Abstract
Children are uniquely susceptible to the health consequences of water contamination. In this review, we summarize the existing, robust literature supporting the importance of examining specific water contaminants (i.e., lead, pesticides, nitrates, arsenic, perchlorate) and the routes of contamination in the United States and globally. We also discuss the health effects of exposure to contaminated water and significant disparities related to access to clean water. Lastly, we offer strategies for prevention and intervention—including those focused on the individual patient level—and review the current US policy framework pertaining to regulation of these toxicants.
Impact
-
A key message in this article is that exposure to water contaminants have serious and long-lasting consequences on children’s health.
-
This review summarizes current existing literature and adds policy recommendations supporting clean water for children.
-
Information from this review has two potential impacts:
-
Guide health professionals in screening and/or treating children’s health problems resulting from water contaminant exposure.
-
Guide policy makers in using evidence-based approaches to improve water quality and clean water access.
Similar content being viewed by others
Introduction
Providing safe drinking water is a challenge both in the United States and globally. The World Health Organization (WHO) 2017 report on drinking water, sanitation, and hygiene showed that three in ten people globally lack access to clean water at home.1 In the United States, safe drinking water is generally available in most areas.2 However, analysis of violations to the Safe Drinking Water Act indicated that 9–45 million Americans were exposed to contaminated water between 1982 and 2015.2 Events such as the Flint water crisis further highlight that, despite widespread availability of high-quality drinking water in the United States, more work is needed to provide safe drinking water in all communities.
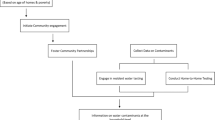
Several sources of water contamination exists (Fig. 1).3 Agriculture and urbanization significantly contributes to water pollution (Fig. 2). Runoff from farms, ranches, or animal feeding operations may contain chemicals derived from the excessive use of fertilizers and pesticides.4 These chemicals can impact water quality, particularly in nearby rivers, lakes, and groundwater.4 Increasing population density, a consequence of greater urbanization, also contributes to pollution.5 Wastewater from buildings, households, and construction contain contaminants that may be discharged into groundwater or surface waters if incompletely removed by water treatment plants.5
Children are uniquely susceptible to the health consequences of contamination. Compared to adults, children have a higher likelihood of exposure since they consume more food and water in proportion to their body weight.6 Stages of development also play a role in children’s vulnerability to contaminants. For example, young children may be at higher risk of coming in contact with or ingesting chemicals when they are teething, putting objects in their mouth, or crawling on the ground.7 Prenatally, exposures during crucial periods of organ development may increase their vulnerability to congenital anomalies. Postnatally, central nervous system development is affected, with animal studies showing effects on synaptic plasticity, neuronal numbers, neuron migration, and myelin deposition.8 These factors increase children’s susceptibility to the health effects of water contamination, thereby placing them at higher risk for long-term disease, disability, and death.6,9
The purpose of this review is to summarize the literature regarding the health outcomes of lead, pesticides, arsenic, nitrate, and perchlorate contamination of water. We summarize water standards for these chemicals by the WHO,10 Environmental Protective Agency (EPA),11 and Health Canada12 (Table 1). We also discuss current policies and prevention and research opportunities that may guide pediatricians and policy makers in addressing environmental risks (Table 2). Although a wide range of contaminants can be found in water, we focus on select chemicals given their mechanisms of contamination, important implications in childhood exposure and health effects, and potential for prevention of exposure via policy change. Information on other types of water contaminants can be found in other resources.13 We also focus on exposures most relevant to children living in the United States.
Select contaminants and their health outcomes
Lead
Children are exposed to lead through various sources. These include drinking water, chips from old paint, toys, toy jewelry, playing in fields with lead-contaminated dust or soil, and imported products such as candy. The presence of other metals also plays a role in lead exposure. Among infants aged 6 and 12 months, low calcium, iron, and zinc blood levels were associated with increased lead absorption.14 In adults, bone turnover during pregnancy, breastfeeding, and periods of calcium deficiency releases stored lead into blood, thereby affecting both maternal and fetal blood lead levels (BLLs).8,14
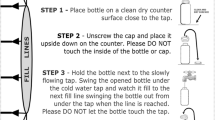
The EPA estimates that 20% of total lead exposures in the United States occur due to water consumption.15 In infants, estimates can be as high as 60% since tap water is frequently used to reconstitute formula.15 For example, a case study described an infant with plumbism due to daily intake of powdered formula that was prepared with home tap water having a first-draw lead content of 130 parts per billion (p.p.b.).16 School-age children may also be at particular risk for lead exposure, given that only 10% of schools nationwide are required to comply with the EPA’s standards for water lead levels.17
The presence of lead in drinking water can be attributed to plumbing materials used in cities and buildings.15 As water leaves treatment plants, it travels through lead-based materials such as pipes and solder. Water fountains and faucets found in buildings and homes also contain equipment made from lead. The EPA mandates that anti-corrosive chemicals must be added in water to prevent these materials from oxidizing.18 However, failure to use chemicals to control corrosion, such as the case in Flint, Michigan, can cause leach from lead service lines, lead solder, and brass fittings.15,19
There are currently no known safe BLLs. At levels of exposure below 5 µg/dL, sufficient evidence shows that children experience decreased academic achievement, lower intelligent quotient (IQ) scores, and increased risks for attention-deficit/hyperactivity disorder.20 At <10 µg/dL, exposure can result in delayed puberty, reduced postnatal growth, and hearing difficulties.20 Early-age lead exposure is further associated with various types of antisocial behaviors, with studies documenting a link between blood or bone lead concentrations and aggression, conduct disorder, and delinquent or criminal behaviors.20 Finally, at levels >10 µg/dL, multiple organ systems are affected, which can result in anemia due to heme synthesis disruption, abdominal pain, vomiting, poor nerve function, and loss of muscle control.3
Exposure during pregnancy has implications for both maternal health and infant development. Lead exposure is also linked to spontaneous abortions, stillbirth, and preterm labor, particularly at levels above 10 µg/dL.21,22,23 Relative to 0 μg/dL, maternal BLLs even at <5 µg/dL are associated with adverse birth outcomes, including reduced infant growth and low birth weight.21,24 Effects on neurodevelopment are also well documented, with studies linking maternal BLL above 5 µg/dL during the first trimester to lower scores on the Neonatal Behavioral Neurological Assessment and Child Development Inventory.25,26
Pesticides
Pesticide contamination of drinking water can be attributed to its widespread use in homes and agriculture. For example, runoff from farms or gardens enter streams that may feed into water supplies.27 Pesticides can also seep into the soil where they eventually come in contact with groundwater.27 Although the ingestion of pesticides is predominantly from foods that have been treated with them, people may be exposed to pesticides (i.e., insecticides, herbicides, and fungicides) in some water supplies given that they may not be removed by conventional drinking water treatment technologies.28 In a 10-year study by the US Geological Survey, pesticides were found in over 50% of sampled wells from shallow groundwater tapped beneath agricultural and urban areas with atrazine, a herbicide being the most frequently detected pesticide group in agricultural areas.29
When acutely exposed to pesticides, symptoms include nausea, vomiting, eye irritation, coughing, and shortness of breath.6 Long-term exposure can result in adverse health effects.
Prenatal exposure to pesticides is associated with poor cognitive function in school-aged children,30 lower scores on tests that examined working memory, reasoning, comprehension and IQ among Latino agricultural families,31 and higher rates of autism spectrum disorder.32 Aside from neurological effects, pesticides can affect musculoskeletal development. Recent evidence suggests that maternal exposure to agricultural pesticides increases the risk of abdominal wall birth defects such as gastroschisis.33
Arsenic
The element arsenic is a widely distributed metalloid in the environment.34 Existing as either organic, inorganic, or gaseous compounds, arsenic can be found in soils, rocks, food, water, and air.34 Release of arsenic into the environment occurs through both natural and human processes. Natural processes include erosion of ores and sediments, volcanic eruptions, and the flow of groundwater through shallow aquifers containing high levels of arsenic.34,35 In the latter case, mining and commercial use contribute to arsenic dispersal in the environmental.36 Geography also contributes to arsenic levels. Drinking water supplies in the southwestern United States have particularly high levels of arsenic, likely due to factors such as irrigation, pH, reducing conditions, and climate that increase the solubility of arsenic in groundwater.37,38
Although arsenic is a known occupational hazard, water intake usually serves as a source of exposure. Infants and school-age children may be at particular risk for arsenic exposure. A report by the Environmental Integrity Project indicated that several California school districts were found to have high levels of arsenic in their water.39 In infants, exposure depends on whether the child is breast- or formula-fed. Breastfed infants have lower arsenic exposure than formula-fed infants40 and the use of tap water in formula has been associated with increased arsenic levels in 6-week-old infants.40 Prenatal exposure may also occur since arsenic readily crosses the placenta.41
While the WHO considers its organic form as non-toxic, inorganic arsenic is associated with negative health outcomes that affect a wide range of organ systems.42,43 For example, issues stemming from chronic arsenic exposure include dermal issues (hyperpigmentation, keratosis, and skin lesions) to hypertension and peripheral neuropathy.43 The International Agency for Research on Cancer also considers inorganic arsenic compounds to be carcinogenic. Numerous studies have documented a strong association between arsenic exposure with skin, urinary bladder, and lung cancers, particularly among individuals exposed through elevated arsenic in drinking water.43 Furthermore, exposure to arsenic impacts cognitive function. For example, arsenic levels above 5 µg/L resulted in lower IQ scores among children grades 3–5 living in Maine.44
Prenatal exposure also has various consequences, particularly on birth outcomes, development, and epigenetics. Studies have shown that increased maternal urinary arsenic levels are associated with respiratory problems in infants 12 months or younger45 and lower birth weights among females born to obese mothers.46 Additionally, in an analysis of cord blood samples, changes in DNA methylation and messenger RNA expression in genes encoding for binding transcription factors were associated with high maternal urinary arsenic levels.47 These epigenetic changes have implications on birth outcomes (e.g., preterm birth) and long-term health (e.g., higher mortality and cancer).47,48
Perchlorate
Perchlorate is used as an oxidizing agent in rocket fuel, explosives, fireworks, road flares, or may occur naturally in groundwater or soil.49,50 Additionally, perchlorate may be found in drinking water from bleach (hypochlorite) degradation as bleach is used to disinfect drinking water.51 Human exposure may occur from water contamination, in vegetables via water or fertilizer, or cow and human milk, and can be assessed by spot urine analysis.49 Analysis of the Food and Drug Association’s Total Diet Study determined that 74% of food samples tested had detectable amounts of perchlorate.52 Furthermore, the source of exposure by age was highest with baby food and formula/dairy products in infants 6 months to 11 months, dairy products in children 2, 6, and 10 years, and vegetables and dairy in adolescents and adults.52
In US residents 6 years and older, based on data from the National Health and Nutrition Examination Survey, Blount et al.49 found that all subjects had detectable amounts of perchlorate, suggesting pervasive exposure to at least small amounts. Interestingly, there were little differences by race and ethnicity.53
Perchlorate competitively inhibits thyroid uptake of iodide via the sodium-iodide symporter.54 It is the same symporter expressed in human mammary tissue that allows perchlorate to enter human milk.49 Perchlorate has a much higher affinity for the symporter than other substances, which may inhibit thyroid uptake of iodine (i.e., nitrates).51 Exposure of women at least 12 years of age to perchlorate has also been linked to increased thyroid-stimulating hormone, regardless of intake of iodine and decreased total thyroxine levels when intake of iodine is <100 µg/L.55 This effect on thyroxine level in women of reproductive age could translate into the fetus and infant impact, especially in breastfeeding infants, as lower thyroid hormone levels in mothers have been associated with lower IQ and poorer neurodevelopment in their progeny.51 This is due to the fetus in the first trimester being dependent on maternal thyroid hormones for proper development. Exposures at other times of fetal or early childhood also impact growth.56 Taylor et al.57 found that mothers with suboptimal thyroid function with perchlorate levels in the top 10% had a higher risk of having offspring with lower IQ at 3 years of age, especially verbal IQ, irrespective of levothyroxine therapy.
Nitrates
Nitrates can be found in well water as a result of human or animal waste and fertilizer contamination of the water.58,59 It can also occur when excess nitrogen is deposited via fossil fuel combustion and nitrogen-fixing plants, including soybeans.60 About half of the nitrogen deposited in land and used in agriculture moves to surface and groundwater.60 The maximum contaminant levels are monitored in public water supplies, but potentially less closely monitored with private wells.60,61
Nearly 14% of the US population has private wells, with 6% of these having elevated nitrate levels in comparison with 2% elevated nitrate levels in public supply wells.60 The location of the well is also important: 21% of the private wells in agricultural regions had elevated levels in comparison with 6% of private wells overall.60
One of the primary concerns related to high levels of nitrate (NO3−) is methemoglobinemia in infants.61 Methemoglobin is formed in the presence of nitrites (converted from ingested nitrates) and leads to methemoglobinemia when it is >10% of all the hemoglobin.34,61 Babies 4 months and younger are especially susceptible to nitrate-induced methemoglobinemia since fetal hemoglobin more easily oxidizes into methemoglobin.34
Nitrates compete with iodine uptake by interfering with the sodium iodide-symporter in the thyroid, thus disrupting thyroid function.56,61 However, perchlorate has a higher affinity for the thyroid than nitrate.54,62 Four of five studies in a 2018 review by Ward et al.60 demonstrated increased risk for subclinical hypothyroidism with exposure to drinking water nitrates among women, pregnant women, and children. One study linked thyroid cancer with nitrate intake.60
A recent review examined pregnancy outcomes in association with maternal intake of nitrates. The studies assessed demonstrated mixed results regarding spontaneous abortions, prematurity, small for gestational age, and low birth weight.60,61 Further, in examining congenital anomalies in the context of maternal drinking water nitrate intake, five of six studies reviewed found an increased risk of neural tube or central nervous system defects.60
Nitrate is converted to nitrite in the human body and then may undergo nitrosation with amines and amides to N-nitroso compounds (NOCs).34,61,63 Since most NOCs are carcinogens, the International Agency for Research on Cancer to classify nitrates and nitrites when nitrosated as Group 2A (“probably carcinogenic to humans”).34,63 The nitrate ingested from water is quickly absorbed via the gastrointestinal tract and transported through blood, which perfuses the salivary glands.60 In saliva, the nitrate is concentrated as high as 20 times more than blood, and some salivary nitrate is converted by oral bacteria into nitrite.60 The saliva is then swallowed exposing the gastrointestinal tract again to nitrates and nitrites to be converted to NOCs.60 NOC conversion can be inhibited by dietary intake of compounds, such as Vitamin C or polyphenols.60 There is, to this end, emerging evidence with four of five studies suggesting an associated risk of colorectal or colon cancer.60
Disparities related to access to clean water and their health effects
Significant disparities related to clean water access and the health effects of exposure to contaminated water exist. One prime example of this is the water crisis in Flint, where poorer communities were disparately affected with higher resultant lead levels. Further, low-income and minority communities may be more malnourished and iron deficient,64 making toxicity more likely due to increased gastrointestinal absorption of lead and other heavy metals.65,66
Despite advancements in water infrastructure, access to clean water continues to be a challenge in many US households.67 Mack and Wrase67 found that almost 12% of US households make US$32,000 or less, meaning that they spend a large proportion of their income paying for water services. These households are concentrated in low-incomes states and metropolitan areas with a high percentage of people who are disabled, uninsured, and unemployed. Hanna-Attisha et al.68 found that during the Flint water crisis, the highest predicted BLLs occurred in areas that have had significant demographic change, an increase in poverty, and an increase in vacant properties.
Racial and ethnic disparities have also been described by several studies examining water contamination. For instance, American Indians and Alaska Natives continuously face contamination of drinking and recreational water, in addition to environmental hazards from mining, military, and agricultural exposures.69 Average BLLs are also usually highest among Black children, particularly those from low-income families.70 Recent events beyond the Flint water crisis highlight this disparity, with reports indicating poor water quality in New York City and Newark among predominantly low-income, Black communities and schools.71,72 Within the Latino community, a study examining the water systems in California’s San Joaquin Valley showed that Latino families disproportionately had higher nitrate levels in their drinking water compared to non-Latino whites and non-Latino people of color.73 Further, immigrant Latinos living in “colonias”—unincorporated areas along the US–Mexico border—are at particular risk for water contamination, given the lack of infrastructure available to regulate their water and sewage systems.74 Water contamination also affects Asian American communities. In 1979, groundwater running along the San Gabriel Valley, an area with a large Asian American community, was found to be contaminated with volatile organic compounds.75,76 The EPA has ordered the private companies responsible to treat the area’s contaminated wells and groundwater, but treatment is not expected to end until 2030.75,77
Policy implications and recommendations
Overview and approach to regulation
Generally, federal policy on contaminants vacillates between degrees of stringency of regulation based on political climate. Relaxation of national standards on air and water protections runs the potential risk of increase exposure of water sources to contaminants. Actions on environmental regulations should be undertaken deliberately, with solicited input from pediatric stakeholders and attention to the impact changes in regulation may have on child health. Proposed changes to environmental reforms should follow the standard federal procedure for rule-making, which is designed to allow for expert opinion. Executive orders should be limited because they may limit solicited input.78,79 Overall regulation related to water quality standards should seek to ensure broad protections for federally protected bodies of water. Actions to limit the scope of federally protected water supplies should themselves be curtailed.80
Ensuring agencies such as the EPA received adequate resources is critical toward optimizing child health protections. Thus, budgets for these agencies should not be reduced, especially during periods of environmental de-regulation.81 Officers charged with specifically addressing the health of children and studying the impact of policies on child health, such as the EPA’s Office of Child Health Protections, the National Institutes of Child Health and Development, and the National Institute of Environmental Health Sciences should be safeguarded from budget reductions in order to be sufficiently resourced to carry out research, which informs further policy development.82
In assessing the potential risks of an exposure, agencies should have available all relevant scientific data that has been peer-reviewed. Rules restricting the types of peer-reviewed studies that can be considered in evaluating regulations on health should be discouraged.83,84,85
Lead
As data indicate that there is no safe level of lead in children, policies should move toward reducing sources of lead exposure via all portals of entry.86,87 The newly released EPA water standards11 (15 µg/L) are not sufficiently low to protect children. The AAP policy statement summarized studies that found blood lead concentrations below 5 µg/dL (50 p.p.b.), is a causal risk factor for impaired cognition, higher rates of neurobehavioral disorders, and lower birth weight in children.20,88 Newly released guidance from Health Canada recommends that the maximum acceptable concentration for total lead in drinking water is 0.005 mg/L (5 µg/L).89 States also have authority to set specific lead levels, which trigger public health investigations and access to special services. New York has proposed to lower this action level from 10 µg/dl to better comply with current data and CDC recommendations, which is considering lowering the level of concern to 3.5 µg/dl.90 Although concerns exist as to whether laboratories can discern levels this low and still be within standard testing errors, there remain fiscal implications related to increased costs for evaluation and treatment; it is clear that enforcement of this policy is a reasonable and long-term cost-effective approach to reducing childhood lead exposure.90 All states should consider this regulation.
Pesticides
The US EPA is mandated to consider contributions of exposures from drinking water when establishing standards for pesticides in foods. Although not found in water, clinicians and policy makers should know about policy related to organophosphates due to their known adverse health effects.91 The EPA regulates organophosphate pesticide exposures due to their known adverse health effects.91 Proposed changes to regulation regarding use of organophosphate pesticides have been repeatedly delayed.92,93,94 In August of 2017, the federal courts ordered the EPA to enforce the ban on the pesticide within 60 days.95 As regulatory practices continue to unfold, rules on the limitations on use should be based on current data, including calculations of cumulative risk, which include inhalation exposures.96 While legislation to ban use of the pesticide nationally has been introduced, the delay in regulation of these compounds suggests that lawmaking at the state level may result in faster reductions in childhood exposures (Senate Bill 921).97 Hawaii banned use of the pesticide within the state in 2018, and New York, California, Oregon, and Connecticut are also considering similar legislation (Hawaii Bill SB3095 and National Resources Defense Council).98,99
Arsenic
While arsenic has been a source of concern in food products and water sources, there has not been significant regulatory action on regulating arsenic levels. Currently, a pending bill in Congress would direct the Food and Drug Administration to set a maximum permissible level of inorganic arsenic for rice and rice-containing products.100 Another important consideration is the challenges in making water safe in public drinking water versus private wells. For instance, in the United States, arsenic is not federally regulated in private wells. Nigra et al.101 describe a decline in urinary arsenic among public water users, but not private well users, in the US population between 2003 and 2014.101
Perchlorate
The EPA reference dose for perchlorate in drinking water is 7 µg/kg/day. The recommended drinking water equivalent level for consideration is calculated at 24.5 p.p.b.—a level that would trigger clean-up efforts under the Comprehensive Environmental Response Compensation and Liability Act of 1980.102 However, EPA efforts to create a drinking water regulation for perchlorate have been ongoing for almost two decades.94,103 Over that time, significant new data has been accumulated about the potential dangers of perchlorate at low levels.103 Regulation and guidance on this issue should be expedited, and levels of safety and concern must consider the impact of levels in the 1st and 2nd trimesters of pregnancy, newer guidelines defining hypothyroxinemia based on age and pregnancy status and model iodine intake.104 States, however, have created their own tolerances. California limited water levels to 6 p.p.b. and Massachusetts to 2 p.p.b.94
Nitrates
The maximum level for nitrate contamination is set by the EPA at 10 mg nitrate-N/L.105 The percentage of public water systems in violation of this EPA standard has been increasing from 0.28% in 1994 to 0.32% in 2016.106 However, the number of people reliant upon systems that exceed this standard has decreased from an estimated 1.5 million to 200,000.106,107 Regulation of nitrate has been successful in Europe, which in 1991 enforced specific agricultural practices in areas deemed “nitrate vulnerable.”60 Levels of nitrate across Europe have averaged 4 mg Nitrate-N/L since the 1990s.60 In 2016, the EPA released proposals to protect water quality from contaminants, emphasizing nitrates.108 The memo called for a $600,000 increase in funding to provide technical support to states and water authorities, prioritizing areas at greatest risk for nitrate contamination.109 Similar to the European Nitrate Directive, the EPA suggested an incremental approach to increased regulation.109 Based on this, major EPA actions should consider mimicking effective European regulation and adhere to the agency’s internal recommendations to move toward a goal of 100% compliance of public water systems with acceptable nitrate levels.
Research gaps
More research is needed to understand the impact of the toxins at different stages of exposure. These exposures include during pre-conception, pregnancy, through breastfeeding, and across the lifecourse. Also, more studies are needed to study contaminants in combination or in mixtures as few are only exposed to a single toxin, but rather several at the same time in various mixtures. Finally, emerging chemical risks need to be further explored, including perfluoroalkyl and polyfluoroalkyl substances (PFAs). PFAs, which enter drinking water via the manufacturing of items, such as nonstick cookware, clothing, stain repellants, and electronic equipment, have been associated with developmental effects and cancer.110
In order to tackle complex, research questions, “team science” has become increasingly common across all fields of research. For example, the National Academy of Sciences, Engineering, and Medicine Gulf Research Program is an independent, science-based program that was created as part of the settlement aftermath of the Deepwater Horizon disaster, the largest offshore oil spill in US history. Its goal is to expedite advances in science, practice, and capacity to generate long-term benefits for the Gulf of Mexico region and the nation.111 Such unique cross-sector collaborations can foster the societal transformation necessary to achieve decreases in water contamination.
Conclusion
Recent environmental disasters suggests higher levels of water contamination than are acceptable.112 The Flint water crisis particularly demonstrates this issue, with studies showing the 90th percentile of water lead levels at 25 p.p.b. As an essential resource, contaminant-free water is an environmental right. Initiatives are needed to mitigate contamination, including more research on acceptable levels of contaminants, demographic risk factors, and the mechanism by which contaminants create harm. More research will allow us to both better understand which populations are at risk and provide treatments for exposed individuals. This is particularly true given the unique vulnerabilities of children and fetuses who may disproportionally suffer harm from exposure. Further, changes at the policy level are important in addressing water contamination. Current federal regulations on these toxicants are bureaucratic and lead to incremental and slow change. However, recent federal actions taking into account the most current data seem to have over-ruled several administrative actions, which may adversely impact contaminant levels. As pediatricians, we must therefore advocate for opportunities for research dollars, family and community safety, and legislative policies to support a safe environment.
References
World Health Organization, United Nations Children’s Fund. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines (2017).
Allaire, M., Wu, H. & Lall, U. National trends in drinking water quality violations. Proc. Natl Acad. Sci. USA 115, 2078–2083 (2018).
Etzel, R. A. & Balk S. J. Drinking Water. Pediatric Environmental Health 4th edn, 277–291 (American Academy of Pediatrics, 2018).
US Environmental Protection Agency Nonpoint Source Control Branch. Protecting Water Quality from Agricultural Runoff (US Environmental Protection Agency Nonpoint Source Control Branch, Washington, 2005).
Pal, A., He, Y., Jekel, M., Reinhard, M. & Gin, K. Y. Emerging contaminants of public health significance as water quality indicator compounds in the urban water cycle. Environ. Int. 71, 46–62 (2014).
Galvez, M. P. & Balk, S. J. Environmental risks to children: prioritizing health messages in pediatric practice. Pediatr. Rev. 38, 263–79. (2017).
Council on Environmental Health. Chemical-management policy: prioritizing children’s health. Pediatrics 127, 983–990 (2011).
Ettinger, A. S. & Wengrovitz, A. G. Guidelines for the Identification and Management of Lead Exposure in Pregnant and Lactating Women (Centers for Disease Control and Prevention, 2010).
Landrigan, P. J. et al. The Lancet Commission on pollution and health. Lancet (Lond., Engl.) 391, 462–512 (2018).
World Health Organization Drinking Water Quality Guidelines. https://www.who.int/water_sanitation_health/publications/drinking-water-quality-guidelines-4-including-1st-addendum/en/.
Enivironmental Protective Agency Regulated Drinking Water Guidelines. https://19january2017snapshot.epa.gov/ground-water-and-drinking-water/table-regulated-drinking-water-contaminants_.html#seven (2017).
Guidelines for Canadian Drinking Water Quality. Health Canada https://www.canada.ca/en/health-canada/services/environmental-workplace-health/reports-publications/water-quality/guidelines-canadian-drinking-water-quality-summary-table.html (2019).
Environmental Protection Agency. Environments and Contaminants: Drinking Water Contaminants (Environmental Protection Agency, 2017).
National Toxicology Program, United States Department of Health and Human Services. NTP Monograph on Health Effects of Low-Level Lead (2012).
Triantafyllidou, S. & Edwards, M. Lead (Pb) in tap water and in blood: implications for lead exposure in the United States. Crit. Rev. Environ. Sci. Technol. 42, 1297–1352 (2012).
Shannon, M. & Graef, J. W. Lead intoxication from lead-contaminated water used to reconstitute infant formula. Clin. Pediatr. 28, 380–382 (1989).
Lambrinidou, Y., Triantafyllidou, S. & Edwards, M. Failing our children: lead in U.S. school drinking water. New solutions. J. Environ. Occup. Health Policy 20, 25–47 (2010).
Lead and Copper Rule. https://www.epa.gov/dwreginfo/lead-and-copper-rule (1991).
Pieper, K. J., Tang, M. & Edwards, M. A. Flint water crisis caused by interrupted corrosion control: investigating “ground zero” home. Environ. Sci. Technol. 51, 2007–2014 (2017).
Council on Environmental Health. Prevention of Childhood Lead Toxicity. Pediatrics 138, e20161493 (2016).
Agency for Toxic Substances and Disease Registry. Case Studies in Environmental Medicine: Lead Toxicity (2017).
Borja-Aburto, V. H. et al. Blood lead levels measured prospectively and risk of spontaneous abortion. Am. J. Epidemiol. 150, 590–597 (1999).
Taylor, C. M., Golding, J. & Emond, A. M. Adverse effects of maternal lead levels on birth outcomes in the ALSPAC study: a prospective birth cohort study. BJOG 122, 322–328 (2015).
Zhu, M., Fitzgerald, E. F., Gelberg, K. H., Lin, S. & Druschel, C. M. Maternal low-level lead exposure and fetal growth. Environ. Health Perspect. 118, 1471–1475 (2010).
Liu, J. et al. Lead exposure at each stage of pregnancy and neurobehavioral development of neonates. Neurotoxicology 44, 1–7 (2014).
Vigeh, M., Yokoyama, K., Matsukawa, T., Shinohara, A. & Ohtani, K. Low level prenatal blood lead adversely affects early childhood mental development. J. Child Neurol. 29, 1305–1311 (2014).
U.S. Geological Survey. Pesticides in ground water: current understanding of distribution and major influences: U.S. Geological Survey Fact Sheet 1995–244, p. 4, https://pubs.usgs.gov/fs/1995/0244 (1996).
US EPA Office of Water. A Review of Contaminant Occurrence in Public Water Systems (1999).
Gilliom, R. J. Pesticides in U.S. streams and groundwater. Environ. Sci. Technol. 41, 3408–3414 (2007).
Liu, J. & Schelar, E. Pesticide exposure and child neurodevelopment: summary and implications. Workplace Health Saf. 60, 235–243 (2012).
Bouchard, M. F. et al. Prenatal exposure to organophosphate pesticides and IQ in 7-year-old children. Environ. Health Perspect. 119, 1189–1195 (2011).
Roberts, E. M. et al. Maternal residence near agricultural pesticide applications and autism spectrum disorders among children in the California Central Valley. Environ. Health Perspect. 115, 1482–1489 (2007).
Shaw, G. M. et al. Early pregnancy agricultural pesticide exposures and risk of gastroschisis among offspring in the San Joaquin Valley of California. Birth Defects Res. Part A 100, 686–694 (2014).
Case Studies in Environmental Medicine. https://www.atsdr.cdc.gov/csem/csem.html (2018).
Arsenic and Drinking Water from Private Wells. https://www.cdc.gov/healthywater/drinking/private/wells/disease/arsenic.html (2015).
Arsenic Toxicity. https://www.atsdr.cdc.gov/csem/arsenic/docs/arsenic.pdf (2009).
Welch, A., Westjohn, D., Helsel, D. & Wanty, R. Arsenic in ground water of the United States—occurrence and geochemistry. Ground Water 38, 589 (2000).
Ayotte, J. D., Medalie, L., Qi, S. L., Backer, L. C. & Nolan, B. T. Estimating the high-arsenic domestic-well population in the conterminous United States. Environ. Sci. Technol. 51, 12443–12454 (2017).
Pelton, T., Bernhardt, C. & Schaeffer, E. Arsenic in California Drinking Water: Environmental Integrity Project (2016).
Carignan, C. C. et al. Estimated exposure to arsenic in breastfed and formula-fed infants in a United States cohort. Environ. Health Perspect. 123, 500–506 (2015).
Punshon, T. et al. Placental arsenic concentrations in relation to both maternal and infant biomarkers of exposure in a US cohort. J. Expo. Sci. Environ. Epidemiol. 25, 599–603 (2015).
Cubadda, F., Jackson, B. P., Cottingham, K. L., Van Horne, Y. O. & Kurzius-Spencer, M. Human exposure to dietary inorganic arsenic and other arsenic species: state of knowledge, gaps and uncertainties. Sci. Total Environ. 579, 1228–39. (2017).
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Arsenic, metals, fibres, and dusts. IARC Monogr. Eval. Carcinog. Risks Hum. 100, 11–465 (2012).
Wasserman, G. A. et al. A cross-sectional study of well water arsenic and child IQ in Maine schoolchildren. Environ. Health Glob. Access Sci. Source 13, 23 (2014).
Farzan, S. F. et al. Infant infections and respiratory symptoms in relation to in utero arsenic exposure in a U.S. Cohort. Environ. Health Perspect. 124, 840–847 (2016).
Gilbert-Diamond, D., Emond, J. A., Baker, E. R., Korrick, S. A. & Karagas, M. R. Relation between in utero arsenic exposure and birth outcomes in a cohort of mothers and their newborns from New Hampshire. Environ. Health Perspect. 124, 1299–1307 (2016).
Rojas, D. et al. Prenatal arsenic exposure and the epigenome: identifying sites of 5-methylcytosine alterations that predict functional changes in gene expression in newborn cord blood and subsequent birth outcomes. Toxicol. Sci. 143, 97–106 (2015).
Bailey, K. & Fry, R. C. Long-term health consequences of prenatal arsenic exposure: links to the genome and the epigenome. Rev. Environ. Health 29, 9–12 (2014).
Blount, B. C., Valentin-Blasini, L., Osterloh, J. D., Mauldin, J. P. & Pirkle, J. L. Perchlorate exposure of the US Population, 2001–2002. J. Expo. Sci. Environ. Epidemiol. 17, 400–407 (2007).
Perchlorate in Drinking Water Proposed Rule. https://www.epa.gov/dwstandardsregulations/perchlorate-drinking-water (2019).
Maffini, M. V., Trasande, L. & Neltner, T. G. Perchlorate and diet: human exposures, risks, and mitigation strategies. Curr. Environ. Health Rep. 3, 107–117 (2016).
Murray, C. W., Egan, S. K., Kim, H., Beru, N. & Bolger, P. M. US Food and Drug Administration’s Total Diet Study: dietary intake of perchlorate and iodine. J. Expo. Sci. Environ. Epidemiol. 18, 571–580 (2008).
United States Environmental Protection Agency. ACE Biomonitoring https://www.epa.gov/ace/ace-biomonitoring (2017).
Wolff, J. Perchlorate and the thyroid gland. Pharmacol. Rev. 50, 89–105 (1998).
Blount, B. C., Pirkle, J. L., Osterloh, J. D., Valentin-Blasini, L. & Caldwell, K. L. Urinary perchlorate and thyroid hormone levels in adolescent and adult men and women living in the United States. Environ. Health Perspect. 114, 1865–1871 (2006).
Trasande, L., Shaffer, R. M. & Sathyanarayana, S. Food additives and child health. Pediatrics 142, e20181408 (2018).
Taylor, P. N. et al. Maternal perchlorate levels in women with borderline thyroid function during pregnancy and the cognitive development of their offspring: data from the Controlled Antenatal Thyroid Study. J. Clin. Endocrinol. Metab. 99, 4291–4298 (2014).
Environmental Protection Agency. Environments and Contaminants: Drinking Water Contaminants—Report Contents (2017).
Council on Environmental Health. Iodine deficiency, pollutant chemicals, and the thyroid: new information on an old problem. Pediatrics 133, 1163–1166 (2014).
Ward, M. H. et al. Drinking water nitrate and human health: an updated review. Int. J. Environ. Res. Public Health 15, 1557 (2018).
Ward, M. H. et al. Workgroup Report: drinking water nitrate and health—recent findings and research needs. Environ. Health Perspect. 113, 1607–1614 (2005).
Rogan, W. Council on Environmental Health. Iodine deficiency, pollutant chemicals, and the thyroid: new information on an old problem. Pediatrics 133, 1163 (2014).
IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Ingested nitrate and nitrite, and cyanobacterial peptide toxins. IARC Monogr. Eval. Carcinog. Risks Hum. 94, v–vii, 1–412 (2010).
Gupta, P. M., Hamner, H. C., Suchdev, P. S., Flores-Ayala, R. & Mei, Z. Iron status of toddlers, nonpregnant females, and pregnant females in the United States. Am. J. Clin. Nutr. 106, 1640S–1646SS (2017).
Bithoney, W. G. Elevated lead levels in children with nonorganic failure to thrive. Pediatrics 78, 891 (1986).
Kwong, W. T., Friello, P. & Semba, R. D. Interactions between iron deficiency and lead poisoning: epidemiology and pathogenesis. Sci. Total Environ. 330, 21–37 (2004).
Mack, E. A. & Wrase, S. A burgeoning crisis? A nationwide assessment of the geography of water affordability in the United States. PLoS ONE 12, e0169488 (2017).
Hanna-Attisha, M., LaChance, J., Sadler, R. C. & Champney Schnepp, A. Elevated blood lead levels in children associated with the flint drinking water crisis: a spatial analysis of risk and public health response. Am. J. Public Health 106, 283–290 (2016).
McOliver, C. A. et al. Community-based research as a mechanism to reduce environmental health disparities in american Indian and Alaska native communities. Int. J. Environ. Res. Public Health 12, 4076–4100 (2015).
White, B. M., Bonilha, H. S. & Ellis, C. Racial/ethnic differences in childhood blood lead levels among children <72 months of age in the United States: a systematic review of the literature. J. Racial Ethn. Health Disparities 3, 145–153 (2016).
Shapiro, E. More than 1,100 School Faucets Still Have Lead, City Says. The New York Times (2018).
Leyden, L. In Echo of Flint, Mich., Water Crisis Now Hits Newark. The New York Times (2018).
Balazs, C., Morello-Frosch, R., Hubbard, A. & Ray, I. Social disparities in nitrate-contaminated drinking water in California’s San Joaquin Valley. Environ. Health Perspect. 119, 1272–1278 (2011).
Esquinca, M., Jamarillo, A. News21. “Colonias” on US Border Struggle with Decades-Old Water Issues, Including Contamination. Desert Sun https://www.texastribune.org/2017/08/22/colonias-border-struggle-decades-old-water-issues/ (2017).
United States Environmental Protection Agency. Administrative order for RD/RA for the Area 4 Puente Valley Operable Unit. https://www.epa.gov/sites/production/files/2013-08/documents/puentevalley-order.pdf (2011).
Asian Americans Advancing Justice. A community of contrasts: Asian Americans, Native Hawaiians and Pacific Islanders in the San Gabriel Valley. https://www.advancingjustice-la.org/sites/default/files/A_Community_of_Contrasts_SGV_2018.pdf (2018).
Scauzillo, S. Progress Report: After 25 years of Cleaning Contaminated Water in San Gabriel Valley, Here’s How It’s Coming Along. San Gabriel Valley Tribune https://www.sgvtribune.com/2018/03/10/progress-report-25-years-cleaning-contaminated-water-in-san-gabriel-valley-heres-how-its-coming-along/ (2018).
Dillon, L. et al. The Environmental Protection Agency in the early Trump administration: prelude to regulatory capture. Am. J. Public Health 108, S89–S94 (2018).
Trump, D. Restoring the Rule of Law, Federalism, and Economic Growth by Review the “Waters of the United States” Rule. Executive Order 13778 (2017).
Kaufman, A. EPA Moves to Replace Obama-Era Rule for Protecting Drinking Water for 117 Million. Huffington Post (2018).
Brady, D. EPA under Trump Shrinks to Near Regan-Era Staffing Levels. Washington Post (2017).
Landrigan, P. J. & Goldman, L. R. Bad Move that Could End Up Exposing Kids to Chemicals. New York Times (2017).
US Environmental Protection Agency. EPA Administrator Pruitt Proposes Rule to Strengthen Science Used in EPA Regulations (Office of the Administrator, 2018).
Rest, K. & Benjamin, G. Trump’s EPA Puts Our Health at Risk. Scientific American (2017).
Berg, J., Campbell, P., Kiermer, V., Raikhel, N. & Sweet, D. Joint statement on EPA proposed rule and public availability of data. Science (New York, NY) 360, eaau0116 (2018).
US Environmental Protection Agency. Lead; Identification of Dangerous Levels of Lead; Final Rule. 1-5-01, Federal Register (66 FR 1206, January 5, 2001) (FRL-6763-5) (2001).
Council on Environmental Health. Prevention of childhood lead toxicity. Pediatrics 138, e20161493 (2016).
Lanphear, B. P. et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ. Health Perspect. 113, 894–899 (2005).
Guidelines for Canadian Drinking Water Quality: Guideline Technical Document—Lead. https://www.canada.ca/en/health-canada/services/publications/healthy-living/guidelines-canadian-drinking-water-quality-guideline-technical-document-lead.html (2019).
Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Environmental Health, Registry AfTSaD. Meeting of the Lead Poisoning Prevention Subcommittee of the NCEH/ATDSR Board of Scientific Counselors (2016).
Wang, L., Liu, Z., Zhang, J., Wu, Y. & Sun, H. Chlorpyrifos exposure in farmers and urban adults: Metabolic characteristic, exposure estimation, and potential effect of oxidative damage. Environ. Res. 149, 164–170 (2016).
Lynn, S. Minutes of the April 19–21. In 2016 FIFRA SAP Meeting Held to Consider and Review Scientific Issues Associated with “Chlorpyrifos: Analaysis of Biomonitoring Data” (2016).
US Environmental Protection Agency. Chlorpyrifos; Order Denying PANNA and NRDCs Petition to Revoke Tolerances (2017).
Snider, A. What Broke the Safe Drinking Water Act? Politico Agenda (2017).
Erickson, B. E. Court orders EPA to ban chlorpyrifos. C&EN 94, p. 19 (2016).
Centner, T. J. Cancelling pesticide registrations and revoking tolerances: the case of chlorpyrifos. Environ. Toxicol. Pharmacol. 57, 53–61 (2018).
Udall. Protect Children, Farmers, and Farmworkers from Nerve Agent Pesticides Act of 2019 (2019).
National Research Defense Council. A New Bill Proposes to Ban Chlorpyrifos Nationwide (2019).
Mandatory Pesticide Disclosure; Pesticide Reporting and Regulation Program; Chlorpyrifos; Pesticide Use Revolving Fund; Pesticide Drift Monitoring Study; Appropriation. https://www.capitol.hawaii.gov/Archives/measure_indiv_Archives.aspx?billtype=SB&billnumber=3095&year=2018 (2018).
DeLauro, R. To establish limitations on the quantity of inorganic arsenic in rice and rice products under Chapter IV of the Federal Food, Drug and Cosmetic Act. H.R. 4535 (2017).
Nigra, A. E. et al. The effect of the Environmental Protection Agency maximum contaminant level on arsenic exposure in the USA from 2003 to 2014: an analysis of the National Health and Nutrition Examination Survey (NHANES). Lancet Public health 2, e513–e521 (2017).
Agency for Toxic Substances and Disease Registry. Public Health Statement for Perchlorates (2008).
Pallone, F. J. Safe Drinking Water Act Amendments of 2017. Press Release (2017).
Allen, D. T. & Roberts, S. M. Scientific Advisory Board Advice on Approaches to Derive a Maximum Contaminant Level Goal for Perchlorate (US Environmental Protection Agency, 2013).
Regulated Drinking Water Contaminants: Inorganic Chemicals. https://www.epa.gov/sites/production/files/2015-10/documents/ace3_drinking_water.pdf (2015).
Pennino, M. J., Compton, J. E. & Leibowitz, S. G. Trends in drinking water nitrate violations across the United States. Environ. Sci. Technol. 51, 13450–60 (2017).
Maupin, M. A. et al. Estimated Use of Water in the United States in 2010. U.S. Geological Survey Circular 1405, 56pp (US Geological Survey, Reston, 2014).
Stoner, N. Working in Partnership with States to Address Phosphorus and Nitrogen Pollution through Use of a Framework for State Nutrient Reductions (Environmental Protection Agency Office of Water Memo, 2011).
Beauvais, J. Renewed Call to Action to Reduce Nutrient Pollution and Support for Incremental Actions to Protect Water Quality and Public Health (Environmental Protection Agency Office of Water Memo, 2016).
United States Environmental Protection Agency. Fact Sheet. PFOA & PFOS Drinking Water Health Advisories https://www.epa.gov/sites/production/files/2016-06/documents/drinkingwaterhealthadvisories_pfoa_pfos_updated_5.31.16.pdf.2016 (2016).
National Research Council. The Gulf Research Program. A Strategic Vision (The National Academies Press, 2014).
Javier, J. R., Brumberg, H. L., Sanders, L., Hannon, T. S. & Shah, S. How gaps in policy implementation cause public health malpractice. Lancet (Lond., Engl.) 391, 2414 (2018).
Prevent Children’s Exposure to Lead. https://www.cdc.gov/features/leadpoisoning/index.html (2017).
US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Environmental Health, Agency for Toxic Substances and Disease Registry. Meeting of the Lead Poisoning Prevention Subcommittee of the NCEH/ATSDR Board of Scientific Counselors https://www.atsdr.cdc.gov/science/lpp/docs/lead_subcommittee_minutes_9_19_2016_508.pdf (2016).
Protect Children, Farmers, and Farmworkers from Nerve Agent Pesticides Act of 2019. https://www.congress.gov/bill/116th-congress/senate-bill/921/text (2019).
Agency for Toxic Substances and Disease Registry. Public Health Statement: Arsenic, CAS#: 7440-38-2 (Division of Toxicology and Environmental Medicine, 2007).
Rogan, W. J. & Brady, M. T. Drinking water from private wells and risks to children. Pediatrics 123, 1599–605 (2009).
Ground Water and Drinking Water. https://safewater.zendesk.com/hc/en-us (2018).
PEHSU. https://www.pehsu.net/ (2019).
Acknowledgements
Drs. Javier, Shah, and Brumberg are members of the Society for Pediatric Research Advocacy Committee, whose mission is to provide leadership in child advocacy through government and public forums for issues related to the mission of the Society. We recommend public and government priorities for advocacy, advocate for prioritized issues in partnership with other agencies and societies, and community effectively with Council and membership regarding advocacy committees. Our multidisciplinary team provides a unique lens for the development of this SPR Perspectives review.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions in analyzing data, drafting the manuscript, and providing critical revisions. All authors approve this final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bantol, K.E.A., Brumberg, H.L., Shah, S.I. et al. Perspectives from the Society for Pediatric Research: contaminants of water and children’s health: Can we do better?. Pediatr Res 88, 535–543 (2020). https://doi.org/10.1038/s41390-020-0985-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0985-4
This article is cited by
-
US drinking water quality: exposure risk profiles for seven legacy and emerging contaminants
Journal of Exposure Science & Environmental Epidemiology (2024)
-
Before the first breath: why ambient air pollution and climate change should matter to neonatal-perinatal providers
Journal of Perinatology (2023)
-
Boil water alerts and their impact on the unexcused absence rate in public schools in Jackson, Mississippi
Nature Water (2023)
-
We can and we must do better to protect children from drinking water contaminants
Pediatric Research (2020)