Abstract
Background
The objective was to determine the association between perioperative risk factors and brain imaging abnormalities on neurologic outcome in neonates with hypoplastic left heart syndrome (HLHS) or d-Transposition of the great arteries (d-TGA) who underwent cardiac surgery including cardiopulmonary bypass.
Methods
A retrospective analysis of neonates with HLHS or d-TGA undergoing cardiac surgery including cardiopulmonary bypass between 2009 and 2017 was performed. Perioperative risk factors and Andropoulos’ Brain Injury Scores from pre- and postoperative brain magnetic resonant images (MRI) were correlated to outcome assessments on patients between 5 and 23 months of age. Neurologic outcome was measured using the Pediatric Stroke Outcome Measure (PSOM) and Pediatric Version of the Glasgow Outcome Scale-Extended (GOS-E).
Results
Fifty-three neonates met our enrollment criteria (24 HLHS, 29 d-TGA). Mechanical ventilation > 12 days and DHCA > 40 min were associated with worse outcome. MRI measures of brain injuries were not associated with worse outcome by PSOM or GOS-E.
Conclusion
For HLHS and d-TGA patients, duration of mechanical ventilation and DHCA are associated with adverse neurologic outcome. Neonatal brain MRI commonly demonstrates acquired brain injuries, but the clinical impact of these abnormalities are not often seen before 2 years of age.
Impact
-
Acquired brain injury is common in high-risk neonates with CHD but poor neurological outcome was not predicted by severity of injury or lesion subtype. Longer stay in ICU is associated with postoperative brain injuries on MRI.
-
Total duration of ventilation > 12 days is predictive of adverse neurological outcome scores.
-
DHCA > 40 min is associated with adverse neurological outcome scores.
-
Neurological outcome before 2 years of age is more affected by the clinical course than by cardiac diagnosis.
Similar content being viewed by others
Introduction
Congenital heart defects are the most common birth defects seen worldwide. The incidence of moderate to severe congenital heart disease (CHD) is estimated to be 6/1000 live birth.1
With advances in prenatal diagnosis of CHD, surgical techniques, cardiopulmonary bypass (CPB) and the perioperative care of patients, the mortality of children with CHD has declined significantly over the last two decades.2
Morbidity, however, remains high, with 30–50% of patients suffering some degree of neurodevelopmental disability.3,4,5 Despite great efforts invested to maximize neurological outcome, brain injury remains the most common extracardiac complication of patients undergoing cardiac surgery.6 White matter injury (WMI) is the most common cerebral injury subtype found in neonates with CHD.7 Andropoulos et al.8 demonstrated that brain immaturity in neonates with CHD is significantly associated with pre- and postoperative brain injury, especially WMI. Fetal studies have shown abnormal brain development and cerebral blood flow in fetuses with CHD.9,10,11,12 Limperopoulos et al.13 provided the first in vivo evidence that impairment of fetal brain growth in fetuses with CHD has its onset in the third trimester. McQuillen et al.14 suggest that failures in brain oxygen and nutrient delivery due to the underlying heart defect and alterations in fetal blood flow lead to the impairments of fetal brain growth. Moreover, the oligodendrocytes that have high activity levels in the third trimester are excessively vulnerable for hypoxia/ischemia, infection, hyperoxia or anesthetic drugs, which increases the risk of hypoxic and oxidative injuries to the white matter in CHD patients due to decreased brain oxygen delivery caused by the underlying cardiac defect.15
Nonmodifiable patient characteristics like CHD subtype, chromosomal anomalies and socioeconomic status are reported to be strong predictors of adverse neurodevelopmental outcome of children with CHD.3,16,17,18 Over the last two decades several studies have sought to improve outcomes by identifying modifiable risk factors as well. Deep hypothermic circulatory arrest (DHCA) for >40 min, longer stay in intensive care unit (ICU) and the duration of ventilation are found to be associated with adverse neurological outcome.19,20,21 Many risk factors for neurodevelopmental disability are also associated with a higher incidence of brain injury seen on magnetic resonance imaging (MRI).5,8,22 Multiple studies have demonstrated a high incidence of both brain injury and abnormal neurodevelopmental outcome in CHD patients, yet little is known about the direct impact of structural brain injury on neurodevelopmental outcome in this population.
In this study we investigated the impact of pre- and postoperative brain injuries on neurological outcome in neonates with hypoplastic left heart syndrome (HLHS) or d-Transposition of the great arteries (d-TGA). Clinical risk factors known to be associated with neurological outcome were also assessed for impact on brain injury in the postoperative period.
Methods
Patient cohort
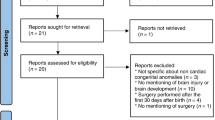
This is a retrospective study of patients receiving congenital heart surgery with CPB during the first month of life. Consecutive patients with a diagnosis of HLHS or d-TGA born between 2009 and 2017 who underwent an open heart surgery with CPB at Children’s National Medical Center in Washington DC within their first month of life were included. Only subjects with pre- and postoperative brain MRIs were enrolled in the study. Patients with gestational age <36 weeks at birth, genetic abnormalities known to be associated with abnormal neurodevelopment, congenital brain abnormalities and/or multiple congenital anomalies were excluded. Patients with incomplete MRIs were also excluded (minimum required sequences: DWI, T2, T1).
The study was approved by the Children’s National Medical Center Institutional Review Board in Washington DC.
Clinical data
Medical records for all subjects were reviewed to extract patient characteristics and clinical data: Perioperative data, collected from electronic medical records, included gestational age (GA), APGAR scores, birth weight and head circumference, age at time of preoperative MRI, length of stay in the ICU, length of hospital stay, duration of intubation and mortality. Intraoperative data, including age and weight at intervention, time of CPB, aortic cross-clamp time, time of DHCA and type of procedure, were also recorded.
MR imaging
Magnetic resonance imaging studies were done pre- and postoperatively on either a 1.5 T (Discovery MR450; GE Healthcare, Waukesha, Wisconsin or Siemens Avanto, Erlangen, Germany) or 3.0 T scanner (Discovery MR750; GE Healthcare, Waukesha, Wisconsin). Scans were obtained clinically as per the institutional routine in all patients. The scans included standard T1- and T2-weighted images, diffusion-weighted imaging, susceptibility-weighted images and magnetic resonance spectroscopy. Postoperative scans were most commonly done in the days prior to discharge once the patients were stable and pacing wires were removed.
MRI analysis
Magnetic resonance images were scored by two clinicians familiar with brain injury associated with CHD, one a pediatric neuroradiologist, the other a pediatric neurologist. Scores were assigned retrospectively and outside of regular clinical practice but because the images were not deidentified, clinicians were not considered blinded. Pre- and postoperative MR images were graded according to a scoring system devised by Andropoulos et al.8 Brain injury was divided into eight categories: WMI, infarction (ischemic stroke), intraparenchymal hemorrhage, punctate lesions, elevated lactate on MR spectroscopy, intraventricular hemorrhage (IVH), subdural hemorrhage and dural sinovenous thrombosis. The subcategories were scored for severity based on Andropoulos’ scorings system—0 for none, 1 for mild, 2 for moderate and 3 for severe. For the total brain injury score, the scores in each category were multiplied by a proposed outcome significant multiplier: 3 for WMI, infarction or intraparenchymal hemorrhage; 2 for punctate lesions or increased lactate on MRS; and 1 for IVH, subdural hemorrhage, dural sinovenous thrombosis. A total brain injury score of 0 represents no injury; a score of 1–5 mild injury, 6–10 moderate injury and >10 severe injury (Supplementary Material).
Measures of neurologic outcome
At our institution, neonates with CHD including surgery with CPB are scheduled for appointments with a pediatric neurologist and developmental psychologist after discharge as part of the Cardiac Neurodevelopmental Outcome (CANDO) program. Based on assessments from these clinical appointments, two different outcome scores were assigned to quantify the neurologic outcome of the patients.
The Pediatric Stroke Outcome Measure (PSOM) is a measure of neurologic deficits, using five categories: sensorimotor function, expressive language, language comprehension, behavior/state regulation and cognition. Each category has four different scores: 0 for no deficit, 0.5 for mild deficit, 1 for moderate deficit and decreased function, or 2 for severe deficit and missing function (Table 1).23 Normal to mild deficits were classified as good outcome, moderate and severe deficits were classified as poor outcome.
Functional scores were assigned using the Pediatric version of the Glasgow Outcome Scale-Extended (GOS-E Ped) modified by Beers et al. The score is a measure of functional outcome of patients <17 years of age after brain injury.24 It evaluates the functional independence inside and outside the home, capacity for school, participation in social and leisure activities and psychological problems with an impact on the interaction with family or friends. The GOS-E Ped was divided into eight categories ranging from 1 = upper good recovery/normal to 8 = death.
Statistical analysis
Univariate analyses were performed with the Mann–Whitney U test for continuous (non-normally distributed) variables, Student’s t tests for normally distributed variables and Fisher’s exact test for categorical or binary variables to evaluate differences between HLHS and d-TGA groups. Changes for HLHS and d-TGA in ordinal brain injury scores between preop and postop were assessed by the Wilcoxon signed-ranks test and presented as median scores and interquartile ranges (IQR). Diagnosis, duration of DHCA, ICU length of stay, duration of ventilation and preoperative total injury score were analyzed as candidate predictors of adverse neurologic outcome. Backwards stepwise multivariable logistic regression modeling with the likelihood ratio test used to assess significance (threshold of p < 0.05 was used for entry and p < 0.10 for removal from the model) was used to define risk factors for worse GOS-E and PSOM scores and derive odds ratios and 95% confidence intervals. It was also used to identify independent risk factors for moderate to severe postoperative brain injuries (total brain injury score ≥ 6). Receiver operating characteristic curve analysis was applied to identify optimal cut-off values of continuous predictor variables using the Youden J-index. To identify candidate predictors of moderate to severe postoperative WMI, infarction and intraparenchymal hemorrhage, the subcategories were analyzed as binary categories. PSOM scores were grouped as normal/mild deficits (scores 0–1) and moderate/severe deficits/death (scores 2–4). GOS-E scores were divided into good recovery (score 1 or 2) and moderate to severe disabilities (scores 3–8). Statistical analysis was performed using IBM SPSS Statistics (version 24.0, IBM Corporation, Armonk, NY). Two-tailed values of p < 0.05 were considered statistically significant without any adjustments for multiple testing and multiple endpoints and therefore should be regarded as exploratory evidence.
Results
Fifty-three patients met our criteria and were included in the study. Twenty-four with the diagnosis of HLHS and twenty-nine with the diagnosis of d-TGA underwent open heart surgery in the time between 2009 and 2017 at Children’s National Medical Center in Washington DC, USA. The characteristics of the cohort are summarized in Table 2.
Variables from the clinical course of our cohort are presented in Table 3.
Twenty three of 29 patients with d-TGA (79%) required balloon atrial septostomy (BAS) before surgery (age = 973 ± 2090 min). No patients with HLHS had a catheter intervention to open the atrial septum prior to surgery.
Two patients (8%) with HLHS required postoperative extracorporeal membrane oxygenation (ECMO) and one patient with d-TGA (3%). Two patients with HLHS had a cardiac arrest after surgery, of which one required ECMO. No patient with d-TGA had a postoperative cardiac arrest. All patients with postoperative ECMO and/or cardiac arrest survived the first 2 years of life.
Four patients (17%) with HLHS died, three within the first year of life (17, 19 and 35 weeks of age) and one at 82 weeks of age. One hundred percent in the group of d-TGA survived the first 2 years of life.
Brain injury scores
The preoperative MRIs were done on day of life 2 ± 1.8 and the postoperative scans 25 ± 20 days after surgery. Preoperative brain injuries were present in 53% of all patients (40% HLHS; 63% d-TGA). The most common preoperative brain injuries in the group of HLHS were IVH (20%), WMI (20%) and infarctions (16%), whereas subdural hemorrhage (27%) and WMI (23%) were the most frequently seen injuries in patients with d-TGA. Two patients with d-TGA (7%) had preoperative infarction. The median preoperative total brain injury score for the HLHS group was 0 (IQR 0–3) and 1 (IQR 0–3) for the d-TGA group. Sixteen patients (30%) had no preoperative and only postoperative lesions noted on MRI (9 HLHS, 7 d-TGA). New lesions (defined as an increase in number or size of preoperative lesions or new type of lesion) were seen in 30 out of 53 patients (57%). The incidence of postoperative brain abnormalities was 72% in patients with HLHS and 77% in patients with d-TGA. The most common new postoperative brain injuries were WMI (33%) and infarction (33%) for HLHS patients and punctuate lesions (26%) and SDH (22%) for d-TGA patients (see Table 4). The median postoperative total brain injury score for the HLHS group was 4 (IQR 1–8) and 3 (IQR 1–5) for the group of d-TGA.
Pre- and postoperative brain MRI findings are summarized in Table 4.
A significant increase of the total brain injury score from preoperative to postoperative was seen in both cardiac diagnosis groups (HLHS: p = 0.006, d-TGA: p = 0.017).
A diagnosis of HLHS correlated with an increased risk for moderate to severe postoperative infarction (size > one-third of a vascular territory in one hemisphere) (p = 0.017). The length of stay in ICU was significantly associated with a moderate to severe total injury score (total score ≥ 6) on postoperative brain MRI (p < 0.001). Among the 17 patients with a moderate to severe postoperative total injury score (≥6), the median (IQR) cardiac ICU time was 33 days (21–55 days) compared to 14 days (10–22 days) for the other 36 patients with postoperative injury scores < 6 (p < 0.001).
Of note, BAS was not associated with an increased risk for preoperative brain injury in the d-TGA group. Specifically, patients with d-TGA, who underwent a BAS, neither show a higher preoperative total brain injury score (p = 0.934), nor a higher preoperative prevalence of WMI (p = 0.380), infarction (p = 0.910) or intraparenchymal hemorrhages (p = 0.070) compared to patients without BAS.
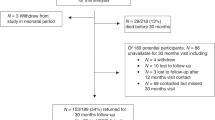
Neurologic outcomes
Eight patients were lost to follow-up. Forty-five out of 53 patients (85%) underwent a neurologic assessment between 5 and 23 months of age. The median age of neurologic assessment was 10 ± 6 months.
An abnormal assessment was seen in 49% of the patients, whereby 82% of the HLHS patients and 17% of the d-TGA patients had an abnormal examination.
PSOM and GOS-E scores were highly correlated with each other (rs = 0.916, p < 0.001).
The mean PSOM scores were 1.82 ± 1.296 for the HLHS group and 0.25 ± 0.608 for the d-TGA group. The mean GOS-E scores were 3.86 ± 2.122 in patients with HLHS and 1.54 ± 0.932 in patients with d-TGA.
The multivariable logistic regression analyses showed a significant correlation between DHCA longer than 40 min (odds ratio (OR) = 11.6; 95% Cl, 2.0–74.7; p = 0.005) and total duration of ventilation more than 12 days (OR = 17.9; 95% Cl, 2.8–113.3; p < 0.001) and moderate to severe deficits based on PSOM scores (Fig. 1).
DHCA more than 40 min (OR = 14.3, 95% Cl, 2.5–84.7, p < 0.001) and a total duration of ventilation more than 12 days (OR = 13.9; 95% Cl, 2.3–84.0; p = 0.002) were also predictive for moderate to severe disabilities based on GOS-E scores (Fig. 2).
Of note, 75% of the patients with DHCA time more than 40 min showed a total injury score ≥ 1 on postoperative brain MRI.
ICU length of stay more than 24 days (PSOM: p = 0.724; GOS-E: p = 0.860) and moderate to severe preoperative brain injuries (PSOM: p = 0.359; GOS-E: p = 0.787) were neither predictive for worse PSOM scores nor for worse GOS-E scores (Table 5).
Discussion
In this retrospective study, we evaluated the impact of patient characteristic, clinical factors and structural brain injury severity on neurological outcome within the first 2 years of life. Abnormal brain MRI findings were present in 53% of the patients prior to surgery and 73% after surgery. New postoperative findings were seen in 55%. The most common brain MRI findings were IVH, WMI and infarctions in the group of HLHS and WMI in patients with d-TGA. The incidence of perioperative brain injuries in our study is concordant with other studies.8,21,22
Independent risk factors for adverse neurological outcome in our cohort were DHCA > 40 min and longer duration of ventilation, which is also consistent with previously published studies.19,20,21
In 2007, McQuillen et al. reported a high rate of new postoperative brain lesions with WMI predominance in their study of 62 patients with CHD. New acquired brain injury in their study cohort were primarily seen in patients with single ventricles who underwent a Norwood procedure.22 In our study, we also noted a high rate of new postoperative lesions (57% of the patients), including a high prevalence of WMI. However, in our cohort, new postoperative lesions subtypes varied based on the CHD diagnosis. Specifically, infants with either HLHS or d-TGA were found to have similar total brain injury scores but differences in injury subcategories were noted. For example, a greater incidence of hemorrhage in the d-TGA group was noted on the postoperative scans. Microhemorrhage, intraventricular hemorrhage and subdural hemorrhage were most commonly seen, all which historically are less likely to impact neurological outcome.8,25 Newly acquired postoperative injuries found in the HLHS cohort, however, were primarily WMI and infarction.
Prior studies have shown an increased risk of infarction after BAS,26,27 but this association is not consistent in the literature.28,29,30 Kelly et al.31 suggest that the patients who undergo BAS have the greatest burden of hypoxia and are therefore at higher risk of brain injuries. Perhaps the failure to consistently demonstrate increased injury in this vulnerable population relates to the timing of the BAS and the associated supportive care received. BAS was not associated with an increased risk for preoperative brain injury in our cohort, including infarction, WMI and hemorrhage which may be a reflection of our center’s high rate of early BAS and cardiac-focused perinatal care.
In univariate analysis, infants with HLHS were identified to have worse neurological outcome compared to those with d-TGA but CHD subtype did not predict outcome in the multivariate analysis. These groups differed significantly in terms of operative and perioperative management. Infants with HLHS had a longer duration of pre- and postoperative ventilation as well as longer stay in ICU. Other studies have also described differences in developmental outcome for single ventricle CHD and d-TGA patients using univariate regression analysis.18,21,32 However, similar to our cohort, these studies were also unable to confirm this finding in a multivariate regression analysis. In repeated analyses, the clinical factors appear to surpass the CHD diagnosis as stronger predictors of adverse neurodevelopmental outcome.21,32 Perhaps, future larger studies using a more substantive tool for measuring outcome, like the Bayley Score of Infant Development and/or multivariate regression analyses, may better determine the association between CHD diagnosis and adverse outcome.
Several studies over the last two decades have defined risk factors associated with perioperative brain injury and adverse neurodevelopmental outcome in children with CHD.3,8,20,26,32
Historically there have been concerns that the use of DHCA increases the risk of perioperative brain injury and adverse neurodevelopmental outcome in children with CHD. However, there are a growing number of studies that suggest a limited period of DHCA does not affect the neurodevelopmental outcome.19,33 Investigators from the Boston Circulatory Arrest Trial concluded that only a duration of DHCA beyond 41 min affects the neurodevelopmental outcome.19 Our results support the concept that DHCA > 40 min is an independent risk factor for poor neurologic outcome
Despite the many investigations of risk factors for perioperative brain injury and adverse neurodevelopmental outcome in the CHD population, the relationship between structural brain injury and abnormal neurological outcome is still not well understood.
Beca et al.34 performed the largest study to date, investigating the impact of brain injuries on neurodevelopmental outcome. In this multicenter study, they examined 153 infants with mixed CHD diagnosis, who underwent congenital heart surgery with or without CPB and evaluated the neurodevelopmental outcome at 2 years of age using the third edition of the Bayley Scales of Infants and Toddler Development (Bayley-III). Brain MRI findings were classified as focal infarction, WMI or hemorrhage. A correlation between the Bayley Scales and brain injuries was not found. They noted the diagnostic group as the strongest predictor for new postoperative WMI. Similar to the results of our study, Beca et al. showed that single ventricle patients are at greatest risk for new postoperative WMI.
More recently, Claessens et al.35 reported an association between perioperative brain injury, especially WMI, and reduced brain volumes with adverse cognitive, behavioral and motor outcome at 2 years of age. These findings confirm the findings of Andropoulos et al., who also described an association between new postoperative WMI and worse cognitive outcome at 12 months of age in a group of varying types of CHD.20 Compared to Beca et al., who analyzed brain injury only as a dichotomous predictor, Claessens et al. also included brain volumes and cortical measures, such as the inner cortical surface and a gyrification index. Neonates with worse neurodevelopmental outcome showed smaller brain volumes and decreased cortical measures in this study.35 The impacts of altered cerebral development and acquired brain injury on the neurodevelopmental outcome of CHD patients are complex and multifaceted. Inconsistencies in the literature may indicate variations among CHD subtypes and the postnatal care received that still need to be explored.
Of note is that, Peyvandi et al. recently suggested that the timing of neurodevelopmental assessment could influence the predictive value of brain injuries on neurological outcome. They showed that only clinical factors, such as cardiac lesion, BAS and maternal education, were associated with worse 12 months Bayley Scales. However, brain injury scores were significantly associated with lower Bayley Scales at 30 months follow-up.36 McGrath et al. further described neurodevelopmental evaluations at 1 year of age modestly predict the status at school-age, thus cautioning long-term follow-up is necessary to predict the risk for adverse developmental outcome. In their study, they demonstrated that children with d-TGA with deficits at 8 years of age frequently have a normal performance at 1 year of age.37 These findings could help explain why we did not find an association between brain injuries and neurological outcomes within the first 2 years of life in our cohort. A correlation could possibly be demonstrated on follow-ups beyond 24 months of age when cognitive and language skills are more accurately tested. Also, patients with HLHS typically undergo multiple surgeries with CPB. Therefore, neurodevelopmental testing in the first 2 years of life may underestimate the cumulative impact of hospital time and of multiple surgeries on performance at school-age. Moreover, assessment of neurodevelopmental outcome using the Bayley Score of Infant Development, the gold standard for the assessment of outcome of infants, may have allowed for a better correlation between brain injuries and neurodevelopmental outcome within the first 2 years of life.
The present study has several limitations. It was a single-center study with a retrospective study design and a small sample size, which limits the statistical power of the analysis. Furthermore, we do not have a control group of either healthy neonates or CHD patients without DHCA or CPB. Only patients with pre- and postoperative MRI scans were included. Therefore, the sickest neonates may be excluded, either because they were not stable enough to undergo a preoperative MRI scan or they died after surgery and for this reason did not undergo a postoperative MRI examination. Moreover, preoperative brain MRI exams were first included into our routine clinical practice in 2009. The consistency of these screening MRIs improved as the program developed and became more standardized. As a result, the patients receiving clinically indicated brain MRIs may have included more screening MRIs over time.
Also, in order to capture a homogeneous group of patients for comparison of clinical variables, we did not include patients born prior to 36 weeks gestation. Because we did not include babies born at <36 weeks in our analysis, our findings may not be applicable to all d-TGA and HLHS patients treated with surgery in the neonatal period.
Also, as our patients were not sedated for their MRI study, they needed to be clinically stable before the scan could be obtained safely. Consequently, the time between surgery and the postoperative MRI scan is variable. The MRI scans for d-TGA patients were on average 2 weeks earlier compared to the HLHS group. The inconsistency in the timing of the postoperative scan may have impacted certain aspects of the scoring, especially in the subcategories IVH, MRS and subdural hemorrhage, which were more commonly seen in the d-TGA group. Also, WMI lesions can become less visible with time.
Eight patients were lost for follow-up and did not have outcome scores assigned which is a significant portion of total patients in this small cohort and may have impacted the analysis. Also, the age range used for assigning neurological outcome covers a broad range of early development that likely impacted sensitivity of the testing. Follow-up assessments were made over a broad range of ages (5–23 months). Due to normal developmental progressions, assessment in infancy is less sensitive at detecting deficits than those obtained in toddlers. Also, due to the retrospective design of the study, the Bayley Score of Infant Development, a more substantive tool for measuring development, was not used. To compensate for the inherent limitations of a retrospective assessment, we chose two complimentary measures of outcome: the PSOM that emphasizes the neurological examination and the GOS-E Peds that focuses on functional outcome. Also, scores were assigned by a single clinician so that scores could be consistently assigned across the spectrum of ages. Finally, neurodevelopmental outcome has been shown to be associated with socioeconomic status (SES). No SES variable was included in this analysis which may have impacted outcomes. Furthermore, the reoperation and re-intervention rate of patients with CHD could have a substantial impact on the neurodevelopmental outcome, which were not included in our analysis. Further larger studies are in preparation and will consider the reoperation and re-intervention rate.
Conclusion
In this study of neonates undergoing surgery for HLHS or d-TGA, prolonged mechanical ventilation and extended duration of DHCA were associated with worse early neurological outcome scores. Brain injury was commonly seen by MRI before and after surgery but no correlation between the total brain injury score and adverse neurological outcome was seen in the first 2 years of life. Neurological outcome seems to be more affected by the clinical course than by the CHD diagnosis itself.
Future studies that include neurodevelopmental assessments beyond 24 months of age may shed further light on the impact of brain injury in the neonatal period on more long-term neurodevelopmental outcome.
References
Hoffman, J. I. E. & Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 39, 1890–1900 (2002).
Gilboa, S. M., Salemi, J. L., Nembhard, W. N., Fixler, D. E. & Correa, A. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation 122, 2254–2263 (2010).
Wernovsky, G. Current insights regarding neurological and developmental abnormalities in children and young adults with complex congenital cardiac disease. Cardiol. Young-. 16, 92–104 (2019).
Latal, B. Neurodevelopmental outcomes of the child with congenital heart disease. Clin. Perinatol. 43, 173–185 (2016).
Limperopoulos, C., Majnemer, A., Shevell, M. I., Rosenblatt, B., Rohlicek, C. & Tchervenkov, C. Neurodevelopmental status of newborns and infants with congenital heart defects before and after open heart surgery. J. Pediatr. 137, 638–645 (2000).
Dittrich, H. Neurodevelopment at 1 year of age in infants with congenital heart disease. Heart 89, 436–441 (2003).
Jain, V. et al. Cerebral oxygen metabolism in neonates with congenital heart disease quantified by MRI and optics. J. Cereb. Blood Flow. Metab. 34, 380–388 (2014).
Andropoulos, D. B. et al. Brain immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J. Thorac. Cardiovasc. Surg. 139, 543–556 (2010).
Clouchoux, C. et al. Delayed cortical development in fetuses with complex congenital heart disease. Cereb. Cortex 23, 2932–2943 (2013).
Donofrio, M. T., DuPlessis, A. J. & Limperopoulos, C. Impact of congenital heart disease on fetal brain development and injury. Curr. Opin. Pediatr. 23, 502–511 (2011).
Donofrio, M. T. et al. Autoregulation of cerebral blood flow in fetuses with congenital heart disease: the brain sparing effect. Pediatr. Cardiol. 24, 436–443 (2003).
Kaltman, J. R., Di, H., Tian, Z. & Rychik, J. Impact of congenital heart disease on cerebrovascular blood flow dynamics in the fetus. Ultrasound Obstet. Gynecol. 25, 32–36 (2005).
Limperopoulos, C. et al. Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation 121, 26–33 (2010).
McQuillen, Patrick S., Goff, Donna A. & Licht, Daniel J. Effects of congenital heart disease on brain development. Prog. Pediatr. Cardiol. 29, 79–85 (2010).
Back, S. A. et al. Protective effects of caffeine on chronic hypoxia-induced perinatal white matter injury. Ann. Neurol. 60, 696–705 (2006).
Marino, B. S. et al. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management a scientific statement from the american heart association. Circulation 126, 1143–1172 (2012).
Miller, S. P. et al. Abnormal brain development in newborns with congenital heart disease. N. Engl. J. Med. 357, 1928–1938 (2007).
Gaynor, J. W. et al. Is cardiac diagnosis a predictor of neurodevelopmental outcome after cardiac surgery in infancy? J. Thorac. Cardiovasc. Surg. 140, 1230–1237 (2010).
Wypij, D. & Newburger, J. W. et al. The effect of duration of deep hypothermic circulatory arrest in infant heart surgery on late neurodevelopment: the Boston Circulatory Arrest Trial. J. Thorac. Cardiovasc Surg. 126, 1397–1403 (2003).
Andropoulos, D. B. et al. The association between brain injury, perioperative anesthetic exposure, and 12-month neurodevelopmental outcomes after neonatal cardiac surgery: a retrospective cohort study. Paediatr. Anaesth. 24, 266–274 (2015).
Sananes, R. et al. Neurodevelopmental outcomes after open heart operations before 3 months of age. Ann. Thorac. Surg. 93, 1577–1583 (2012).
McQuillen, P. S. et al. Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Stroke 38, 736–741 (2007).
Cooper, A. N. et al. The pediatric stroke outcome measure. Neurology 90, e365–e372 (2018).
Beers, S. R. et al. Validity of a Pediatric Version of the Glasgow Outcome Scale—extended. J. Neurotrauma 29, 1126–1139 (2012).
Tavani, F., Zimmerman, R. A., Clancy, R. R., Licht, D. J. & Mahle, W. T. Incidental intracranial hemorrhage after uncomplicated birth: MRI before and after neonatal heart surgery. Neuroradiology 45, 253–258 (2003).
Dimitropoulos, A. et al. Brain injury and development in newborns with critical congenital heart disease. Neurology 81, 241–248 (2013).
McQuillen, P. S. et al. Balloon atrial septostomy is associated with preoperative stroke in neonates with transposition of the great arteries. Circulation 113, 280–285 (2006).
Beca, J. et al. Pre-operative brain injury in newborn infants with transposition of the great arteries occurs at rates similar to other complex congenital heart disease and is not related to balloon atrial septostomy. J. Am. Coll. Cardiol. 53, 1807–1811 (2009).
Petit, C. J. et al. Preoperative brain injury in transposition of the great arteries is associated with oxygenation and time to surgery, not balloon atrial septostomy. Circulation 119, 709–716 (2009).
Bertholdt, S. et al. Cerebral lesions on magnetic resonance imaging correlate with preoperative neurological status in neonates undergoing cardiopulmonary bypass surgery. Eur. J. Cardio-Thorac. Surg. 45, 625–632 (2014).
Kelly, C. J. et al. Neuroimaging findings in newborns with congenital heart disease prior to surgery: an observational study. Arch. Dis. Child 104, 1042–1048 (2019).
Forbess, J. M., Visconti, K. J., Hancock-friesen, C., Howe, R. C., Bellinger, D. C. & Jonas, R. A. Neurodevelopmental outcome after congenital heart surgery: results from an institutional registry. Circulation 106, 95–102 (2002).
Fuller, S. et al. Deep hypothermic circulatory arrest does not impair neurodevelopmental outcome in school-age children after infant cardiac surgery. Ann. Thorac. Surg. 90, 1985–94-5 (2010).
Beca, J. et al. New white matter brain injury after infant heart surgery circulatory arrest. Circulation 127, 971–979 (2013).
Claessens, N. H. P. et al. Perioperative neonatal brain injury is associated with worse school-age neurodevelopment in children with critical congenital heart disease. Dev. Med. Child Neurol. 60, 1052–1058 (2018).
Peyvandi, S. et al. Neonatal brain injury and timing of neurodevelopmental assessment in patients with congenital heart disease. J. Am. Coll. Cardiol. 71, 1986–1996 (2018).
Mcgrath, E., Wypij, D., Rappaport, L. A., Newburger, J. W. & Bellinger, D. C. Prediction of IQ and achievement at age 8 years from neurodevelopmental status at age 1 year in children with D-transposition of the great arteries. Pediatrics 114, 572–576 (2004).
Acknowledgements
V.A.K. was supported by the Kaltenbach doctoral candidate-grant, funded by the German Heart Foundation. This sponsor has no influence on the study design, the collection, analysis, and interpretation of data, the writing of the report or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
V.A.K.: Study design, initial drafting, project administration, data collection, visualization, critical review, final revision. J.L.C.: Study design, initial drafting, project administration, data collection, data analysis, critical review, final revision, approval of the article. D.Z.: Study design, statistics, data analysis, visualization, critical review, final revision, approval of the article. J.G.R.: Data collection, visualization, critical review. L.T.: Initial drafting, data collection, critical review, approval of the article. M.T.D.: Study design, initial drafting, critical review, approval of the article. R.A.-F.: Initial drafting, critical review, approval of the article. C.L.: Study design, initial drafting, critical review, approval of the article. C.Y.: Supervision, study design, initial drafting, project administration, visualization, data analysis, critical review, final revision, approval of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplemental information
Rights and permissions
About this article
Cite this article
Kuhn, V.A., Carpenter, J.L., Zurakowski, D. et al. Determinants of neurological outcome in neonates with congenital heart disease following heart surgery. Pediatr Res 89, 1283–1290 (2021). https://doi.org/10.1038/s41390-020-1085-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1085-1
This article is cited by
-
Altered brain structure in preschool-aged children with tetralogy of Fallot
Pediatric Research (2023)
-
Altered white matter connectivity in children with congenital heart disease with single ventricle physiology
Scientific Reports (2023)
-
Predictors of Neurological Outcome Following Infant Cardiac Surgery Without Deep Hypothermic Circulatory Arrest
Pediatric Cardiology (2022)