Abstract
Background
To investigate relationships between infant body composition (BC) and human milk (HM) immunomodulatory proteins (IMPs) during the first 12 months of lactation.
Methods
BC of breastfeeding dyads (n = 20) was measured with ultrasound skinfolds (infants) and bioimpedance spectroscopy (infants/mothers) at 2, 5, 9, and/or 12 months post partum. Breastfeeding frequency, 24-h milk intake, and IMP concentrations (lactoferrin, lysozyme, secretory immunoglobulin A (sIgA)) were measured, and calculated daily intakes (CDIs) were determined. We used linear regression/mixed-effects models and adjusted results for multiple comparisons.
Results
No associations were seen between maternal characteristics and IMP concentrations/CDIs or between IMP concentrations and infant BC. Lactoferrin CDI was negatively associated with infant fat-free mass index (P = 0.002); lysozyme CDI was positively associated with infant fat mass (P = 0.004) and fat mass index (P = 0.004) measured with ultrasound skinfolds.
Conclusion
In this small cohort of infants breastfed on demand during first year of life, we report differential associations of HM IMPs with infant BC, showing that in addition to their critical role in shaping infant immunity, lactoferrin, and lysozyme also influence development of infant BC, highlighting the importance of breastfeeding for 12 months and beyond.
Impact
-
HM IMPs (concentrations and, most importantly, daily intakes) time-dependently and differentially associate with development of infant lean mass and adiposity during first 12 months of lactation.
-
There is no information on how intakes and concentrations of these components affect development of infant BC.
-
HM contains IMPs—lactoferrin, lysozyme, and sIgA, which not only play a critical role in shaping infant’s immunity, but also influence infant growth and development of BC, highlighting the importance of breastfeeding for 12 months and beyond and warranting careful consideration of the dose effects of supplemented formula.
Similar content being viewed by others
Introduction
Human milk (HM) protects infants against infections and inflammation, with both the whey and casein fractions containing immunological factors that ensure the infant’s survival.1,2,3 Along with α-lactalbumin, the most abundant proteins in HM whey fraction are the multifunctional immunomodulatory proteins (IMPs)—lactoferrin, lysozyme, and secretory immunoglobulin A (sIgA), which provide anti-infective responses and affect neonatal gut and microbiome.3,4,5 Limited studies also show associations of these IMPs with infant growth,6,7,8,9 but little is known about their effect on development of infant body composition (BC). Associations of other HM immunological factors with infant BC have been reported recently; tumor necrosis factor‐α concentration showed negative association with fat-free mass (FFM), but not adiposity; interleukin‐6 negatively related to infant growth and adiposity;10 thus, the relationships of HM IMPs that are present in high concentrations and infant BC are of interest.
Lactoferrin, the most studied HM IMP with respect to facilitation of iron absorption and bacteriostatic activities,11,12,13 also has multiple anti-infective, anti-inflammatory, enzymatic activities, and is involved in cells’ growth regulation,14,15,16 playing an important role in gastrointestinal development and function.17,18 Supplementation with bovine lactoferrin is associated with greater infant height and weight gains in formula-fed infants;9,19 lactoferrin is therefore a target for preclinical and clinical research,4,20 with current suggestions to increase dosages,6 despite the absence of evaluations of infant growth outcomes in relationship to the natural variations of this component in HM.
Lysozyme is also present in HM whey in high concentrations (6%), it lyses Gram-positive bacteria and, in combination with lactoferrin, some Gram-negative bacteria, and has multiple roles in infant digestion, influencing the stomach microbial profile and speeding up the microbial protein digestion.21,22,23,24 Lysozyme is implicated in the homeostasis of bone and cartilage growth,25 and in preterm infants both, orally administered lysozyme8 and higher HM lysozyme concentration,7 are associated with increased weight gain; thus, it is possible that HM lysozyme could contribute to the development of breastfed infants’ BC.
sIgA is the predominant HM immunoglobulin (90%) that provides passive immunity to the newborn against range of pathogens,12,26 and in higher concentrations enables better protection of breastfed infants against respiratory illnesses and gastrointestinal issues.27 In murine model, sIgA is shown to maintain healthy gut microbiome,28 again indicating a potential effect on infant growth.
As infant growth relates to the ingested volume of HM,6,29 it is necessary to discern the mechanisms by which HM IMPs (concentrations and intakes) could impact infant BC development, allowing for future targeted interventions that may improve infant outcomes. The main objective of this pilot longitudinal study was to assess relationships of HM lactoferrin, lysozyme, and sIgA with BC and anthropometrics of healthy term breastfed infants and their mothers during the first year of breastfeeding on demand. We also investigated the relationships of these IMPs with 24-h milk intake and breastfeeding frequency.
Methods
Subjects and design
This longitudinal observational study focused on 20 mothers and healthy term infants who were exclusively breastfed up to 5 months and continued breastfeeding on demand until 12 months. Participants were recruited from the community, primarily from the West Australian branch of the Australian Breastfeeding Association, and visited our laboratory at King Edward Memorial Hospital for Women (Subiaco, Perth, WA, Australia) for up to four monitored breastfeeding sessions (March 2013–September 2015). The eligibility criteria were as follows: singletons, gestational age ≥37 weeks, exclusively breastfed to 5 months, and breastfed at 9 and 12 months. The exclusion criteria were as follows: infant health issues potentially influencing growth and development, formula supplementation, maternal low milk supply, and smoking. Mothers provided written informed consent for participation in the study, which was approved by The University of Western Australia Human Research Ethics Committee (RA/4/1/4253, RA/4/1/2639) and registered with Australian New Zealand Clinical Trials Registry (ACTRN12616000368437).
The study design, participants, data collection procedures, and sample preparation have been described in detail previously, together with the methods for determining maternal and infant anthropometrics and BC, and the relationships between the measured parameters.30,31,32 Briefly, milk samples were collected and BC (FFM, fat mass (FM), %FM) of healthy dyads (no suspected infectious illness, such as cold or flu, and no indication of mastitis in mothers at the time of measurements) was determined when the infants were 2 and/or 5, 9, and 12 months old using ultrasound 2-skinfolds (US2SF: triceps, subscapular; infants), ultrasound 4-skinfolds (US4SF: biceps, subscapular, suprailiac and triceps; infants), and bioelectrical impedance spectroscopy (BIS; infants and mothers) measurements.30,33 The indices of mothers/infants height-normalized BC were calculated: FFM index (FFMI) was calculated as FFM/length2; FM index (FMI) was calculated as FM/length2, both expressed as kg/m2.34 The ratio of FM-to-FFM (FM/FFM) was also calculated. Twenty-four-hour milk intake and breastfeeding frequency (meals/24-h) were measured using infant test weighing before and after breastfeeding between 2 and 5 months, and within 2 weeks of 9 and 12 months.35,36 Self-reported breastfeeding frequency data was collected at the sessions as the current typical time (h) between the meals.
Measurements of IMPs
Pre-/post-feed samples were pooled and defatted for measuring IMPs.37 Lysozyme was measured by a modification of Selsted and Martinez,38,39 lactoferrin and sIgA were determined by ELISA (enzyme-linked immunosorbent assay),39,40 with the following recovery (added lactoferrin: 100.3 ± 3.0% (n = 7); lysozyme: 97.0 ± 5.0% (n = 8); sIgA: 100.6 ± 3.3% (n = 6)), detection limit (lactoferrin: 1.1 × 10−7 mg/mL; lysozyme: 0.07 g/L; sIgA: 2.4 × 10−6 mg/mL), and an inter-assay coefficient of variation (lactoferrin: 5.1% (n = 2); lysozyme: 13.0% (n = 8); sIgA: 14.5% (n = 3)). Twenty-four-hour milk intake values from the 24-h test weighing,35 and IMP concentrations measured in HM samples taken at the study sessions were used to calculate daily intakes (CDIs), which were considered representative of a typical daily intake for that time point.
Statistical analyses
Data for this analysis came from the longitudinal study, details of which, along with power calculation and statistical methods, have been described previously.30,31,32,41 Briefly, relationships were analyzed using linear mixed-effects models. Fitted models included (as explanatory variable and response) (a) maternal BC and IMP concentration/CDI; (b) IMP concentration/CDI and infant BC; (c) IMP concentration and breastfeeding parameters (24-h milk intake/breastfeeding frequency); and (d) IMP concentration/24-h milk intake/breastfeeding frequency and IMP CDI. The fixed effects were infant age (as a categorical variable) and an age interaction with the explanatory variable of interest and a random effect for each participant. The P value associated with the interaction was examined, and if it was below 0.05, the results are reported for a model with fixed effects for infant age and the explanatory variable of interest and a random effect for each participant. Where the interaction was not significant, results are reported for the same model fitted without the interaction.
The analyses for systematic differences between measured parameters at different months post partum used linear mixed model, with age as a fixed factor and participant as a random factor. Differences between months were analyzed using general linear hypothesis tests (Tukey’s all pair comparisons).
Relationships between IMP CDI measured between 2 and 5, and at 9 and 12 months post partum and changes (Δ) in infant BC and anthropometric parameters between the time points were analyzed using linear regression models.
A false discovery rate (FDR) adjustment was applied to the subgroupings of results to the interaction P value if it was <0.05 or to the main effect P value.42 The adjusted significance levels are reported in the tables and set at the 5% level otherwise. Descriptive statistics are reported as mean ± standard deviation (SD) and range; modeling results as parameters estimates ± standard error (SE). Missing data were dealt with using available case analysis. Statistical analysis and graphics were performed in R 3.1.2.
Results
Subjects
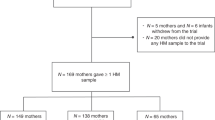
Participant demographic characteristics, determinants of maternal and infant BC, anthropometrics, and breastfeeding parameters (24-h milk intake, 24-h breastfeeding frequency, self-reported breastfeeding frequency), as well as participant attrition and missing BC data have been reported previously.30,31,32,41 Briefly, mean maternal age at the start of the study was 33.3 ± 4.7 (24–44) years, mean height was 167.4 ± 7.4 (150–181) cm, and mean parity was 2.3 ± 0.9 (1–4). Infant male/female ratio was 1:1, mean birth weight was 3.486 ± 0.498 (2.660–4.455) kg, and mean gestational age was 39.4 ± 1.3 (37.6–43.0) weeks. Demographic, anthropometric, and breastfeeding characteristics measured at the four study sessions as well as the sample sizes at each time point are presented in Table 1. The missing data also included (a) from 80 expected due to missed visits concentrations of lactoferrin and sIgA (n = 11), concentrations of lysozyme (n = 15); (b) from 60 expected due to difficulties with completing 24-h milk intakes measurements CDI of lactoferrin, sIgA (n = 27), and lysozyme CDI (n = 30). The missing data were spread across the time points (Tables 1 and 2; Supplementary Fig. S1).
Longitudinal changes in IMP
HM IMP concentrations and CDI over the first year of lactation are detailed in Table 2. Concentrations of all measured IMPs continued to increase from 2 to 12 months, while CDI did not differ (Table 3).
IMP and body composition
No associations were seen between maternal characteristics and either concentrations or CDI of IMP (data not shown).
There were no associations between IMP concentrations and infant characteristics after the FDR adjustment. However, prior to the adjustment higher lysozyme concentrations were associated with a decrease in infant FMI and FM/FFM (measured with BIS) at 2 and 12 months and an increase at 5 and 9 months, while higher sIgA concentrations were associated with smaller infant FM measured with US4SF (Supplementary Table S1).
Higher lactoferrin CDI was associated with decreased FFMI (measured with US4SF: P = 0.002), while higher lysozyme CDI was associated with increased infant adiposity (US4SF; FM: P = 0.004; FMI: P = 0.004) (Table 4, Fig. 1). No further associations were seen after the FDR adjustment (Table 4).
Breastfeeding parameters and IMP
No significant associations were seen between concentrations of IMP and 24-h milk intake, 24-h breastfeeding frequency, and SR breastfeeding frequency (data not shown).
Higher IMP concentrations were associated with higher CDI of all measured IMP (lactoferrin: P = 0.001; lysozyme: P < 0.001; sIgA: P = 0.002); higher 24-h milk intake was associated with higher CDI of lysozyme (P = 0.024) and sIgA (P < 0.001). Both higher 24-h breastfeeding frequency and lower self-reported breastfeeding frequency were associated with higher sIgA CDI (24-h breastfeeding frequency: P = 0.011; self-reported breastfeeding frequency: P = 0.002). No further associations were seen after the FDR adjustment (Table 5, Fig. 2).
Significant associations between a CDI of lysozyme and infant 24-h milk intake (p = 0.024); CDI of secretory immunoglobulin A (sIgA) and b 24-h milk intake (p < 0.001), c breastfeeding frequency (h between meals) (p = 0.002), and d breastfeeding frequency (meals/24-h) (p = 0.011). Lines represent linear regression and grouped by the month of lactation. US4SF ultrasound 4-skinfolds.
Changes in infant BC and calculated daily intakes of IMP
A significant association was seen between changes (Δ) in infant BC/anthropometrics between the time points and lysozyme CDI; higher lysozyme CDI at 12 months was associated with larger decrease in infant FFMI (US2SF: P = 0.0003) between 5 and 12 months (Table 6). No significant associations were seen at any time points between changes (Δ) in infant BC between the time points and CDI of lactoferrin and sIgA after the FDR adjustment (Supplemental Tables S2, S3).
Discussion
Increasingly, studies focus on the potential use of HM IMPs to combat multiple infections during infancy, yet childhood obesity, a risk factor for multiple non-communicable diseases, is on the rise. Our proof-of-concept longitudinal study points to the possible complex mechanisms by which HM and breastfeeding may contribute to the development of infant BC and provide some degree of protection from obesity. Previously, we have reported the absence of associations between infant BC and both HM total and whey protein.32 In this study, we focused on daily intakes of HM IMPs, which are abandoned in whey and found that the CDI of lactoferrin and lysozyme differentially relate to infant BC (Fig. 3) throughout the first 12 months of lactation.
Lactoferrin is prominent as a clinical intervention for infant health, and in this study for the first time we evaluated how natural variations of this HM component relate to BC of infants that breastfed on demand. Interestingly, concentration of HM lactoferrin did not produce significant associations with infant BC parameters (Supplementary Table S1). However, when we accounted for the variations in milk intake and calculated lactoferrin CDI, we found higher CDI was related to lower infant FFM (Table 4). Also, prior to the FDR adjustment lactoferrin CDI throughout the lactation had multiple weak positive relationships with changes in infant FFM, weight, and adiposity parameters compared with 2 months, while CDI measured between 2 and 5 months was negatively related to changes in weight and FFM between 9 and 12 months (Supplementary Table S2). There are no direct comparisons available in the literature; the few studies that evaluated the effect of lactoferrin on infant growth have used bovine lactoferrin-supplemented formula, reporting contrasting results. High concentrations of bovine lactoferrin have been associated with lower weight gain rate in healthy term 2-month-old female infants,43 have no association with 12-month-old infants’ growth parameters,44 or have been related to greater 4–6-month-old infants’ length and weight;9 the latter study suggesting that bovine lactoferrin may not have the same modulatory effects as HM lactoferrin and could be utilized by an infant as a nutrient rather than as an IMP.
In vitro studies on selected cell lines indicate that bovine lactoferrin may be a more potent effector of growth than HM lactoferrin (immature Caco-2 cells);18 may be growth inhibitory and decrease cell proliferation (MAC-T bovine mammary epithelial cells);45 and may have a dose-dependent effect, with lower doses (<1 g/L) associated with increased cell proliferation (porcine intestinal epithelial cell line), and higher doses (10 g/L) associated with reduced cell proliferation.46 Our results are consistent with these findings, highlighting the importance of considering dose effects of supplemented formula.
Additional mechanisms by which lactoferrin could impact infant growth parameters include modulation of infant gut microbiome, as shown in low birth infants,47 since microbiome has been implicated in infant weight gain and obesity,48 and increasing the bioavailability of iron to the infant. Iron supplementation in iron-replete infants has been shown both to decrease linear growth and weight and alter gut microbiota to more pathogenetic species.49 The exact mechanisms of these outcomes are not clear and interactions between lactoferrin and infant growth appear complex and require further study.
HM lactoferrin works synergistically with lysozyme, another IMP attracting growing research interest as it may improve gut health and ability to resist bacterial infection,21,22,23,24 both potentially culminating in optimal infant growth. In our study, prior to FDR adjustment, lysozyme concentration differentially associated with infant adiposity (Supplementary Table S1), with higher concentrations associating with lower adiposity parameters (FMI, FM/FFM) at 2 and 12 months, but with substantially higher adiposity at 5 and 9 months, when infant %FM is reaching a peak.50 Lysozyme CDI, however, was positively associated with infant adiposity at all time points (FM, FMI; Table 4, Fig. 1), while higher lysozyme CDI at 12 months was associated with larger decrease in FFMI between 5 and 12 months (Table 6). Prior to the FDR adjustment, we also saw positive relationships of lysozyme CDI measured earlier in lactation (between 2 and 5 months) with changes in infant weight, FM, and FFM parameters at all later time points compared with 2 months, with significance becoming weaker with time. Previously, both administered bovine8 and HM lysozyme,7 related to increased weight gain in preterm infants, support our findings.
Lysozyme is involved in protection of mucosal segments against chronic inflammation51 and in the homeostasis of bone and cartilage growth.25 Furthermore, lysozyme supports intestinal maturation and health through both reduction of the detrimental microbes and promotion of infant gut colonization by the beneficial infant-type human-residential bifidobacteria.5,52 Animal models also confirm lysozyme as an alternative to growth-promoting subtherapeutic antibiotics,53 as it shifts the microbial population towards a host-beneficial profile (porcine model)54 and leads to a significant increase in intestinal villi, providing greater area for nutrient absorption (chicken, piglet), and subsequently, increased fat accretion.55,56 However, higher doses of dietary lysozyme have been reported to suppress growth. Thus, it is possible that HM lysozyme may differentially contribute to the development of infant FM and FFM in dose-dependent manner at different times post partum and ensure the optimal FM development during infancy, resulting in a beneficial adipose phenotype of breastfed infants that is associated with a reduced risk of non-communicable diseases and obesity.57,58
HM sIgA demonstrated no significant associations with infant BC, although prior to the FDR adjustment the associations of sIgA CDI were similar to the relationships of lactoferrin CDI with infant FFM (negative) and of lysozyme CDI with infant adiposity (positive; Table 4), while the association of concentration of sIgA with infant adiposity was negative at all time points (Supplementary Table S1). Also, similar to lactoferrin CDI, sIgA CDI measured at all time points had multiple weak positive relationships with changes in infant FFM, weight, and adiposity parameters compared with 2 months (Supplementary Table S3), while CDI measured between 2 and 5 months also was negatively related to changes in weight and FFM between 9 and 12 months, again non-significant after FDR adjustment. We are not aware of any other study that investigated infant growth parameters in regards to sIgA intake, but can speculate that effect may be similar to that of lysozyme and/or lactoferrin, as a high diversity and broad spectrum of sIgA antibodies may be implicated in the development of infant mucosa and tissue-protective and anti-inflammatory activities.59 In fact, a study of sIgA-deficient mice revealed that sIgA assists in the development and maintenance of a healthy gut microbiome and influences epithelial cell gene expression, inclusive of genes associated with intestinal human inflammatory diseases.28 Interestingly, we found that sIgA CDI was positively associated with breastfeeding frequency (Table 5), which in turn is also related to milk intake.30 This is similar to a Gambian study that reported higher milk and sIgA intakes during the dry season compared with the rainy season,60 probably due to the increased transport of sIgA across mammary gland in response to the higher volumes produced.
In our study, we collected milk samples at the time when dyads were reportedly healthy and we observed a steady rise in concentrations of all three IMPs from 2 to 12 months, which resulted in consistent CDI of these components over the first year post partum (Tables 2 and 3). Previous studies report an initial decrease of IMP concentrations from colostrum to mature milk,12,61 followed by a steady increase in later lactation61,62,63 and/or when weaning.64 Other studies report a decline in lactoferrin and sIgA concentrations during first year of lactation and no clear trend for lysozyme.12 IMP concentrations were not related to maternal adiposity in our study, similar to previous reports of lack of associations between maternal body mass index and both sIgA65 and lactoferrin,66 and between lysozyme and maternal weight/height ratio.67 The absence of association with maternal adiposity and the continuous increase in concentration to maintain stable infant daily intake of these IMPs may ensure protection of the infant gut during the weaning phase, a period sensitive from an immunologic perspective. It is also possible that with slowing of infant growth rates and the introduction of solids, HM IMPs may take on a different role as growth regulators, something that might be the focus of future research.
This proof-of-concept cohort study focused on dyads that were breastfeeding on demand for 12 months; thus, it is more reflective of normative lactation and development of infant BC. The strong points of this study include the longitudinal assessment of BC of dyads and HM composition, as well as the intake of components, and the wide variation in maternal adiposity. We also had some limitations, such as the modest sample size associated with the multiple measurement time points and the small number of 24-h milk intake measurements at 9 and 12 months post partum. With a relatively homogeneous (predominantly Caucasian term healthy fully-breastfed singletons from urban mothers of higher social-economic status with lower exposure to pathogens) sample, our results may not be transferable to broader populations.
Conclusions
The findings from this small pilot study point to the complex mechanisms by which breastfeeding and HM may provide some degree of protection from obesity and reduce risk factor for non-communicable diseases later in life. We show a time-dependent differential effect of daily intakes of HM lactoferrin and lysozyme on development of infant lean mass and adiposity during the first year of life, indicating a potential to improve infant outcomes through interventions, such as extending the duration of breastfeeding to the first year and beyond.
References
Goldman, A. S. Modulation of the gastrointestinal tract of infants by human milk. Interfaces and interactions. An evolutionary perspective. J. Nutr. 130, 426S–431S (2000).
Gao, X. et al. Temporal changes in milk proteomes reveal developing milk functions. J. Proteome Res. 11, 3897–3907 (2012).
Ballard, O. & Morrow, A. L. Human milk composition: nutrients and bioactive factors. Pediatr. Clin. North. Am. 60, 49–74 (2013).
Demmelmair, H., Prell, C., Timby, N. & Lonnerdal, B. Benefits of lactoferrin, osteopontin and milk fat globule membranes for infants. Nutrients 9, 817 (2017).
Wong, C. B. & Xiao, J. Breast milk on the infant faecal microbiome: components of breast milk orchestrating the establishment of bifidobacteria species. J. Hum. Nutr. Food Sci. 6, 1123 (2018).
Manzoni, P. Clinical benefits of lactoferrin for infants and children. J. Pediatr. 173S, S43–S52 (2016).
Braun, O. H. & Sandkuhler, H. Relationships between lysozyme concentration of human milk, bacteriologic content, and weight gain of premature infants. J. Pediatr. Gastroenterol. Nutr. 4, 583–586 (1985).
Bol’shakova, A. M., Shcherbakova, E. G., Ivanova, S. D., Medvedeva, M. M. & Zhuravleva, T. P. Lysozyme in the feeding of premature infants with mixed pathology. Antibiotiki 29, 784–790 (1984).
Hernell, O. & Lonnerdal, B. Iron status of infants fed low-iron formula: no effect of added bovine lactoferrin or nucleotides. Am. J. Clin. Nutr. 76, 858–864 (2002).
Fields, D. & Demerath, E. Relationship of insulin, glucose, leptin, IL-6 and TNF-a in human breast milk with infant growth and body composition. Pediatr. Obes. 7, 304–312 (2012).
Steijns, J. M. & van Hooijdonk, A. C. M. Occurrence, structure, biochemical properties and technological characteristics of lactoferrin. Br. J. Nutr. 84, S11–S17 (2000).
Lonnerdal, B., Erdmann, P., Thakkar, S. K., Sauser, J. & Destaillats, F. Longitudinal evolution of true protein, amino acids and bioactive proteins in breast milk: a developmental perspective. J. Nutr. Biochem. 41, 1–11 (2017).
Lonnerdal, B. Nutritional and physiologic significance of human milk proteins. Am. J. Clin. Nutr. 77, 15375–15435 (2003).
Beljaars, L. et al. Inhibition of cytomegalovirus infection by lactoferrin in vitro and in vivo. Antivir. Res. 63, 197–208 (2004).
Kuipers, M. E., de Vries, H. G., Eikelboom, M. C., Meijer, D. K. & Swart, P. J. Synergistic fungistatic effects of lactoferrin in combination with antifungal drugs against clinical Candida isolates. Antimicrob. Agents Chemother. 43, 2635–2641 (1999).
Hamosh, M. Protective function of proteins and lipids in human milk. Biol. Neonate 74, 163–176 (1998).
Liao, Y., Jiang, R. & Lonnerdal, B. Biochemical and molecular impacts of lactoferrin on small intestinal growth and development during early life. Biochem. Cell Biol. 90, 476–484 (2012).
Buccigrossi, V. et al. Lactoferrin induces concentration-dependent functional modulation of intestinal proliferation and differentiation. Pediatr. Res. 61, 410–414 (2007).
Ochoa, T. J. et al. Impact of lactoferrin supplementation on growth and prevalence of Giardia colonization in children. Clin. Infect. Dis. 46, 1881–1883 (2008).
Donovan, S. M. The role of lactoferrin in gastrointestinal and immune development and function: a preclinical perspective. J. Pediatr. 173S, S16–S28 (2016).
Artym, J. & Zimecki, M. Milk-derived proteins and peptides in clinical trials. Postepy Hig. Med. Dosw. 67, 800–816 (2013).
Wang, G., Lo, L., Forsberg, L. & Maier, R. Helicobacter pylori peptidoglycan modifications confer lysozyme resistance and contribute to survival in the host. mBio 3, e00409–e00412 (2012).
Montagne, P., Cuilliere, M. L., Mole, C., Bene, M. C. & Faure, G. Changes in lactoferrin and lysozyme levels in human milk during the first twelve weeks of lactation. Adv. Exp. Med. Biol. 501, 241–247 (2001).
Qasba, P. K. & Kumar, S. Molecular divergence of lysozymes and alpha-lactalbumin. Crit. Rev. Biochem. Mol. Biol. 32, 255–306 (1997).
Reynolds, J. in The Biochemistry and Physiology of Bone (ed. Bourne, G.) 113–118 (Academic Press, New York, 1972).
Lonnerdal, B. Bioactive proteins in breast milk. J. Paediatr. Child Health 49, 1–7 (2013).
Breakey, A. A., Hinde, K., Valeggia, C. R., Sinofsky, A. & Ellison, P. T. Illness in breastfeeding infants relates to concentration of lactoferrin and secretory Immunoglobulin A in mother’s milk. Evol. Med. Publ. Health 1, 21–31 (2015).
Rogier, E. W. et al. Secretory antibodies in breast milk promote long-term intestinal homeostasis by regulating the gut microbiota and host gene expression. Proc. Natl Acad. Sci. USA 111, 3074–3079 (2014).
Vohr, B. R. et al. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics 120, e953–e959 (2007).
Gridneva, Z. et al. Relationships between breastfeeding patterns and maternal and infant body composition over the first 12 months of lactation. Nutrients 10, 45 (2018).
Gridneva, Z. et al. Human milk adiponectin and leptin and infant body composition over the first 12 months of lactation. Nutrients 10, 1125 (2018).
Gridneva, Z. et al. Human milk casein and whey protein and infant body composition over the first 12 months of lactation. Nutrients 10, 1332 (2018).
Gridneva, Z. et al. Determinants of body composition in breastfed infants using bioimpedance spectroscopy and ultrasound skinfolds—methods comparison. Pediatr. Res. 81, 423–433 (2016).
Van Itallie, T. B., Yang, M. U., Heymsfield, S. B., Funk, R. C. & Boileau, R. A. Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am. J. Clin. Nutr. 52, 953–959 (1990).
Arthur, P., Hartmann, P. & Smith, M. Measurement of the milk intake of breast-fed infants. J. Pediatr. Gastroenterol. Nutr. 6, 758–763 (1987).
Kent, J. C. et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics 117, e387–e395 (2006).
Keller, R. & Neville, M. Determination of total protein in human milk: comparison of methods. Clin. Chem. 32, 120–123 (1986).
Selsted, M. & Martinez, R. A simple and ultrasensitive enzymatic assay for the quantitative determination of lysozyme in the picogram range. Anal. Biochem. 109, 67–70 (1980).
Zhang, G. et al. Anti-infective proteins in breast milk and asthma-associated phenotypes during early childhood. Pediatr. Allergy Immunol. 25, 544–551 (2014).
Tijssen, P. in Laboratory Techniques in Biochemistry and Molecular Biology (eds Burdon, R. H. & van Knippenberg, P. H.) (Elsevier, New York, 1985).
Gridneva, Z. et al. Carbohydrates in human milk and body composition of term infants during the first 12 months of lactation. Nutrients 11, 1472 (2019).
Curran-Everett, D. Multiple comparisons: philosophies and illustrations. Am. J. Physiol. Regul. Integr. Compar. Physiol. 279, R1–R8 (2000).
Johnston, W. H. et al. Growth and tolerance of formula with lactoferrin in infants through one year of age: double-blind, randomized, controlled trial. BMC Pediatr. 15, 173 (2015).
King, J. C. et al. A double-blind, placebo-controlled, pilot study of bovine lactoferrin supplementation in bottle-fed infants. J. Pediatr. Gastroenterol. Nutr. 44, 245–251 (2007).
Rejman, J. J., Oliver, S. P., Muenchen, R. A. & Turner, J. D. Proliferation of the MAC-T bovine mammary epithelial cell line in the presence of mammary secretion whey proteins. Cell Biol. Int. Rep. 16, 993–1001 (1992).
Nguyen, D. N., Li, Y., Sangild, P. T., Bering, S. B. & Chatterton, D. E. W. Effects of bovine lactoferrin on the immature porcine intestine. Br. J. Nutr. 111, 321–331 (2014).
Sherman, M. P., Sherman, J., Arcinue, R. & Niklas, V. Randomized control trial of human recombinant lactoferrin: a substudy reveals effects on the fecal microbiome of very low birth weight infants. J. Pediatr. 173S, S37–S42 (2016).
Koleva, P. T., Bridgman, S. L. & Kozyrskyj, A. L. The infant gut microbiome: evidence for obesity risk and dietary intervention. Nutrients 7, 2237–2260 (2015).
Lonnerdal, B. Excess iron intake as a factor in growth, infections, and development of infants and young children. Am. J. Clin. Nutr. 106, 1681S–1687S (2017).
Fomon, S. & Nelson, S. Body composition of the male and female reference infants. Rev. Nutr. 22, 1–17 (2002).
Rubio, C. A. The natural antimicrobial enzyme lysozyme is up-regulated in gastrointestinal inflammatory conditions. Pathogens 3, 73–92 (2014).
Minami, J., Odamaki, T., Hashikura, N., Abe, F. & Xiao, J. Z. Lysozyme in breast milk is a selection factor for bifidobacterial colonisation in the infant intestine. Benef. Microbes 7, 53–60 (2015).
Oliver, W. T. & Wells, J. E. Lysozyme as an alternative to growth promoting antibiotics in swine production. J. Anim. Sci. Biotechnol. 6, 35 (2015).
Maga, E. A. et al. Consumption of lysozyme-rich milk can alter microbial fecal populations. Appl. Environ. Microbiol. 78, 6153–6160 (2012).
Abdel-Latif, M. A. et al. Exogenous dietary lysozyme improves the growth performance and gut microbiota in broiler chickens targeting the antioxidant and non-specific immunity mRNA expression. PLoS ONE 12, e0185153 (2017).
Long, Y. et al. Effects of dietary lysozyme levels on growth performance, intestinal morphology, non-specific immunity and mRNA expression in weanling piglets. Anim. Sci. J. 87, 411–418 (2016).
Breij, L. M. et al. Impact of early infant growth, duration of breastfeeding and maternal factors on total body fat mass and visceral fat at 3 and 6 months of age. Ann. Nutr. Metab. 71, 203–210 (2017).
Booth, A., Magnuson, A. & Foster, M. Detrimental and protective fat: body fat distribution and its relation to metabolic disease. Horm. Mol. Biol. Clin. Investig. 17, 13–27 (2014).
Pribylova, J. et al. Colostrum of healthy mothers contains broad spectrum of secretory IgA autoantibodies. J. Clin. Immunol. 32, 1372–1380 (2012).
Weaver, L. T., Arthur, H. M., Bunn, J. E. G. & Thomas, J. E. Human milk IgA concentrations during the first year of lactation. Arch. Dis. Child 78, 235–239 (1998).
Hassiotou, F. et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin. Transl. Immunol. 2, e3 (2013).
Perrin, M. T., Fogleman, A. D., Newburg, D. S. & Allen, J. C. A longitudinal study of human milk composition in the second year postpartum: implications for human milk banking. Matern. Child Nutr. 13, e12239 (2017).
Verd, S., Ginovart, G., Calvo, J., Ponce-Taylor, J. & Gaya, A. Variation in the protein composition of human milk during extended lactation: a narrative review. Nutrients 10, 1124 (2018).
Hartmann, P. E. & Kulski, J. K. Changes in the composition of the mammary secretion of women after abrupt termination of breast feeding. J. Physiol. 275, 1–11 (1978).
Bachour, P., Yafawi, R., Jaber, F., Choueiri, E. & Abdel-Razzak, Z. Effects of smoking, mother’s age, body mass index, and parity number on lipid, protein, and secretory Immunoglobulin A concentrations of human milk. Breastfeed. Med. 7, 179–188 (2012).
Yang, Z. et al. Concentration of lactoferrin in human milk and its variation during lactation in different Chinese populations. Nutrients 10, 1235 (2018).
Miranda, R. et al. Effect of maternal nutritional status on immunological substances in human colostrum and milk. Am. J. Clin. Nutr. 37, 632–640 (1983).
Acknowledgements
Many thanks are extended to all mothers and infants who participated in this study and Ms. Anna R. Hepworth for consultation on research design and assistance with data analyses. Each author has met the Pediatric Research authorship requirements. This work was supported by an unrestricted research grant from Medela AG (Switzerland). Z.G. was supported by an Australian Postgraduate Award, The University of Western Australia (Australia).
Author information
Authors and Affiliations
Contributions
All authors substantially contributed to conception and design, acquisition of data, or analysis and interpretation of data, and approved the final version of manuscript. Z.G., A.R., D.T.G., and K.M. have drafted the article and revised it critically for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare that Medela AG provided an unrestricted research grant to D.T.G., from which salaries to D.T.G., Z.G., C.T.L., and W.J.T. were paid. Medela AG provided a Top-up Scholarship for Z.G. and has provided speaker’s fees to D.T.G. for educational lectures. The funding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. Author L.C.W. provides consultancy services to ImpediMed Ltd. ImpediMed Ltd. was not involved in the inception and conducting of this research or in the writing of the manuscript. Other authors have no conflicts of interest to disclose.
Patient consent
Mothers provided written informed consent for participation in the study, which was approved by The University of Western Australia Human Research Ethics Committee (RA/4/1/4253, RA/4/1/2639) and registered with Australian New Zealand Clinical Trials Registry (ACTRN12616000368437).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gridneva, Z., Lai, C.T., Rea, A. et al. Human milk immunomodulatory proteins are related to development of infant body composition during the first year of lactation. Pediatr Res 89, 911–921 (2021). https://doi.org/10.1038/s41390-020-0961-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0961-z