Abstract
Pulmonary hypertension has emerged as a life-threatening disease in preterm infants suffering from bronchopulmonary dysplasia (BPD). Its development is closely linked to respiratory disease, as vasculogenesis and alveologenesis are closely interconnected. Once clinically significant, BPD-associated pulmonary hypertension (BPD-PH) can be challenging to manage, due to poor reversibility and multiple comorbidities frequently associated. The pulmonary vascular disease process underlying BPD-PH is the result of multiple innate and acquired factors, and emerging evidence suggests that it progressively develops since birth and, in certain instances, may begin as early as fetal life. Therefore, early recognition and intervention are of great importance in order to improve long-term outcomes. Based on the most recent knowledge of BPD-PH pathophysiology, we review state-of-the-art screening and diagnostic imaging techniques currently available, their utility for clinicians, and their applicability and limitations in this specific population. We also discuss some biochemical markers studied in humans as a possible complement to imaging for the detection of pulmonary vascular disease at its early stages and the monitoring of its progression. In the second part, we review pharmacological agents currently available for BPD-PH treatment or under preclinical investigation, and discuss their applicability, as well as possible approaches for early-stage interventions in fetuses and neonates.
Impact
-
BPD-associated PH is a complex disease involving genetic and epigenetic factors, as well as environmental exposures starting from fetal life.
-
The value of combining multiple imaging and biochemical biomarkers is emerging, but requires larger, multicenter studies for validation and diffusion.
-
Since “single-bullet” approaches have proven elusive so far, combined pharmacological regimen and cell-based therapies may represent important avenues for research leading to future cure and prevention.
Similar content being viewed by others
Introduction
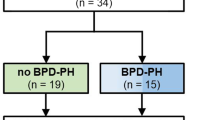
Despite major improvements in antenatal and neonatal care for preterm babies, the incidence of bronchopulmonary dysplasia (BPD) has not decreased over the 2–3 past decades1 and remains one of the most common complications of prematurity.2 The majority of BPD patients will have a favorable respiratory outcome. However, severe BPD cases (~15%) are at risk of persisting comorbidities, including chronic respiratory insufficiency and pulmonary hypertension (PH).3 BPD-related PH (BPD-PH) has emerged as a major determinant of morbidity and mortality in the first years of age.4,5 Increased pulmonary vascular resistance (PVR), the hallmark of pulmonary vascular disease (PVD), can be detected in up to 20% of extremely low birth weight infants affected with BPD6 and is correlated with BPD severity.7 Elevated PVR during the first days of life is a predictor of BPD and late PH.8 PVD significantly affects pre- and post-discharge mortality,5 with up to 50% mortality during the first 2–3 years of life in the most severe cases.4 PVD can persist and progress with time in BPD survivors. In a large prospective cohort, Levy et al.9 showed elevated PVR at 1-year corrected age in infants with BPD compared to non-BPD controls, but also in preterm compared to term infants regardless of the BPD status.
The association of PVD with BPD is not surprising, given the overlap between the alveolarization and angiogenesis processes during fetal development. Nowadays, in the surfactant era, the BPD phenotype evolved from predominantly inflammatory to a developmental disorder. This so-called “new BPD” is characterized by a disruption of alveolarization and vascularization starting with premature birth or even during fetal life, and progressing in the neonatal period as a consequence of oxidative, mechanical, infectious, and other lung injuries. These alterations of angiogenesis result in PVD, characterized by reduced capillary density, vascular wall remodeling, and altered endothelial function, all of which lead to increased PVR and, ultimately, clinical PH in the most severe cases.10 BPD-associated PVD is, therefore, a unique developmental disease, emerging in the context of lung immaturity and postnatal injuries following preterm birth. The third trimester of gestation and early postnatal period may represent a window of opportunity for intervention at its inception, potentially preventing disease progression and adverse outcomes, yet detecting PVD at its preclinical stage is challenging, if ever possible.
Available evidence regarding the PVD process derives mostly from animal studies focusing on selected aspects, due to the lack of an accurate BPD model. Antenatal disorders such as fetal growth restriction (FGR), chorioamnionitis, pulmonary hypoplasia, or congenital diaphragmatic hernia (CDH) may represent valuable proxies, but should be translated with caution to human BPD-PH. Postnatal PVD is technically more accessible for assessment, and has been studied more extensively in newborns. However, most therapeutic interventions derive from pediatric or adult research on established PH. This review will focus on recent advances in the detection of PVD and PH in extremely premature infants and potential translation into personalized therapies based on molecular mechanisms and individual determinants.
How to detect and evaluate PVD?
Several techniques have been proposed for the detection of PVD as early as possible. However, many of them derived from adult, children, or term newborn babies suffering from PH of diverse etiologies, and evidence of their validity in BPD-PH infants is still limited.
Echocardiography
Because of its limited invasiveness and its ease of use at the bedside, echocardiography represents the most practical approach for the detection of early hemodynamic alterations related to PVD, but also for ruling out anatomical defects, such as patent foramen ovale, atrial septal defects, patent ductus arteriosus (PDA), systemic pulmonary collaterals, or pulmonary vein stenosis (PVS), that can occur during or contribute to the PVD process.4,11 PVS has emerged as a significant complication in BPD patients, leading to increased mortality.12
Specific functional indices primarily developed in adult populations have been long translated to infants and neonates for the hemodynamic evaluation of PH,13 but evidence supporting their validity and significance are more limited.14,15,16,17 While more and more neonatal units use echocardiogram at the bedside and more and more parameters are emerging, their validation in the detection of PVD and grading the severity of BPD-PH is still scarce. Table 1 synthesizes current evidence for the diagnosis of PVD and PH by echocardiogram in BPD-PH patients.
Tricuspid regurgitation jet velocity (TRJV) may provide an estimation of right ventricular pressure (RVP) and thus give an indirect indication of PVR in the absence of a ductal shunt. However, this index has several limitations: first, it requires a proper transvalvular flow, lacking in as many as 85–92% of preterm infants;8,18 second, its absence does not imply the absence of PH; third, TRJV-derived RVP lacks sensitivity and specificity compared to direct systolic pulmonary arterial pressure (sPAP) measured by right heart catheterization (RHC) in chronic lung disease infants.19 Combining TRJV with classic echocardiogram parameters, such as cardiac chamber diameters, intraventricular septum (IVS) flattening, and Doppler flow direction through PDA or other shunts, improves echocardiogram sensitivity and specificity for PH diagnosis. However, in the absence of TRVJ, these conventional measurements correlate relatively poorly with the gold standard of RHC.19
Other indices commonly used in adults are increasingly studied in neonates. The eccentricity index (EI) estimates right ventricular (RV) afterload more specifically and sensitively than IVS configuration. McCrary et al.20 have demonstrated its significant correlation with BPD-PH in a cohort of preterm infants. Pulmonary artery acceleration time (PAAT) and its ratio with RV ejection time (PAAT/RVET), an accurate index of RV afterload in children,21 resulted as a valid early marker of PVD in a large cohort of 239 preterm infants.22 These findings were confirmed in another preterm cohort, showing decreased PAAT and PAAT/RVET values in the infants with PH signs by echocardiogram compared to those without.23 At a more advanced stage, elevated PVR leads to RV dysfunction, which may translate into RV and/or right atrial dilatation and altered RV contractility on echocardiogram. Multiple functional indices have been developed in order to detect and quantify RV dysfunction, such as fractional area change (FAC), tricuspid annular plane systolic excursion (TAPSE), Tissue doppler index, its derived myocardial performance index (MPI), and speckle tracking echocardiography (STE). Reference values are available in term and preterm infants for each of these indices.16,22,24,25,26,27 Fractional area change and MPI show a good correlation with BPD-PH.28,29 Low TAPSE values were associated with increased mortality in a study on late preterm/term infants with persistent pulmonary hypertension of the newborn (PPHN).30 Lower TAPSE and higher RV-MPI values were observed during the first 2 weeks of life in a subset of preterm infants with clinical evidence of PH compared to controls.31 However, larger studies are needed to validate the diagnostic and prognostic value of these indices in BPD-PH. Although it requires specific equipment, STE may be an important addition to PH evaluation as a tool for assessing myocardial strain. By analyzing the motion of speckles in two-dimensional ultrasonic image, this technique allows a non-Doppler, angle-independent, quantitative analysis of myocardial deformation, with the possibility of quantifying myocardial thickening, shortening, and rotation.32 During PH, RV dilates, hypertrophies, and develops both systolic and diastolic dysfunction.33 PH-related RV dysfunction also leads to secondary changes in left ventricular (LV) filling and performance.34,35 Extension of RV dysfunction to the LV is presumably a consequence of ventricular interdependence, including the shared septum, muscle fibers, and pericardium.36,37 STE demonstrated persistent abnormal RV and IVS strain at 1 year of age in a cohort of ex-preterm infants with BPD and PH.26 Some STE studies in infants with BPD showed the presence of a prevalent LV diastolic dysfunction,38 even though an RV-dominant pattern is expected.26,39
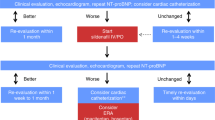
Combinations of indices have been studied and developed into protocols for the detection and grading of BPD-PH (for a review, see the PPHNet group11) However, specific scoring systems including both standard and functional parameters are still poorly developed, and do not allow yet to diagnose and establish the severity of PVD and BPD-PH accurately, especially in cases when TR is absent or shunts are present.15,19,40 Moreover, echocardiogram studies systematically assessing the responsiveness of BPD-PH patients to treatment are lacking.
The majority of published studies and clinical guidelines are based on echocardiogram assessment at 36 weeks. However, echocardiogram has the potential of detecting signs of PVD from the first days of life. In a cohort of preterm infants, PH markers at 7 days were predictive of severe BPD (RR 1.12) and late PH (14%, RR 2.85).8 In another cohort, persistent PH at 72–96 h of life was predictive of death or BPD by 36 weeks.41 Furthermore, since disruption of pulmonary development in utero represents an initial step towards PVD, antenatal identification of such risk factors could further advance the boundaries of prevention. Fetal echocardiogram is an important technique for early identification of fetuses at risk of PH, allowing fetal biometry and Doppler placental dysfunction assessment. In a large cohort of preterm infants, several antenatal factors showed a clear association with later PH development, the strongest predictors being FGR, maternal hypertension, and smoking (odds ratios 2.40, 2.11, and 2.02, respectively), each of which suggests maternal vascular underperfusion and placental dysfunction as a common pathway.42 Lio et al.43 showed that FGR 2–5 days prior to birth was associated with a fivefold increase in BPD at 36 weeks. Whether functional indices provide additional indications on nascent PVD in the fetus is still an open question. Fetal PAAT/RVET shows a correlation with lung maturity,44 development of respiratory distress syndrome (RDS),45 or pulmonary hypoplasia-related PH.46 Maternal hyperoxia test with lack of fetal pulmonary artery blood flow response is associated with neonatal PH and mortality in lung hypoplasia47 or CDH.48 Although promising, these techniques lack sensitivity and specificity that limit their clinical application49 and have not been systematically evaluated as predictors of BPD.
In summary, in the specific population of BPD-PH, echocardiogram is the more widely used noninvasive diagnostic technique. Scoring system including multiple conventional and advanced parameters, with the potential addition of other noninvasive biomarkers (see below), could improve echocardiogram effectiveness, but still need to be elaborated and validated for BPD-PH.
Cardiac catheterization
RHC remains the gold standard for accurate quantification of hemodynamic parameters in children PH, allowing direct measurement of PAP and PVR, characterization of the hemodynamic subtype (pre- and/or postcapillary), and assessing disease severity and prognosis.50 Angiography allows the identification of PVS, aortopulmonary collaterals, shunts, and left and right heart dysfunction, all significant comorbidities of BPD-PH for which early recognition is essential.51 Functional studies such as acute vasoreactivity testing yield important information on reversibility and potential response to treatment.52 PVR correlates with outcome.12,53 Although several published studies include BPD-PH patients, the specific value of RHC has not been specifically investigated in this group. RHC is often postponed and performed only in a subset of infants because of its invasiveness, technical challenges, associated risks, and lack of availability. Vascular complications, sedation-related risks, and death were reported in up to 5.3% of procedures performed <6 months.54,55 Thus, many teams restrict RHC to severe PH requiring prolonged/combined pulmonary vasodilator therapy or suspicion of cardiovascular anomalies.56 Specifically designed sheaths, catheters and guidewires, new system components and improved postprocessing,57 advanced modeling techniques (3D rotational angiography fusion imaging techniques), or MRI-guided catheterization58,59 are expected to improve feasibility and safety in neonates.
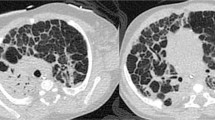
Computed tomography and magnetic resonance imaging
With its unsurpassable spatial resolution, computed tomography (CT) remains a technique of choice for anatomical assessment of respiratory and cardiovascular structures and detection of alternate causes of PH such as lung parenchymal disorders, thromboembolic disorders, or PVS.60 Conventional magnetic resonance imaging (MRI) is not well suited for lung imaging due to inherently low proton density and fast signal decay in pulmonary tissues. However, some sequences mainly based on quiet-breathing acquired (fast) gradient-echo or ultrashort-echo time have been successfully applied for BPD grading based on pulmonary density.61,62 Moreover, lung MRI may offer more information than the CT in terms of functional information through quantification of emphysematous and fibrotic interstitial remodeling,63 and follow-up of ventilation and perfusion defects through specific techniques.64 Cardiovascular magnetic resonance (CMR) in neonates remains challenging because of small size and rapid rate, requiring high temporal and spatial resolution. Traditional CMR imaging requires apnea; however, free-breathing techniques are developed. CMR could represent an interesting approach for the assessment of modifications resulting from PH as it is ideally suited for the study of ventricular morphometry and function, and vascular dimensions and flow.51 Main pulmonary artery-to-aorta ratio obtained from fast spin-echo acquisition and LV EI obtained from short-axis steady-state free precession cine images were recently described as indicators of disease severity and clinical outcome in neonates with BPD.65 MRI strain techniques (tagging, displacement encoding with stimulated echoes or tissue phase mapping) could also be applied in neonates similarly to echocardiographic STE techniques.
Biological markers
Brain natriuretic peptide (BNP) and its inactive but more stable N-terminal pro-hormone segment (NTproBNP),66 widely used in the diagnosis and monitoring of left or right cardiac failure,67,68 have emerged as useful biomarkers for early prediction and monitoring of BPD-PH.11 Several single-center observational studies showed that elevated BNP or NT-pro BNP values correlated with RV overload in neonates. Although normal ranges are not established in preterm infants, BNP or NTproBNP levels are higher in those with echocardiogram evidence of PH at or near term,69 correlate with mortality,70 and persisting PH at 1-year follow-up.71 In a retrospective cohort of children with various forms of PH, among which 62% of cases were ex-preterm infants with BPD, iterative NTproBNP values increase with PH progression and mortality.72 If BNP or NTproBNP values at birth were shown to correlate with RVP in term/near-term infants with PPHN73 or in postsurgical CDH infants,74 such evidence is lacking in preterm infants,75 possibly because of the confounding effects of PDA and LV strain.76,77
Endothelin-1 (ET-1) has been studied as a biomarker of PH in adults, showing a prognostic value for treatment response.78 A key role of ET-1 in impaired fetal angiogenesis has been demonstrated in a neonatal rat bleomycin-induced lung injury model with impaired vascular and alveolar development resembling BPD.79 In preterm infants at risk of BPD, early ET-1 measurements have yielded mixed results, as some studies have shown a correlation between plasma or tracheal ET-1 levels in the first days of life and BPD development,80,81 whereas others have shown opposite trends.82 More recently, a positive correlation was found with its more stable precursor (CTproET-1).83,84 As for today, studies evaluating the predictive value of ET-1 in the specific BPD-PH population are still lacking.
Since disrupted angiogenesis plays a key role in the early development of PVD85 and alterations of angiogenic factors correlate with placenta underperfusion86 and the development of PH in BPD patients,87 several studies have assessed the potential predictive value of angiogenesis biomarkers. Some of those, like endostatin, angiopoietin-1, vascular endothelial growth factor (VEGF), placental growth factor, or granulocyte colony-stimulating factor, seem promising.88,89 In a prospective cohort of preterm infants developing BPD-PH, cord blood biomarkers of placental maternal vascular underperfusion, individually or in combination, were shown to have a strong predictive value.86
In summary, while chemical biomarkers seem to be promising noninvasive tools in the detection of PVD, numerous gaps of knowledge remain. Future research is needed in order to establish which ones are most relevant for BPD-PH diagnosis and for early PVD detection, whether they provide added value to imaging techniques, and what is their potential for treatment responsiveness assessment.
Pharmacological approaches to PVD
The current mainstay of PH therapy aims at restoring the balance between endothelium cell-derived vasodilator and vasoconstrictor factors, which consist of the nitric oxide and prostaglandin pathways, as well as the endothelin pathway. However, therapies aimed at pulmonary vascular remodeling are increasingly developed, tested, and applied. The figure summarizes the main pathways involved and highlights several existing pharmacological compounds and cell-based therapies susceptible to target them (Fig. 1).
Vasodilator and anti-remodeling pathways are indicated with blue arrows; vaasoconstrictor and pro-remodeling pathways with red arrows. Pharmacological agents are labelled with squares (green: agonist effect; red s: antagonist effects). Molecular agents and targets are abbreviated as follows: NO nitric oxide, NOS NO synthase, l-Arg l-arginine, l-Cit l-citrulline, PGI2 prostacyclin, IP PGI2 receptor, ECE endothelin-converting enzyme, ET-1 endothelin-1, GC guanyl cyclase, GTP guanosine triphosphate, cGMP cyclic guanosine monophosphate, PDE-5 phosphodiesterase type 5, ATP adenosine triphosphate, cAMP cyclic adenosine monophosphate, AC adenyl cyclase, Ca2+ calcium ion, ETA endothelin receptor A, GP G protein-coupled receptor, IP3 inositol triphosphate, DAG diacylglycerol, PKC protein kinase C, BMP bone morphogenetic protein, TGF-β transforming growth factor beta, PDGF platelet-derived growth factor, RTK receptor tyrosine kinase, IL-6 interleukin-6, PKA protein kinase A, SMAD small body size mothers against dpp (signal transducer protein family for TGF-β), MAPK mitogen-activated protein kinases, JAK/STAT Janus kinases/signal transducer and activator of transcription, ROCK rho-associated protein kinase, CDK cyclin-dependent kinases, PPARγ peroxisome proliferator-activated receptor gamma, MMP matrix metalloproteases.
Targeting the NO/cGMP pathway
Phosphodiesterase type 5 inhibitors (Sildenafil, Tadalafil) have antiproliferative, proapoptotic, and vasodilating effects in pulmonary vasculature. In 2009, a small retrospective study in former preterm infants with established BPD-PH suggested that sildenafil led to hemodynamic improvement.90 But can early sildenafil in the first week of life prevent the development of BPD-PH in RDS infants? Small human trials published so far do not suggest any benefit, but are clearly underpowered.91,92 A large retrospective study looking at the use of sildenafil in the first month of life in infants <32 weeks, showing no difference in retinopathy of prematurity as a primary outcome, did not mention any benefit in BPD prevention either.93 Tadalafil is a longer-acting phosphodiesterase-5 (PDE-5) inhibitor approved for PH since 2009 with a similar/better efficacy and side-effect profile in children.94 Some small studies suggest that Tadalafil can be used safely in children.95,96 Tadalafil is more potent than sildenafil at reducing remodeling in vitro,97 but its use in neonatal patients is not yet established.
Animal studies have suggested a potentiality for sildenafil in restoring disrupted vascular and airway architecture in CDH fetuses.98 These finding gave way to the SToP-PH phase I/II randomized controlled trial (RCT),99 currently underway. In 2012, the STRIDER (Sildenafil Therapy In Dismal prognosis Early-onset FGR) Individual Participant Data Study Group was established with the goal of preventing FGR with sildenafil by restoring adequate uterine perfusion.100 The group published a first UK multicenter RCT in 22–29 week pregnancies, showing no difference in neonatal outcomes, including BPD,101 further confirmed in the Australia–New Zealand arm of the consortium,102 albeit with a trend toward better neonatal outcomes. However, the Dutch arm was halted due to concern over a greater incidence of PPHN in the infants of treated mothers. A smaller phase II RCT testing tadalafil in early-onset FGR started in Japan, but halted for interim safety analysis, showing a decreased antenatal and perinatal mortality, but no differences in neonatal outcomes.103
Direct stimulation of soluble guanylyl cyclase independent of endogenous NO production is a promising approach in PH, given its potential synergy with inducible nitric oxide and PDE-5 inhibitors.104 In phase III trials in adult PH patients (PATENT-1 and PATENT-2), the soluble guanylyl cyclase agonist riociguat demonstrated improvements in hemodynamics, functional class, and clinical course.105,106 Animal high-dose studies showed heart defects in the developing fetus, abortion, and fetal toxicity, especially an adverse effect on growing bone, precluding its use during pregnancy and neonates so far (http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Risk-management-plan_summary/human/002737/WC500162588.pdf). Nevertheless, in a rat BPD model, riociguat was beneficial in preventing hyperoxia-induced lung injury and PH without affecting long bone growth and structure, suggesting it may be a potential novel agent for preventing BPD and PH in neonates.107 A recent case report described the first off-label pediatric use of riociguat in a child diagnosed with severe, suprasystemic PH at 10 months, refractory to combined amlodipine, bosentan, and sildenafil, who responded well to the riociguat–bosentan combined regimen at 2 years, with no significant adverse effects.108
Targeting the endothelin pathway
There is an imbalance between endothelin and prostacyclin (PGI2) synthesis at the core of several forms of PH. Three different endothelin receptor antagonists (ERAs) are commercially available: bosentan, ambrisentan, and macitentan. Bosentan is a nonselective ERA, acting on both ET-1 receptors ETA and ETB, with vasodilator109 and anti-remodeling effects. Anecdotal use of bosentan has been described in advanced severe BPD-PH.110 Ambrisentan is an oral-selective ETA receptor antagonist with a longer half-life than bosentan.111 In an animal model of hyperoxia-induced BPD, ambrisentan reduced PH but did not prevent alveolar and vascular maldevelopment.112 Macitentan, a dual ETA with tissue-targeting properties, may have improved receptor binding capacity and fewer drug–drug interactions than bosentan.113,114 In a multicenter phase III RCT in patients ≥12 years with PH, macitentan alone or as an adjunct drug significantly reduced mortality and morbidity,115 but no systematic trials compared different ERAs nor addressed their use in infants.
Targeting the PGI2 pathway
PGI2 is a potent vasodilator in the lung and other districts, with side effects such as systemic hypotension and thrombocytopenia. PGI2 binds to the PGI2 receptor (IP), leading to Ca2+ extrusion and pulmonary arterial smooth muscle cell (PASMC) relaxation through adenyl cyclase/PKA activation and cAMP synthesis. In addition, IP reduces PASMC proliferation and migration through peroxisome proliferator-activated receptor γ (PPARγ) nuclear receptor binding.116 Epoprostenol, the synthetic equivalent of PGI2, was first approved for PH in 1995 as a continuous intravenous (IV) infusion given its very short half-life, followed by treprostinil, iloprost (2004), and epoprostenol. Despite anecdotic reports of IV epoprostenol in refractory PPHN, a 2019 Cochrane review117 failed to identify any conclusive trial supporting the use of PGI2 analogs for acute PH. A recent review of 19 studies encompassing 421 cases suggested that subcutaneous (SC) treprostinil is a valid alternative to IV PGI2 analogs and a useful adjunct therapy in children with refractory PH of various classes. SC treprostinil allowed significant clinical improvement in three case series of infants with late PH after CDH repair.118,119,120 In five extreme preterm infants with refractory BPD-PH, treprostinil leads to clinical improvement, improved RV function, and decrease of respiratory support.121 Iloprost is a PGI2 analog with a serum half-life of 20–25 min but limited IP selectivity, hence mostly administered by inhalation. Iloprost attenuated hyperoxia-induced inhibition of alveolar development and microvascular density in an animal BPD model, highlighting its potentiality for early BPD prevention.122 Conversely, oral PGI2 analogs such as treprostinil diolamine and beraprost, despite encouraging initial results in human, failed to prove the benefits so far.123,124 Selexipag is a Food and Drug Administration-approved, non-prostanoid, oral-selective IP agonist, with an established efficacy in adults with PH.125 Selexipag has a 130-fold higher selectivity compared to other IP agonists. Selexipag pediatric use was first reported in 2017 in a 12-year-old child with PH unresponsive to sildenafil plus bosentan, who showed clinical improvement after selexipag addition.126 An off-label trial on combined pulmonary vasodilators, including one former preterm infant with BPD, showed a good tolerance of the treatment and moderate hemodynamic improvement.127,128 A recent prospective observational study of the add-on, incremental selexipag in fifteen 7.4 ± 1.6-year-old children, two of whom had BPD, resulted in clinical and hemodynamic improvement in half of them, with transient side effects.129 One former preterm infant with severe chronic IUGR-related PH was reported to transition successfully from IV treprostinil to selexipag, showing sustained improvement after the switch.130 In an animal model, antenatal selexipag had the property of reversing lung vascular (but not alveolar) anomalies secondary to CDH,131 suggesting a potential applicability to human fetuses at risk for developing PH.
Targeting remodeling
Peroxisome proliferator-activated receptor γ (PPARγ) acts as a hub controlling gene induction PASMC and several other cell types. PPARγ agonists are widely used in the treatment of hyperlipidemia and diabetes. A seminal article highlighted a relationship between PH and insulin resistance and showed the potentiality of these drugs for PAH.132 The concept was consolidated in several animal PH models, showing the efficacy of rosiglitazone in preventing arterial remodeling and cardiac failure.133 In experimental CDH, antenatal rosiglitazone decreases vascular remodeling and inflammation.134 In a neonatal rat hyperoxia model, rosiglitazone prevented the alveolar changes typical of BPD.135 Given its good safety profile, including during pregnancy and its tolerability, rosiglitazone has potentialities to be repurposed as an antenatal treatment for BPD-PH prevention, yet to be clinically tested for this use.
Statins are a class of HMG-CoA (β-hydroxy β-methylbutyryl-CoA) reductase inhibitors clinically used for the reduction of plasma cholesterol levels and prevention of cardiovascular diseases, with antagonist effect on the pro-remodeling endothelin/ROCK (Rho-associated protein kinase) pathway as well as beneficial effects on endothelial function, in particular on the NO-cGMP and the VEGF pathways. Several preclinical studies demonstrated a beneficial effect of statins in the placental vasculopathy of pre-eclampsia.136 Simvastatin restored the VEGF pathway and prevented arterial remodeling in a neonatal rabbit hyperoxia model of BPD137 and prevented vascular remodeling in fetal CDH138 or hypoxia-induced PH.139 A pilot RCT of second-trimester pravastatin in 20 pregnant women suggested its efficacy in preventing pre-eclampsia without adverse maternal or fetal effects, although not providing any data on neonatal outcome.140
In the remodeling process, PASMC proliferation is governed by several growth factors, including platelet-derived growth factor, VEGF, fibroblast growth factor, and others, that exert their mitogenic signaling through multiple kinase pathways. Kinase inhibitors, such as Imatinib, have been used as anti-remodeling agents in animal models of PH.141,142 In a RCT in adult patients with advanced PH (IMatinib in Pulmonary hypertension: a Randomized Efficacy Study - IMPRES), imatinib improved exercise capacity and hemodynamics, but serious adverse events were common.143 Imatinib use was reported in one case of an infant with CDH and postsurgical refractory PH, leading to marked clinical improvement. One nonrandomized noncontrolled prospective trial of imatinib ± bevacizumab (a VEGF antagonist with anti-angiogenic properties) of 48 children 2.5 to 5.5 years old with multivessel PVS, five of which secondary to chronic lung disease, showed improved outcomes with minimal toxicity.144 Paclitaxel, an anticancer drug inhibiting cycle-dependent kinases responsible for cell proliferation, prevented monocrotaline- and hypoxia-induced PH in rats and reduced the hyperproliferative phenotype of PASMC isolated from PH patients.145 Fasudil, an inhibitor of the endothelin-associated ROCK pathway, significantly improved PH to a greater degree than did bosentan and sildenafil in a rat PH model.146 Mitogen-activated protein kinase and extracellular signal-regulated kinase are other key regulators of PASMC proliferation, mediating several effects of cytokine and chemokine signals in PH pathophysiology. As an example, tolicizumab, an interleukin-6 receptor-specific antagonist, reversed experimental PH in two rat models.147
Tacrolimus, a calcineurin inhibitor, used as an immunosuppressor in organ transplantation and recently identified as a potent BMPR2 agonist reversed the endothelial dysfunction in PAH patient cell cultures and experimental PH. A phase II RCT in adults with PAH demonstrated good safety and tolerability, but failed to show significant benefits.148 In a newborn rat hyperoxia model of BPD, simultaneous treatment with bone morphogenetic protein 9, the ligand of BMPR2, improved aberrant alveolar development, inflammation, and fibrosis.149
In summary, appropriately powered RCTs of various pulmonary vasodilators targeting endothelial dysfunction, the mainstay of PH therapy in children and adults, are still needed in order to demonstrate their efficacy and establish treatment protocols in BPD-PH. Agents targeting specific pathways involved in pulmonary vascular development and remodeling shows promising results in preclinical studies. However, animal models are imperfect and only reproduce certain aspects of BPD and/or PVD. Translation to the human neonate is still at a very preliminary, often anecdotal stage. Repurposing existing drugs to BPD-PH appears to be a possible strategy, but formal clinical trials should be conducted before implementing their use at the bedside.
Cell-based therapies and application to BPD and PH
Lung-resident stem cells are key regulators of pulmonary homeostasis and play an important role in regulating the lung immune and repair responses in processes, such as inflammation, angiogenesis, and fibrosis; their depletion or dysfunction plays a key role in the genesis of BPD.150 With their self-renewing and pluripotent properties, stem cells have been extensively studied as therapies for various neonatal conditions, including BPD. A recent meta-analysis of 25 animal studies has demonstrated a clear efficacy of mesenchymal stem cells (MSCs) in the hyperoxia rat model of BPD, improving both alveolarization and vascularization.151 These results gave way to a first human phase I trial of intratracheally administered MSC in nine preterm infants <29 weeks at high risk of BPD during the second week of life, showing good tolerability and decreased pro-inflammatory biomarkers.152 The same investigators are currently conducting a multicenter phase II RCT (NCT03392467) using human umbilical cord blood-derived MSC (Pneumostem®) for the prevention of severe BPD. Similarly, a phase I study confirmed the tolerability of intra-tracheal human umbilical cord blood-derived MSC in twelve 25-week preterm infants in the second week of life, two of which developed severe PH.153 Another phase I trial was undertaken in Australia using amnion epithelial cells (AECs). AECs were administered IV at 36 weeks corrected age in six ex-preterm infants <28 weeks with severe BPD; one died of pulmonary embolism shortly after AEC administration, four out of five survivors had PH at discharge,154 which resolved in two patients by 2 years of age.155 A subsequent dose-escalation trial is underway.156 Only appropriately sized studies with control groups will tell whether and which postnatal stem cell-based therapies significantly impact BPD-related PH in the neonatal intensive care unit setting.
Initially thought to promote lung regeneration by trans-differentiation into alveolar type II cells, stem cells actually show a low rate of in vivo engraftment, suggesting that they exert their effect indirectly through a paracrine mechanism. Extracellular vesicles, or exosomes, are the main vector of these effects, and many animal studies support MSC-derived exosome efficacy in lung injury repair, BPD therapy (for a review, see Worthington and Hagood157 and Wang et al.158), and PVD prevention.159,160 The efficacy of purified MSC exosomes appears equal to superior to live stem cells, even though their bioactive component(s) remain elusive (integrins, fatty acids, microRNA, DNA, growth, and transcription factors).161 A human phase-1 study with IV stem cell-derived exosomes in preterm neonates at high risk for BPD is currently underway (UNEX-42, NCT03857841). However, there are important limitations to stem cell or exosome therapeutic use in neonates. Manufacturing pharmacological-grade cells and compounds would require an extended knowledge of their composition and features, as well as a rigorous assessment of quality, potency, homogeneity, and purity. Safety, clinical efficacy, dosages, and protocols will require further appropriately sized and controlled clinical trials.161
Conclusions
BPD-PH is a unique disease affecting a unique population, and remains a major concern for neonatologists, as its development is associated with severe morbidities and a significant mortality. PVD develops from the earliest stages of BPD, as early as fetal life, before its clinical manifestations become detectable. Although alveolar and vascular development and disease are tightly bound, they represent distinct entities that may present and evolve differently among premature infants, as a consequence of individual genetic susceptibilities and specific environmental exposures. To date, direct evidence on antenatal PVD identification is poor, and mostly derived from other entities distinct from BPD-PH. Progress in diagnostic techniques and biomarkers open the potentiality of an earlier detection and personalized approaches to PVD and BPD comorbidities. However, larger trials for early postnatal diagnosis are needed in order to validate indices and determine their diagnostic and prognostic value.
Regarding therapeutic options, the core evidence derives from adult and children PH studies, highlighting the need for larger comparative RCTs specifically addressing the management of established BPD-PH in neonates, in order to determine which agents or which protocols and combinations are the most effective. Most prevention research is at a preclinical stage. Future studies should focus on interventions aimed at avoiding the inception of PVD as early as fetal life. Since single-agent, single-target strategies have failed to decrease BPD incidence and novel approaches in BPD-PH prevention are mostly at a preclinical stage, stem cell-based therapies, including exosomes, that harvest the regenerative and homeostatic power of MSCs without the challenges and potential risks related to live cell transplantation, may represent a possible approach for the cure and the prevention of such a complex and multifactorial disease, if and when their efficacy, safety, and sustainability will be soundly established.
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 314, 1039–1051 (2015).
Stensvold, H. J. et al. Neonatal morbidity and 1-year survival of extremely preterm infants. Pediatrics 139, e20161821 (2017).
Abman, S. H. et al. Interdisciplinary care of children with severe bronchopulmonary dysplasia. J. Pediatr. 181, 12–28 e1 (2017).
Khemani, E. et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics 120, 1260–1269 (2007).
Lagatta, J. M. et al. The impact of pulmonary hypertension in preterm infants with severe bronchopulmonary dysplasia through 1 year. J. Pediatr. 203, 218–24 e3 (2018).
Bhat, R., Salas, A. A., Foster, C., Carlo, W. A. & Ambalavanan, N. Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics 129, e682–e689 (2012).
Kim, D. H. et al. Risk factors for pulmonary artery hypertension in preterm infants with moderate or severe bronchopulmonary dysplasia. Neonatology 101, 40–46 (2012).
Mourani, P. M. et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 191, 87–95 (2015).
Levy, P. T., Patel, M. D., Choudhry, S., Hamvas, A. & Singh, G. K. Evidence of echocardiographic markers of pulmonary vascular disease in asymptomatic infants born preterm at one year of age. J. Pediatr. 197, 48–56 e2 (2018).
Baker, C. D., Abman, S. H. & Mourani, P. M. Pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. Pediatr. Allergy Immunol. Pulmonol. 27, 8–16 (2014).
Krishnan, U. et al. Evaluation and management of pulmonary hypertension in children with bronchopulmonary dysplasia. J. Pediatr. 188, 24–34 e1 (2017).
Steurer, M. A. et al. Mortality in infants with bronchopulmonary dysplasia: data from cardiac catheterization. Pediatr. Pulmonol. 54, 804–813 (2019).
Newth, C. J., Gow, R. M. & Rowe, R. D. The assessment of pulmonary arterial pressures in bronchopulmonary dysplasia by cardiac catheterization and M-mode echocardiography. Pediatr. Pulmonol. 1, 58–62 (1985).
Singh, A., Feingold, B., Rivera-Lebron, B., Weiner, D. & Drant, S. Correlating objective echocardiographic parameters in patients with pulmonary hypertension due to bronchopulmonary dysplasia. J. Perinatol. 39, 1282–1290 (2019).
Nawaytou, H. et al. Clinical utility of echocardiography in former preterm infants with bronchopulmonary dysplasia. J. Am. Soc. Echocardiogr. 33, 378–388 e1 (2020).
Di Maria, M. V. et al. Maturational changes in diastolic longitudinal myocardial velocity in preterm infants. J. Am. Soc. Echocardiogr. 28, 1045–1052 (2015).
Murase, M. & Ishida, A. Serial pulsed Doppler assessment of pulmonary artery pressure in very low birth-weight infants. Pediatr. Cardiol. 21, 452–457 (2000).
Ehrmann, D. E. et al. Echocardiographic measurements of right ventricular mechanics in infants with bronchopulmonary dysplasia at 36 weeks postmenstrual age. J. Pediatr. 203, 210–7 e1 (2018).
Mourani, P. M., Sontag, M. K., Younoszai, A., Ivy, D. D. & Abman, S. H. Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics 121, 317–325 (2008).
McCrary, A. W. et al. Differences in eccentricity index and systolic-diastolic ratio in extremely low-birth-weight infants with bronchopulmonary dysplasia at risk of pulmonary hypertension. Am. J. Perinatol. 33, 57–62 (2016).
Levy, P. T. et al. Pulmonary artery acceleration time provides a reliable estimate of invasive pulmonary hemodynamics in children. J. Am. Soc. Echocardiogr. 29, 1056–1065 (2016).
Patel, M. D. et al. Echocardiographic assessment of right ventricular afterload in preterm infants: maturational patterns of pulmonary artery acceleration time over the first year of age and implications for pulmonary hypertension. J. Am. Soc. Echocardiogr. 32, 884–94 e4 (2019).
Gaulton, J. S. et al. Relationship between pulmonary artery acceleration time and pulmonary artery pressures in infants. Echocardiography 36, 1524–1531 (2019).
Levy, P. T. et al. Right ventricular function in preterm and term neonates: reference values for right ventricle areas and fractional area of change. J. Am. Soc. Echocardiogr. 28, 559–569 (2015).
Koestenberger, M. et al. Systolic right ventricular function in preterm and term neonates: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 258 patients and calculation of Z-score values. Neonatology 100, 85–92 (2011).
Levy, P. T. et al. Maturational patterns of systolic ventricular deformation mechanics by two-dimensional speckle-tracking echocardiography in preterm infants over the first year of age. J. Am. Soc. Echocardiogr. 30, 685–98 e1 (2017).
Erickson, C. T. et al. Persistence of right ventricular dysfunction and altered morphometry in asymptomatic preterm Infants through one year of age: cardiac phenotype of prematurity. Cardiol. Young 29, 945–953 (2019).
Ligon, R. A., Vaiyani, D. & Deshpande, S. Right ventricular myocardial performance index in pediatric patients with bronchopulmonary dysplasia-related pulmonary hypertension. Echocardiography 36, 1353–1356 (2019).
Blanca, A. J. et al. Right ventricular function in infants with bronchopulmonary dysplasia and pulmonary hypertension: a pilot study. Pulm. Circ. 9, 2045894018816063 (2019).
Malowitz, J. R. et al. Right ventricular echocardiographic indices predict poor outcomes in infants with persistent pulmonary hypertension of the newborn. Eur. Heart J. Cardiovasc. Imaging 16, 1224–1231 (2015).
Seo, Y. H. & Choi, H. J. Clinical Utility of echocardiography for early and late pulmonary hypertension in preterm infants: relation with bronchopulmonary dysplasia. J. Cardiovasc. Ultrasound 25, 124–130 (2017).
Cameli, M. et al. Speckle tracking echocardiography: a practical guie]. G Ital. Cardiol. 18, 253–269 (2017).
Patel, N. & Kipfmueller, F. Cardiac dysfunction in congenital diaphragmatic hernia: Pathophysiology, clinical assessment, and management. Semin. Pediatr. Surg. 26, 154–158 (2017).
Gorter, T. M., Willems, T. P. & van Melle, J. P. Ventricular interdependence in pulmonary arterial hypertension: providing small pieces of a complex puzzle. Eur. J. Heart Fail. 17, 1–2 (2015).
Motoji, Y. et al. Interdependence of right ventricular systolic function and left ventricular filling and its association with outcome for patients with pulmonary hypertension. Int. J. Cardiovasc. Imaging 31, 691–698 (2015).
Buckberg, G. D., Hoffman, J. I., Coghlan, H. C. & Nanda, N. C. Ventricular structure-function relations in health and disease: part I. The normal heart. Eur. J. Cardiothorac. Surg. 47, 587–601 (2015).
Massolo, A. C. et al. Ventricular dysfunction, interdependence, and mechanical dispersion in newborn infants with congenital diaphragmatic hernia. Neonatology 116, 68–75 (2019).
Bokiniec, R., Wlasienko, P., Borszewska-Kornacka, M. & Szymkiewicz-Dangel, J. Evaluation of left ventricular function in preterm infants with bronchopulmonary dysplasia using various echocardiographic techniques. Echocardiography 34, 567–576 (2017).
James, A. T. et al. Longitudinal assessment of left and right myocardial function in preterm infants using strain and strain rate imaging. Neonatology 109, 69–75 (2016).
Nagiub, M., Lee, S. & Guglani, L. Echocardiographic assessment of pulmonary hypertension in infants with bronchopulmonary dysplasia: systematic review of literature and a proposed algorithm for assessment. Echocardiography 32, 819–833 (2015).
Mirza, H. et al. Pulmonary hypertension in preterm infants: prevalence and association with bronchopulmonary dysplasia. J. Pediatr. 165, 909–14 e1 (2014).
Morrow, L. A. et al. Antenatal determinants of bronchopulmonary dysplasia and late respiratory disease in preterm infants. Am. J. Respir. Crit. Care Med. 196, 364–374 (2017).
Lio, A. et al. Fetal Doppler velocimetry and bronchopulmonary dysplasia risk among growth-restricted preterm infants: an observational study. BMJ Open 7, e015232 (2017).
Azpurua, H. et al. Acceleration/ejection time ratio in the fetal pulmonary artery predicts fetal lung maturity. Am. J. Obstet. Gynecol. 203, 40 e1–40 e8 (2010).
Moety, G. A., Gaafar, H. M. & El Rifai, N. M. Can fetal pulmonary artery Doppler indices predict neonatal respiratory distress syndrome? J. Perinatol. 35, 1015–1019 (2015).
Fuke, S. et al. Antenatal prediction of pulmonary hypoplasia by acceleration time/ejection time ratio of fetal pulmonary arteries by Doppler blood flow velocimetry. Am. J. Obstet. Gynecol. 188, 228–233 (2003).
Broth, R. E. et al. Prenatal prediction of lethal pulmonary hypoplasia: the hyperoxygenation test for pulmonary artery reactivity. Am. J. Obstet. Gynecol. 187, 940–945 (2002).
Done, E. et al. Maternal hyperoxygenation test in fetuses undergoing FETO for severe isolated congenital diaphragmatic hernia. Ultrasound Obstet. Gynecol. 37, 264–271 (2011).
Triebwasser, J. E. & Treadwell, M. C. Prenatal prediction of pulmonary hypoplasia. Semin. Fetal Neonatal Med. 22, 245–249 (2017).
Beghetti, M. et al. Diagnostic evaluation of paediatric pulmonary hypertension in current clinical practice. Eur. Respir. J. 42, 689–700 (2013).
Hansmann, G. et al. Executive summary. Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart 102, ii86–ii100 (2016).
Ivy, D. Pulmonary hypertension in children. Cardiol. Clin. 34, 451–472 (2016).
Frank, B. S. et al. Acute vasoreactivity testing during cardiac catheterization of neonates with bronchopulmonary dysplasia-associated pulmonary hypertension. J. Pediatr. 208, 127–133 (2019).
Taylor, C. J., Derrick, G., McEwan, A., Haworth, S. G. & Sury, M. R. Risk of cardiac catheterization under anaesthesia in children with pulmonary hypertension. Br. J. Anaesth. 98, 657–661 (2007).
O’Byrne, M. L., Kennedy, K. F., Kanter, J. P., Berger, J. T. & Glatz, A. C. Risk factors for major early adverse events related to cardiac catheterization in children and young adults with pulmonary hypertension: an analysis of data from the IMPACT (Improving Adult and Congenital Treatment) Registry. J. Am. Heart Assoc. 7, e008142 (2018).
Kumar, V. H. S. Diagnostic approach to pulmonary hypertension in premature neonates. Children 4, 75 (2017).
Lamers, L. J. et al. Multicenter assessment of radiation exposure during pediatric cardiac catheterizations using a novel imaging system. J. Inter. Cardiol. 2019, 7639754 (2019).
Zampi, J. D. & Whiteside, W. Innovative interventional catheterization techniques for congenital heart disease. Transl. Pediatr. 7, 104–119 (2018).
Kang, S. L. & Benson, L. Recent advances in cardiac catheterization for congenital heart disease. F1000Res 7, 370 (2018).
Latus, H. et al. Cardiac MR and CT imaging in children with suspected or confirmed pulmonary hypertension/pulmonary hypertensive vascular disease. Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart 102, ii30–ii35 (2016).
Hahn, A. D. et al. Pulmonary MRI of neonates in the intensive care unit using 3D ultrashort echo time and a small footprint MRI system. J. Magn. Reson. Imaging 45, 463–471 (2017).
Higano, N. S. et al. Neonatal pulmonary magnetic resonance imaging of bronchopulmonary dysplasia predicts short-term clinical outcomes. Am. J. Respir. Crit. Care Med. 198, 1302–1311 (2018).
Forster, K. et al. Altered relaxation times in MRI indicate bronchopulmonary dysplasia. Thorax 75, 184–187 (2020).
Voskrebenzev, A. & Vogel-Claussen, J. Proton MRI of the lung: how to tame scarce protons and fast signal decay. J. Magn. Reson. Imaging 27122 (2020).
Critser, P. J. et al. Cardiac magnetic resonance imaging evaluation of neonatal bronchopulmonary dysplasia-associated pulmonary hypertension. Am. J. Respir. Crit. Care Med. 201, 73–82 (2020).
Casserly, B. & Klinger, J. R. Brain natriuretic peptide in pulmonary arterial hypertension: biomarker and potential therapeutic agent. Drug Des. Dev. Ther. 3, 269–287 (2009).
Yasue, H. et al. Localization and mechanism of secretion of B-type natriuretic peptide in comparison with those of A-type natriuretic peptide in normal subjects and patients with heart failure. Circulation 90, 195–203 (1994).
Nagaya, N. et al. Plasma brain natriuretic peptide levels increase in proportion to the extent of right ventricular dysfunction in pulmonary hypertension. J. Am. Coll. Cardiol. 31, 202–208 (1998).
Montgomery, A. M. et al. Biochemical screening for pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. Neonatology 109, 190–194 (2016).
Cuna, A., Kandasamy, J. & Sims, B. B-type natriuretic peptide and mortality in extremely low birth weight infants with pulmonary hypertension: a retrospective cohort analysis. BMC Pediatr. 14, 68 (2014).
Behere, S., Alapati, D. & McCulloch, M. A. Screening echocardiography and brain natriuretic peptide levels predict late pulmonary hypertension in infants with bronchopulmonary dysplasia. Pediatr. Cardiol. 40, 973–979 (2019).
Amdani, S. M., Mian, M. U. M., Thomas, R. L. & Ross, R. D. NT-pro BNP-A marker for worsening respiratory status and mortality in infants and young children with pulmonary hypertension. Congenit. Heart Dis. 13, 499–505 (2018).
Reynolds, E. W., Ellington, J. G., Vranicar, M. & Bada, H. S. Brain-type natriuretic peptide in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatrics 114, 1297–1304 (2004).
Steurer, M. A. et al. B-type natriuretic peptide: prognostic marker in congenital diaphragmatic hernia. Pediatr. Res. 76, 549–554 (2014).
Konig, K., Guy, K. J., Walsh, G., Drew, S. M. & Barfield, C. P. Association of BNP, NTproBNP, and early postnatal pulmonary hypertension in very preterm infants. Pediatr. Pulmonol. 51, 820–824 (2016).
Choi, B. M. et al. Utility of rapid B-type natriuretic peptide assay for diagnosis of symptomatic patent ductus arteriosus in preterm infants. Pediatrics 115, e255–e261 (2005).
Farombi-Oghuvbu, I., Matthews, T., Mayne, P. D., Guerin, H. & Corcoran, J. D. N-terminal pro-B-type natriuretic peptide: a measure of significant patent ductus arteriosus. Arch. Dis. Child Fetal Neonatal Ed. 93, F257–F260 (2008).
McMahon, T. J. & Bryan, N. S. Biomarkers in pulmonary vascular disease: gauging response to therapy. Am. J. Cardiol. 120, S89–S95 (2017).
Gien, J., Tseng, N., Seedorf, G., Kuhn, K. & Abman, S. H. Endothelin-1-Rho kinase interactions impair lung structure and cause pulmonary hypertension after bleomycin exposure in neonatal rat pups. Am. J. Physiol. Lung Cell. Mol. Physiol. 311, L1090–L1100 (2016).
El Sayed, M. et al. Endothelin-1 and L-arginine in preterm infants with respiratory distress. Am. J. Perinatol. 28, 129–136 (2011).
Niu, J. O., Munshi, U. K., Siddiq, M. M. & Parton, L. A. Early increase in endothelin-1 in tracheal aspirates of preterm infants: correlation with bronchopulmonary dysplasia. J. Pediatr. 132, 965–970 (1998).
Alvarez-Fuente, M. et al. Exploring clinical, echocardiographic and molecular biomarkers to predict bronchopulmonary dysplasia. PLoS ONE 14, e0213210 (2019).
Benzing, J. et al. Plasma pro-endothelin-1 and respiratory distress in newborn infants. J. Pediatr. 160, 517–519 (2012).
Baumann, P. et al. Plasma proendothelin-1 as an early marker of bronchopulmonary dysplasia. Neonatology 108, 293–296 (2015).
Stenmark, K. R. & Abman, S. H. Lung vascular development: implications for the pathogenesis of bronchopulmonary dysplasia. Annu. Rev. Physiol. 67, 623–661 (2005).
Mestan, K. K. et al. Cord blood biomarkers of placental maternal vascular underperfusion predict bronchopulmonary dysplasia-associated pulmonary hypertension. J. Pediatr. 185, 33–41 (2017).
Mestan, K. K. et al. Placental pathologic changes of maternal vascular underperfusion in bronchopulmonary dysplasia and pulmonary hypertension. Placenta 35, 570–574 (2014).
Kim, D. H. & Kim, H. S. Serial changes of serum endostatin and angiopoietin-1 levels in preterm infants with severe bronchopulmonary dysplasia and subsequent pulmonary artery hypertension. Neonatology 106, 55–61 (2014).
Bhatt, A. J. et al. Disrupted pulmonary vasculature and decreased vascular endothelial growth factor, Flt-1, and TIE-2 in human infants dying with bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 164, 1971–1980 (2001).
Mourani, P. M., Sontag, M. K., Ivy, D. D. & Abman, S. H. Effects of long-term sildenafil treatment for pulmonary hypertension in infants with chronic lung disease. J. Pediatr. 154, 379–384 e1–2 (2009).
Abounahia, F. F. et al. Prophylactic sildenafil in preterm infants at risk of bronchopulmonary dysplasia: a pilot randomized, double-blinded, placebo-controlled trial. Clin. Drug Investig. 39, 1093–1107 (2019).
Konig, K., Barfield, C. P., Guy, K. J., Drew, S. M. & Andersen, C. C. The effect of sildenafil on evolving bronchopulmonary dysplasia in extremely preterm infants: a randomised controlled pilot study. J. Matern. Fetal Neonatal Med. 27, 439–444 (2014).
Samiee-Zafarghandy, S. et al. Sildenafil and retinopathy of prematurity risk in very low birth weight infants. J. Perinatol. 36, 137–140 (2016).
Sabri, M. R. & Beheshtian, E. Comparison of the therapeutic and side effects of tadalafil and sildenafil in children and adolescents with pulmonary arterial hypertension. Pediatr. Cardiol. 35, 699–704 (2014).
Shiva, A. et al. Oral Tadalafil in children with pulmonary arterial hypertension. Drug Res. 66, 7–10 (2016).
Takatsuki, S., Calderbank, M. & Ivy, D. D. Initial experience with tadalafil in pediatric pulmonary arterial hypertension. Pediatr. Cardiol. 33, 683–688 (2012).
Yamamura, A. et al. Tadalafil induces antiproliferation, apoptosis, and phosphodiesterase type 5 downregulation in idiopathic pulmonary arterial hypertension in vitro. Eur. J. Pharm. 810, 44–50 (2017).
Russo, F. M. et al. Transplacental sildenafil rescues lung abnormalities in the rabbit model of diaphragmatic hernia. Thorax 71, 517–525 (2016).
Russo, F. M. et al. Antenatal sildenafil administration to prevent pulmonary hypertension in congenital diaphragmatic hernia (SToP-PH): study protocol for a phase I/IIb placenta transfer and safety study. Trials 19, 524 (2018).
Pels, A. et al. STRIDER (Sildenafil TheRapy in dismal prognosis early onset fetal growth restriction): an international consortium of randomised placebo-controlled trials. BMC Pregnancy Childbirth 17, 440 (2017).
Sharp, A. et al. Maternal sildenafil for severe fetal growth restriction (STRIDER): a multicentre, randomised, placebo-controlled, double-blind trial. Lancet Child Adolesc. Health 2, 93–102 (2018).
Groom, K. M. et al. STRIDER NZAus: a multicentre randomised controlled trial of sildenafil therapy in early-onset fetal growth restriction. BJOG 126, 997–1006 (2019).
Maki, S. et al. Safety evaluation of Tadalafil treatment for fetuses with early-onset growth restriction (TADAFER): results from the phase II trial. J Clin Med. 8, 856 (2019).
Dasgupta, A., Bowman, L., D’Arsigny, C. L. & Archer, S. L. Soluble guanylate cyclase: a new therapeutic target for pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Clin. Pharm. Ther. 97, 88–102 (2015).
Ghofrani, H. A. et al. Riociguat for the treatment of pulmonary arterial hypertension. N. Engl. J. Med. 369, 330–340 (2013).
Rubin, L. J. et al. Riociguat for the treatment of pulmonary arterial hypertension: a long-term extension study (PATENT-2). Eur. Respir. J. 45, 1303–1313 (2015).
Donda, K. et al. Riociguat prevents hyperoxia-induced lung injury and pulmonary hypertension in neonatal rats without effects on long bone growth. PLoS ONE 13, e0199927 (2018).
Spreemann, T., Bertram, H., Happel, C. M., Kozlik-Feldmann, R. & Hansmann, G. First-in-child use of the oral soluble guanylate cyclase stimulator riociguat in pulmonary arterial hypertension. Pulm. Circ. 8, 2045893217743123 (2018).
Steinhorn, R. H. et al. Bosentan as adjunctive therapy for persistent pulmonary hypertension of the newborn: results of the randomized multicenter placebo-controlled exploratory trial. J. Pediatr. 177, 90–6 e3 (2016).
Rugolotto, S. et al. Weaning of epoprostenol in a small infant receiving concomitant bosentan for severe pulmonary arterial hypertension secondary to bronchopulmonary dysplasia. Minerva Pediatr. 58, 491–494 (2006).
Takatsuki, S. et al. Clinical safety, pharmacokinetics, and efficacy of ambrisentan therapy in children with pulmonary arterial hypertension. Pediatr. Pulmonol. 48, 27–34 (2013).
Wagenaar, G. T. et al. Ambrisentan reduces pulmonary arterial hypertension but does not stimulate alveolar and vascular development in neonatal rats with hyperoxic lung injury. Am. J. Physiol. Lung Cell. Mol. Physiol. 304, L264–L275 (2013).
Iglarz, M. et al. Pharmacology of macitentan, an orally active tissue-targeting dual endothelin receptor antagonist. J. Pharm. Exp. Ther. 327, 736–745 (2008).
Weiss, J. et al. Interaction profile of macitentan, a new non-selective endothelin-1 receptor antagonist, in vitro. Eur. J. Pharm. 701, 168–175 (2013).
Pulido, T. et al. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N. Engl. J. Med. 369, 809–818 (2013).
Majed, B. H. & Khalil, R. A. Molecular mechanisms regulating the vascular prostacyclin pathways and their adaptation during pregnancy and in the newborn. Pharm. Rev. 64, 540–582 (2012).
Shivanna, B., Gowda, S., Welty, S. E., Barrington, K. J. & Pammi, M. Prostanoids and their analogues for the treatment of pulmonary hypertension in neonates. Cochrane Database Syst. Rev. 10, CD012963 (2019).
Olson, E., Lusk, L. A., Fineman, J. R., Robertson, L. & Keller, R. L. Short-term treprostinil use in infants with congenital diaphragmatic hernia following repair. J. Pediatr. 167, 762–764 (2015).
Carpentier, E. et al. Safety and tolerability of subcutaneous treprostinil in newborns with congenital diaphragmatic hernia and life-threatening pulmonary hypertension. J. Pediatr. Surg. 52, 1480–1483 (2017).
Lawrence, K. M. et al. Treprostinil improves persistent pulmonary hypertension associated with congenital diaphragmatic hernia. J. Pediatr. 200, 44–49 (2018).
Ferdman, D. J., Rosenzweig, E. B., Zuckerman, W. A. & Krishnan, U. Subcutaneous treprostinil for pulmonary hypertension in chronic lung disease of infancy. Pediatrics 134, e274–e278 (2014).
Olave, N., Lal, C. V., Halloran, B., Bhandari, V. & Ambalavanan, N. Iloprost attenuates hyperoxia-mediated impairment of lung development in newborn mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 315, L535–L544 (2018).
Barst, R. J. et al. Beraprost therapy for pulmonary arterial hypertension. J. Am. Coll. Cardiol. 41, 2119–2125 (2003).
Galie, N. et al. Effects of beraprost sodium, an oral prostacyclin analogue, in patients with pulmonary arterial hypertension: a randomized, double-blind, placebo-controlled trial. J. Am. Coll. Cardiol. 39, 1496–1502 (2002).
Beghetti, M. et al. Selexipag treatment for pulmonary arterial hypertension associated with congenital heart disease after defect correction: insights from the randomised controlled GRIPHON study. Eur. J. Heart Fail. 21, 352–359 (2019).
Geerdink, L. M., Bertram, H. & Hansmann, G. First-in-child use of the oral selective prostacyclin IP receptor agonist selexipag in pulmonary arterial hypertension. Pulm. Circ. 7, 551–554 (2017).
Rothman, A., Cruz, G., Evans, W. N. & Restrepo, H. Hemodynamic and clinical effects of selexipag in children with pulmonary hypertension. Pulm. Circ. 10, 2045894019876545 (2020).
Frost, A. et al. Safety and tolerability of transition from inhaled treprostinil to oral selexipag in pulmonary arterial hypertension: results from the TRANSIT-1 study. J. Heart Lung Transplant. 38, 43–50 (2019).
Hansmann, G. et al. Selexipag for the treatment of children with pulmonary arterial hypertension: First multicenter experience in drug safety and efficacy. J. Heart Lung Transplant. 39, 695–706 (2020).
Koo, R., Lo, J. & Bock, M. J. Transition from intravenous treprostinil to enteral selexipag in an infant with pulmonary arterial hypertension. Cardiol. Young 29, 849–851 (2019).
Mous, D. S. et al. Treatment of rat congenital diaphragmatic hernia with sildenafil and NS-304, selexipag’s active compound, at the pseudoglandular stage improves lung vasculature. Am. J. Physiol. Lung Cell. Mol. Physiol. 315, L276–L285 (2018).
Hansmann, G. et al. Pulmonary arterial hypertension is linked to insulin resistance and reversed by peroxisome proliferator-activated receptor-gamma activation. Circulation 115, 1275–1284 (2007).
Rashid, J., Nozik-Grayck, E., McMurtry, I. F., Stenmark, K. R. & Ahsan, F. Inhaled combination of sildenafil and rosiglitazone improves pulmonary hemodynamics, cardiac function, and arterial remodeling. Am. J. Physiol. Lung Cell. Mol. Physiol. 316, L119–L130 (2019).
Gosemann, J. H. et al. Prenatal treatment with rosiglitazone attenuates vascular remodeling and pulmonary monocyte influx in experimental congenital diaphragmatic hernia. PLoS ONE 13, e0206975 (2018).
Dasgupta, C. et al. Hyperoxia-induced neonatal rat lung injury involves activation of TGF-{beta} and Wnt signaling and is protected by rosiglitazone. Am. J. Physiol. Lung Cell. Mol. Physiol. 296, L1031–L1041 (2009).
Katsi, V. et al. The role of statins in prevention of preeclampsia: a promise for the future? Front. Pharm. 8, 247 (2017).
Salaets, T. et al. Simvastatin attenuates lung functional and vascular effects of hyperoxia in preterm rabbits. Pediatr. Res. 87, 1193–1200 (2020).
Makanga, M. et al. Prevention of pulmonary hypoplasia and pulmonary vascular remodeling by antenatal simvastatin treatment in nitrofen-induced congenital diaphragmatic hernia. Am. J. Physiol. Lung Cell. Mol. Physiol. 308, L672–L682 (2015).
Wong, M. J., Kantores, C., Ivanovska, J., Jain, A. & Jankov, R. P. Simvastatin prevents and reverses chronic pulmonary hypertension in newborn rats via pleiotropic inhibition of RhoA signaling. Am. J. Physiol. Lung Cell. Mol. Physiol. 311, L985–L999 (2016).
Costantine, M. M. et al. Safety and pharmacokinetics of pravastatin used for the prevention of preeclampsia in high-risk pregnant women: a pilot randomized controlled trial. Am. J. Obstet. Gynecol. 214, 720 e1–e17 (2016).
Leong, Z. P., Okida, A., Higuchi, M., Yamano, Y. & Hikasa, Y. Reversal effects of low-dose imatinib compared with sunitinib on monocrotaline-induced pulmonary and right ventricular remodeling in rats. Vasc. Pharm. 100, 41–50 (2018).
Schermuly, R. T. et al. Reversal of experimental pulmonary hypertension by PDGF inhibition. J. Clin. Invest. 115, 2811–2821 (2005).
Hoeper, M. M. et al. Imatinib mesylate as add-on therapy for pulmonary arterial hypertension: results of the randomized IMPRES study. Circulation 127, 1128–1138 (2013).
Callahan, R. et al. Adjunct targeted biologic inhibition agents to treat aggressive multivessel intraluminal pediatric pulmonary vein stenosis. J. Pediatr. 198, 29–35 e5 (2018).
Savai, R. et al. Pro-proliferative and inflammatory signaling converge on FoxO1 transcription factor in pulmonary hypertension. Nat. Med. 20, 1289–1300 (2014).
Mouchaers, K. T. et al. Fasudil reduces monocrotaline-induced pulmonary arterial hypertension: comparison with bosentan and sildenafil. Eur. Respir. J. 36, 800–807 (2010).
Tamura, Y. et al. Ectopic upregulation of membrane-bound IL6R drives vascular remodeling in pulmonary arterial hypertension. J. Clin. Invest. 128, 1956–1970 (2018).
Spiekerkoetter, E. et al. Randomised placebo-controlled safety and tolerability trial of FK506 (tacrolimus) for pulmonary arterial hypertension. Eur. Respir. J. 50, 1602449 (2016).
Chen, X. et al. Bone morphogenetic protein 9 protects against neonatal hyperoxia-induced impairment of alveolarization and pulmonary inflammation. Front. Physiol. 8, 486 (2017).
Balasubramaniam, V., Mervis, C. F., Maxey, A. M., Markham, N. E. & Abman, S. H. Hyperoxia reduces bone marrow, circulating, and lung endothelial progenitor cells in the developing lung: implications for the pathogenesis of bronchopulmonary dysplasia. Am. J. Physiol. Lung Cell. Mol. Physiol. 292, L1073–L1084 (2007).
Augustine, S. et al. Mesenchymal stromal cell therapy in bronchopulmonary dysplasia: systematic review and meta-analysis of preclinical studies. Stem Cells Transl. Med. 6, 2079–2093 (2017).
Chang, Y. S. et al. Mesenchymal stem cells for bronchopulmonary dysplasia: phase 1 dose-escalation clinical trial. J. Pediatr. 164, 966–72 e6 (2014).
Powell, S. B. & Silvestri, J. M. Safety of intratracheal administration of human umbilical cord blood derived mesenchymal stromal cells in extremely low birth weight preterm infants. J. Pediatr. 210, 209–13 e2 (2019).
Lim, R. et al. First-in-human administration of allogeneic amnion cells in premature infants with bronchopulmonary dysplasia: a safety study. Stem Cells Transl. Med. 7, 628–635 (2018).
Malhotra, A., Lim, R., Mockler, J. C. & Wallace, E. M. Two-year outcomes of infants enrolled in the first-in-human study of amnion cells for bronchopulmonary dysplasia. Stem Cells Transl. Med. 9, 289–294 (2020).
Baker, E. K. et al. Human amnion cells for the prevention of bronchopulmonary dysplasia: a protocol for a phase I dose escalation study. BMJ Open 9, e026265 (2019).
Worthington, E. N. & Hagood, J. S. Therapeutic use of extracellular vesicles for acute and chronic lung disease. Int. J. Mol. Sci. 21, 2318 (2020).
Wang, Y. et al. Mesenchymal stem cell-derived secretomes for therapeutic potential of premature infant diseases. Biosci. Rep. 40, BSR20200241 (2020).
Klinger, J. R. et al. Mesenchymal stem cell extracellular vesicles reverse sugen/hypoxia pulmonary hypertension in rats. Am. J. Respir. Cell Mol. Biol. 62, 577–587 (2020).
Suzuki, T. et al. Mesenchymal stem/stromal cells stably transduced with an inhibitor of CC chemokine ligand 2 ameliorate bronchopulmonary dysplasia and pulmonary hypertension. Cytotherapy 22, 180–192 (2020).
Mitsialis, S. A. The unsettling ambiguity of therapeutic extracellular vesicles from mesenchymal stromal cells. Am. J. Respir. Cell Mol. Biol. 62, 539–540 (2020).
Author information
Authors and Affiliations
Consortia
Contributions
C.H. and O.D. collaborated on the conception and writing of this review. A.G. and O.D. contributed to the pharmacology section. C.H., L.V., and A.C.M. contributed to the imaging section. F.P., B.V.G., and K.C. contributed to the redaction and revision of the manuscript. All authors critically reviewed and agreed upon the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hocq, C., Vanhoutte, L., Guilloteau, A. et al. Early diagnosis and targeted approaches to pulmonary vascular disease in bronchopulmonary dysplasia. Pediatr Res 91, 804–815 (2022). https://doi.org/10.1038/s41390-021-01413-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01413-w
This article is cited by
-
Identification and validation of cuproptosis related genes and signature markers in bronchopulmonary dysplasia disease using bioinformatics analysis and machine learning
BMC Medical Informatics and Decision Making (2023)
-
The role of rhIGF-1/BP3 in the prevention of pulmonary hypertension in bronchopulmonary dysplasia and its underlying mechanism
BMC Pulmonary Medicine (2023)
-
Patent ductus arteriosus and the risk of bronchopulmonary dysplasia-associated pulmonary hypertension
Pediatric Research (2023)
-
Neonatal pulmonary hypertension after severe early-onset fetal growth restriction: post hoc reflections on the Dutch STRIDER study
European Journal of Pediatrics (2022)