Abstract
Background
The United States Environmental Protection Agency (EPA) recently lowered residential floor and windowsill dust lead hazard standards, but maintained previous post-abatement clearance standards. We examined whether the discrepancy in these regulations places children at higher risk of lead poisoning.
Methods
In 250 children from Cincinnati, Ohio (2004–2008) living in homes built before 1978, we measured residential floor and windowsill dust lead loadings and blood lead concentrations at ages 1 and 2 years. Using linear regression with generalized estimating equations, we estimated covariate-adjusted associations of dust lead levels with blood lead concentrations and risk of lead poisoning.
Results
An increase in floor dust lead from 10 (revised dust lead hazard standard) to 40 μg/ft2 (post-abatement clearance standard) was associated with 26% higher (95% confidence interval (CI):15, 38) blood lead concentrations and 2.1 times the risk of blood lead concentrations ≥5 μg/dL (95% CI: 1.44, 3.06). Extrapolating our findings to US children age 1–5 years, we estimated that 6.9% (95% CI: 1.5, 17.2) of cases of blood lead concentrations ≥5 μg/dL are attributable to floor dust lead loadings between 10 and ≤40 μg/ft2.
Conclusions
The EPA’s residential dust lead regulations place children at increased risk of lead poisoning. We recommend adopting more protective dust lead standards.
Impact
-
We determined whether children are at increased risk of lead poisoning with the 2019 EPA residential post-abatement lead clearance standards being higher than dust lead hazard standards.
-
In this observational study, 2019 EPA dust lead clearance standards were associated with increased risk of lead poisoning compared to the revised dust lead hazard standard. Both EPA standards were associated with increased risk of lead poisoning compared to more stringent standards employed in our study.
-
Extrapolating our findings to US children, the 2019 EPA dust lead clearance standards could place up to 36,700 children at risk of lead poisoning.
Similar content being viewed by others
Introduction
Increasingly stringent regulations limiting environmental sources of lead and lead abatement of older housing have resulted in dramatic declines in childhood lead poisoning in the United States and internationally over the past five decades.1,2,3,4 However, 2–3% of US children still have blood lead concentrations above the Centers for Disease Control and Prevention (CDC) reference level of 5 μg/dL, defined as the 97.5th percentile of blood lead concentrations among US children ages 1–5 years.4,5 Overwhelming evidence indicates that childhood blood lead concentrations, even those below 5 μg/dL, are associated with cognitive impairments and behavioral disorders in childhood, as well as criminal arrests, psychopathology, and reduced earnings in adulthood.6,7,8,9,10,11
To protect children from lead poisoning, Congress mandated the US Environmental Protection Agency (EPA) to set health-based, residential dust lead hazard standards that define levels of lead on residential floors and windowsills that are hazardous to children and clearance standards for floors and windowsills that must be attained after abatement of residential lead hazards (Table 1). In June 2018, the Ninth Circuit Court of Appeals ordered the EPA to reduce the dust lead hazard standards.12,13 In July, 2019, the EPA lowered floor and windowsill dust lead hazard standards from 40 to 10 μg/ft2 and 250 to 100 μg/ft2, respectively (1 ft2 = 0.09 m2).14 However, the EPA maintained post-abatement floor (40 μg/ft2) and windowsill (250 μg/ft2) clearance standards that were established in 2001 and have historically been the same as the dust lead hazard standard.
With the EPA post-abatement clearance standards set higher than the health-based dust lead hazard standard, young children could be at increased risk of lead poisoning by continuing to live in homes with hazardous dust lead levels after abatement to EPA clearance standards.15 Thus, we estimated the potential effect of the discrepancy in these two regulatory standards on lead exposure among children age 1–2 years and compared them to a more protective standard used in the Health Outcomes and Measures of the Environment (HOME) Study by examining the relations of childhood blood lead concentrations and risk of lead poisoning with floor and windowsill dust lead levels.
Methods
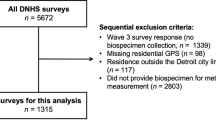
Between March 2003 and January 2006, we recruited pregnant women into a longitudinal pregnancy and birth cohort study, the HOME Study.16 We identified women living in the Cincinnati, OH region who attended one of nine prenatal practices affiliated with three hospitals. Eligibility criteria included 16 ± 3 weeks gestation, ≥18 years old, residing in a residence built in or before 1978, not living in a mobile/trailer home, HIV negative, not taking medications for seizures or thyroid disorders, planning to continue prenatal care and deliver at the collaborating clinics and hospitals, planning to live in the greater Cincinnati area for the next year, English fluency, and no diagnosis of diabetes, bipolar disorder, schizophrenia, or cancer resulting in radiation treatment or chemotherapy. To target children at increased risk of lead exposure, we enrolled women living in homes built before 1978 and oversampled women self-identifying as Black.17,18
Nested within the HOME Study is a randomized clinical trial of two interventions designed to reduce residential lead and injury hazards; we previously described the results of these trials.19,20 Briefly, we randomly assigned pregnant women to either the residential lead or injury hazard intervention.19,20 By 32 weeks gestation and before delivery, the lead hazard intervention group received a combination of activities designed to reduce residential lead exposure (see Supplemental Methods). We ensured that residences receiving the lead hazard intervention achieved floor and windowsill dust lead loadings ≤5 and 50 μg/ft2, respectively, following the intervention (Table 1). These levels were considerably lower than EPA dust lead hazard and clearance standards at the time (≤40 and ≤250 μg/ft2) and the recently revised EPA dust lead hazard standard (10 and 100 μg/ft2).21,22 Families assigned to the control group received an injury prevention intervention before children were age 6 months.19 For the present study, we used the observational components of this study and adjusted for the intervention in our analyses.
The institutional review boards of Cincinnati Children’s Hospital Medical Center and the participating delivery hospitals approved this study. Research assistants explained study protocols to prospective participants before obtaining written informed consent for women and their children to participate in the study and trial. This protocol information was registered with www.clinicaltrials.gov on August 11, 2005 (Identifier: NCT00129324).
Dust lead measurements
We measured floor and interior windowsill dust lead loadings in the main activity room, child’s bedroom, and kitchen using lead-free wipes, using the standard Department of Housing and Urban Development (HUD) protocol, at three times: before the intervention (i.e., baseline) and when children were ages 1 and 2 years.23 We collected three samples from each surface at each time point and analyzed them as a single composite. We attempted to sample the same floor area or window at each visit. Lead loadings (μg/ft2) were quantified using flame atomic absorption spectrometry or graphite furnace atomic absorption spectrometry. Our primary analysis focused on the floor and windowsill samples collected at ages 1 and 2 years. Laboratory staff were blinded to intervention status and children’s blood lead concentrations.
Blood lead concentrations
We collected whole blood from children at an average age of 1.1 (range 0.9–1.6) and 2.1 (range 1.8–2.4) years using lead-free materials. Blood samples were stored at −80 °C until they were shipped on dry ice to the CDC laboratories where blood lead concentrations were quantified using inductively coupled plasma mass spectrometry methods.24 All batches included reagent blanks and quality control (QC) samples (QC sample coefficient of variation <3.5%). Laboratory staff were blinded to intervention status and dust lead loadings.
Covariates
We adjusted for variables that could confound associations between dust lead loadings and blood lead concentrations, including maternal race, maternal education, child’s age at the time of blood lead measurement, child’s sex, season of blood/dust sample collection, age of home, secondhand tobacco smoke exposure (assessed using children’s serum cotinine concentrations), and intervention assignment.
Statistical analysis
We estimated covariate-adjusted geometric mean (GM) blood lead concentrations and risk of blood lead concentrations ≥5 μg/dL as a function of log2-transformed, time-varying dust lead loadings using linear and modified Poisson regression with generalized estimating equations, respectively.25,26 We modeled log2-transformed blood lead concentrations to satisfy normality assumptions of our model, and the GMs from these models can be interpreted in the same way as arithmetic means. From this model, we estimated GMs and risks of blood lead concentrations ≥5 μg/dL at the following floor and windowsill dust lead loadings: the current EPA post-abatement clearance regulatory standard (floors: 40 μg/ft2; windowsills: 250 μg/ft2), the newly revised EPA health-based dust lead hazard regulatory standard (floors: 10 μg/ft2; windowsills: 100 μg/ft2), and the clearance standard used in the HOME Study lead hazard intervention (floors: 5 μg/ft2; windowsills: 50 μg/ft2). We modeled the relation between continuous blood lead concentrations and dust lead loadings using linear and quadratic terms for dust lead loadings because we observed significant nonlinear associations for continuous blood lead concentrations (natural spline nonlinearity p values < 0.01). While there was not strong evidence of a nonlinear association for the risk of elevated blood lead concentrations, we obtained more plausible risk estimates when using both linear and quadratic terms (natural spline nonlinearity p values > 0.43).
Finally, we assessed the potential public health impact of the discrepancy in the EPA lead hazard standard and post-abatement clearance standard. To do so, we estimated the risk of blood lead concentrations ≥5 μg/dL among children living in homes with floor dust lead loadings of <10, 10–≤40, and >40 μg/ft2, with 10 and 40 μg/ft2 being EPA’s dust lead hazard standard and post-abatement clearance standard, respectively. Using these risks, we calculated the percent of children who would have blood lead concentrations ≥5 μg/dL (i.e., population attributable fraction [PAF]), assuming a counterfactual scenario where children who lived in residences with floor dust lead loadings of 10–≤40 μg/ft2 instead lived in residences with loadings ≤10 μg/ft2. We did this using previously reported prevalence of floor dust lead loadings in US homes built before 1978 and Hanley’s formula.27,28 We applied this PAF to the most recent (2010) population-based estimate of lead poisoning prevalence among 1–5-year-old children in the United States.4
Sensitivity analyses
We conducted three sensitivity analyses to assess the robustness of our results. First, we compared our unadjusted and adjusted associations to evaluate the magnitude of potential confounding present in our data. Second, we adjusted for children’s body surface area (m2) at the time of the blood lead measurement.29 Finally, we adjusted for average maternal blood lead concentrations during pregnancy. We measured whole blood concentrations in samples collected from women at 16 and 26 weeks’ gestation and shortly before or within 48 h of delivery using the methods described above.
Results
A total of 250 children with complete covariate data had 455 repeated dust and blood lead measurements at ages 1 and 2 years. The majority of children were female (54.4%) and born to non-Hispanic White (72.8%) and college-educated (58.8%) women (Table 2).
Median floor dust lead loadings at ages 1 and 2 years were an order of magnitude lower than median windowsill dust lead loadings (1.2 vs. 12 μg/ft2). Further, 6.8% and 1.5% of floor dust lead loadings were >10 and >40 μg/ft2, respectively, and 14.5% and 7.5% of windowsill dust lead loadings were >100 and >250 μg/ft2, respectively (Supplementary Table S1). Median blood lead concentrations were 1.5 μg/dL at both ages 1 and 2 years; 6.8% (n = 17) and 3.9% (n = 8) of children had blood lead concentrations ≥5 μg/dL at ages 1 and 2 years, respectively (Supplementary Table S2).
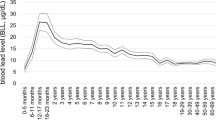
Blood lead concentrations and risk of blood lead concentrations ≥5 μg/dL were positively associated with floor and windowsill dust lead loadings, rising more steeply at higher loadings (Table 3, Figs. 1 and 2). GM blood lead concentrations were 26% (95% confidence interval (CI): 15, 38) and 11% (95% CI: 7, 16) higher at floor and windowsill dust lead loadings of 40 and 250 μg/ft2 (EPA post-abatement clearance standard), compared to loadings of 10 and 100 μg/ft2 (EPA dust lead hazard standard), respectively. At floor and windowsill dust lead loadings of 40 and 250 μg/ft2, the risk of blood lead concentration ≥5 μg/dL was 2.20 (95% CI: 1.40, 3.45) and 1.47 (95% CI: 1.28, 1.69) times that of the risk at loadings of 10 and 100 μg/ft2, respectively.
a Adjusted for maternal race (non-Hispanic White, non-Hispanic Black, and other), maternal education (high school or less, some college, and undergraduate/graduate degree), child age (continuous, years), child sex (male and female), season of blood sample collection (Winter/Spring and Summer/Fall), home age (pre-1940 and 1940–1977), intervention assignment (lead hazard group and injury hazard group), and child serum cotinine concentrations (continuous, log10 transformed). b Geometric means are derived from a covariate-adjusted model that included a linear and quadratic term for log2-transformed floor or windowsill dust lead loadings. Estimated GMs and risks are derived using mean-centered covariates. Estimated GMs are presented from the 1st to 99th percentile of floor and windowsill dust lead loadings. Blue shading indicates the 95% CI of the estimated GM. X-axis reference lines indicate floor/windowsill dust lead loadings of 5/50, 10/100, and 40/250 μg/ft2, which are the HOME Study dust lead standards, 2019 United States Environmental Protection Agency dust lead hazard standards, and 2019 United States Environmental Protection Agency post-abatement clearance standards, respectively.
a Adjusted for maternal race (non-Hispanic White, non-Hispanic Black, and other), maternal education (high school or less, some college, and undergraduate/graduate degree), child age (continuous, years), child sex (male and female), season of blood sample collection (Winter/Spring and Summer/Fall), home age (pre-1940 and 1940–1977), intervention assignment (lead hazard group and injury hazard group), and child serum cotinine concentrations (continuous, log10 transformed). b Estimated risks are derived from a mean-centered covariate-adjusted model that included a log2-transformed linear and quadratic terms for floor or dust lead loadings. Blue shading indicates the 95% CI of the risk estimates. Estimated risks are presented from the 1st to 99th percentile of floor and windowsill dust lead loadings. Blue shading indicates the 95% CI of the estimated GM. X-axis reference lines indicate floor/windowsill dust lead loadings of 5/50, 10/100, and 40/250μg/ft2, which are the HOME Study dust lead standards, 2019 United States Environmental Protection Agency dust lead hazard standards and 2019 United States Environmental Protection Agency post-abatement clearance standards, respectively.
GM blood lead concentrations and risk of having a blood lead concentrations ≥5 μg/dL was significantly higher among children living in homes with floor and windowsill dust lead loadings at the revised EPA dust lead hazard standard for floors (10 μg/ft2) and windowsills (100 μg/ft2) compared to the HOME Study clearance standards (floors: ≤5 μg/ft2 and windowsills: ≤50 μg/ft2) (Table 3).
Children who lived in homes with floor dust lead loadings >10 and ≤40 μg/ft2 had almost four times the risk (relative risk (RR): 3.95; 95% CI: 1.58, 9.87) of having a blood lead concentration ≥5 μg/dL compared with children who lived in homes with floor dust lead loadings ≤10 μg/ft2 (Table 4). Assuming that 2.6% of US homes built before 1978 have floor dust lead loadings >10 and ≤40 μg/ft2, 7.0% (95% CI: 1.5, 17.6) of cases of blood lead concentrations ≥5 μg/dL could be attributed to living in a home with floor dust loadings at these levels. Further, assuming that 2.6% of US children age 1–5 years have blood lead concentrations ≥5 μg/dL (n = 535,000), we estimated that ~36,700 cases of blood lead concentrations ≥5 μg/dL are related to floor dust lead loadings >10 and ≤40 μg/ft2.
In sensitivity analyses, the adjusted estimates were modestly attenuated compared to unadjusted estimates (Supplementary Table S3). Adjusting for children’s body surface area (Supplementary Table S4) or average maternal blood lead concentrations during pregnancy (Supplementary Table S5) did not meaningfully change the results.
Discussion
In this cohort, we observed that the discrepancy in the EPA’s newly revised health-based dust lead hazard standard and existing post-abatement clearance standard for residential floor and windowsill dust lead levels was associated with higher childhood blood lead concentrations and an increased risk of blood lead concentrations ≥5 μg/dL compared to a more protective standard we used in an intervention designed to reduce residential lead hazards. We estimate that up to 7% of cases of blood lead concentrations ≥5 μg/dL—potentially equivalent to ~36,700 US children—could be attributed to children continuing to live in homes with floor dust lead levels above the EPA dust lead hazard standard, but below the post-abatement clearance standard. Moreover, the 2019 EPA dust lead hazard standard does not adequately protect children from residential dust lead hazards; children were at 45% and 33% higher risk of having blood lead concentrations ≥5 μg/dL at the newly revised floor and windowsill dust lead hazards of 10 and 100 μg/ft2 compared to the HOME Study standards of 5 and 50 μg/ft2, respectively.
While the EPA proposes to lower the post-abatement floor and windowsill clearance standards to 10 and 100 μg/ft2, respectively, our results show that delays in reducing the current post-abatement clearance standard will place a significant number of children at increased risk of lead poisoning in the intervening period.15 For instance, a housing unit might have floor dust lead levels higher than the 2019 EPA health-based dust lead hazard standards of 10 μg/ft2 (e.g., 18 μg/ft2) and then undergo abatement to remediate lead hazards. Following abatement, an infant or child could continue be exposed to a floor dust lead level considerably higher than the revised health-based dust lead hazard standard, but lower than the 2019 EPA post-abatement clearance standard of 40 μg/ft2 (e.g., 39 μg/ft2). Even if EPA reduces the post-abatement clearance standards to 10 and 100 μg/ft2, this study and prior ones show that children would still be at significantly increased risk of lead poisoning.
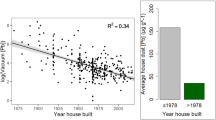
Historically, the US EPA residential dust lead hazard and post-abatement clearance standards have been based on adverse health effects, perceived feasibility to achieve compliance, and instrument detection limits (Table 1). Yet, other studies, and the present one, show that these standards fail to protect children from the risk of lead poisoning.30,31 Moreover, there is considerable evidence that it is feasible to achieve floor and windowsill dust lead levels lower than those required by the EPA, which would adequately protect children from the risk of lead poisoning.32 Using current lead hazard control practices, US Department of HUD grantees were able to achieve floor and windowsill dust lead levels of ≤5 and ≤40 μg/ft2 in 72% and 87% of surveyed housing units, respectively.32 This is, in part, why HUD has a lower post-abatement clearance standard than the 2019 EPA post-abatement clearance standard.33 Moreover, in the HOME Study, we demonstrated that our residential lead hazard intervention was able to further reduce floor and windowsill dust lead loadings to levels below 5 and 50 μg/ft2, respectively, in 100% of the homes assigned to the intervention.20 Given that older housing (i.e., pre-1978 construction) typically has more lead paint hazards, interventions reducing dust lead loadings in communities with a high prevalence of older housing units could have significant public health impacts (e.g., Northeastern US).34,35
Our results confirm that there is no threshold for the association of floor and windowsill dust lead loadings with children’s blood lead concentrations. Indeed, the risk of blood lead concentrations ≥5 μg/dL at floor dust lead loadings of 10 μg/ft2 was 45% higher than the risk at floor dust lead loadings of 5 μg/ft2 (risks: 0.05 vs. 0.07) This finding is consistent with earlier studies that reported positive associations between residential dust lead loadings and children’s blood lead concentrations, with no threshold.30,31 The most recent cross-sectional National Health and Nutrition Examination Survey (1999–2004) that included dust lead measurements indicates that floor dust lead loadings of 1 μg/ft2 are associated with a 3.8% prevalence of blood lead concentrations ≥5 μg/dL, approximately the risk we observed at ≤5 μg/ft2.28
Floor dust lead loadings in this study were more strongly associated with children’s blood lead concentrations than windowsill dust lead loadings, a phenomenon previously documented.36 This is likely because young children are closer to the floor and spend more time playing on the ground and engaging in hand-to-mouth behaviors with objects that have been placed on floors, relative to time spent playing on or mouthing windowsills.37 Windows may also serve as a reservoir of lead that drifts onto floors, thus making windows one of multiple determinants of floor dust lead levels.38
We note some limitations of the present study. First, there were a relatively small number of children with blood lead concentrations ≥5 μg/dL in the HOME Study. Despite this, we observed significantly increased risk of lead poisoning associated with elevated dust lead loadings. Relatedly, the current CDC 5 μg/dL reference value is not based on health hazards, but is defined by the 97.5th percentile from population-based biomonitoring. Thus, if this threshold is reduced in response to ongoing evaluations of the current reference value, then the proportion of children with elevated blood lead concentrations (defined by any new and lower reference value) attributable to residential dust lead exposure would be greater.39 Second, the risk estimates derived from this study and values used to calculate PAFs are based on data collected in the early 2000s. Thus, these results may not be entirely generalizable to young children today given declining lead exposure and blood lead concentrations. For instance, if the current prevalence of blood lead concentrations ≥5 μg/dL among US children age 1–5 years is 1.3% (n = 267,500), then ~18,400 cases of elevated blood lead concentrations would be attributable to floor dust lead loadings >10 and ≤40 μg/ft2. However, we used the most contemporaneous prospectively collected blood and dust lead data we are aware of to estimate the potential effect of low-level residential dust lead exposure on children’s blood lead concentrations. An additional limitation is that we used the dust lead loadings during childhood and not those taken after randomization (i.e., post clearance in the intervention arm) because the control arm of the study did not have these data. However, we speculate that dust lead loadings during childhood would be most strongly related to childhood blood lead concentrations relative to other time periods. Finally, there is the potential for residual confounding of the association between dust lead loadings and childhood blood lead concentrations. Our adjusted estimates were modestly attenuated relative to the unadjusted ones. Thus, if other factors that we did not adjust for were related to dust lead loadings and children’s blood lead concentrations (e.g., time spent at other locations or nutrition), then the true association may be weaker than what we observed.
Our results show that the discrepancy in the 2019 EPA health-based lead hazard and post-abatement clearance standards place children at heightened risk of lead poisoning. Moreover, our analyses show that the 2019 EPA health-based hazard standard is insufficient to protect children from residential lead hazards. Until the EPA dust lead hazard and post-abatement clearance regulatory standards are aligned with more protective standards to limit the preventable and harmful effects of lead exposure in children, public health professionals, clinicians, parents, and housing providers should engage in prevention activities to ensure that children are protected from residential lead hazards. We recommend that these stakeholders strive to achieve the more protective HOME Study standards that we have successfully implemented.
Change history
30 October 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41390-020-01229-0
References
Centers for Disease Control and Prevention. Lead: CDC’s National Surveillance Data (1997–2015) (Centers for Disease Control and Prevention, 2016).
Bellinger, D. C. & Bellinger, A. M. Childhood lead poisoning: the torturous path from science to policy. J. Clin. Invest. 116, 853–857 (2006).
Hwang, Y. H., Hsiao, C. K. & Lin, P. W. Globally temporal transitions of blood lead levels of preschool children across countries of different categories of Human Development Index. Sci. Total Environ. 659, 1395–1402 (2019).
Centers for Disease Control and Prevention. Blood lead levels in children aged 1–5 years—United States, 1999–2010. MMWR Morb. Mortal Wkly Rep. 62, 245–248 (2013).
ACoCLP Prevention. Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention (Centers for Disease Control and Prevention, 2012).
Reuben, A. et al. Association of childhood lead exposure with adult personality traits and lifelong mental health. JAMA Psychiatry 76, 418–425 (2019).
Reuben, A. et al. Association of childhood blood lead levels with cognitive function and socioeconomic status at age 38 years and with IQ change and socioeconomic mobility between childhood and adulthood. JAMA 317, 1244–1251 (2017).
Lanphear, B. P. et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ. Health Perspect. 113, 894–899 (2005).
Braun, J. M. et al. Exposures to environmental toxicants and attention deficit hyperactivity disorder in U.S. children. Environ. Health Perspect. 114, 1904–1909 (2006).
NT Program. Health Effects of Low-Level Lead (US Department of Health and Human Services, 2012).
Wright, J. P. et al. Association of prenatal and childhood blood lead concentrations with criminal arrests in early adulthood. PLoS Med 5, e101 (2008).
USCoAftN Circuit. A Community Voice v. EPA, No. 16-72816, Order (2018).
USCoAftN Circuit. A Community Voice v. EPA, No. 16-72816, Opinion (2017).
Wheeler, A. Review of the Dust-Lead Hazards Standards and the Definition of Lead-Based Paint (USEP Agency, 2019).
NTP Program. NTP monograph on health effects of low-level lead. NTP Monogr. 1, xiii, xv-148 (2012).
Braun, J. M. et al. Cohort profile: the Health Outcomes and Measures of the Environment (HOME) study. Int. J. Epidemiol. 46, 24 (2017).
Raymond, J. et al. Lead screening and prevalence of blood lead levels in childrenaged 1-2 years—Child Blood Lead Surveillance System, United States, 2002–2010 and National Health and Nutrition Examination Survey, United States, 1999–2010. MMWR Suppl. 63, 36–42 (2014).
Levin, R. et al. Lead exposures in U.S. Children, 2008: implications for prevention. Environ. Health Perspect. 116, 1285–1293 (2008).
Phelan, K. J. et al. A randomized controlled trial of home injury hazard reduction: the HOME injury study. Arch. Pediatr. Adolesc. Med. 165, 339–345 (2011).
Braun, J. M. et al. Effect of residential lead-hazard interventions on childhood blood lead concentrations and neurobehavioral outcomes: a Randomized Clinical Trial. JAMA Pediatr. 172, 934–942 (2018).
USEP Agency. Lead; Identification of Dangerous Levels of Lead; Final Rule. 40 CFR Part 745. Federal Register 1205–1240 (2001).
USDoHaU Development. Revised Dust-Lead Action Levels for Risk Assessment and Clearance; Clearance of Porch Floors (USDoHaU Development, 2017).
HUD. Evaluation and Control of Lead-Based Paint Hazards in Housing (US Department of Housing and Urban Development, Washington, 1995).
Jones, D. R. et al. Analysis of whole human blood for Pb, Cd, Hg, Se, and Mn by ICP-DRC-MS for biomonitoring and acute exposures. Talanta 162, 114–122 (2017).
Zou, G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 159, 702–706 (2004).
CACoCLP Prevention. Low Level Lead Exposure Harms Children: A Renewed Call For Primary Prevention (US Department of Health and Human Services, CDC, Atlanta, 2012).
Hanley, J. A. A heuristic approach to the formulas for population attributable fraction. J. Epidemiol. Community Health 55, 508–514 (2001).
Dixon, S. L. et al. Exposure of U.S. children to residential dust lead, 1999–2004: II. The contribution of lead-contaminated dust to children’s blood lead levels. Environ. Health Perspect. 117, 468–474 (2009).
Haycock, G. B., Schwartz, G. J. & Wisotsky, D. H. Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J. Pediatr. 93, 62–66 (1978).
Lanphear, B. P. et al. The contribution of lead-contaminated house dust and residential soil to children’s blood lead levels. A pooled analysis of 12 epidemiologic studies. Environ. Res. 79, 51–68 (1998).
Lanphear, B. P. et al. Lead-contaminated house dust and urban children’s blood lead levels. Am. J. Public Health 86, 1416–1421 (1996).
HUD. Lead Hazard Control Survey (US Department of Housing and Urban Development, Office of Lead Hazard Control and Healthy Homes). https://www.hud.gov/sites/documents/CLEARANCESURVEY_24OCT15.PDF (2015).
USDoHaU Development. Revised Dust-Lead Action Levels for Risk Assessment and Clearance; Clearance of Porch Floors (USDoHaU Development, Washington, 2017).
Gaitens, J. M. et al. Exposure of U.S. children to residential dust lead, 1999–2004: I. Housing and demographic factors. Environ. Health Perspect. 117, 461–467 (2009).
Jacobs, D. E. et al. The prevalence of lead-based paint hazards in U.S. housing. Environ. Health Perspect. 110, A599–A606 (2002).
Lanphear, B. P., Hornung, R. & Ho, M. Screening housing to prevent lead toxicity in children. Public Health Rep. 120, 305–310 (2005).
Bearer, C. F. How are children different from adults? Environ. Health Perspect. 103(Suppl. 6), 7–12 (1995).
Clark, S. et al. Occurrence and determinants of increases in blood lead levels in children shortly after lead hazard control activities. Environ. Res. 96, 196–205 (2004).
Paulson, J. A. & Brown, M. J. The CDC blood lead reference value for children: time for a change. Environ. Health 18, 16 (2019).
Acknowledgements
The HOME Study was supported by grants from the National Institutes of Environmental Health Sciences (P01 ES011261 and R01 ES014575) and United States Environmental Protection Agency (RD—83544201). Housing remediation costs were supported by the United States Department of Housing and Urban Development through an interagency agreement.
Author information
Authors and Affiliations
Contributions
K.Y., N.N., D.E.J., and B.P.L. contributed to the study conception and design, as well as acquisition of the data. J.M.B. conducted the statistical analyses and drafted the manuscript. J.M.B., K.Y., N.N., D.E.J., M.T., and B.P.L. all contributed to the interpretation of the data and revising the manuscript. All authors approve of the submitted version.
Corresponding author
Ethics declarations
Competing interests
B.P.L. served as an expert witness in cases related to childhood lead poisoning, but he has not personally received any compensation for these services. J.M.B. was financially compensated for serving as an expert witness for plaintiffs in litigation related to tobacco smoke exposures and received a honoraria for serving on an advisory board to Quest Diagnostics. M.T. was compensated for providing expert advice to lawyers in cases related to childhood lead poisoning and to the New South Wales EPA Broken Hill Environmental Lead Program. D.E.J. was compensated providing expert testimony in lead poisoning cases. N.N. receives research funding from Meridian Biosciences and was compensated for providing expert advice in a lead exposure case. The authors have no conflicts of interest.
Informed consent
Research assistants explained study protocols to prospective participants before obtaining written informed consent for women and their children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Braun, J.M., Yolton, K., Newman, N. et al. Residential dust lead levels and the risk of childhood lead poisoning in United States children. Pediatr Res 90, 896–902 (2021). https://doi.org/10.1038/s41390-020-1091-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1091-3
This article is cited by
-
Associations between perfluoroalkyl acids in serum and lead and mercury in whole blood among US children aged 3–11 years
Environmental Science and Pollution Research (2021)