Abstract
Background
Teaching caregivers to respond to normal infant night awakenings in ways other than feeding is a common obesity prevention effort. Models can simulate caregiver feeding behavior while controlling for variables that are difficult to manipulate or measure in real life.
Methods
We developed a virtual infant model representing an infant with an embedded metabolism and his/her daily sleep, awakenings, and feeds from their caregiver each day as the infant aged from 6 to 12 months (recommended age to introduce solids). We then simulated different night feeding interventions and their impact on infant body mass index (BMI).
Results
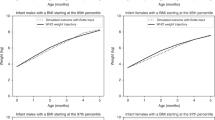
Reducing the likelihood of feeding during normal night wakings from 79% to 50% to 10% lowered infant BMI from the 84th to the 75th to the 62nd percentile by 12 months, respectively, among caregivers who did not adaptively feed (e.g., adjust portion sizes of solid foods with infant growth). Among caregivers who adaptively feed, all scenarios resulted in relatively stable BMI percentiles, and progressively reducing feeding probability by 10% each month showed the least fluctuations.
Conclusions
Reducing night feeding has the potential to impact infant BMI, (e.g., 10% lower probability can reduce BMI by 20 percentile points) especially among caregivers who do not adaptively feed.
Impact
-
Teaching caregivers to respond to infant night waking with other soothing behaviors besides feeding has the potential to reduce infant BMI.
-
When reducing the likelihood of feeding during night wakings from 79% to 50% to 10%, infants dropped from the 84th BMI percentile to the 75th to the 62nd by 12 months, respectively, among caregivers who do not adaptively feed.
-
Night-feeding interventions have a greater impact when caregivers do not adaptively feed their infant based on their growth compared to caregivers who do adaptively feed.
-
Night-feeding interventions should be one of the several tools in a multi-component intervention for childhood obesity prevention.
Similar content being viewed by others
Introduction
Caregivers often rely on feeding in order to soothe infants, beginning soon after birth. Since night awakenings normally occur frequently in infants,1,2,3,4 added nighttime feedings for infants who are at least 6 months old may be one of many factors contributing to childhood obesity.5,6 As a result, reducing this behavior by teaching caregivers to respond to normal night awakenings in ways other than feeding is a common goal of childhood obesity prevention efforts later in infancy.7,8,9 Caregivers and physicians need to understand the impact of such interventions. Many, though not all,10,11 interventions that aim to teach caregivers to replace feeding with other soothing behaviors upon infant night waking observe an effect on weight later in childhood.10,11,12,13 Methodological challenges exist within this body of work, with studies often limited by their reliance upon parental report and many potentially confounding variables,14 including the overall level of responsiveness to infant cues that caregivers show in feeding infants. The question remains, then, to what extent night feeding interventions can be expected to impact infant body weight, given the uncertainty and variability in effectiveness and compliance rates in reality.
Computational modeling can help overcome these limitations by simulating changes to caregiver feeding behavior in the safety of a computer while controlling for variables that are difficult to manipulate or measure in real life. For example, our previous work has explored how caregivers adjusting the portion sizes they feed their infants within feeding guidelines can impact infant weight.15,16 Therefore, we developed a computational simulation model representing infant metabolism, hunger, and sleep behavior and caregiver feeding behavior, to simulate various levels of effectiveness and compliance with an intervention aimed at reducing night feeding in infants 6 months of age and older to determine the impact on infant body mass index (BMI) at 12 months of age.
Methods
Virtual infant model
We developed a virtual infant agent-based model in Python17 representing a virtual infant and their caregiver beginning at 6 months. Similar to a real infant, each virtual infant has a variety of characteristics, including sex, starting length, starting weight, and starting BMI. Each infant also has an embedded metabolic model that includes fat mass, fat-free mass, physical activity, the thermic effect of feeding, and basal metabolic rate, adapted from the Hall and Rahmandad metabolic models,18,19 as described in previous publications.15,16 This metabolic model translates caloric intake and expenditure to corresponding changes to fat and fat-free mass.
The model proceeds in 1-day time steps, with the infant waking each day in the morning and moving, napping, and feeding throughout the day before going to sleep at night. The infant’s physical activity levels are higher when they are awake compared to when they are asleep due to differences in intensity of metabolic equivalents during wake time and sleep. As a result, the infant uses more calories while awake and less while asleep. We calibrated these values to match observed daily energy expenditure in infants.20 When the infant wakes up, they stay awake for a period of time, which is determined daily by the following equation:
Total wake time is calculated by subtracting total day sleep and total night sleep, which are pulled from distributions (Table 1), from 24 hours. Nocturnal wakefulness and number of naps are also pulled from distributions (Table 1).21 We add one to the number of naps to account for all periods of daytime wakefulness after each nap as well as before the first nap. While the infant is awake, their caregiver decides every hour (between months 6 and 8) or every 1.5 hours (months 9–12) whether to feed the infant breast milk, representing a gradual transition to more frequent and larger solid food portions.22,23 Since the composition of breast milk and resulting metabolic responses to breast milk are more consistent, we assumed that all infants consume breast milk. There is much greater variability in the composition of formula and how the body may respond. The infant’s hunger increases linearly over time, with the rate of increase in hunger varying based on age and peaking between 2 and 4 hours.24,25 As the infant’s hunger increases, the probability a caregiver decides to feed their infant increases concordantly. Once a caregiver feeds the infant, the infant’s hunger drops to baseline and begins increasing again. At the end of the wake period, the infant falls asleep for a nap; nap duration is based on the average time an infant stays asleep for their age, based on the equation: (total day sleep)/(number of naps), where both values are pulled from distributions, as shown in Table 1.21 After the sleep period has concluded, the wake cycle begins again, with the caregiver deciding whether to feed the infant immediately upon waking.
After 6:00 p.m. each day, the next time the infant falls asleep marks the beginning of night sleep, to approximate the average bedtime for infants under 1 year of age.26 At night, the infant wakes a certain number of times based on age and is awake for a certain period of time at night (see Table 1). The amount of time an infant is awake during each night waking is determined by the calculation: (total nocturnal wakefulness)/(total number of night wakings). Upon night waking, the caregiver has a 79% probability of feeding the infant when there is no intervention.27,28
Each daytime and nighttime feed is a certain amount (portion size in kilocalories) consistent with empirical averages for breastfed infants according to age.20,29,30 Daytime feedings consisted of breast milk as well as solid food meals. We calculated the mean of the portion size range of solid foods to correspond to the remaining energy requirements of the age of the infant20 after subtracting the typical portion size of breast milk according to age.29 Nighttime feedings consisted of breast milk only.
To represent caregivers with adaptive feeding behaviors, virtual caregivers could assess if and how to respond to their infant’s growth on a weekly basis. As described in our previous studies,15,16 caregivers start off feeding an amount of solid food from the full range (Table 1), and if the infant’s BMI increases and passes a major BMI percentile (5th, 10th, 25th, 50th, 75th, 90th, and 95th), then the caregiver will reduce the amount they feed their infant using an amount from the lower half of this distribution.
If an infant’s BMI continues to increase and crosses another major BMI percentile and they are already consuming the lower end of the range, then they will continue to consume portions at the lower end. If their BMI starts to decrease and crosses a major BMI percentile by the next week, the caregiver will adjust and feed from the full range. If after another week their BMI continues to decrease and crosses another major BMI percentile, the caregiver will adjust to the upper half. We allowed for only one adjustment per week, such that the portion size would not jump from the lower half to the upper half in 1 week.
Validation of simulation model
Data used to validate the model were separate from all model input data (Table 1). As shown in our previous studies, we compared infant weights when virtual infants (15th to 85th BMI percentile) were fed the age and BMI percentile-specific total energy requirements from Butte20 to the infant weights presented in the World Health Organization (WHO) growth curves. The outputs were not statistically different from the data.30,31,32 For example, a 50th BMI percentile virtual female weighs 6.058 kg at 3 months of age (compared to 5.84 kg on the WHO growth curve), 7.376 kg at 6 months of age (compared to 7.297 kg on the WHO growth curve), and 8.244 kg at 9 months of age (compared to 8.225 kg on the WHO growth curve).
After introducing infant sleep cycles, we compared total sleep duration to the reference curves established by Iglowstein et al.26 Model-generated output showed that the total sleep duration of a 6-month-old virtual infant was, on average, 13.4 hours (standard deviation [SD]: 0.8) and nocturnal wakefulness was 0.8 hours (SD: 0.2). This is comparable to the total sleep duration reported by Iglowstein et al. (mean of 14.2 hours [SD: 1.9]). For a virtual 12 month old, model-generated total sleep duration was, on average, 12.8 hours (SD: 0.6) with an average of 0.5 h (SD: 0.1) of nocturnal wakefulness compared to the total sleep reported mean of 13.9 hours (SD: 1.2). The model values are not statistically different from Iglowstein et al. As expected, the total sleep generated by the model is higher than total sleep reported by Iglowstein et al., which did not subtract nocturnal wakeful periods.
Modeled interventions
Experiments consisted of 1000 runs. We first simulated individual infants’ growth over the course of 6 months (6–12 months) without any night feeding intervention, both with and without adaptive caregiver feeding behaviors. Our simulations began at the age of 6 months, before which solids are generally not recommended for breastfed infants and night feeding is encouraged27; some literature suggests that behavioral night feeding interventions may not be developmentally appropriate earlier in life.33 To simulate various success rates for an educational intervention targeting the reduction of night feeding by infants’ caregivers, we tested various reductions in the probability of night feeding. We reduced the probability of feeding an infant during each night waking, ranging the probability from 70% to 10% beginning in month 6 (down from 79% when there was no intervention). We then explored the possibility of progressively reducing the probability of night feeding each month so that it was 79% in the 6th month, then decreasing by 10 percentage points each month until reaching 29% in the 11th month. We conducted our full range of experiments first without adaptive feeding behavior in caregivers and then repeated experiments while including this behavior (e.g., when caregivers can adjust the amount of solid food they feed their infant depending on their growth). Sensitivity analysis increased and decreased the total duration night sleep by a relative 10%.
Results
No intervention
When caregivers did not adjust portions in response to changes in body weight (representing less adaptive overall feeding practices), average BMI percentile continued to rise each week, beginning in week 27, ending at the highest point of 84th BMI percentile (95% confidence interval [CI]: 83–85), as is shown in Fig. 1. When caregivers adjusted portions in response to changes in body weight (representing more adaptive feeding practices), the average BMI percentile remained more stable, peaking at the 61st BMI percentile (95% CI: 59–62) in week 32 and then beginning to level off to end at the 55th percentile (95% CI: 53–58) (Fig. 2).
Experiments simulated a reduction in the number of times virtual caregivers respond to infant night awakenings with feeding. In these scenarios, virtual caregivers did not adjust to the infants’ weight trajectory by feeding in the lower or upper quartile of feeding amounts in response to significant weight gain or loss, respectively.
Experiments simulated a reduction in the number of times virtual caregivers respond to infant night awakenings with feeding. In these scenarios, virtual caregivers adjusted to the infants’ weight trajectory by feeding in the lower or upper quartile of feeding amounts in response to significant weight gain or loss, respectively.
Impact of night feeding interventions without adaptively feeding based on infant growth
When caregivers did not adjust portion sizes, reducing their probability of feeding their infants upon night waking to 70% resulted in lower average BMI percentiles over time compared to the baseline probability, though the line followed the same upward trajectories, ending at the 82nd (95% CI: 81–83) percentile as seen in Fig. 1. Reducing the probability of feeding upon night waking to 50% resulted in a similar trend, ending at the 75th (95% CI: 74–76) percentile. Reducing the probability to 10% produced variations in average BMI percentile that remained within the 62nd percentile (95% CI: 60–62) at the highest and the 56th percentile (95% CI: 56–57) at the lowest.
Finally, progressively reducing the probability of feeding upon night waking so that it was 29% in the 11th month resulted in a differently shaped growth curve, with BMI percentile stabilizing after 33 weeks (8.25 months of age), varying from the 70th percentile (95% CI: 70–71) at the lowest to the 72th percentile at the highest (95% CI: 70–73).
Impact of night feeding interventions with adaptive feeding based on infant growth
Reducing the probability of feeding upon night waking to 70% or 50% resulted in slightly lower average BMI percentiles compared to baseline, with reductions of 2.1 percentile points and 5 percentile points at most at week 37, respectively. When reducing probability of feeding upon night waking to 10%, infant BMI was 10 percentile points below the baseline at week 37 (the time point of greatest divergence) averaging at the 48th BMI percentile (95% CI: 47–49) and averaging at the 53rd BMI percentile (95% CI: 51–54) at the end of the first year. As shown in Fig. 2, when caregivers responded to 10, 50, and 70% of night feedings, the average BMI percentiles of infants ultimately converged within the CI of the baseline scenario at 52 weeks.
Reducing the probability of feeding upon night waking by 10 percentage points each month until reaching 29% in the 11th month resulted in the lowest ending BMI percentile at 51 (95% CI: 49–53) compared to other experimental scenarios.
Varying total sleep and number of night wakings
As shown in Fig. 3, when caregivers did not adaptively feed and infants’ total night sleep time decreased by a relative 10%, we found that there were more opportunities to feed, with an average of 7.17 feedings per day (95% CI: 7.15–7.18) for those with 10% less sleep compared with 6.44 feedings per day (95% CI: 6.43–6.45) at baseline. Thus, when total sleep decreased, consumption increased as a result, and the infants’ average BMI neared the obese weight category at the end of 1 year (94th BMI percentile). When caregivers did not adaptively feed infants and total sleep increased by a relative 10%, we found that BMI followed a similar trajectory compared to the baseline (not adjusting total sleep) and was at the 71st BMI percentile at the end of 1 year (Fig. 3). Simulations with a caregiver who did adaptively feed their infant initially showed similar trends to the non-adaptive feeding caregiver, with increased sleep resulting in lower BMI and decreased sleep resulting in higher BMI. However, after 40 weeks, caregivers adjusting portion sizes due to infant growth compensated for the changes in growth due to sleep and ultimately resulted in the infant with less sleep having, on average, a lower BMI compared to infants at both the baseline and with increased total sleep by 10% (Fig. 4). This demonstrates that our model is more sensitive to caregivers adjusting portion sizes than changes to total sleep (+/−10%).
Experiments simulated a reduction in the number of times virtual caregivers respond to infant night awakenings with feeding. In these scenarios, virtual caregivers adjusted to the infants’ weight trajectory by feeding in the lower or upper quartile of feeding amounts in response to significant weight gain or loss, respectively.
Sensitivity analyses simulated an increase and a reduction in total night sleep by a relative 10%. In these scenarios, virtual caregivers adjusted to the infants’ weight trajectory by feeding in the lower or upper quartile of feeding amounts in response to significant weight gain or loss, respectively.
Discussion
This study shows the impact of night feeding interventions on infant BMI when reducing a caregiver’s likelihood of feeding their infant during wake time at night. We found that, while there is value in an intervention that reduces the probability of feeding upon night waking to 70%, interventions that reduce the probability to 10% can reduce infant BMI by over 20 percentile points (e.g., 84th percentile to 62nd percentile), and further, infants maintained their BMI percentile between 6 and 12 months among caregivers who did not adaptively feed them based on their growth. Among caregivers who adaptively fed their infants, progressively reducing the probability of feeding by 10% each month showed the most stability in BMI percentile between months 6 and 12. Thus, our study showed that, as infants over the age of 6 months were fed less at night, they attained a lower BMI percentile at 12 months, which supports clinical guidance to night-wean infants as appropriate based on their health statuses and growth trajectories. These findings may be of interest to researchers and clinicians in the fields of child obesity, pediatric and behavioral sleep medicine, child psychiatry, developmental–behavioral pediatrics, and primary care. Although the paper was not intended to test specific hypotheses involving sleep disturbances and parental feeding decisions, it may serve as an impetus toward greater study of the inter-relationship between feeding and sleep issues in children.
Results also show that night feeding interventions had a more substantial impact for caregivers who did not adaptively feed their infant based on their growth compared to caregivers who did adaptively feed their infants. This may be because caregivers who did not adaptively feed their infants have more “room for improvement” and so the impact of the intervention is more prominent compared to interventions with caregivers who are already adjusting feeds, even if those adjustments are not directly tied to sleeping and waking.
Our model did not make any assumptions about what caregivers did when infants woke in the night rather than feeding, and interventions vary in what they train caregivers to do. This could entail other ways to soothe infants, often in conjunction with a larger responsive parenting curriculum12,34; some, conversely, encourage caregivers not to respond to night wakings at all, which is thought to encourage longer sleep durations and fewer night wakings35,36 but is not without controversy.37,38,39 However, reducing night feeding may be one of the simpler parenting interventions to follow, since caregivers do not have to learn to recognize cues to reduce the frequency they feed their infants at night.
It is known that a variety of factors contribute to excessive weight gain, so in considering the impact of changing any single behavior (e.g., reducing night feeding), a big picture perspective is important. This simulation shows that, especially for caregivers who are not adaptively feeding, reducing night feeding in response to awakening is one strategy that could help promote healthy growth, but alone might not move the needle. For caregivers who are already engaged in adaptive feeding, infants experience diminished changes to their average BMI percentile. Thus incorporating this strategy as one of several tools in a multi-component intervention for obesity prevention for very young children is likely the most promising opportunity for the biggest impact. One key contribution of the work is that it can inform how including this intervention component has the potential to impact BMI and which caregivers it might be most impactful for.
Limitations
All models, by definition, are simplifications of reality and do not include every possible variable. Sleep in infants is complex but has been simplified for the purpose of the model. For example, we did not include the potential effects of sleep on hunger and satiety hormones, which have been observed in other age groups but not quantified in infants.40,41,42 The entrainment of homeostatic, circadian, and ultradian rhythms, as well as the connections from sleep patterns to the hormonal regulation of stress and hunger, have all been less studied in infants than in adults. Macronutrient composition of food intake is not represented in the infant metabolic model, which may affect growth patterns. Physical activity is also challenging to study in infants and is represented simplistically.
Conclusion
This study shows that night feeding interventions could have a more substantial impact for caregivers who do not adaptively feed their infant based on their growth compared to caregivers who do adaptively feed their infants. While there is value in an intervention that reduces the probability of feeding upon night waking to 70%, interventions that reduce the probability to 10% could reduce BMI by over 20 percentile points (e.g., 84th percentile to 62nd percentile) among infants with caregivers who do not adaptively feed them based on their growth.
References
Taheri, S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch. Dis. Child. 91, 881–884 (2006).
Taveras, E. M. et al. Short sleep duration in infancy and risk of childhood overweight. Arch. Pediatr. Adolesc. Med. 162, 305–311 (2008).
Hart, C. N. & Jelalian, E. Shortened sleep duration is associated with pediatric overweight. Behav. Sleep Med. 6, 251–267 (2008).
Reilly, J. J. et al. Early life risk factors for obesity in childhood: cohort study. BMJ 330, 1357 (2005).
McDonald, L. et al. Sleep and nighttime energy consumption in early childhood: a population‐based cohort study. Pediatr. Obes. 10, 454–460 (2015).
Miller, M. A. et al. Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep 41, zsy018 (2018).
Magee, L. & Hale, L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med. Rev. 16, 231–241 (2012).
Snell, E. K., Adam, E. K. & Duncan, G. J. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 78, 309–323 (2007).
Nielsen, L., Danielsen, K. & Sørensen, T. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes. Rev. 12, 78–92 (2011).
Wake, M. et al. Does an intervention that improves infant sleep also improve overweight at age 6? Follow-up of a randomised trial. Arch. Dis. Child. 96, 526–532 (2011).
Taylor, B. J. et al. Targeting sleep, food, and activity in infants for obesity prevention: an RCT. Pediatrics 139, e20162037 (2017).
Savage, J. S. et al. Effect of the INSIGHT responsive parenting intervention on rapid infant weight gain and overweight status at age 1 year: a randomized clinical trial. JAMA Pediatr. 170, 742–749 (2016).
Paul, I. M. et al. Preventing obesity during infancy: a pilot study. Obesity 19, 353–361 (2011).
Field, T. Infant sleep problems and interventions: a review. Infant Behav. Dev. 47, 40–53 (2017).
Ferguson, M. C. et al. Can following formula-feeding recommendations still result in infants who are overweight or have obesity? Pediatr. Res. 88, 661–667 (2020).
Ferguson, M. C. et al. The impact of following solid food feeding guides on BMI among infants: a simulation study. Am. J. Prev. Med. 57, 355–364 (2019).
van Rossum, G. & Drake, F. L. Python Reference Manual (PythonLabs, 2001).
Hall, K. D. Modeling metabolic adaptations and energy regulation in humans. Annu. Rev. Nutr. 32, 35–54 (2012).
Rahmandad, H. Human growth and body weight dynamics: an integrative systems model. PLoS ONE 9, e114609 (2014).
Butte, N. F. Energy requirements of infants. Public Health Nutr. 8, 953–967 (2005).
Sadeh, A., Mindell, J. A., Luedtke, K. & Wiegand, B. Sleep and sleep ecology in the first 3 years: a web‐based study. J. Sleep Res. 18, 60–73 (2009).
Prell, C. & Koletzko, B. Breastfeeding and complementary feeding: recommendations on infant nutrition. Dtsch. Ärzteblatt Int. 113, 435 (2016).
Grummer-Strawn, L. M., Scanlon, K. S. & Fein, S. B. Infant feeding and feeding transitions during the first year of life. Pediatrics 122, S36–S42 (2008).
Casiday, R. E., Wright, C. M., Panter-Brick, C. & Parkinson, K. Do early infant feeding patterns relate to breast-feeding continuation and weight gain? Data from a longitudinal cohort study. Eur. J. Clin. Nutr. 58, 1290–1296 (2004).
Syrad, H., Johnson, L., Wardle, J. & Llewellyn, C. H. Appetitive traits and food intake patterns in early life. Am. J. Clin. Nutr. 103, 231–235 (2016).
Iglowstein, I., Jenni, O. G., Molinari, L. & Largo, R. H. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 111, 302–307 (2003).
Ball, H. L. Breastfeeding, bed‐sharing, and infant sleep. Birth 30, 181–188 (2003).
Brown, A. & Harries, V. Infant sleep and night feeding patterns during later infancy: association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breastfeed. Med. 10, 246–252 (2015).
Dewey, K. G. Nutrition, growth, and complementary feeding of the brestfed infant. Pediatr. Clin. North Am. 48, 87–104 (2001).
Butte, N. F. et al. Energy requirements derived from total energy expenditure and energy deposition during the first 2 y of life. Am. J. Clin. Nutr. 72, 1558–1569 (2000).
World Health Organization. WHO Growth charts - data table for girls length-for-age and weight-for-age charts. National Center for Health Statistics, Centers for Disease Control and Prevention, https://www.cdc.gov/growthcharts/who/girls_length_weight.htm (2010).
World Health Organization. WHO Growth charts - data table for boys length-for-age and weight-for-age charts. National Center for Health Statistics, Centers for Disease Control and Prevention, https://www.cdc.gov/growthcharts/who/boys_length_weight.htm (2010).
Douglas, P. S. & Hill, P. S. Behavioral sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review. J. Dev. Behav. Pediatr. 34, 497–507 (2013).
Toomey, E. et al. A collaborative approach to developing sustainable behaviour change interventions for childhood obesity prevention: development of the Choosing Healthy Eating for Infant Health (CHErIsH) intervention and implementation strategy. Br. J. Health Psychol. 25, 275–304 (2020).
Adair, R. et al. Reducing night waking in infancy: a primary care intervention. Pediatrics 89, 585–588 (1992).
St James-Roberts, I., Roberts, M., Hovish, K. & Owen, C. Video evidence that parenting methods predict which infants develop long night-time sleep periods by three months of age. Prim. Health Care Res. Dev. 18, 212–226 (2017).
Scher, A. Attachment and sleep: a study of night waking in 12‐month‐old infants. Dev. Psychobiol. 38, 274–285 (2001).
Blunden, S. L., Thompson, K. R. & Dawson, D. Behavioural sleep treatments and night time crying in infants: challenging the status quo. Sleep Med. Rev. 15, 327–334 (2011).
Gradisar, M. et al. Behavioral interventions for infant sleep problems: a randomized controlled trial. Pediatrics 137, e20151486 (2016).
Mullins, E. N. et al. Acute sleep restriction increases dietary intake in preschool‐age children. J. Sleep Res. 26, 48–54 (2017).
Leproult, R. & Van Cauter, E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr. Dev. 17, 11–21 (2010).
Hart, C. N. et al. Changes in children’s sleep duration on food intake, weight, and leptin. Pediatrics 132, e1473–e1480 (2013).
Acknowledgements
This project was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) via grant U01HD086861 and 5R01HD086013-02, as well as the NICHD and Office of Behavioral and Social Sciences Research (OBSSR) under award number U54HD070725, and the National Institute of General Medical Sciences (NIGMS) as part of the Models of Infectious Disease Agent Study (MIDAS) network under grant 1 R01 GM127512-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, U.S. Department of Health and Human Services, NICHD, NIGMS or OBSSR. None of the study sponsors had any role in the study design, collection, analysis, and interpretation of data, writing the report, nor the decision to submit the report for publication. This study was approved by the Johns Hopkins Bloomberg School of Public Health IRB (IRB #00006667).
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design; acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
O’Shea, K.J., Ferguson, M.C., Esposito, L. et al. The impact of reducing the frequency of night feeding on infant BMI. Pediatr Res 91, 254–260 (2022). https://doi.org/10.1038/s41390-021-01397-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01397-7