Abstract
Background
Studies in adults showed a relationship between low hemoglobin (Hb) and acute kidney injury (AKI). We performed this study to evaluate this association in newborns.
Methods
We evaluated 1891 newborns from the Assessment of Worldwide AKI Epidemiology in Neonates (AWAKEN) database. We evaluated the associations for the entire cohort and 3 gestational age (GA) groups: <29, 29–<36, and ≥36 weeks’ GA.
Results
Minimum Hb in the first postnatal week was significantly lower in neonates with AKI after the first postnatal week (late AKI). After controlling for multiple potential confounders, compared to neonates with a minimum Hb ≥17.0 g/dL, both those with minimum Hb ≤12.6 and 12.7–14.8 g/dL had an adjusted increased odds of late AKI (aOR 3.16, 95% CI 1.44–6.96, p = 0.04) and (aOR 2.03, 95% CI 1.05–3.93; p = 0.04), respectively. This association was no longer evident after controlling for fluid balance. The ability of minimum Hb to predict late AKI was moderate (c-statistic 0.68, 95% CI 0.64–0.72) with a sensitivity of 65.9%, a specificity of 69.7%, and a PPV of 20.8%.
Conclusions
Lower Hb in the first postnatal week was associated with late AKI, though the association no longer remained after fluid balance was included.
Impact
-
The current study suggests a possible novel association between low serum hemoglobin (Hb) and neonatal acute kidney injury (AKI).
-
The study shows that low serum Hb levels in the first postnatal week are associated with increased risk of AKI after the first postnatal week.
-
This study is the first to show this relationship in neonates.
-
Because this study is retrospective, our observations cannot be considered proof of a causative role but do raise important questions and deserve further investigation. Whether the correction of low Hb levels might confer short- and/or long-term renal benefits in neonates was beyond the scope of this study.
Similar content being viewed by others
Introduction
Neonatal acute kidney injury (AKI) used to be an under-recognized morbidity among neonates. Single-center studies1,2,3 and reports from a recent multicenter study, Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN), suggest that AKI occurs in up to 30% of critically ill neonates admitted to the neonatal intensive care unit (NICU) who receive intravenous (IV) fluids for at least 48 h. Neonates with AKI have 4.6 times higher independent odds of mortality.4 Risk factors associated with neonatal AKI have been reported in single-center studies1,2,5,6,7,8 and in the multicenter AWAKEN study.4 To the best of our knowledge, the relationship between hemoglobin (Hb) levels and neonatal AKI has not been explored. Understanding whether lower Hb levels are associated with neonatal AKI is important as this could be a modifiable risk factor to prevent or mitigate AKI.
Anemia was found to be associated with increased mortality and morbidity in neonates. Banerjee and colleagues9 reported that neonates with Hb levels <12 g/dL at birth were more likely to have intraventricular hemorrhage, necrotizing enterocolitis (NEC), bronchopulmonary dysplasia, retinopathy of prematurity, and death. Using the American College of Surgeons National Surgical Quality Improvement Program Databases, Goobie et al. showed that preoperative anemia was an independent risk factor for mortality in children undergoing non-cardiac surgeries (odds ratio (OR): 2.62; 95% confidence interval (CI): 1.51–4.57).10 A preoperative hematocrit level <40% was the optimal cutoff point to predict overall mortality.
Although the relationship of anemia and AKI has not been explored in neonatal or pediatric patients, a few studies have examined this association in adults.11,12,13,14,15 For example, Han et al.15 found a longer AKI duration in patients admitted to the intensive care unit (ICU) with low Hb levels. De Santo et al. reported that preoperative anemia is independently associated with AKI after coronary artery bypass grafting,16 and Shema-Didi et al. demonstrated a similar relationship between anemia at hospital admission and AKI during hospital stay in patients aged ≥17 years.17
To improve our understanding of the association between Hb levels and neonatal AKI, we analyzed the AWAKEN database. Our primary aim was to determine whether the minimum Hb levels measured during the first postnatal week of life were independently associated with early and/or late neonatal AKI. Our secondary aim was to investigate whether the maximum Hb levels measured during the first postnatal week were associated with a lower risk of early and/or late neonatal AKI.
Methods and statistical analysis
Study population
Our study utilized data from the AWAKEN database. The methodology for data collection has been previously published.18 The AWAKEN cohort included 2162 neonates admitted to the NICU at 24 institutions from 4 different countries from January 1, 2014 to March 31, 2014. Inclusion criteria included admission during the study period and receiving at least 48 h. of IV fluids as the primary source of hydration or nutrition. The inclusion criteria were designed to capture sick neonates at significant risk for AKI and those who had an expected hospitalization of at least 48 h. The AWAKEN group did not include those who were admitted for diagnoses such as transient tachypnea of the newborn and transient hypoglycemia or those who simply needed ultraviolet light for hyperbilirubinemia as the group felt these patients would have less risk of AKI and that serum creatinine (SCr) measurements would be rare in these neonates. Newborns receiving routine care in the newborn nursery were also excluded from this study for the same reason. In addition, the exclusion criteria for AWAKEN included admission >2 weeks of age, congenital heart disease (repaired at <7 days of age), lethal anomaly, and death within 48 h. For this analysis, we excluded infants who did not have at least one Hb level documented during the first postnatal week and infants who did not have at least two SCr measurements or at least 1 day of urine output (UOP) quantification during NICU stay (Fig. 1).
The University of Alabama at Birmingham Institutional Review Board (IRB) approved this collaborative study, and each center received approval from their respective IRB or Human Research Ethics Committee. The study was registered at ClinicalTrials.gov (NCT02443389).
Data collection
The data collected for the AWAKEN study included five components: baseline demographics, daily information for the first postnatal week, weekly snapshots for the remaining hospitalization, and discharge data (discharge or death at 120 days of age).18 Day of birth was defined as postnatal day 1. The highest and lowest Hb levels in the medical records for each day were recorded for each neonate.
Hb levels as the main exposure
For neonates who had only hematocrit values entered in the medical record, the Hb level was calculated by dividing the hematocrit value by three. The minimal and maximum Hb levels during the first postnatal week were calculated for each neonate. The primary exposure was minimum Hb levels during the first postnatal week. The secondary exposure was maximum Hb levels during the same time frame. For both measures of Hb levels, only measures prior to the occurrence of AKI were considered. To determine whether the association between Hb levels and AKI is non-linear, we also categorized the primary exposure of minimum Hb based on quartiles with categories of ≤12.6, 12.7–14.8, 14.9–16.9, and ≥17.0 g/dL.
Outcomes/definition of neonatal AKI
The primary outcome was neonatal AKI during the first postnatal week (i.e., early AKI) and after the seventh postnatal day (i.e., late AKI). These timepoints were chosen to be consistent with previous risk factors analysis of early AKI19 and late AKI20 from the AWAKEN study. Only neonates who were alive after day 7 and did not have early AKI were considered for late AKI analysis. Early AKI was defined using the modified neonatal Kidney Disease Improving Global Outcomes (KDIGO) by either SCr or UOP; late AKI was defined using only the SCr-based definition. Based on these criteria, AKI was defined as UOP <1 ml/Kg/h over a 24-h period and/or SCr rise ≥0.3 mg/dL or 50% from the previous trough (Table 1). The secondary outcome of interest was the severity of AKI, defined as stage II and III using the KDIGO staging (Table 1). This definition was chosen based on the consensus recommendation made after the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases workshop.21 Baseline SCr was the lowest prior measured value as we have done in other AWAKEN studies.
Fluid balance (FB) is known to impact Hb levels.22 Therefore, the percentage of FB was determined using the following formula23,24,25:
Statistical analysis
Differences between maternal and neonatal characteristics were compared among the no AKI and early and late AKI groups using the chi-square test for categorical variables and the analysis of variance for continuous variables. In addition, the cohort was analyzed as a whole and stratified into 3 gestational age (GA) subgroups: (1) <29 weeks (n = 259), (2) ≥29–<36 weeks (n = 864) and (3) ≥36 weeks (n = 768). This stratification was consistent with those utilized across the AWAKEN studies.4 The minimum and maximum Hb levels across different AKI stages were compared within the whole cohort and the three subgroups were stratified by GA using a general estimating equation (GEE) regression model (to account for possible clustering by study site) with an identity link and normal distribution.
GEE logistic regression models were utilized to determine the independent association between minimum Hb values during the first postnatal week and late AKI. The logistic regression models were built with a stepwise selection procedure with a significance level of 0.2 for a variable to be included in the model and a significance level of 0.05 to remain in the model.
In secondary analysis, these models were run on a subsample of subjects who had FB data (n = 963 out of 1229 in the late AKI analysis). We developed a separate GEE regression model that included FB in those who had FB data.
To determine the threshold of minimum Hb that best predicts late AKI (both overall and specifically stage II/III), we performed receiver operating characteristic analysis, utilizing the Hb value at which the Youden index26 was maximized to select the threshold. Screening diagnostic measures including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratio positive (LR+) were calculated for each analysis. All statistical analyses were performed using SAS version 9.4 (SAS, Cary, NC).
Results
Patient characteristics
The AWAKEN study screened 4273 neonates, of whom 2162 met the inclusion criteria. A total of 1793 neonates were excluded because they did not receive IV fluids, 278 were admitted at >14 days of life, 68 had cardiac surgery <7 days, 60 were not admitted to the NICU, 45 died <48 h, and 25 had lethal congenital anomalies. Subjects may have been excluded for more than one reason and may be counted more than once in the “not enrolled” numbers.18 For this study, we excluded an additional 159 infants who did not have at least one Hb level documented during the first postnatal week and 140 infants who did not have at least 2 SCr measures or at least 1 day of UOP quantification during the first week. The final sample size for this analysis was 1891 neonates (Fig. 1). Of the 1891 neonates enrolled in the study, 259 were <29 weeks’ GA, 864 were 29–<36 weeks’ GA and 768 were ≥36 weeks’ GA.
Incidence of AKI
AKI occurred in 551/1891 (29%) neonates. The percentage of neonates with early or late AKI was 47.5% (n = 123), 18% (n = 155), and 35.5% (n = 273) among those <29 weeks, ≥29–<36 weeks, and ≥36 weeks, respectively. Of the 551 neonates with AKI, 299 neonates (54.3%) were diagnosed with AKI based on SCr criteria, 196 (35.6%) were diagnosed based on UOP criteria, and 56 (10.2%) were diagnosed based on both criteria.
Early AKI occurred in 419/1891 (22%) of the entire cohort. The incidence of early AKI for the <29 weeks’ GA group was 27.8% (n = 72), 13.9% (n = 120) for the ≥29–<36 weeks’ GA group, and 29.6% (n = 227) among the ≥36 weeks’ GA group. Late AKI occurred in 132/1891 (7.0%) for the entire cohort. By GA, the incidence of late AKI was 19.7% (n = 51) among those <29 weeks’ GA, 4% (n = 35) in ≥29–<36 weeks, and 6% (n = 46) for the ≥36 weeks’ GA group.
Demographic differences by AKI status
Demographic differences between the no AKI and early and late AKI groups are shown in Table 2. GA, birth weight, sex, outborn status, mode of delivery, resuscitation following delivery (intubation, chest compression, epinephrine, and normal saline), sepsis evaluation, hypoxic ischemic encephalopathy, seizures, hypoglycemia, hyperbilirubinemia, metabolic evaluation, congenital heart disease, NEC, admission for surgical evaluation, amniotic fluid volume, maternal hypertension, maternal hemorrhage, multiple gestation, assisted conception, maternal steroids, antihypertension medication intake, meconium aspiration, and vaginal bleeding were significantly different (p < 0.05) between the three groups. In addition, for GA and birth weight, all pairwise comparisons were significant.
Time of lowest Hb levels and AKI diagnosis
The median day of early AKI diagnosis was postnatal day 2 (interquartile range (IQR) 1–4) and postnatal day 16 (IQR 11–27) for late AKI diagnosis. Among the early AKI group, the median day of lowest Hb was postnatal day 1 (IQR 1–2). For neonates who developed late AKI, the lowest Hb in the first postnatal week was recorded on postnatal day 4 (IQR 2–5). Finally, the lowest Hb level was recorded on postnatal day 2 (IQR 1–4) for the no AKI group (p < 0.0001). The median duration between the lowest Hb level and the diagnosis of early AKI was 1 day (IQR 0–2) and was 12 days (IQR 7–23) for late AKI.
Minimum and maximum Hb levels and AKI
Daily mean Hb levels were consistently lower in both the early and late AKI groups compared to the no AKI group (Fig. 2). However, the observed differences were significant for late AKI only. Specifically, mean minimum Hb levels were not significantly lower in those with early AKI (14.9 ± 3.4, p = 0.7) compared to those with no AKI (15.1 ± 3.0). However, Hb levels were significantly lower among those with late AKI (12.7 ± 3.0, p < 0.0001) than among those with no AKI (p < 0.0001) and early AKI (p < 0.0001). Conversely, maximum Hb levels were significantly lower in the early (15.5 ± 3.3, p < 0.05) and late AKI (15.1 ± 2.9, p < 0.003) groups than in the no AKI group (16.1 ± 2.7). There was no difference in maximum Hb levels between the early and late AKI groups (p = 0.55).
Hb levels and AKI stages
For early AKI, the mean minimum Hb levels were not significantly lower in AKI stage I and stage II/III compared to those without AKI among the whole cohort and in all the subgroups (Table 3). The mean maximum Hb levels were not significantly lower in the AKI stage I and stage II/III groups compared to the no AKI group for the whole cohort and GA subgroups except for the <29 weeks’ GA group in which the mean maximum Hb levels were lower in stage I AKI (12.9 ± 3.0, p = 0.004) compared to the no AKI group (14.3 ± 2.4).
In contrast, among the whole cohort, the mean minimum Hb levels were significantly lower in late AKI stage I (12.9 ± 3.1, p = 0.003) and stage II/III (12.5 ± 3.0, p < 0.0001) when compared to those without AKI who were in the hospital after the seventh postnatal day (14.9 ± 3.1). In the stratified analysis by GA groups, we found a significant difference only between those with and without AKI in the 29–<36 weeks’ GA group for stage I (13.2 ± 3.3, p = 0.02) and stage II/III AKI (12.1 ± 2.8, p = 0.0005). Though maximum Hb levels were higher in the no AKI group vs. stage II/III within the whole cohort (16.1 ± 2.8 vs. 14.7 ± 3.0, p < 0.0001), we did not find significant differences in the stratified GA group analysis. We did not observe a significant difference between the minimum and maximum Hb levels between stage I and stage II/III combined in the whole cohort or any of the subgroups for both early and late AKI.
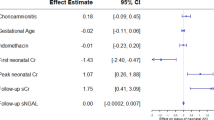
Association between Hb levels and late AKI
Based on logistic regression analysis, for every 1 g/dL decrease in minimum Hb levels, there was 26% increased crude odds of late AKI (OR: 1.26, 95% CI 1.17–1.36; Table 4). This association remained after adjusting for potential confounders, including GA, intubation, and amniotic fluid volume (OR 1.15, 95% CI 1.04–1.26; p = 0.005). When examining Hb levels by quartiles, compared to the highest quartile (i.e., ≥17.0 g/dL), the observed increased adjusted association was significant for neonates with minimum Hb levels ≤12.6 g/dL (OR 3.16, 95% CI 1.44–6.96, p = 0.04) and 12.7–14.8 g/dL (OR 2.03, 95% CI 1.05–3.93; p = 0.04). Total of 148 neonates had FB data. In secondary analyses limiting the analytical population to neonates with FB data [n = 963, after excluding the newborns with early AKI (n = 268) and the newborns discharged prior to the seventh postnatal day (n = 197))] and adjusting for FB (in addition to the prior adjusted factors), no association was observed between minimum Hb levels and late AKI.
Receiver operating characteristic analysis
For late AKI, a minimum Hb level of 13.4 g/dL best predicted AKI with an area under the curve of 0.68. Nevertheless, sensitivity and PPV were low (65.9% and 20.8%, respectively) at this threshold (Table 5). The threshold was similar for stage II/III AKI, though the PPV was much lower (11.8%). By GA, the Hb threshold was lowest for neonates with a GA <29 weeks. Notably, for any AKI stage, the Hb threshold was 11.7 g/dL; for stage II/III AKI, the threshold was 11.3 g/dL. A similar pattern for screening diagnostics was observed with low PPV and high NPV. Hb levels were most predictive for late AKI in neonates with a GA of 29–<36 weeks as evidenced by an LR+ of 2.6 for any stage AKI and 2.7 for stage II/III AKI. However, the PPV was very low for this cohort. The thresholds and diagnostics for GA ≥36 weeks were similar to those for the whole cohort.
Discussion
To our best knowledge, this study is the first to examine the relationship between Hb levels and neonatal AKI. Using this multicenter retrospective AWAKEN cohort, we report that neonates with lower minimum Hb levels in the first postnatal week had higher independent odds of late AKI after controlling for confounders. Although this association remained even after controlling for numerous confounders, we were no longer able to see this independent association once we corrected for FB. We were unable to demonstrate an association between Hb levels with the severity of AKI. We also report that maximum Hb levels were significantly lower in the early and late AKI groups compared to the no AKI group.
AKI is associated with significant morbidity and mortality in critically ill neonates.2,27,28 Improving our understanding of the risk factors that lead to AKI may help develop strategies for prevention and early detection of AKI. Anemia and AKI are both important factors that predict morbidity and mortality,10,27,28 and further understanding of their relationships is needed.
Studies in adults in different clinical settings have shown an association between Hb levels and AKI.13,15,29 Henn et al. showed higher odds of AKI in adults admitted to the ICU with Hb <10.5 g/dL compared to those who presented with higher Hb levels.15 Others have demonstrated a significant association between preoperative Hb and/or postoperative Hb drop with the development of AKI in adults who undergo cardiac procedures.13,14,21,30 A similar relationship was reported in patients undergoing other non-cardiac interventions.12,31
Although the exact mechanisms linking lower Hb levels to AKI remain unclear, several feasible explanations for this link have been suggested. As we showed that controlling for FB removes the association we documented, it is possible that lower Hb values are simply a reflection of a dilutional effect on the blood. Lower Hb levels can directly reduce the delivery of oxygen to the kidneys with subsequent development of a hypoxic environment and development of AKI. Segment S3 of the proximal tubule is extremely sensitive to changes in oxygen delivery,32 which suggests that hypoxia-related anemia would increase the severity of renal tubular cell damage and thus contribute to kidney impairment.33 Because AKI frequently develops in the setting of ischemic conditions, low Hb may be a mitigating risk factor of AKI during hospitalization.34 The effect of low Hb on the kidney may be exacerbated in neonates due to the presence of fetal Hb (HbF). At term, HbF comprises 70–80% of total Hb; this increases to 90% of total Hb in preterm babies. The high oxygen affinity of HbF is detrimental as oxygen is not readily given up to the tissues. The HbF oxygen dissociation curve moves to the left after delivery due to increased pH and lower carbon dioxide concentration, further limiting oxygen delivery to the periphery.35 Another possible explanation is that low Hb may represent hemolysis due to ABO incompatibility or bleeding (subclinical or overt), which may cause direct tubular injury and/or reduced renal perfusion pressures.36,37 Low Hb may also result from other illnesses like sepsis and/or extensive surgeries that result in greater systemic inflammation that may compound the risk of AKI. A few studies have suggested that blood transfusion in anemic patients is another possible mechanism of AKI development in the setting of anemia.38,39 Transfused red cells may be unable to properly load and unload oxygen, have a shortened lifespan, and can result in higher levels of circulating catalytic iron, which may, in theory, lead to AKI.40 Importantly, the hypothesized harmful effect of blood transfusion on AKI was opposed by another study41 in which blood transfusion significantly improved renal function in endotoxemic rats. Those authors speculated that the specific beneficial effect of blood transfusion on the kidney could have been mediated in part by improvements in renal microvascular oxygenation and sepsis-induced endothelial dysfunction via the restoration of endothelium-derived nitric oxide synthase expression within the kidney. Unfortunately, the AWAKEN database does not contain sufficient data for uncovering these possible mechanisms to explain why patients with lower Hb are more likely to have AKI. Specifically, the database does not contain information on blood transfusions, delayed cord clamping, cord milking, iron levels, presence of ABO incompatibility, or the use of erythropoietin-stimulating agents.
A major strength of this study is the large number of enrolled subjects that spanned the GA spectrum and the variety of centers involved in the study. Our findings were present in the whole cohort, and similar findings were evident in each of the three GA subgroups. Our sample size allowed us to control for potential confounders such that we were able to show an independent association between low Hb levels and AKI. Despite these strengths, we acknowledge limitations inherent to retrospective chart review studies, including the reliance on retrospectively collected data (Hb levels, SCr, and UOP). There is the possibility of unrecognized or unmeasured confounders affecting the outcome. Another limitation is the lack of available information that could allow us to better decipher the mechanism(s) that may lead to kidney injury. Finally, the inclusion criteria for the AWAKEN cohort including receiving at least 48 h of IV fluids were designed to capture sick neonates at significant risk for AKI and those who had an expected hospitalization of at least 48 h. As a result, it is possible that the results of our study may not be generalizable to all neonates admitted to the NICU and instead applicable only to those who met the eligibility criteria for the AWAKEN cohort. In addition, the exclusion of these neonates could have biased the currently reported associations. However, the direction of the bias is difficult to ascertain as only data on sex, race, and ethnicity were collected for the excluded neonates. That said, of the possible scenarios, the most likely scenario is one in which the excluded, who are likely less sick than the neonates included in the AWAKEN cohort, are more likely to have higher Hb levels and lower AKI risk. As a result, the currently reported estimates are biased toward the null hypothesis and underestimate the true association as our observed Hb levels among those without AKI are, overall, lower than those had all neonates been included. As a final limitation, whether the correction of low Hb levels might confer long-term renal benefits in neonates was beyond the scope of this study.
Conclusion/future directions
In this retrospective multicenter study, we describe a novel association between lower Hb levels and neonatal AKI after the first postnatal week, which remained after controlling for multiple confounders. This independent association was no longer evident when we controlled for FB. As Hb could be a modifiable factor to prevent AKI, future studies that evaluate whether and how interventions to treat low Hb (e.g., blood transfusions, delaying cord clamping and/or milking of the umbilical cord, and erythropoietin) protect the kidney in term and preterm babies are warranted.
References
Bolat, F. et al. Acute kidney injury in a single neonatal intensive care unit in Turkey. World J. Pediatr. 9, 323–329 (2013).
Koralkar, R. et al. Acute kidney injury reduces survival in very low birth weight infants. Pediatr. Res. 69, 354–358 (2011).
Kaur, S. et al. Evaluation of glomerular and tubular renal function in neonates with birth asphyxia. Ann. Trop. Paediatr. 31, 129–134 (2011).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc. Health 1, 184–94 (2017).
Askenazi, D. J. et al. Fluid overload and mortality are associated with acute kidney injury in sick near-term/term neonate. Pediatr. Nephrol. 28, 661–666 (2013).
Cataldi, L. et al. Potential risk factors for the development of acute renal failure in preterm newborn infants: a case-control study. Arch. Dis. Child. Fetal Neonatal Ed. 90, F514–F519 (2005).
Cuzzolin, L. et al. Postnatal renal function in preterm newborns: a role of diseases, drugs and therapeutic interventions. Pediatr. Nephrol. 21, 931–938 (2006).
Selewski, D. T. et al. Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J. Pediatr. 162, 725–729 e1 (2013).
Banerjee, J. et al. Haemoglobin level at birth is associated with short term outcomes and mortality in preterm infants. BMC Med. 13, 16 (2015).
Goobie, S. M., Faraoni, D., Zurakowski, D. & DiNardo, J. A. Association of preoperative anemia with postoperative mortality in neonates. JAMA Pediatr. 170, 855–862 (2016).
Shacham, Y. et al. Association of admission hemoglobin levels and acute kidney injury among myocardial infarction patients treated with primary percutaneous intervention. Can. J. Cardiol. 31, 50–55 (2015).
Walsh, M. et al. The association between perioperative hemoglobin and acute kidney injury in patients having noncardiac surgery. Anesth. Analg. 117, 924–931 (2013).
Karkouti, K. et al. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation 119, 495–502 (2009).
Morabito, S. et al. Incidence of contrast-induced acute kidney injury associated with diagnostic or interventional coronary angiography. J. Nephrol. 25, 1098–1107 (2012).
Han, S. S. et al. Anemia is a risk factor for acute kidney injury and long-term mortality in critically ill patients. Tohoku J. Exp. Med. 237, 287–295 (2015).
De Santo, L. et al. Preoperative anemia in patients undergoing coronary artery bypass grafting predicts acute kidney injury. J. Thorac. Cardiovasc Surg. 138, 965–970 (2009).
Shema-Didi, L., Ore, L., Geron, R. & Kristal, B. Is anemia at hospital admission associated with in-hospital acute kidney injury occurrence? Nephron Clin. Pract. 115, c168–c176 (2010).
Jetton, J. G. et al. Assessment of worldwide acute kidney injury epidemiology in neonates: design of a retrospective cohort study. Front Pediatr. 4, 68 (2016).
Charlton, J. R. et al. Incidence and risk factors of early onset neonatal AKI. Clin. J. Am. Soc. Nephrol. 14, 184–95 (2019).
Charlton, J. R. et al. Late onset neonatal acute kidney injury: results from the AWAKEN Study. Pediatr. Res. 85, 339–48 (2019).
Zappitelli, M. et al. Developing a neonatal acute kidney injury research definition: a report from the NIDDK neonatal AKI workshop. Pediatr. Res. 82, 569–73 (2017).
Wolf, M. B. Hemoglobin-dilution method: effect of measurement errors on vascular volume estimation. Comput Math. Methods Med. 2017, 3420590 (2017).
Selewski, D. T. et al. Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med. 37, 1166–1173 (2011).
Selewski, D. T. et al. The impact of fluid balance on outcomes in critically ill near-term/term neonates: a report from the AWAKEN study group. Pediatr. Res. 85, 79–85 (2019).
Selewski, D. T. et al. The impact of fluid balance on outcomes in premature neonates: a report from the AWAKEN study group. Pediatr. Res. 87, 550–7 (2020).
Ruopp, M. D., Perkins, N. J., Whitcomb, B. W. & Schisterman, E. F. Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom. J. 50, 419–430 (2008).
Sarkar, S. et al. Relationship between acute kidney injury and brain MRI findings in asphyxiated newborns after therapeutic hypothermia. Pediatr. Res. 75, 431–435 (2014).
Askenazi, D. J. et al. Acute kidney injury is independently associated with mortality in very low birthweight infants: a matched case-control analysis. Pediatr. Nephrol. 24, 991–997 (2009).
Powell-Tuck, J. et al. Anaemia is not a risk factor for progression of acute kidney injury: a retrospective analysis. Crit. Care. 20, 52 (2016).
Gorla, R. et al. Impact of preoperative anemia and postoperative hemoglobin drop on the incidence of acute kidney injury and in-hospital mortality in patients with type B acute aortic syndromes undergoing thoracic endovascular aortic repair. Vasc. Endovasc. Surg. 51, 131–138 (2017).
Choi, Y. J., Kim, S. O., Sim, J. H. & Hahm, K. D. Postoperative anemia is associated with acute kidney injury in patients undergoing total hip replacement arthroplasty: a retrospective study. Anesth. Analg. 122, 1923–1928 (2016).
Brezis, M. & Rosen, S. Hypoxia of the renal medulla-its implications for disease. N. Engl. J. Med. 332, 647–655 (1995).
Abuelo, J. G. Normotensive ischemic acute renal failure. N. Engl. J. Med. 357, 797–805 (2007).
Susantitaphong, P. et al. World incidence of AKI: a meta-analysis. Clin. J. Am. Soc. Nephrol. 8, 1482–93 (2013).
Ford, S. C. J. Adaptation for life: a review of neonatal physiology. Anaesth. Intensive Care Med. 9, 93–98 (2008).
Karrowni, W. et al. Blood transfusion and the risk of acute kidney injury among patients with acute coronary syndrome undergoing percutaneous coronary intervention. Circ. Cardiovasc. Interv. 9, e003279 (2016).
Nuis, R. J. et al. Blood transfusion and the risk of acute kidney injury after transcatheter aortic valve implantation. Circ. Cardiovasc. Interv. 5, 680–688 (2012).
Haase, M. et al. Effect of mean arterial pressure, haemoglobin and blood transfusion during cardiopulmonary bypass on post-operative acute kidney injury. Nephrol. Dial. Transplant. 27, 153–160 (2012).
Kotal, R., Habib, Y., Karim, R. & Saikia, M. Influence of packed red cell transfusion on risk of acute kidney injury after cardiopulmonary bypass in anemic and non-anemic patients. Anaesth. Pain Intensive Care 20(Suppl), S42–S47 (2016).
de Vries, B. et al. Reduction of circulating redox-active iron by apotransferrin protects against renal ischemia-reperfusion injury. Transplantation 77, 669–675 (2004).
Zafrani, L., Ergin, B., Kapucu, A. & Ince, C. Blood transfusion improves renal oxygenation and renal function in sepsis-induced acute kidney injury in rats. Crit. Care 20, 406 (2016).
Acknowledgements
The authors thank the outstanding work of the following clinical research personnel and colleagues for their involvement in AWAKEN: Ariana Aimani, Samantha Kronish, Ana Palijan, MD, and Michael Pizzi from Montreal Children’s Hospital, McGill University Health Centre, Montreal, QC, Canada; Laila Ajour, BS, and Julia Wrona, BS, from University of Colorado, Children’s Hospital Colorado, Aurora, CO; Melissa Bowman, RN, University of Rochester, Rochester, NY; Teresa Cano, RN, Marta G. Galarza, MD, Wendy Glaberson, MD, Aura Arenas Morales, MD, and Denisse Cristina Pareja Valarezo, MD, from Holtz Children’s Hospital, University of Miami, Miami, FL; Sarah Cashman, BS, and Madeleine Stead, BS, from University of Iowa Children’s Hospital, Iowa City, IO; Jonathan Davis, MD, and Julie Nicoletta, MD, from Floating Hospital for Children at Tufts Medical Center, Tufts University School of Medicine, Boston, MA; Alanna DeMello, British Columbia Children’s Hospital, Vancouver, BC, Canada; Lynn Dill, RN, University of Alabama at Birmingham, Birmingham, AL; Ellen Guthrie, RN, Metro Health Medical Center, Case Western Reserve University, Cleveland, OH; Nicholas L. Harris, BS, and Susan M. Hieber, MSQM, from C.S. Mott Children’s Hospital, University of Michigan, Ann Arbor, MI; Katherine Huang and Rosa Waters from University of Virginia Children’s Hospital, Charlottesville, VA; Judd Jacobs, Ryan Knox, BS, Hilary Pitner, MS, and Tara Terrell from Cincinnati Children’s Hospital Medical Center, Cincinnati, OO; Nilima Jawale, MD, Maimonides Medical Center, Brooklyn, NY; Emily Kane, Australian National University, Canberra, ACT, Australia; Vijay Kher, DM, and Puneet Sodhi, MBBS, from Medanta Kidney Institute, The Medicity Hospital, Gurgaon, Haryana, India; Grace Mele, New York College of Osteopathic Medicine, Westbury, NY; Patricia Mele, DNP, Stony Brook Children’s Hospital, Stony Brook, NY; Charity Njoku, Tennille Paulsen, and Sadia Zubair from Texas Children’s Hospital, Baylor College of Medicine, Houston, TX; Emily Pao, University of Washington, Seattle Children’s Hospital, Seattle, WA; Becky Selman, RN, and Michele Spear, CCRC, from University of New Mexico Health Sciences Center Albuquerque, NM; Melissa Vega, PA-C, The Children’s Hospital at Montefiore, Bronx, NY; and Leslie Walther, RN, Washington University, St. Louis, MO. Cincinnati Children’s Hospital Center for Acute Care Nephrology provided funding to create and maintain the AWAKEN Medidata Rave electronic database. The Pediatric and Infant Center for Acute Nephrology (PICAN) provided support for web meetings, the NKC steering committee annual meeting at the University of Alabama at Birmingham (UAB), and support for some of the AWAKEN investigators at UAB (L.B.J., R.J.G.). PICAN is part of the Department of Pediatrics at UAB and is funded by Children’s of Alabama Hospital, the Department of Pediatrics, UAB School of Medicine, and UAB’s Center for Clinical and Translational Sciences (CCTS, NIH grant UL1TR003096). The AWAKEN study at the University of New Mexico was supported by the Clinical and Translational Science Center (CTSC, NIH grant UL1TR001449) and by the University of Iowa Institute for Clinical and Translational Science (U54TR001356). C.L.A. was supported by the Micah Batchelor Foundation. A.A.A. and C.J.R. were supported by the Section of Pediatric Nephrology, Department of Pediatrics, Texas Children’s Hospital. J.R.C. and J.R.S. were supported by a grant from 100 Women Who Care. F.S.C. and K.T.D. were supported by the Edward Mallinckrodt Department of Pediatrics at Washington University School of Medicine. J.F. and A.K. were supported by the Canberra Hospital Private Practice Fund. R.G. and E.R. were supported by the Department of Pediatrics, Golisano Children’s Hospital, University of Rochester. P.E.R. was supported by R01 HL-102497 and R01 DK 49419. S.S. and D.T.S. were supported by the Department of Pediatrics & Communicable Disease, C.S. Mott Children’s Hospital, University of Michigan. S.S. and R.W. were supported by Stony Brook Children’s Hospital Department of Pediatrics funding. Funding sources for this study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Consortia
Contributions
All listed authors provided substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, drafting the article or revising it critically, and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
All authors declare no real or perceived conflicts of interest that could affect the study design, collection, analysis and interpretation of data, writing of the report, or the decision to submit for publication. For full disclosure, we provide here an additional list of other author’s commitments and funding sources that are not directly related to this study: D.J.A. is a consultant for CHF solutions, Baxter, and Medtronic, and he receives grant funding for studies not related to this manuscript from National Institutes of Health—National Institute of Diabetes and Digestive and Kidney Diseases (NIH-NIDDK, R01 DK103608 and NIH-FDA (R01 FD005092), CHF solutions, and Baxter.
Patient consent
Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nada, A., Askenazi, D., Boohaker, L.J. et al. Low hemoglobin levels are independently associated with neonatal acute kidney injury: a report from the AWAKEN Study Group. Pediatr Res 89, 922–931 (2021). https://doi.org/10.1038/s41390-020-0963-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0963-x