Abstract
Background
The definition of pediatric AKI continues to evolve. We aimed to find a better AKI definition to predict outcomes and identify risk factors for AKI in a Chinese PICU.
Methods
This study consisted of 3338 patients hospitalized in a Chinese PICU between 2016 and 2018. AKI was defined and staged using pROCK criteria, which were compared with KDIGO criteria. AKI outcomes, including mortality, daily cost and length of stay (LOS), were assessed. Risk factors for AKI were also estimated.
Results
The incidence of AKI in the PICU was 7.7% according to pROCK criteria. The characteristics of patients with KDIGO-defined AKI who did not meet the pROCK were similar to those without AKI. pROCK outperformed KDIGO in predicting mortality with a higher c index in the Cox models (0.81 versus 0.79, P = 0.013). AKI, as well as AKI stages, were associated with higher mortality (HR: 10.5, 95%CI: 6.66–19.5), daily cost (β = 2064, P < 0.01) and LOS (β = 2.30, P < 0.01). Age, comorbidities, mechanical ventilation (MV), pediatric critical illness score (PCIS) and exposure to drugs had significant influence on AKI occurrence.
Conclusions
The mortality predictability of pROCK was slightly greater than that of KDIGO. Older age, underlying comorbidities, MV, decreased PCIS and exposure to drugs were potential risk factors for AKI.
Impact
-
Two AKI criteria, pROCK and KDIGO, were significantly associated with an increased risk of mortality and pROCK was slightly greater than that of KDIGO.
-
Older age, comorbidities, mechanical ventilation, decreased PCIS and exposure to drugs were potential risk factors for AKI.
-
This study first used the pROCK criteria to provide an epidemiologic description of pediatric AKI in Chinese PICU.
-
This study compared the AKI outcomes across the pROCK and KDIGO AKI criteria, indicating the prior utility for AKI classification in Chinese children.
-
This study indicated that the potential risk factors for AKI were older age, comorbidities, mechanical ventilation, decreased PCIS and exposure to drugs.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is strongly associated with higher morbidity, mortality, and disease burden. It also leads to an abrupt decline in renal function that can cause chronic kidney disease (CKD), which may severely impact the quality of life.1,2,3,4 Epidemiological studies on AKI in hospitalized children have been performed in developed countries and Asian populations5,6,7,8,9,10; however, high-quality studies describing the predictive factors and epidemiological features among critically ill children in China are particularly scarce. In fact, previous studies on pediatric AKI were mostly focused on patients with specific comorbidities, such as cardiac surgery and nephrotic syndrome.11,12,13
The definition of pediatric AKI remains an evolving field,9,14 including the Kidney Disease Improving Global Outcomes (KDIGO), Acute Kidney Injury Network (AKIN), and Pediatric Risk, Injury, Failure, Loss, End Stage Renal Disease (pRIFLE) criteria.15,16,17 These criteria were originally designed for adult populations and then adapted for children18; however, the high variability of serum creatinine (SCr) in children was not taken into account. Incorporating the within-individual variability in SCr into the definition of AKI is more important in children, since both the level and the variability of SCr depend on age.
The pediatric reference change value optimized for AKI in children (pROCK criteria)19 was derived from a multicenter epidemiologic study from hospitalized children in China. The data were from 100,081 hospitalized children who met the following criteria: at least two creatinine tests within 30 days, between 1-month-old and 18 years old, no kidney disease, and no known risk of AKI. The new definition of pediatric AKI (pROCK) is based on the simple concept that only acute increase in SCr above the upper limit of normal variability (termed as “reference change value”, RCV) represents a true decline in renal function. The RCV of SCr, defined as the 95th percentile of the distribution of absolute SCr change given age and baseline SCr, approximated to the greater of an increase of 20 μmol/L and 30% of baseline SCr in children. Children with an SCr increase of both ≥20 μmol/L and ≥30% over the baseline within 7 days will be defined as pediatric AKI by pROCK.
The authors claim that pROCK criteria outperform other criteria in predicting the risk of death and other adverse outcomes in children who need intensive care, thus improving clinicians’ ability to diagnose AKI. To verify the new criteria, we conducted an analysis in a Chinese pediatric intensive care unit (PICU), aiming to define AKI using the pROCK criteria, to compare its performance for predicting risk of death with the KDIGO criteria, and to investigate the risk factors for AKI.
Methods
Study design
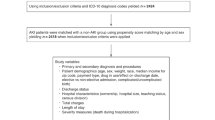
This was a retrospective, clinical observational study utilizing electronic medical record data, which included patients admitted to the PICU from January 2016 to December 2018. The study included 3491 PICU patients aged from 1 month to 18 years who had at least two SCr tests during their hospitalization. We excluded patients diagnosed with end-stage kidney disease (ESKD) or receiving renal replacement therapy or kidney transplantation. For patients with multiple hospitalizations, only their first hospitalization was included (Fig. 1).
Data were extracted from the electronic medical records, which included laboratory and prescription data, age, sex, diagnostic code at admission, in-hospital death, PICU length of stay (LOS), total hospitalization cost, pediatric critical illness score (PCIS), and the level and time of SCr. Pediatric critical illness score was collected to depict the severity of illness at admission, and the lower the score was, the more severe the disease. Serum creatinine evaluations were performed using an enzymatic assay. The baseline estimated glomerular filtration rate (eGFR) was calculated by the updated Schwartz formula: eGFR = 41.3 [height/SCr].20 This study was approved by the Ethics Committee of Anhui Provincial Children’s Hospital, Hefei, China.
Definition and stage of AKI
According to the pROCK criteria, AKI was defined as an increase in the level of SCr of both ≥20 μmol/L and ≥30% over the baseline SCr within 7 days.19 The reference SCr level was represented as the mean value of the SCr within 90 days before PICU admission or the lowest creatinine during hospitalization16 (if the mean SCr aforementioned was not available). Acute kidney injury was classified into three stages as follows: an increase in SCr ≥ 20–39 μmol/L and ≥30–59% increase from baseline SCr was stage 1, an increase in SCr of both ≥40–79 μmol/L and ≥60–119% was stage 2, and an increase of both ≥80 μmol/L and ≥120% was stage 3. Acute kidney injury was also defined using KDIGO criteria, i.e., a ≥50% increase in SCr within 7 days or an absolute increase in SCr of ≥26.5 μmol/L within 2 days (Supplementary Table S3). Since urine output data were not available from our database, only the creatinine criteria were used.
Statistical analyses
R software (http://www.R-project.org) was used for all statistical analyses. Continuous variables were represented as the mean ± standard deviation (SD) or median (interquartile range), while categorical variables were described using proportions. The differences in population characteristics were compared using Student’s t test, Mann−Whitney U tests, signed chi-square tests and Kruskal−Wallis test.
We determined the relationship between AKI severity and the outcomes (in-hospital mortality, PICU daily cost, and PICU LOS) with a Cox proportional hazard model and linear regression models. The concordance between AKI and the survival time was assessed by the Harrell c index of Cox models, and the Akaike information criteria (AICs) of the linear regression model were compared between the pROCK and KDIGO criteria. Generalized linear models with a logit link were used to test the risk effects of age, sex, underlying comorbidities, MV, PCIS, and exposure to drugs on AKI status (binary variables) with adjustments for related factors. A two-tailed P < 0.05 was considered to be statistically significant in all analyses.
Results
Characteristics of study participants
A total of 3338 PICU hospitalizations were included in the final analysis (Fig. 1). In the population, 49%, 37.3%, 12.4%, and 1.29% were infants (1-month to 1-year-old), preschool children (1–5 years old), school children (5–12 years old), and adolescents (12–18 years old), respectively. Participants were grouped according to AKI status defined by the pROCK criteria. Participants with AKI had a higher daily cost (median, 2657 vs 875 yuan; P < 0.01), lower PCIS (mean, 85.4 vs 92.9, P < 0.01), and higher mortality (12.5% vs 1.03%; P < 0.001). Additionally, patients with AKI were more likely to have drug use and MV (11.7% vs 7.43%, P = 0.015). Other characteristics and comorbidities stratified by AKI status are listed in Table 1. During PICU hospitalization, AKI occurred in 257 (7.7%) participants as determined by the pROCK criteria. With respect to AKI stages, there were 123, 83, and 51 patients who were stages 1, 2, and 3, respectively. Characteristics stratified by different age strata were also assessed (Supplementary Table S1).
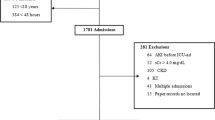
To identify the characteristics of participants with AKI defined by KDIGO who did not meet the pROCK criteria, participants were classified into a new AKI category with three groups: the KDIGO-defined non-AKI group (Group 1, n = 2984), KDIGO-defined AKI as well as pROCK-defined non-AKI group (Group 2, n = 97) and pROCK-defined AKI group (Group 3, n = 257). Of note, all 97 patients in group 2 were from stage 1 based on the KDIGO criteria. We found that most of the characteristics of group 2 were similar to the characteristics of the children in group 1 (Supplementary Table S2).
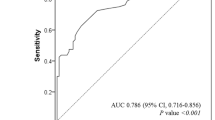
Performance of different AKI definitions for AKI outcomes
Sixty-four deaths in total were observed in 3338 hospitalized children, with in-hospital deaths occurring in 12.5% and 1.03% of the sample with or without AKI defined by pROCK, respectively (Table 1). After adjusting for age, sex, baseline eGFR and PCIS, comorbidities, MV, and exposure to drugs, Cox proportional hazard models for death were developed in both pROCK-defined AKI (HR: 10.5, 95% CI: 6.66–19.5) and KDIGO-defined AKI models (HR: 9.05, 95% CI: 5.38–15.2) to predict the increased risk of death. The model with pROCK-defined AKI produced a higher c index (0.81 vs 0.79, P = 0.013) than the KDIGO model (Table 2). Moreover, the pROCK criteria yielded a better separation between non-AKI and AKI on the survival curves than the KDIGO criteria in this study (Fig. 2). The association between pROCK-defined AKI severity and increased mortality rate was also observed within 8.28 (95% CI: 4.17–16.4), 10.1 (95% CI: 4.60–22.2), and 17.1 (95% CI: 8.05–36.5) for AKI stage 1, stage 2, and stage 3, respectively (Table 2).
After adjusting for confounding factors, linear regression models revealed that AKI was linked to higher daily cost and an increased length of PICU stay during hospitalization (P < 0.05) (Table 2), with lower AIC observed in the model with AKI defined by the pROCK criteria. Children with severe AKI stages defined by pROCK were associated with higher daily cost (stage 1 (β = 1260), stage 2 (β = 2761), and stage 3 (β = 2849)) than children without AKI (P < 0.001 for all). Increased LOS was also observed in children with AKI (β = 2.30, P < 0.001), but no significant differences were observed among different AKI stages.
We also evaluated AKI outcomes with the new AKI category. After adjusting for related confounders, group 2 only showed a trend to better predict mortality compared to group 1 (HR: 3.33, 95% CI: 0.79–9.64). In contrast, compared with group 1, a significantly higher risk of mortality was found in group 3 (HR: 13.3, 95% CI: 7.81–22.6) (Table 3).
Risk factors for pediatric AKI
A multiple logistic regression model was used to estimate the ORs of possible risk factors for pediatric AKI, including age, comorbidities, PCIS, MV, and exposure to drugs (Table 3). Overall, a significant association was found between age and AKI occurrence (Supplementary Fig. S1), with a 23% increase per year (OR: 1.23, 95% CI: 1.06–1.44; P < 0.001). We also estimated the risk effects of comorbidities on AKI occurrence using respiratory diseases as a reference. Cardiovascular diseases (OR: 9.06, 95% CI: 2.17–15.8), tumors (OR: 6.54, 95% CI: 3.94–10.9), metabolic diseases (OR: 12.4, 95% CI: 5.76–25.6), and immune diseases (OR: 4.74, 95% CI: 2.39–8.97) were the potential risk factors in patients with AKI.
Exposure to drugs, such as vancomycin, nonsteroidal anti-inflammatory drugs (NSAIDs), amino glycosides (AG), diuretics, and cardiac inotropes (CI) (with exposure rates of 13%, 30%, 40%, 36.2%, and 8.09%, respectively) was common in this study. Drug exposure was associated with higher odds for AKI, especially exposure to CI (OR: 9.39, 95% CI: 5.36–16.4). In addition, we performed the same analysis with KDIGO-defined AKI, and similar results were observed (Table 2).
Discussion
To our knowledge, this is the first analysis that used the pROCK creatinine criteria to estimate the epidemiologic characteristics of pediatric AKI in a Chinese PICU. We estimated an overall rate of occurrence of AKI of 7.7% during PICU hospitalization and compared the performance for predicting the risk of death and other outcomes with the KDIGO criteria. We also evaluated the potential risk factors for age, underlying comorbidities, PCIS, MV, and exposure to drugs.
It has been reported that even a small increase in SCr has been reported to be associated with worsening prognosis in patients with AKI,21,22 and we also observed that increasing SCr was associated with a higher mortality rate (Supplementary Fig. S2). Without considering the biological and analytical variability of SCr changes, it is impossible to accurately reflect the true change in renal function.23 While taking the RCV of creatinine into account based on age and baseline creatinine level in children, the pROCK criteria have been reported to have a higher probability of accurately predicting the risk of mortality and other adverse outcomes than the KDIGO and pRIFLE criteria, especially in children with intensive care,19 which is appropriate for the present study population.
In this study, both the pROCK and KDIGO criteria were used to define pediatric AKI and its stages. As a result, we found that the incidence of AKI was lower when using the pROCK criteria (7.7% vs 10.6%) compared with the KDIGO creatinine criteria; 97 KDIGO-defined AKI stage 1 children were reclassified as non-AKI by pROCK criteria. The characteristics and mortality of those 97 children were similar to those of children without AKI using the pROCK criteria, which indicated that the reclassification in the population was valuable for avoiding the overdiagnosis of mild AKI using the KDIGO criteria. Moreover, we compared the c index of Cox models between pROCK and KDIGO criteria for predicting the risk of death and found that the pROCK-defined model produced a higher c index (0.81 and 0.79, P = 0.013) (Table 2), which confirmed the better performance of pROCK criteria in predicting the mortality risk. We also defined AKI with the pRIFLE criteria with an incidence of 16.8%, and Cox proportional hazard models for death were also performed with an HR of 8.14 (95% CI: 4.75–13.9) and a c index of 0.76, which is lower than the index for both the pROCK and KDIGO criteria. Thus, we only focused on the comparison between the pROCK and KDIGO criteria.
Acute kidney injury was associated with a higher mortality rate (HR: 11.4; 95% CI: 6.66–19.5), higher daily cost (β = 1907, P < 0.001), and longer LOS (β = 1.54, P = 0.009) according to both the pROCK and the KDIGO criteria, which is consistent with other reports.18,24,25,26 In addition, more severe AKI stages were significantly associated with an increased mortality rate and an increased daily cost (P trend < 0.001). Thus, the mortality rate and daily cost were not only positively associated with AKI but also increased significantly with the progression of AKI. Of note, although AKI was associated with an increased LOS (β = 1.54, P = 0.009), no positive correlation was observed between LOS and AKI stages, which was contrary to previous findings.18,24,25,26,27 The reason for this difference is unclear, but it may be related to the fact that severe patients give up on the treatment.
The incidence of AKI in PICUs and critically ill children has varied greatly in the literature (10−80%), which may result from different AKI definitions, confounders, and study populations.15,18,26,27 Schneider et al.25 reported a lower prevalence of 10% with 3396 PICU admissions, while Hui et al.28 evaluated 140 PICU admissions with an AKI prevalence rate of 56% in a Hong Kong hospital using the same KDIGO definition. In this study, AKI had an estimated incidence of 7.7% in the PICU according to the pROCK criteria, which was much lower than the range of 10−80% that was previously reported using different defining criteria. The lower incidence rate mainly relied on the aforementioned strict definitions (the KDIGO-defined AKI incidence of 10.6% in this study). Moreover, the present study excluded patients diagnosed with ESKD or patients who had undergone maintenance dialysis or kidney transplantation, which may reduce the incidence of AKI in our sample. In addition, the fact that neonates were excluded in this study could be another factor contributing to a lower incidence rate of AKI.
In this study, age and comorbidities were considered to be potential risk factors for AKI. The association between age and AKI incidence remains controversial in the literature.24,26,29 In this study, although no age differences were observed between the AKI and non-AKI groups (P = 0.641), we found that older age was associated with a higher morbidity of AKI (OR: 1.23; 95% CI: 1.04–1.44, P < 0.01), and a J-shaped association was observed after adjustments for related confounders (Supplementary Fig. S1). Comorbidities are considered an important factor in the development of AKI. The present study indicated that cardiovascular disease, tumors, immune disease, and metabolic disease were all linked to a higher incidence of AKI, using respiratory diseases as the reference (Table 3), indicating that additional attention is needed during the treatment of these comorbidities to help prevent AKI.
Drug exposure was reported to be a risk factor for pediatric AKI.30 In our study, approximately three-quarters of children had a history of exposure to drugs such as CI, diuretics, vancomycin, NSAIDs, and AG (Table 4). Among these drugs, exposure to CI was the most significant risk factor for AKI, with an OR of 9.39. It is imperative to avoid the inappropriate use of these drugs for preventing pediatric AKI.
We also evaluated the association between AKI and other factors such as MV and PCIS. The results revealed that MV (OR: 2.26; 95% CI: 1.16–4.32) was a potential risk factor, while PCIS was a protective factor (OR: 0.88; 95% CI: 0.86–0.90) for pediatric AKI, which was consistent with another study.30
Our study had some limitations. First, since the SCr data before hospitalization were lacking for some of the hospitalized children, the baseline SCr was based on in-hospital SCr, which may lead to an underestimation in AKI incidence. Second, both SCr and urine output should be taken into account to define AKI; however, urine output data were not available from our database. Third, we did not estimate the relationship between percent fluid overload and mortality due to lack of data. Fourth, in our current study, the mean age of the participants was about 2.3 years old. Although most of the hospitalized children were infants and preschool children in Chinese PICU and also had a mean age of about 2–3 years,31,32 the generality of the result to other PICUs requires caution.
Conclusions
In summary, we discovered a 7.7% incidence of AKI in Chinese PICU hospitalizations using the pROCK criteria. The pROCK criteria led to a slightly improved prediction of mortality risk when compared with the KDIGO criteria. Older age, underlying comorbidities, MV, decreased PCIS, and exposure to drugs were potential risk factors for AKI.
References
Rudiger, A. & Singer, M. Acute kidney injury. Lancet 380, 1904 (2012).
Kam Tao Li, P., Burdmann, E. A., Mehta, R. L. & World Kidney Day Steering C. Acute kidney injury: global health alert. J. Nephropathol. 2, 90–97 (2013).
Volpon, L. C. et al. Epidemiology and outcome of acute kidney injury according to pediatric risk, injury, failure, loss, end-stage renal disease and kidney disease: improving global outcomes criteria in critically ill children—a prospective study. Pediatr. Crit. Care Med. 17, e229–e238 (2016).
Kaddourah, A., Basu, R. K., Bagshaw, S. M., Goldstein, S. L. & Investigators, A. Epidemiology of acute kidney injury in critically ill children and young adults. N. Engl. J. Med. 376, 11–20 (2017).
Xu, X. et al. Epidemiology and clinical correlates of AKI in Chinese hospitalized adults. Clin. J. Am. Soc. Nephrol. 10, 1510–1518 (2015).
Yang, L. et al. Acute kidney injury in China: a cross-sectional survey. Lancet 386, 1465–1471 (2015).
Lunyera, J., Kilonzo, K., Lewington, A., Yeates, K. & Finkelstein, F. O. Acute kidney injury in low-resource settings: barriers to diagnosis, awareness, and treatment and strategies to overcome these barriers. Am. J. Kidney Dis. 67, 834–840 (2016).
Yang, L. Acute kidney injury in Asia. Kidney Dis. 2, 95–102 (2016).
Lameire, N., Van Biesen, W. & Vanholder, R. Epidemiology of acute kidney injury in children worldwide, including developing countries. Pediatr. Nephrol. 32, 1301–1314 (2017).
Xu, X. et al. Acute kidney injury among hospitalized children in China. Clin. J. Am. Soc. Nephrol. 13, 1791–1800 (2018).
Chang, J.-W. et al. The epidemiology and prognostic factors of mortality in critically ill children with acute kidney injury in Taiwan. Kidney Int. 87, 632–639 (2015).
Zappitelli, M. et al. Association of definition of acute kidney injury by cystatin C rise with biomarkers and clinical outcomes in children undergoing cardiac surgery. JAMA Pediatrics 169, 583 (2015).
Rheault, M. N. et al. AKI in children hospitalized with nephrotic syndrome. Clin. J. Am. Soc. Nephrol. 10, 2110–2118 (2015).
Ingelfinger, J. R., Kalantar-Zadeh, K., Schaefer, F. & World Kidney Day Steering C. Averting the legacy of kidney disease: focus on childhood. Nephrol. Dial. Transpl. 31, 327–331 (2016).
Akcan-Arikan, A. et al. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 71, 1028–1035 (2007).
Group, K. A. W. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2, 1–138 (2012).
Mehta, R. L. et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit. Care 11, R31 (2007).
Sutherland, S. M. et al. AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin. J. Am. Soc. Nephrol. 10, 554–561 (2015).
Xu, X. et al. A new criterion for pediatric AKI based on the reference change value of serum creatinine. J. Am. Soc. Nephrol. 29, 2432–2442 (2018).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Chertow, G. M., Burdick, E., Honour, M., Bonventre, J. V. & Bates, D. W. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J. Am. Soc. Nephrol. 16, 3365–3370 (2005).
Lassnigg, A. et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J. Am. Soc. Nephrol. 15, 1597–1605 (2004).
Thomas, M. E. et al. The definition of acute kidney injury and its use in practice. Kidney Int. 87, 62–73 (2015).
Bailey, D. et al. Risk factors of acute renal failure in critically ill children: a prospective descriptive epidemiological study. Pediatr. Crit. Care Med. 8, 29–35 (2007).
Schneider, J., Khemani, R., Grushkin, C. & Bart, R. Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit. Care Med. 38, 933–939 (2010).
Soler, Y. A., Nieves-Plaza, M., Prieto, M., Garcia-De Jesus, R. & Suarez-Rivera, M. Pediatric risk, injury, failure, loss, end-stage renal disease score identifies acute kidney injury and predicts mortality in critically ill children: a prospective study. Pediatr. Crit. Care Med. 14, e189–e195 (2013).
Kavaz, A. et al. Acute kidney injury in a paediatric intensive care unit: comparison of the pRIFLE and AKIN criteria. Acta Paediatr. 101, e126–e129 (2012).
Hui, W. F., Chan, W. K. & Miu, T. Y. Acute kidney injury in the paediatric intensive care unit: identification by modified RIFLE criteria. Hong Kong Med. J. 19, 13–19 (2013).
Zappitelli, M. et al. A small post-operative rise in serum creatinine predicts acute kidney injury in children undergoing cardiac surgery. Kidney Int. 76, 885–892 (2009).
Moffett, B. S. G. S. Acute kidney injury and increasing nephrotoxic-medication exposure in noncritically-ill children. Clin. J. Am. Soc. Nephrol. 6, 856–863 (2011).
Qiu, J. et al. Comparison of the pediatric risk of mortality, pediatric index of mortality, and pediatric index of mortality 2 models in a pediatric intensive care unit in China: a validation study. Medicine 96, e6431 (2017).
Wang, D. et al. Medical adhesive-related skin injuries and associated risk factors in a pediatric intensive care unit. Adv. Ski. Wound Care 32, 176–182 (2019).
Acknowledgements
We thank all the participants of the study for their valuable contributions. This work was supported by the Key Research and Development Program Projects in Anhui, China (ID: 1704a0802172).
Author information
Authors and Affiliations
Contributions
C.W., G.H., F.H., and L.H. made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; C.W., F.H., L.H., J.D., and Q.X. contributed to the draft of the article or revising it critically for important intellectual content. J.D. contributed to the study on data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Informed consent was waived for the retrospective nature and the lack of participant interaction.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wei, C., Hongxia, G., Hui, F. et al. Impact of and risk factors for pediatric acute kidney injury defined by the pROCK criteria in a Chinese PICU population. Pediatr Res 89, 1485–1491 (2021). https://doi.org/10.1038/s41390-020-1059-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1059-3