helmand, Kandahar, Nimroz, Urozgan and Zabul as the Southern region; Khost, Paktika and Paktya as the South Eastern region; and Kunarha, Laghman, Nangarhar and Nooristan as the Eastern region. Neither the effects of duration of breastfeeding nor exclusive breastfeeding on under-five mortality were investigated in the present study and breastfeeding status ‘breastfed’ included children who were breastfed for any length of time. Not breastfed children were those who were never breastfed. Breastfeeding status was measured through questions from the interview that asked if the child was ever breastfed or currently breastfeeding.
Outcome variable
Under-five mortality was disaggregated into neonatal (first 28 days), post-neonatal (between 28 days and 1 year) and child mortality (between 1 year and 5 years). The outcome variable was the survival status of the child for these three age groups. One (1) was used if the child died during the period and 0 if the child survived the period.
Univariable analysis
Mortality rates, as a percentage of live births, were calculated for each category of the independent variables. Log-rank tests were performed to identify any statistical difference between the various levels. This was done for the neonatal, post-neonatal and child age groups.
Multivariable analysis
The determinants were identified using piecewise versions of the traditional Cox proportional hazard model, two Cox variance-corrected models (clustered by family and community) and two frailty models that tested familial and community frailty. Here, familial refers to a mother and her offspring and community refers to the cluster or sample point used during the fieldwork. The survival times of individuals belonging to the same family or community may be dependent; therefore, the variance-corrected model adjusts at the inferential level for the dependency in such instances.9 The estimates for the traditional model and the variance-corrected model are usually the same. However, there is an adjustment of the confidence interval (CI) with the variance-corrected model where naive standard errors are replaced by robust sandwich type standard errors.
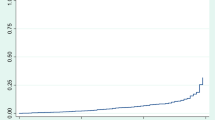
The main assumption of the Cox proportional hazard model is the assumption of proportional hazard.10 This was tested using a global Chi-square test and per-variable test using the cox.zph command in R. The Chi-square test, with one degree of freedom, tested the null hypothesis that the slopes of plots of scaled Schoenfled residuals were equal to zero. The independent variables where the null hypothesis was rejected (p value <0.05) were deemed time dependent. Log–log plots were also drawn to test the proportional hazard assumption for each independent variable.
The analytical models, used in the present study, were similarly used in a study done in India by Mani et al.,11 however, the use of the piecewise version is a major adaption. The piecewise versions catered for time-varying independent variables and involved dividing the time period into strata where the proportional hazard assumption held true for each stratum. The strata were chosen after inspection of plots of Schoenfled residuals derived from the per-variable tests.
The structure of the traditional Cox proportional piecewise model is
where ℎji (t) is the hazard for the ith child in the jth interval, h0(t) is the baseline hazard, and βj are log hazard ratios for covariates xji in the jth interval.
The structure of the variance-corrected Cox proportional hazard piecewise model is given by
where hjik(t) is the marginal hazard for the failure time of the ith child belonging to the kth mother or kth community in the jth interval. The xjik is the covariate for the ith child belonging to the kth mother or kth community, in the jth interval.
The structure of the Cox frailty piecewise models is
where hjik(t) is the hazard function for failure time for the ith child belonging to the kth mother or kth community and vk is the frailty for the kth mother or kth community. Gamma frailty was assumed, and a Chi-squared test examined the null hypothesis that the variance of frailty was equal to zero. The difference between estimates of the Cox frailty model and the estimates of the other two models is frailty.12,13,14,15,16
Model selection
The variables for each model were selected using backward elimination. A time-independent, traditional Cox proportional hazard model was first fitted with all the variables and backward elimination was performed. This involved removing each variable in turn and comparing the Akaike information criterion (AIC). The variable that resulted in the lowest AIC was permanently removed from the model. This was done until there was no further reduction in AIC. Hence the model with the lowest AIC was selected.
Assessing model fit
Model fit was assessed using likelihood ratio test (LRT), Wald test and Score (log-rank test). The AIC and concordance was also observed in assessing model fit. An examination for influential observation was also conducted. DFBETAs, which measure the difference in the estimated parameters with and without each data point, were plotted. A data point was considered an influential observation if its DFBETA was not within a ±2 threshold. A search for interactive terms was also carried out where interaction terms were added to the models and plots developed to test possible interaction between variables.
Ethical considerations
This study is based upon data made available through the Demographic Health Survey (DHS) programme with prior approval. The AfDHS 2015 received ethical approval from the ICF Institutional Review Board and the Ministry of Public Health of Afghanistan.
Results
The sampled live births for the neonatal period were 17,014 males and 15,698 females; for the post-neonatal period there were 16,570 males and 15,367 females; and, for the child age group there were 16,224 males and 15,072 females, respectively. There were 1644 deaths in total, where 775 were during the neonatal period, 641 during the post-neonatal period and 228 were child mortalities. The distribution of live births and number of deaths for the respective categories of the independent variables, for each sub-age group, are presented in Table 1.
Univariable analysis
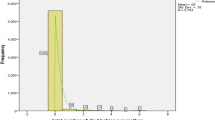
Overall, 2.37% and 2.01% of the neonates and post-neonates died, respectively. This was high when compared with the 0.73% that died from the child age group. The highest mortality rate of 29.31% of live births was observed for neonates who were not breastfed. The corresponding rates for not breastfed post-neonates and those from the child age group were 5.63% and 1.00%, respectively. The highest post-neonatal mortality and child mortality rates were found among children of mothers working in agriculture/self-employed, 7.21% and 3.11% of live births, respectively. The corresponding neonatal mortality rate for this category was 5.30% of live births (Table 1).
Multivariable analysis
The Likelihood ratio, Wald test and Score (log rank) tests all indicated that the models were better at predicting mortality than the null model. The concordance also indicated good model fit (Tables 2–4) and the AIC improved with the introduction of the piecewise models over the time-independent, traditional Cox proportional hazard model that was used during model selection. No influential data points were identified and there were no statistically significant interactions between variables. Only variables that were statistically significant for all five models, for the respective sub-age groups, were identified as determinants of neonatal, post-neonatal, and child mortality, thereby ensuring the robustness of the results. There was statistically significant evidence of community frailty for all three sub-age groups. This made the hazard ratios reported by the community frailty model, in the respective sub-age groups, more reliable and are therefore quoted in the following results.
The selected variables for the neonatal models were sex of child, mother’s age at first birth, mother’s age group, number of births in the past one year, birth order, size of child at birth, breastfeeding status, source of drinking water, place of delivery, mode of delivery, father’s education, father’s occupation and place of residence. In the post-neonatal models, sex of child, mother’s age at first birth, mother’s age group and mode of delivery got dropped even as mother’s occupation became statistically significant. The selected variables for the child models got further reduced and were: birth order, breastfeeding status and source of drinking water.
Neonatal mortality
Of all the variables, only breastfeeding status was found to be time-dependent. The piecewise model consisted of three strata: birth to 2 days, 2–6 days and 6–28 days. Not breastfeeding was associated with increased neonatal mortality in all three strata, HR 48.89 (95% CI 38.81, 61.59), 15.11 (95% CI 10.20, 22.36) and 13.44 (95% CI 8.99, 20.12), respectively. Other variables associated with increased neonatal mortality were males, HR 1.27 (95% CI 1.09, 1.48), one or more births in the past 1 year, HR 1.33 (95% CI 1.13, 1.56), mother’s age group less than 20 years, HR 1.77 (95% CI 1.17, 2.68), birth order 5+, HR 1.74 (95% CI 1.28, 2.36), very small and small births, HR 2.02 (95% CI 1.70, 2.41) and very large and large births, HR 1.66 (95% CI 1.32, 2.09), non-institutional deliveries, HR 1.35 (95% CI 1.12, 1.62) and rural place of residence, HR 1.64 (95% CI 1.28, 2.10) (Table 2).
Post-neonatal mortality
Of all the variables, breastfeeding status was found to be again time-dependent. The piecewise models consisted of two strata, 1 month to 6 months and 6 months to 1 year. There was a 20% increase in post-neonatal mortality for one or more births when compared to no births in the past year, HR 1.20 (95% CI 1.02, 1.42). Birth order 5+, HR 1.45 (95% CI 1.13, 1.90), size of child, very small and small, HR 2.23 (95% CI 1.86, 2.67), non-institutional delivery, HR 1.52 (95% CI 1.24, 1.85), mother’s occupation, professional/technical/managerial/clerical, HR 1.50 (95% CI 1.04, 2.16), agricultural/self-employed, HR 2.77 (95% CI 2.10, 3.65), service/manual skilled and unskilled, HR 1.88 (95% CI 1.30, 2.71) and rural place of residence, HR 1.41 (95% CI 1.08, 1.85) were all associated with increased post-neonatal mortality. Not breastfeeding was associated with increased post-neonatal mortality in both the strata of 1 to 6 months, HR 3.28 (95% CI 2.18, 4.95) and 6 months to 1 year, HR 3.01 (95% CI 1.40, 6.50) (Table 3).
Child mortality
There were no time-dependent variables for child mortality. Children of birth order 5+, HR 1.86 (95% CI 1.21, 2.87) and children whose source of drinking water were open source/unprotected/others, HR 1.38 (95% CI 1.03, 1.85) experienced increased child mortality (Table 4).
Discussion
Community frailty was statistically significant for the neonatal, post-neonatal and child age sub- groups. There are, therefore, unobserved factors shared by members of the same community that have a multiplicative effect on the hazard function.17 At risk communities were, however, not identified. Our study is new in suggesting that work be undertaken to identify vulnerable communities so as to improve under-five survival rates in Afghanistan. Our study also identifies determinants that are statistically significant for neonatal, post-neonatal and child mortality. It is important to note that as the child grows, the number of determinants of mortality decreases. Therefore, our study suggests that the period of up to one year is crucial for the survival of the child and additional measures must be put in place for this vulnerable population.
Not breastfeeding, particularly in the first 2 days after birth, was statistically significant for neonatal mortality. The use of the Cox piecewise model was instrumental in pinpointing this high-risk period and in so doing justifies its use in the present study. As a matter of policy early initiation of breastfeeding, on the first day or hour of life is encouraged in an effort to reduce neonatal mortality.18 However, breastfeeding was also statistically significant for post-neonatal mortality. This was also observed in a study done in the United States, by Chen and Rogan,19 where ever-breastfed children experienced a decreased risk for post-neonatal mortality. The implication here is that the benefits of breastfeeding extend beyond the neonatal period into the post-neonatal period and the child sub-age group. The present study made no attempt to establish causation with respect to breastfeeding in that underlying illnesses may have prevented breastfeeding and led to the death of the children.
Mother’s age group less than 20 years was statistically significant for increased neonatal mortality. Number of births in the past 1 year was found to be a determinant of neonatal and post-neonatal mortality. Also birth order 5+ was associated with increased neonatal, post-neonatal and child mortality. These factors may lead to increased competition for family resources and maternal depletion which may contribute to the increased mortality observed.20 Neal et al.21 in a study encompassing 45 countries found that young maternal age was associated with increased neonatal mortality. As per Neal et al., young mothers should also be exposed to educational programmes to assist and guide them in caring for their children. Small and very small birth sizes were associated with increased neonatal and post-neonatal mortality. Very large and large birth sizes were also found to be associated with increased neonatal mortality. The mother had been asked to assess the relative size of a specific child at birth. She was asked, “When (name) was born, was he/she very large, larger than average, average, smaller than average or very small?” The answer was based on maternal recall and estimation. Even though this is based on mother’s assessment, studies have found it to be a good estimate for child health along with child weight at birth.22 The results confirm an earlier study done in Afghanistan, where smaller and larger than average birth sizes were identified as determinants of neonatal mortality.6 It also concurs, in part, with a study done in Pakistan by Nisar and Dibley23 where smaller than average birth size was identified as a determinant of neonatal mortality. Males experienced increased hazard for neonatal mortality. Past studies have also reported a similar disadvantage for males. One study done by Sawyer24 found that under-five mortality was 2% higher for boys in developing countries.
The disadvantage of non-institutional delivery with respect to the neonatal and post-neonatal sub-age groups was similarly observed in a study by Rasooly et al.,25 in relation to maternal mortality. They believed that unhygienic conditions of home delivery contributed to increased maternal mortality. This was not explored in the present study, nonetheless, the explanation put forward may be plausible with respect to under-five mortality. Rural place of residence was associated with increased hazard for neonatal and post-neonatal mortality. The rural disadvantage was established by a number of studies, including a study among Greek mothers where rural place of residence was statistically significant for infant (neonatal plus post-neonatal) mortality.26 Siahanidou et al. demonstrated that the infant mortality rates were increasing in rural areas even while decreases were being observed in urban areas. A possible implication here is that policies to reduce disparities in infrastructure and amenities that support young life between urban and rural areas must be developed and implemented.
Post-neonatal children of mothers employed in all the employment categories experienced increased mortality. This was particularly evident for post-neonates of mothers employed in agriculture. Singh and Tripathi27 observed increased hazard for under-five mortality among children of mothers working in agriculture and postulated that the arduous tasks mothers have to undertake, during agricultural work, may affect mother’s health and in turn the health of the child. Mothers involved in the service and professional sectors may be likewise affected.
There were not many determinants of child mortality; however, open or unprotected source of drinking water was associated with increased hazard for this age group. The dangers of unprotected sources of water were also observed in a study by Gebretsadik and Gobreyohannes28 that analysed the 2011 Ethiopia DHS. They observed that there was a 72.7% increase in under-five mortality for children who did not have access to piped water. A possible explanation proffered by the authors is that sources of water other than piped sources, such as rivers, were contaminated and this gave rise to the increased mortality observed.28 This was not explored in the present study; however, it is a possible association that can be explored in future research.
Conclusion
The study analysed the 2015 AfDHS where under-five mortality was disaggregated into neonatal, post-neonatal and child mortality. The existence of community frailty was established therefore identifying at risk communities and providing support in terms of information, education and vital resources may assist in reducing under-five mortality. The use of the piecewise Cox models allowed for closer examination of the problem and identified areas of major concerns. Quite notably the hazard ratio was extremely high for neonates that were not breastfed in the first two days after birth. As such early initiation of breastfeeding should be encouraged and this should be continued throughout the post-neonatal period.
Recommendations
-
(1)
It is recommended that mothers be encouraged to breastfeed throughout the post-neonatal period.
-
(2)
Since mother’s age less than 20 years was a determinant of neonatal mortality, more than one birth in the past year was a determinant of neonatal and post-neonatal mortality and birth order 5+ was a determinant of neonatal, post-neonatal and child mortality, mothers who become pregnant in teenage years, or become pregnant again soon after the birth of a child and pregnancies of higher birth order should be tracked during clinical visits or via outreach programmes and resources provided for at risk families.
-
(3)
Healthcare providers need to have policies to flag birth sizes that are above or below average and institute special healthcare interventions to preserve lives.
-
(4)
The increase in post-neonatal mortality with respect to non-institutional deliveries, may be, indicative of poor healthcare choices. Post-natal visits should also be encouraged to promote better healthcare.
-
(5)
Records of maternal employment should be kept as a matter of policy and support for vulnerable families should be provided. A system of day care can also be developed to assist.
-
(6)
Increasing access to piped water will assist in reducing child mortality and hence under-five mortality.
The study presents an opportunity for policies to be implemented by the Islamic Republic of Afghanistan Ministry of Public Health that would reduce the ill effects of all the observed determinants. These strategies may reinforce, complement and build on the national health strategies 2016–2020 established by the ministry.
References
World Health Organisation. Global Health Observatory Data—Explore a World of Health Data. Child Mortality and Causes of Death. https://www.who.int/gho/child_health/mortality/mortality_under_five_text/en/ (2018).
Chowdhury, A. H. Determinants of under-five mortality in Bangladesh. Open J. Stat. 03:03, 213–219 (2013).
Sohail, H. & Neupane, S. Prevalence of and factors associated with under-5 mortality in South Asia. Int. Health 11:02, 119–127 (2018).
Khan, J. R. & Awan, N. A comprehensive analysis on child mortality and its determinants in Bangladesh using frailty models. Arch. Public Health 75:1, 75 (2017).
World Bank| Data. Mortality Rates, Neonatal (Per 1,000 Live Births)—Afghanistan. https://data.worldbank.org/indicator/SH.DYN.NMRT?locations=AF (2020).
Kibria, G. M. A. et al. Determinants of early neonatal mortality in Afghanistan: an analysis of the demographic and health survey 2015. Global. Health 14:1, 47 (2018).
Afghanistan Demographic Health Survey. https://dhsprogram.com/pubs/pdf/FR323/FR323.pdf (2015).
Therneau, T. M. CRAN—Package Survival. Survival: Survival Analysis. https://cran.r-project.org/web/packages/survival/index.html (2020).
Ezell, M. E., Land, K. C. & Cohen, L. E. Modeling multiple failure time data: a survey of variance-corrected proportional hazards models with empirical applications to arrest data. Sociol. Methodol. 33:1, 111–167 (2003).
Cox, D. R. Regression models and life-tables. J. R. Stat. Soc. Ser. B Methodol. 34:2, 187–202 (1972).
Mani, K. Determinants of under-five mortality in rural empowered action group states in India: an application of Cox frailty model. Int. J. MCH AIDS 1, 60–72 (2012).
Duchateau, L., & Janssen, P. The Frailty Model (Statistics for Biology and Health), 2008th edn (Springer, 2007).
Hougaard, P. in Analysis of Multivariate Survival Data. Statistics for Biology and Health (eds Dietz, K., Gail, M., Krickeberg, K., Tsiatis, A., & Samet, J.) (Springer, 2000).
Klein, J. P. Semiparametric estimation of random effects using the Cox model based on the EM algorithm. Biometrics 48:3, 795 (1992).
Parner, E. Asymptotic theory for the correlated gamma-frailty model. Ann. Stat. 26:1, 183–214 (1998).
Therneau, T. M., Grambsch, P. M. & Pankratz, V. S. Penalized survival models and frailty. J. Comput. Graph. Stat. 12:1, 156–175 (2003).
Gutierrez, R. G. Parametric frailty and shared frailty survival models. Stata J.: Promoting Commun. Stat. Stata 2:1, 22–44 (2002).
Mullany, L. C. et al. Breast-feeding patterns, time to initiation, and mortality risk among newborns in southern Nepal. J. Nutr. 138:3, 599–603 (2008).
Chen, A. & Rogan, W. J. Breastfeeding and the risk of postneonatal death in the United States. Pediatrics 113:5, e435–e439 (2004).
Kozuki, N. & Walker, N. Exploring the association between short/long preceding birth intervals and child mortality: using reference birth interval children of the same mother as comparison. BMC Public Health 13(Suppl 3), S6 (2013).
Neal, S., Channon, A. A. & Chintsanya, J. The impact of young maternal age at birth on neonatal mortality: evidence from 45 low and middle income countries. PLoS ONE 13:5, e0195731 (2018).
Blanc, A. N. & Wardlaw, T. Monitoring low birth weight: an evaluation of International estimates and an updated estimation procedure. Bull. World Health Organ. 83, 178–185 (2005).
Nisar, Y. B. & Dibley, M. J. Determinants of neonatal mortality in Pakistan: secondary analysis of Pakistan Demographic and Health Survey 2006–07. BMC Public Health 14, 663 (2014).
Sawyer, C. C. Child mortality estimation: estimating sex differences in childhood mortality since the 1970s. PLoS Med. 9:8, e1001287 (2012).
Rasooly, M. H. et al. Success in reducing maternal and child mortality in Afghanistan. Glob. Public Health 9(Suppl 1), S29–S42 (2014).
Siahanidou, T. et al. Disparities of infant and neonatal mortality trends in Greece during the years of economic crisis by ethnicity, place of residence and human development index: a nationwide population study. BMJ Open 9:8, e025287 (2019).
Singh, R. & Tripathi, V. Maternal factors contributing to under-five mortality at birth order 1 to 5 in India: a comprehensive multivariate study. SpringerPlus 2:1, 284 (2013).
Gebretsadik, S. & Gabreyohannes, E. Determinants of under-five mortality in high mortality regions of ethiopia: an analysis of the 2011 Ethiopia Demographic and Health Survey Data. Int. J. Popul. Res. 2, 1–7 (2016).
Acknowledgements
The research would not have been possible were it not for the assistance from my son, Dr. Ian Forde II, with the acquisition and download of the statistical software used in the analysis. All authors have met the Pediatric Research authorship requirement. Their contributions are listed below. I.A.F. contributed to the conception and design, acquisition of data, analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and the final approval of the version submitted for publication. V.T. contributed to the conception and design and interpretation of data; drafting the article or revising it critically for important intellectual content and gave final approval of the version submitted for publication. The study was self-funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
No consent was required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Forde, I.A., Tripathi, V. Determinants of neonatal, post-neonatal and child mortality in Afghanistan using frailty models. Pediatr Res 91, 991–1000 (2022). https://doi.org/10.1038/s41390-021-01527-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01527-1