Abstract
In spite of a large number of randomized placebo-controlled clinical trials and observational cohort studies including >50,000 preterm infants from 29 countries that have demonstrated a decrease in the risk of necrotizing enterocolitis, death, and sepsis, routine prophylactic probiotic administration to preterm infants remains uncommon in much of the world. This manuscript reflects talks given at NEC Society Symposium in 2019 and is not intended to be a state-of-the-art review or systematic review, but a summary of the probiotic-specific aspects of the symposium with limited additions including a recent strain-specific network analysis and position statement from the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN). We address ten common questions related to the intestinal microbiome and probiotic administration to the preterm infant.
Similar content being viewed by others
Introduction
Probiotic use in neonatal units varies widely across the world. While some clinicians recommend routine prophylactic supplementation to premature infants,1 others suggest awaiting more definitive evidence and/or better probiotic products.2 A large number of meta-analyses of randomized controlled trials (RCTs) and observational studies of probiotic use in preterm infants have been published. To summarize data presented and discussed at the 2019 Necrotizing Enterocolitis (NEC) Symposium, we have opted to address ten common questions.
What is intestinal dysbiosis?
Dysbiosis is an alteration in the composition or function of the microbes in a given anatomic location that is associated with disease. Common well-accepted examples include antibiotic-associated diarrhea and Clostridium difficile colitis. Novel tools that identify microbes that are difficult or impossible to grow in culture and the functional capacity of these microbes have increased understanding of how the microbes that colonize the host impact health. This is particularly important in the intestinal tract, which houses trillions of bacteria, viruses, fungi, and archaea. Indeed, the intestinal microbiome is viewed by many as an integral part of the host immune system.3,4
Intestinal dysbiosis has been associated with many chronic diseases with potential causal mechanisms demonstrated in preclinical studies.5,6 Recent reviews of the role of dysbiosis in such widely differing disease processes as type 1 diabetes,7 human immunodeficiency virus infection,8 colorectal cancer,9 liver fibrosis,10 chronic kidney disease,11 and inflammatory eye diseases12 underscore the profound local and systemic effects associated with alterations in the gut microbiome. Modern hygiene practices and antibiotic administration have altered horizontal transmission of intestinal microbes among communities while the introduction of cesarean sections and formula feeding have altered vertical transmission from mother to baby. As a result, it is highly likely that the intestinal microbiota that evolved with our ancestors has been substantially (and perhaps irreversibly) modified. In many developed countries today, even a mother who delivers vaginally receives no peripartum antibiotics and exclusively breast-feeds may still not be able to provide certain beneficial commensal bacteria to her infant.13,14
Why does intestinal dysbiosis matter in the preterm infant?
Preterm infants are at a uniquely elevated risk for intestinal dysbiosis, with potential consequences including NEC and sepsis. The gut of the preterm infant becomes colonized at a time when gastrointestinal function and innate and adaptive immune systems are immature. For instance, intestinal motility in the very preterm infant is often reduced, when compared to more mature infants, Paneth cells are not yet functional,15 intestinal mucus, immunoglobulins, and antimicrobial peptides are all less abundant,16 apoptosis is poorly regulated, and signaling molecules such as Toll-like receptors (TLRs) are highly expressed. For instance, in the fetus TLR4 is highly expressed in enterocytes and is important in stimulating maturation of the gut, whereas in the term infant TLR4 expression is low and serves predominantly as a pattern recognition sensor for intestinal bacteria and viruses. In the very preterm infant, high expression of TLR4 leads to an exuberant and poorly controlled inflammatory response and impairment of the intestinal barrier, and in animal models, suppression of TLR4 reduces NEC severity.17
Preterm infants are exposed for long time periods to hospital surface microbes, indwelling tubes,18 antibiotics,19,20 and other medications,21 all of which influence the intestinal microbiome. As a result of these developmental and environmental factors, the fecal microbiome of the preterm infant is often dominated by pro-inflammatory γ-Proteobacteria that contain TLR4 ligands, particularly between 28 and 33 weeks of corrected gestational age.22 Expansion of this bacterial phylum (which includes the family Enterobacteriaceae and genera Escherichia and Klebsiella) has been described as the “signature” of intestinal dysbiosis.23 A recent meta-analysis including almost 3000 fecal samples from nearly 400 preterm infants demonstrated that this “signature” of dysbiosis precedes the onset of NEC.24 The peak postmenstrual age for the onset of NEC25 coincides with the period of predominance of γ-Proteobacteria22 and with poorly controlled pro-inflammatory responses in the immature developing gut.26,27 Furthermore, inducers of dysbiosis such as prolonged antibiotic administration and medications that suppress gastric acid have been associated with increased risk of NEC in preterm infants.28,29
Late-onset sepsis (LOS) is frequent among preterm infants. Recent analyses of the intestinal microbiome and metabolome have demonstrated significant differences between infants with LOS and carefully matched controls suggesting that translocation of pathogens from the intestinal tract (including coagulase-negative staphylococci) is a common source of infection in the preterm infant.30,31 This is likely related to the combination of intestinal dysbiosis and increased permeability of the intestinal barrier in this population. As with NEC, early exposure to prolonged antibiotics is associated with an increased risk of LOS.28
Do probiotics alter the intestinal microbiome?
A recent cohort study demonstrated alleviation of antibiotic-associated dysbiosis in very preterm infants with probiotic administration.32 If increased γ-Proteobacteria is the signature of dysbiosis in premature infants, a probiotic that decreases the numbers of γ-Proteobacteria and reduces inflammatory responses to these bacteria while also increasing the numbers of probiotic organisms in the intestinal lumen would seem desirable. Several studies in preterm babies have demonstrated effective colonization of ingested probiotic microbes.33,34 Studies reporting changes in colonization with both the administered probiotic microbe and Enterobacteriaceae in preterm infants are summarized in Table 1.35,36,37,38,39 Note that only two probiotics demonstrated both an increase in the administered microbe and a decrease in Enterobacteriaceae. One mechanism by which probiotic microbes displace Enterobacteriaceae in the intestinal lumen is competition for sources of nutrition. Human milk oligosaccharides (HMOs) are abundant in human milk but not digestible by the human intestinal tract. Only a few bacteria are able to consume HMOs, predominantly Bifidobacterium and Bacteroides species. For example, Bifidobacterium longum subsp. infantis 15697 is able to consume the full range of HMOs, Bifidobacterium animalis subsp. lactis is unable to consume HMOs, while strains of Bifidobacterium breve are able to consume a limited number of HMOs.37,40,41,42 The capacity of probiotic B. infantis to outcompete all other gut microbes in the breast-fed term infant has recently been demonstrated.43
In addition to bacteria, probiotics may influence fungal colonization in the gut. A recent meta-analysis of RCTs found that probiotics decreased colonization with Candida species in preterm infants.44 An additional prospective randomized study not included in the meta-analysis found Lactobacillus reuteri 17938 as effective as nystatin in preventing colonization with Candida in preterm very low birth weight infants; among the 300 infants enrolled, fecal colonization rates were 19% in the L. reuteri group and 16% in the nystatin group (p = 0.54).45 It is noteworthy that this study was not blinded and that the infants who received L. reuteri in this clinical trial had a lower incidence of culture-positive sepsis and a shorter length of hospital stay than the infants who received nystatin.
The impact of probiotic administration on viral colonization of the intestinal tract has not been explored in preterm infants. In adults, administration of B. animalis subsp. lactis Bl-04 decreased nasal shedding following administration of rhinovirus.46 In children, administration of Lactobacillus rhamnosus 35 at a dose of 6 × 108 organisms/day for 3 days decreased fecal shedding of rotavirus.47
The studies of colonization described above rely on the assumptions that the fecal microbiome is equivalent to that of the distal small bowel or proximal colon and that the organisms identified by current non-culture methods are living microbes. Clearly, both of these assumptions have limitations. In spite of these limitations, the evidence supports favorable changes in the intestinal microbiome associated with administration of several probiotic strains.
Do probiotics prevent disease in preterm infants?
A large number of RCTs and observational cohort studies have been performed to examine the impact of probiotic administration on the outcomes of death, NEC, and LOS in preterm infants. These studies from 29 countries now include >50,000 preterm infants for whom NEC is reported as an outcome. The meta-analyses of these studies have used varying statistical approaches and included differing studies, but all have concluded that probiotics significantly decrease the risk of both NEC and death in infants weighing <1500 g at birth.48,49,50,51,52,53,54,55,56 Some meta-analyses also suggest a modest reduction in the risk of LOS in this population. A critical appraisal of the quality of these systematic reviews and/or the individual studies is beyond the scope of this paper; however, a recent review of 98 meta-analyses of RCTs of interventions to reduce the risk of NEC in preterm infants included 1 of the meta-analyses of probiotic administration49 and found the quality of the review to be high based on the AMSTAR criteria (see Table 2).57
One of the concerns expressed regarding the large number of probiotic clinical trials in preterm infants is that many of them are small single-center trials. Table 3 summarizes the impact of probiotics on NEC including only the RCTs with ≥400 preterm infants with 3 of these trials demonstrating benefit and 4 showing no benefit.58,59,60,61,62,63,64 Table 4 summarizes the published cohort studies of probiotics with >1000 infants with 8 showing benefit, 2 showing no benefit, and 1 showing a modest benefit with multivariate regression.65,66,67,68,69,70,71,72,73,74,75
There have also been concerns about the relatively small numbers of extremely low birth weight infants in the meta-analyses published to date. In some of the early randomized clinical trials, there appeared to be no benefit of probiotic administration in prevention of NEC in the most premature infants with a possible increase in sepsis.76 However, subgroup analyses should be viewed cautiously, particularly due to issues with interpretation.77 As more studies have been published, it has become clear that the incidences of NEC, death, and sepsis are not higher in extremely premature infants receiving probiotics. In addition, two large cohort studies have shown a lower incidence of NEC in extremely preterm infants receiving probiotics.74,78
How do probiotics work?
In addition to competition for nutrients within the gut lumen, the metabolic products of the probiotic microbe likely shape the intestinal microbiota. For instance, Lactobacillus and Bifidobacterium species produce lactate and short-chain fatty acids, such as acetate, propionate, and butyrate. These microbial products lower the pH in the colon inhibiting the growth of microbes that are less tolerant of an acidic environment.13,38,43 In addition, several probiotic microbes produce bacteriocins, which have antibacterial properties inhibiting the growth of competing bacteria. Bacteriocins produced by Lactobacillus species and other lactic-acid bacteria have been the most studied to date with emphasis on their capacity to inhibit growth of bacteria associated with food spoilage.79 How effective probiotic-associated bacteriocins are at preventing or treating infections remains uncertain.80
Some probiotic microbes also have an anti-inflammatory effect, particularly in the preterm infant. The mechanisms underlying this effect include decreased expression of TLR4 and TLR2, activation of TLR9 leading to inhibition of TLR4 activity, decreased interleukin-1β (IL-1β)-mediated expression of IL-6 and IL-8, and increased expression of molecules that inhibit the TLR4 pathway.81,82 Probiotic microbes also decrease intestinal permeability, which may be particularly relevant in the preterm infant as a leaky gut appears to be an important aspect of increased risk for both NEC and LOS.83 Mechanisms by which probiotic microbes alter intestinal permeability include the expression of surface molecules that interact with host immune receptors (e.g., flagella, pili, and capsular polysaccharides) and secreted molecules in addition to the previously noted organic acids and bacteriocins (e.g., secreted proteins, indoles, and microvesicles).84,85
Are probiotics safe for preterm infants?
Clinical trials of probiotics have been criticized for not reporting adverse events and side effects.86 In preterm infants, many trials have reported no significant difference in bloating, diarrhea, vomiting, or feeding tolerance with probiotic administration. Meta-analyses of clinical trials in preterm infants have shown shorter time to full enteral feeding and shorter length of hospitalization with probiotic administration.50,87 The risks of probiotic administration appear to be limited to sepsis caused by the probiotic organism and to infection associated with contamination of the probiotic product. Probiotic sepsis has been reported for the common probiotic microbes administered to premature infants and may be underestimated due to the challenges of isolating and identifying Bifidobacterium and Lactobacillus species.88 Large studies that have specifically sought evidence of probiotic sepsis have not found such cases.89,90 The decrease in mortality and in episodes of sepsis with administration of probiotic microbes suggests that probiotic sepsis is uncommon and that there is a net beneficial effect in reducing infection.
Studies of commercially available probiotics have demonstrated that many products do not contain the advertised strain or contain additional strains that are not noted on the label.91 The report of a death in a premature infant who received a contaminated probiotic92 underscores the importance of increased oversight of probiotic production in the USA. Probiotics produced in other countries that provide a higher level of oversight than that provided in the USA for dietary supplements represent a reasonable option for neonatologists who prefer not to continue to await a product produced in the USA.74
Recent meta-analyses have found no differences in common outcomes such as bronchopulmonary dysplasia, retinopathy of prematurity, intraventricular hemorrhage, or neurodevelopmental delay between infants receiving probiotics and those receiving a placebo.50,93,94 As noted above, early analyses suggested that the most premature infants may not benefit from probiotic administration95; however, the largest observational study to date, including 4683 infants with birth weight <1000 g, demonstrated a decrease in the incidence of NEC and death with probiotic administration in this more immature group of infants.70,74,78
Several studies have demonstrated cross-contamination with probiotics within a given neonatal intensive care unit (NICU) wherein the probiotic strain has been isolated from the feces of infants who did not receive the probiotic. This suggests that probiotic microbes are passed from infant to infant or from care provider to infant in the NICU. Whether this is a problem or not remains unclear, as the intestinal tract is continually being exposed to environmental bacteria. One case report of a probiotic fungus Saccharomyces boulardii causing infection in an infant adjacent to an infant who was receiving the probiotic suggests that cross-contamination may involve risk.96 This appears to be a very rare phenomenon.
In summary, probiotic administration has potential risks as well as benefits. As with essentially all interventions in very preterm infants, clinicians and parents must weigh the risks and benefits in deciding to provide probiotic administration. The risks of probiotic administration to very preterm infants appear to be low and perhaps comparable to, or even lower than, the risk of symptomatic cytomegalovirus infection from feeding unpasteurized mother’s milk to preterm infants.97 It is our impression that the benefits of mother’s milk and probiotics both outweigh the risks. We believe it is important to engage parents in this decision.
How do the safety and efficacy of probiotics compare to other common interventions in preterm infants?
The practice of evidence-based medicine is particularly challenging in neonatology given the relative paucity of high-quality studies in support of common interventions. Table 5 summarizes several meta-analyses in very preterm infants of common interventions that included mortality as an outcome.98,99,100,101,102,103,104,105,106,107,108 The beneficial effect of probiotic administration on mortality in preterm infants is similar to that seen with studies of antenatal corticosteroids and with the early studies of a single dose of surfactant vs no treatment; there are stronger data to support probiotic administration than many of the other listed common interventions in very preterm infants.
Other interventions, besides human milk and probiotics, to alter the intestinal microbiota or augment the innate immune system have been studied in preterm infants. For instance, a recent meta-analysis of 18 RCTs of prebiotic glycans including >1300 preterm infants showed a decrease in LOS and death but no significant impact on the incidence of NEC. All of the included trials were individually underpowered to detect clinically important differences in these three outcomes.109 Lactoferrin, a component of human milk with antibacterial properties, showed low-quality evidence of benefit in reducing sepsis and NEC in a recent meta-analysis of small clinical trials in preterm infants110; however, a subsequent much larger clinical trial including >2200 preterm infants demonstrated no benefit in reducing NEC, sepsis, or death.111
Which probiotic product is most effective for preterm infants?
Most of the RCTs and cohort studies published to date have compared a single probiotic product (containing one or more strains) to either a placebo or to no probiotic treatment. The largest probiotic RCT to date in preterm infants compared a single strain probiotic, B. breve BBG-001 in >1300 infants and found no difference between the probiotic and placebo groups for NEC, sepsis, or death.58 This strain was chosen based on previous demonstration of improved weight gain112; however, there were no mechanistic data from human or preclinical studies to suggest alterations in inflammation or intestinal permeability with this strain. The observation that more studies of combination products (containing more than one probiotic strain) have shown benefit in reduction of NEC than studies of single microbe probiotic products has been interpreted as evidence that multi-strain products are more effective; however, in the absence of comparisons between actual products or consistent findings of subgroup heterogeneity in meta-analyses, such conclusions are not justified.113
Observations which suggest that administration of a Bifidobacterium strain would be potentially beneficial include (1) antibiotic administration decreases fecal bifidobacteria20 and is associated with increased risk of NEC; (2) preterm infants with LOS have lower numbers of bifidobacteria prior to onset of sepsis30; (3) as noted above, many strains of bifidobacteria consume HMOs and are historically the dominant gut microbes in breast-fed infants13; and (4) a meta-analysis of RCTs of Bifidobacterium strains demonstrated reduced risk of NEC and death53 and a strain-specific network meta-analysis demonstrated a decrease in NEC with B. lactis Bb12 (relative risk (RR) 0.25 (0.10, 0.56).114
Observations in favor of administration of Lactobacillus strains to preterm infants include (1) a large body of animal studies demonstrating protective mechanisms in the preterm gut115; (2) a meta-analysis of clinical trials of L. reuteri 17938 demonstrating benefit116; and (3) the previously noted strain-specific network meta-analysis demonstrating benefit with L. rhamnosus GG and L. reuteri 17938.114
Combination probiotic products containing more than one microbial strain offer the potential advantage of synergism between strains and the potential disadvantage of negative interactions between administered strains. Several combination products have shown benefit in decreasing the risks of death and NEC.114
Among products available in North America, there are good data available suggesting safety and efficacy in preterm infants for several commercial products, including L. reuteri 17938 (Biogaia, Gerber)117 and Ultimate Flora Baby (Renew Life, a combination of four Bifidobacterium and one Lactobacillus strains).118 The combination of B. infantis Bb-02, Streptococcus thermophilus TH-4, and B. lactis Bb12 (ABC Dophilus) demonstrated a significant decrease in NEC in a large multicenter trial.61 Following the clinical trial, this product was altered to contain B. lactis, S. thermophilus, and L. rhamnosus and then taken off the market following the death of a premature infant from contamination as noted above. The original combination product is now available in the U.S. (Similac Probiotic Tri-blend) and Europe (Neobiomics ProPrems). Safety and sustained colonization have been shown in term breast-fed infants for the B. infantis EVC001 strain.43,119 Long-term follow-up of term infants receiving L. rhamnosus GG has demonstrated safety and some efficacy at decreasing allergic disease.120,121 L. rhamnosus GG (Culturelle) is the most commonly administered probiotic strain in U.S. NICUs. The previously noted strain-specific network analysis demonstrated decreased risk of NEC (RR 0.24 (0.064, 0.67)) with administration of L. rhamnosus GG,114 though a recent US cohort study of preterm infants did not demonstrate benefit.90
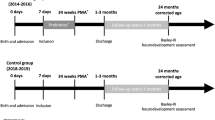
Dose comparison studies are few and do not address the possibility that different strains have different optimum dosage.37,122 Similarly, duration of probiotic administration varies with most studies commencing probiotic administration with the first enteral feeding and continuing until 34–36 weeks corrected gestation.
A recent position paper from the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) Committee on Nutrition and the ESPGHAN Working Group for Probiotics and Prebiotics summarized current evidence with reliance on the strain-specific network meta-analysis.114 Emphasis was placed on quality assurance of the probiotic product, absence of transferable antibiotic-resistance genes, and local ability to routinely detect probiotic sepsis with a conditional recommendation (with low certainty of evidence) to provide either L. rhamnosus GG (e.g., Culturelle) or the combination of B. infantis Bb-02, B. lactis Bb-12, and S. thermophilus TH-4 (e.g., Similac Tri-blend, NeoBiomics ProPrems) in order to reduce NEC rates.123
What would the definitive clinical trial of probiotics in preterm infants look like?
Given the large magnitude of treatment benefit toward reduction of NEC and death demonstrated in both RCTs and observational studies of probiotic administration in preterm infants, it is unlikely that further placebo-controlled RCTs will alter the conclusion that probiotics prevent NEC and death or meaningfully change the estimates of treatment benefit. For instance, using the larger clinical trials summarized in Table 3 (incidence of NEC 97/2520 or 3.8% for infants receiving probiotic and 151/2554 or 5.9% for infants receiving placebo) to guide a reasonable effect size estimate and assuming α = 0.05 and β = 0.9, a sample size of 2292 babies in each group would be needed for a definitive trial to detect a similar or larger magnitude difference. Even if the incidence of NEC were equivalent in each group (and midway between the incidences in Table 3) in such a large study, the unadjusted RR for NEC of the studies in Table 3 plus the new theoretical large study would still suggest benefit (RR 0.79, 95% confidence interval 0.66, 0.95). For this reason, future studies should ideally compare promising probiotic products to each other rather than to placebo. Furthermore, as noted earlier, cross-contamination occurs frequently in the NICU,37,89 suggesting that beneficial effects of probiotics may be underestimated with traditional placebo-controlled parallel-group randomized trial designs. For this reason, a cluster-randomized cross-over trial (in which the NICU is randomized to a given probiotic product for a time period and then crosses over to the other product) may be of particular value. Such a study would require a large sample size, possibly in the tens of thousands, and significant funding. In the absence of such a definitive study, pooling the observational data on routine probiotic use from dozens or hundreds of NICUs, as has been recently reported from Germany70 and Canada,74 has high value.
How can we best communicate with NICU parents about probiotics and human milk?
The role of parents in the NICU has changed dramatically over the past decades. Today, many units are moving away from their traditional clinician-driven hierarchical structure toward family-centered care, where parents are considered core members of their baby’s care team. In this model, clinicians and staff value parents’ concerns and actively seek their engagement. Family-centered care has the potential to improve outcomes, including reduced length of stay124,125 and complications.124 While the benefits of inclusion of parents as an essential part of the team caring for their preterm neonate are becoming apparent,126,127 parental participation in NICU care and decision-making remains highly variable.128 In focus groups and in surveys, parents of very premature infants expressed frustration at the limited information they received in the NICU.129 Parents overwhelmingly report to the NEC Society that they wish they had more information about NEC and potential NEC prevention strategies, and sooner.68
The current variability in practice regarding probiotics is an additional reason to include parents in this discussion. Parents should understand why the decision has been made to give their baby probiotics or not. The fear of overwhelming families with information should not preclude such a discussion. A conversation with the parents of the risks of sepsis and NEC and the potential risks and benefits of mother’s own milk and probiotics in the first days after the delivery of a very preterm infant is viewed by families as empowering rather than frightening. Ensuring that the family understands and actively supports care decisions sets the stage for a more positive and less stressful parent experience, regardless of the outcome.
It may well be that family-centered care in the NICU will have greater long-term benefit for both parents and extremely preterm infants than many common interventions.95 An example of a concise summary for parents of NEC and the risks and benefits of human milk and probiotics is presented on the NEC website: https://necsociety.org/wp-content/uploads/2019/02/Probiotics_HumanMilk_Resource_Parents.pdf.
References
Athalye-Jape, G. & Patole, S. Probiotics for preterm infants - time to end all controversies. Microb. Biotechnol. 12, 249–253 (2019).
Pell, L. G., Loutet, M. G., Roth, D. E. & Sherman, P. M. Arguments against routine administration of probiotics for NEC prevention. Curr. Opin. Pediatr. 31, 195–201 (2019).
Weiss, G. A. & Hennet, T. Mechanisms and consequences of intestinal dysbiosis. Cell. Mol. Life Sci. 74, 2959–2977 (2017).
Takiishi, T., Fenero, C. I. M. & Camara, N. O. S. Intestinal barrier and gut microbiota: shaping our immune responses throughout life. Tissue Barriers 5, e1373208 (2017).
Vatanen, T. et al. Variation in microbiome LPS immunogenicity contributes to autoimmunity in humans. Cell 165, 842–853 (2016).
Chua, H. H. et al. Intestinal dysbiosis featuring abundance of Ruminococcus gnavus associates with allergic diseases in infants. Gastroenterology 154, 154–167 (2018).
Abdellatif, A. M. & Sarvetnick, N. E. Current understanding of the role of gut dysbiosis in type 1 diabetes. J. Diabetes 11, 632–644 (2019).
Lujan, J. A., Rugeles, M. T. & Taborda, N. A. Contribution of the microbiota to intestinal homeostasis and its role in the pathogenesis of HIV-1 infection. Curr. HIV Res. 17, 13–25 (2019).
Jackson, D. N. & Theiss, A. L. Gut bacteria signaling to mitochondria in intestinal inflammation and cancer. Gut Microbes 11, 285–304 (2019).
Zhou, R., Fan, X. & Schnabl, B. Role of the intestinal microbiome in liver fibrosis development and new treatment strategies. Transl. Res. 209, 22–38 (2019).
Jazani, N. H., Savoj, J., Lustgarten, M., Lau, W. L. & Vaziri, N. D. Impact of gut dysbiosis on neurohormonal pathways in chronic kidney disease. Diseases 7, E21 (2019).
Lin, P. Importance of the intestinal microbiota in ocular inflammatory diseases: a review. Clin. Exp. Ophthalmol. 47, 418–422 (2019).
Henrick, B. M. et al. Elevated fecal pH indicates a profound change in the breastfed infant gut microbiome due to reduction of bifidobacterium over the past century. mSphere 3, e00041-18 (2018).
Rook, G. A., Lowry, C. A. & Raison, C. L. Microbial ‘old friends’, immunoregulation and stress resilience. Evol. Med. Public Health 2013, 46–64 (2013).
Heida, F. H. et al. Paneth cells in the developing gut: when do they arise and when are they immune competent? Pediatr. Res. 80, 306–310 (2016).
Brandtzaeg, P. Gate-keeper function of the intestinal epithelium. Benef. Microbes 4, 67–82 (2013).
Mihi, B. & Good, M. Impact of Toll-like receptor 4 signaling in necrotizing enterocolitis: the state of the science. Clin. Perinatol. 46, 145–157 (2019).
Taft, D. H. et al. Bacterial colonization and antimicrobial resistance genes in neonatal enteral feeding tubes. FEMS Microbiol. Ecol. 95, fiz039 (2019).
Gasparrini, A. J. et al. Antibiotic perturbation of the preterm infant gut microbiome and resistome. Gut Microbes 7, 443–449 (2016).
Zwittink, R. D. et al. Association between duration of intravenous antibiotic administration and early-life microbiota development in late-preterm infants. Eur. J. Clin. Microbiol. Infect. Dis. 37, 475–483 (2018).
Gupta, R. W. et al. Histamine-2 receptor blockers alter the fecal microbiota in premature infants. J. Pediatr. Gastroenterol. Nutr. 56, 397–400 (2013).
La Rosa, P. S. et al. Patterned progression of bacterial populations in the premature infant gut. Proc. Natl Acad. Sci. USA 111, 12522–12527 (2014).
Litvak, Y., Byndloss, M. X., Tsolis, R. M. & Baumler, A. J. Dysbiotic Proteobacteria expansion: a microbial signature of epithelial dysfunction. Curr. Opin. Microbiol. 39, 1–6 (2017).
Pammi, M. et al. Intestinal dysbiosis in preterm infants preceding necrotizing enterocolitis: a systematic review and meta-analysis. Microbiome 5, 31 (2017).
Yee, W. H. et al. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics 129, e298–e304 (2012).
Hackam, D. J. & Sodhi, C. P. Toll-like receptor-mediated intestinal inflammatory imbalance in the pathogenesis of necrotizing enterocolitis. Cell. Mol. Gastroenterol. Hepatol. 6, 229.e1–238.e1 (2018).
Lueschow, S. R. et al. Loss of murine Paneth cell function alters the immature intestinal microbiome and mimics changes seen in neonatal necrotizing enterocolitis. PLoS ONE 13, e0204967 (2018).
Cantey, J. B., Pyle, A. K., Wozniak, P. S., Hynan, L. S. & Sanchez, P. J. Early antibiotic exposure and adverse outcomes in preterm, very low birth weight infants. J. Pediatr. 203, 62–67 (2018).
More, K., Athalye-Jape, G., Rao, S. & Patole, S. Association of inhibitors of gastric acid secretion and higher incidence of necrotizing enterocolitis in preterm very low-birth-weight infants. Am. J. Perinatol. 30, 849–856 (2013).
Stewart, C. J. et al. Longitudinal development of the gut microbiome and metabolome in preterm neonates with late onset sepsis and healthy controls. Microbiome 5, 75 (2017).
Taft, D. H. et al. Center variation in intestinal microbiota prior to late-onset sepsis in preterm infants. PLoS ONE 10, e0130604 (2015).
Esaiassen, E. et al. Effects of probiotic supplementation on the gut microbiota and antibiotic resistome development in preterm infants. Front. Pediatr. 6, 347 (2018).
Dutta, S., Ray, P. & Narang, A. Comparison of stool colonization in premature infants by three dose regimes of a probiotic combination: a randomized controlled trial. Am. J. Perinatol. 32, 733–740 (2015).
Tobin, J. M., Garland, S. M., Jacobs, S. E., Pirotta, M. & Tabrizi, S. N. Rapid assay to assess colonization patterns following in-vivo probiotic ingestion. BMC Res. Notes 6, 252 (2013).
Chrzanowska-Liszewska, D., Seliga-Siwecka, J. & Kornacka, M. K. The effect of Lactobacillus rhamnosus GG supplemented enteral feeding on the microbiotic flora of preterm infants-double blinded randomized control trial. Early Hum. Dev. 88, 57–60 (2012).
Underwood, M. A. et al. Digestion of human milk oligosaccharides by Bifidobacterium breve in the premature infant. J. Pediatr. Gastroenterol. Nutr. 65, 449–455 (2017).
Underwood, M. A. et al. A comparison of two probiotic strains of bifidobacteria in premature infants. J. Pediatr. 163, 1585.e9–1591.e9 (2013).
Mohan, R. et al. Effects of Bifidobacterium lactis Bb12 supplementation on body weight, fecal pH, acetate, lactate, calprotectin, and IgA in preterm infants. Pediatr. Res. 64, 418–422 (2008).
Underwood, M. A. et al. A randomized placebo-controlled comparison of 2 prebiotic/probiotic combinations in preterm infants: impact on weight gain, intestinal microbiota, and fecal short-chain fatty acids. J. Pediatr. Gastroenterol. Nutr. 48, 216–225 (2009).
Smilowitz, J. T., Lebrilla, C. B., Mills, D. A., German, J. B. & Freeman, S. L. Breast milk oligosaccharides: structure-function relationships in the neonate. Annu. Rev. Nutr. 34, 143–169 (2014).
Underwood, M. A., German, J. B., Lebrilla, C. B. & Mills, D. A. Bifidobacterium longum subspecies infantis: champion colonizer of the infant gut. Pediatr. Res. 77, 229–235 (2015).
Garrido, D. et al. Utilization of galactooligosaccharides by Bifidobacterium longum subsp. infantis isolates. Food Microbiol. 33, 262–270 (2013).
Frese, S. A. et al. Persistence of supplemented Bifidobacterium longum subsp. infantis EVC001 in breastfed infants. mSphere 2, e00501–e00517 (2017).
Hu, H. J., Zhang, G. Q., Zhang, Q., Shakya, S. & Li, Z. Y. Probiotics prevent candida colonization and invasive fungal sepsis in preterm neonates: a systematic review and meta-analysis of randomized controlled trials. Pediatr. Neonatol. 58, 103–110 (2017).
Oncel, M. Y. et al. Comparison of Lactobacillus reuteri and nystatin prophylaxis on Candida colonization and infection in very low birth weight infants. J. Matern. Fetal Neonatal Med. 28, 1790–1794 (2015).
Turner, R. B. et al. Effect of probiotic on innate inflammatory response and viral shedding in experimental rhinovirus infection - a randomised controlled trial. Benef. Microbes 8, 207–215 (2017).
Fang, S. B. et al. Dose-dependent effect of Lactobacillus rhamnosus on quantitative reduction of faecal rotavirus shedding in children. J. Trop. Pediatr. 55, 297–301 (2009).
Alfaleh, K. & Anabrees, J. Probiotics for prevention of necrotizing enterocolitis in preterm infants. Cochrane Database Syst. Rev. 4, CD005496 (2014).
Sawh, S. C., Deshpande, S., Jansen, S., Reynaert, C. J. & Jones, P. M. Prevention of necrotizing enterocolitis with probiotics: a systematic review and meta-analysis. PeerJ 4, e2429 (2016).
Sun, J. et al. Effects of probiotics on necrotizing enterocolitis, sepsis, intraventricular hemorrhage, mortality, length of hospital stay, and weight gain in very preterm infants: a meta-analysis. Adv. Nutr. 8, 749–763 (2017).
Dermyshi, E. et al. The “golden age” of probiotics: a systematic review and meta-analysis of randomized and observational studies in preterm infants. Neonatology 112, 9–23 (2017).
Deshpande, G., Jape, G., Rao, S. & Patole, S. Benefits of probiotics in preterm neonates in low-income and medium-income countries: a systematic review of randomised controlled trials. BMJ Open 7, e017638 (2017).
Zhu, X. L. et al. Bifidobacterium may benefit the prevention of necrotizing enterocolitis in preterm infants: a systematic review and meta-analysis. Int. J. Surg. 61, 17–25 (2019).
Jiang, T., Zhang, H., Xu, X., Li, H. & Yang, J. Mixed probiotics decrease the incidence of stage II-III necrotizing enterocolitis and death: a systematic review and meta-analysis. Microb. Pathog. 138, 103794 (2020).
Balasubramanian, H., Ananthan, A., Rao, S. & Patole, S. Probiotics for preterm infants in India - systematic review and meta-analysis of randomized controlled trials. Indian J. Pediatr. https://doi.org/10.1007/s12098-020-03223-0 (2020).
Olsen, R., Greisen, G., Schroder, M. & Brok, J. Prophylactic probiotics for preterm infants: a systematic review and meta-analysis of observational studies. Neonatology 109, 105–112 (2016).
Xiong, T., Maheshwari, A., Neu, J., Ei-Saie, A. & Pammi, M. An overview of systematic reviews of randomized-controlled trials for preventing necrotizing enterocolitis in preterm infants. Neonatology 117, 46–56 (2020).
Costeloe, K. et al. Bifidobacterium breve BBG-001 in very preterm infants: a randomised controlled phase 3 trial. Lancet 387, 649–660 (2016).
Oncel, M. Y. et al. Lactobacillus reuteri for the prevention of necrotising enterocolitis in very low birthweight infants: a randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 99, F110–F115 (2014).
Manzoni, P. et al. Oral supplementation with Lactobacillus casei subspecies rhamnosus prevents enteric colonization by Candida species in preterm neonates: a randomized study. Clin. Infect. Dis. 42, 1735–1742 (2006).
Jacobs, S. E. et al. Probiotic effects on late-onset sepsis in very preterm infants: a randomized controlled trial. Pediatrics 132, 1055–1062 (2013).
Rojas, M. A. et al. Prophylactic probiotics to prevent death and nosocomial infection in preterm infants. Pediatrics 130, e1113–e1120 (2012).
Lin, H. C. et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight preterm infants: a multicenter, randomized, controlled trial. Pediatrics 122, 693–700 (2008).
Dani, C., Biadaioli, R., Bertini, G., Martelli, E. & Rubaltelli, F. F. Probiotics feeding in prevention of urinary tract infection, bacterial sepsis and necrotizing enterocolitis in preterm infants. A prospective double-blind study. Biol. Neonate 82, 103–108 (2002).
Guthmann, F., Arlettaz Mieth, R. P., Bucher, H. U. & Buhrer, C. Short courses of dual-strain probiotics appear to be effective in reducing necrotising enterocolitis. Acta Paediatr. 105, 255–259 (2016).
Hartel, C. et al. Prophylactic use of Lactobacillus acidophilus/Bifidobacterium infantis probiotics and outcome in very low birth weight infants. J. Pediatr. 165, 285–289. e281 (2014).
Bonsante, F., Iacobelli, S. & Gouyon, J. B. Routine probiotic use in very preterm infants: retrospective comparison of two cohorts. Am. J. Perinatol. 30, 41–46 (2013).
Hoyos, A. B. Reduced incidence of necrotizing enterocolitis associated with enteral administration of Lactobacillus acidophilus and Bifidobacterium infantis to neonates in an intensive care unit. Int. J. Infect. Dis. 3, 197–202 (1999).
Luoto, R., Matomaki, J., Isolauri, E. & Lehtonen, L. Incidence of necrotizing enterocolitis in very-low-birth-weight infants related to the use of Lactobacillus GG. Acta Paediatr. 99, 1135–1138 (2010).
Denkel, L. A. et al. Protective effect of dual-strain probiotics in preterm infants: a multi-center time series analysis. PLoS ONE 11, e0158136 (2016).
Patole, S. K. et al. Benefits of Bifidobacterium breve M-16V supplementation in preterm neonates - a retrospective cohort study. PLoS ONE 11, e0150775 (2016).
Samuels, N. et al. Necrotising enterocolitis and mortality in preterm infants after introduction of probiotics: a quasi-experimental study. Sci. Rep. 6, 31643 (2016).
Sharpe, J., Way, M., Koorts, P. J. & Davies, M. W. The availability of probiotics and donor human milk is associated with improved survival in very preterm infants. World J. Pediatr. 14, 492–497 (2018).
Singh, B. et al. Probiotics for preterm infants: a national retrospective cohort study. J. Perinatol. 39, 533–539 (2019).
Meyer, M. P. et al. Probiotics for prevention of severe necrotizing enterocolitis: experience of New Zealand neonatal intensive care units. Front. Pediatr. 8, 119 (2020).
Lin, H. C., Wu, S. F. & Underwood, M. Necrotizing enterocolitis. N. Engl. J. Med. 364, 1878–1879 (2011). Author reply 1879.
Wallach, J. D. et al. Evaluation of evidence of statistical support and corroboration of subgroup claims in randomized clinical trials. JAMA Intern. Med. 177, 554–560 (2017).
Denkel, L. A. et al. Dual-strain probiotics reduce NEC, mortality and neonatal bloodstream infections among extremely low birthweight infants. Arch. Dis. Child. Fetal Neonatal Ed. 102, F559–F560 (2017).
Favaro, L. & Todorov, S. D. Bacteriocinogenic LAB strains for fermented meat preservation: perspectives, challenges, and limitations. Probiotics Antimicrob. Proteins 9, 444–458 (2017).
Mokoena, M. P. Lactic acid bacteria and their bacteriocins: classification, biosynthesis and applications against uropathogens: a mini-review. Molecules 22, E1255 (2017).
Arciero, J. et al. Modeling the interactions of bacteria and Toll-like receptor-mediated inflammation in necrotizing enterocolitis. J. Theor. Biol. 321, 83–99 (2013).
Ganguli, K. et al. Probiotics prevent necrotizing enterocolitis by modulating enterocyte genes that regulate innate immune-mediated inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 304, G132–G141 (2013).
Halloran, K. & Underwood, M. A. Probiotic mechanisms of action. Early Hum. Dev. 135, 58–65 (2019).
Meng, D. et al. Indole-3-lactic acid, a metabolite of tryptophan, secreted by Bifidobacterium longum subspecies infantis is anti-inflammatory in the immature intestine. Pediatr. Res. https://doi.org/10.1038/s41390-019-0740-x (2020).
Liu, Q. et al. Surface components and metabolites of probiotics for regulation of intestinal epithelial barrier. Microb. Cell Fact. 19, 23 (2020).
Bafeta, A., Koh, M., Riveros, C. & Ravaud, P. Harms reporting in randomized controlled trials of interventions aimed at modifying microbiota: a systematic review. Ann. Intern. Med. 169, 240–247 (2018).
Athalye-Jape, G., Deshpande, G., Rao, S. & Patole, S. Benefits of probiotics on enteral nutrition in preterm neonates: a systematic review. Am. J. Clin. Nutr. 100, 1508–1519 (2014).
Esaiassen, E. et al. Bifidobacterium longum subspecies infantis bacteremia in 3 extremely preterm infants receiving probiotics. Emerg. Infect. Dis. 22, 1664–1666 (2016).
Costeloe, K. et al. A randomised controlled trial of the probiotic Bifidobacterium breve BBG-001 in preterm babies to prevent sepsis, necrotising enterocolitis and death: the Probiotics in Preterm infantS (PiPS) trial. Health Technol. Assess. 20, 1–194 (2016).
Kane, A. F., Bhatia, A. D., Denning, P. W., Shane, A. L. & Patel, R. M. Routine supplementation of Lactobacillus rhamnosus GG and risk of necrotizing enterocolitis in very low birth weight infants. J. Pediatr. 195, 73.e2–79.e2 (2018).
Jackson, S. A. et al. Improving end-user trust in the quality of commercial probiotic products. Front. Microbiol. 10, 739 (2019).
Vallabhaneni, S. et al. Notes from the field: fatal gastrointestinal mucormycosis in a premature infant associated with a contaminated dietary supplement—Connecticut, 2014. Morbidity Mortal. Wkly. Rep. 64, 155–156 (2015).
Villamor-Martinez, E. et al. Probiotic supplementation in preterm infants does not affect the risk of bronchopulmonary dysplasia: a meta-analysis of randomized controlled trials. Nutrients 9, E1197 (2017).
Cavallaro, G., Villamor-Martinez, E., Filippi, L., Mosca, F. & Villamor, E. Probiotic supplementation in preterm infants does not affect the risk of retinopathy of prematurity: a meta-analysis of randomized controlled trials. Sci. Rep. 7, 13014 (2017).
Berrington, J. & Ward Platt, M. Recent advances in the management of infants born <1000 g. Arch. Dis. Child. 101, 1053–1056 (2016).
Perapoch, J. et al. Fungemia with Saccharomyces cerevisiae in two newborns, only one of whom had been treated with ultra-levura. Eur. J. Clin. Microbiol. Infect. Dis. 19, 468–470 (2000).
Hamprecht, K. & Goelz, R. Postnatal cytomegalovirus infection through human milk in preterm infants: transmission, clinical presentation, and prevention. Clin. Perinatol. 44, 121–130 (2017).
Roberts, D., Brown, J., Medley, N. & Dalziel, S. R. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst. Rev. 3, CD004454 (2017).
Conde-Agudelo, A. & Diaz-Rossello, J. L. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst. Rev. CD002771 (2016).
Jensen, E. A., Foglia, E. E. & Schmidt, B. Association between prophylactic indomethacin and death or bronchopulmonary dysplasia: a systematic review and meta-analysis of observational studies. Semin. Perinatol. 42, 228–234 (2018).
Hennes, H. M., Lee, M. B., Rimm, A. A. & Shapiro, D. L. Surfactant replacement therapy in respiratory distress syndrome. Meta-analysis of clinical trials of single-dose surfactant extracts. Am. J. Dis. Child. 145, 102–104 (1991).
Singh, N. et al. Comparison of animal-derived surfactants for the prevention and treatment of respiratory distress syndrome in preterm infants. Cochrane Database Syst. Rev. CD010249 (2015).
Askie, L. M. et al. Effects of targeting lower versus higher arterial oxygen saturations on death or disability in preterm infants. Cochrane Database Syst. Rev. 4, CD011190 (2017).
Quigley, M., Embleton, N. D. & McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 6, CD002971 (2018).
Mitra, S. et al. Association of placebo, indomethacin, ibuprofen, and acetaminophen with closure of hemodynamically significant patent ductus arteriosus in preterm infants: a systematic review and meta-analysis. JAMA 319, 1221–1238 (2018).
Osborn, D. A., Schindler, T., Jones, L. J., Sinn, J. K. & Bolisetty, S. Higher versus lower amino acid intake in parenteral nutrition for newborn infants. Cochrane Database Syst. Rev. 3, CD005949 (2018).
McCall, E. M., Alderdice, F., Halliday, H. L., Vohra, S. & Johnston, L. Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants. Cochrane Database Syst. Rev. 2, CD004210 (2018).
Barrington, K. J., Finer, N. & Pennaforte, T. Inhaled nitric oxide for respiratory failure in preterm infants. Cochrane Database Syst. Rev. 1, CD000509 (2017).
Chi, C., Buys, N., Li, C., Sun, J. & Yin, C. Effects of prebiotics on sepsis, necrotizing enterocolitis, mortality, feeding intolerance, time to full enteral feeding, length of hospital stay, and stool frequency in preterm infants: a meta-analysis. Eur. J. Clin. Nutr. 73, 657–670 (2019).
Pammi, M. & Suresh, G. Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst. Rev. 6, CD007137 (2017).
Griffiths, J. J. P. et al. Enteral lactoferrin supplementation for very preterm infants: a randomised placebo-controlled trial. Lancet 393, 423–433 (2019).
Kitajima, H. et al. Early administration of Bifidobacterium breve to preterm infants: randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 76, F101–F107 (1997).
Chang, H. Y. et al. Multiple strains probiotics appear to be the most effective probiotics in the prevention of necrotizing enterocolitis and mortality: an updated meta-analysis. PLoS ONE 12, e0171579 (2017).
van den Akker, C. H. P. et al. Probiotics for preterm Infants: a strain specific systematic review and network meta-analysis. J. Pediatr. Gastroenterol. Nutr. 67, 103–122 (2018).
Underwood, M. A. Probiotics and the prevention of necrotizing enterocolitis. J. Pediatr. Surg. 54, 405–412 (2019).
Athalye-Jape, G., Rao, S. & Patole, S. Lactobacillus reuteri DSM 17938 as a probiotic for preterm neonates: a strain-specific systematic review. JPEN J. Parenter. Enter. Nutr. 40, 783–794 (2016).
Rolnitsky, A. et al. A quality improvement intervention to reduce necrotizing enterocolitis in premature infants with probiotic supplementation. Pediatr. Qual. Saf. 4, e201 (2019).
Sekhon, M. K., Grubb, P. H., Newman, M. & Yoder, B. A. Implementation of a probiotic protocol to reduce rates of necrotizing enterocolitis. J. Perinatol. 39, 1315–1322 (2019).
Smilowitz, J. T. et al. Safety and tolerability of Bifidobacterium longum subspecies infantis EVC001 supplementation in healthy term breastfed infants: a phase I clinical trial. BMC Pediatr. 17, 133 (2017).
Scalabrin, D., Harris, C., Johnston, W. H. & Berseth, C. L. Long-term safety assessment in children who received hydrolyzed protein formulas with Lactobacillus rhamnosus GG: a 5-year follow-up. Eur. J. Pediatr. 176, 217–224 (2017).
Lundelin, K., Poussa, T., Salminen, S. & Isolauri, E. Long-term safety and efficacy of perinatal probiotic intervention: evidence from a follow-up study of four randomized, double-blind, placebo-controlled trials. Pediatr. Allergy Immunol. 28, 170–175 (2017).
Watkins, C. et al. Dose-interval study of a dual probiotic in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 104, F159–F164 (2019).
van den Akker, C. H. P. et al. Probiotics and preterm infants: a position paper by the ESPGHAN Committee on Nutrition and the ESPGHAN Working Group for Probiotics and Prebiotics. J. Pediatr. Gastroenterol. Nutr. 70, 664–680 (2020).
Ortenstrand, A. et al. The Stockholm Neonatal Family Centered Care Study: effects on length of stay and infant morbidity. Pediatrics 125, e278–e285 (2010).
White-Traut, R. C. et al. Influence of H-HOPE intervention for premature infants on growth, feeding progression and length of stay during initial hospitalization. J. Perinatol. 35, 636–641 (2015).
Raiskila, S., Axelin, A., Rapeli, S., Vasko, I. & Lehtonen, L. Trends in care practices reflecting parental involvement in neonatal care. Early Hum. Dev. 90, 863–867 (2014).
Gianni, M. L. et al. Does parental involvement affect the development of feeding skills in preterm infants? A prospective study. Early Hum. Dev. 103, 123–128 (2016).
Franck, L. S., McNulty, A. & Alderdice, F. The perinatal-neonatal care journey for parents of preterm infants: what is working and what can be improved. J. Perinat. Neonatal Nurs. 31, 244–255 (2017).
Umberger, E., Canvasser, J. & Hall, S. L. Enhancing NICU parent engagement and empowerment. Semin. Pediatr. Surg. 27, 19–24 (2018).
Acknowledgements
M.A.U. and R.M.P. received funding from the NIH: M.A.U. R01 HD059127 and R21 HD096247 and R.M.P. KL2 TR000455, UL1 TR000454, and K23 HL128942. The NIH had no role in: (1) study design; (2) the collection, analysis, and interpretation of data; (3) the writing of the report; and (4) the decision to submit the paper for publication. Publication of this article was sponsored by the Necrotizing Enterocolitis (NEC) Society, Patient-Centered Outcomes Research Institute, and National Institutes of Health Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Author information
Authors and Affiliations
Contributions
M.A.U. wrote the initial and final drafts; E.U. and R.M.P. edited the initial draft and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
M.A.U. has received grant support from Evolve Bioscience, honoraria and travel support from Abbott, and received consulting fees from Avexegen. R.M.P. has received honoraria and travel support from Mednax, Inc., partial travel support from Danone to attend the SIGNEC UK meeting, and consults for Shipman & Goodwin, LLP. M.A.U. and R.M.P. serve on the data-monitoring committee for a probiotic study conducted by Premier Research/Infant Bacterial Therapeutics. E.U. serves as a director of the NEC Society, the sponsor of the NEC Symposium and of this supplement to Pediatric Research. None of these entities had any role in this manuscript. The authors are not endorsing the use of any specific probiotic product.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Underwood, M.A., Umberger, E. & Patel, R.M. Safety and efficacy of probiotic administration to preterm infants: ten common questions. Pediatr Res 88 (Suppl 1), 48–55 (2020). https://doi.org/10.1038/s41390-020-1080-6
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1080-6
This article is cited by
-
Bifidobacterium infantis as a probiotic in preterm infants: a systematic review and meta-analysis
Pediatric Research (2023)
-
Capturing the antibiotic resistome of preterm infants reveals new benefits of probiotic supplementation
Microbiome (2022)
-
Probiotic sepsis in preterm neonates—a systematic review
European Journal of Pediatrics (2022)