Abstract
Background
While institution-sponsored wellness programs may be effective, little is known about their availability and utilization in pediatric subspecialists, and about programs physicians wish were available.
Methods
A survey of perceptions about, and availability and utilization of institutional wellness activities, was distributed electronically to pediatric subspecialists nationally. Bivariate analyses were performed using χ2 tests or independent t tests. Multivariable logistic regression models for categories of institution-sponsored programming as a function of potential predictors of program utilization were performed. Qualitative content analysis was performed for free-text survey answers.
Results
Approximately 60% of respondents participated in institution-sponsored wellness opportunities. Debriefs, Schwartz Center Rounds, mental health services, and team building events were the most available institution-sponsored wellness activities, whereas debriefs, team building, Schwartz Center Rounds, and pet therapy were most frequently utilized. Respondents desired greater social/emotional support, improved leadership, enhanced organizational support, and modifications to the physical work environment, with no significant differences across subspecialties for “wish list” items.
Conclusions
Physician wellness requires more than a “one-size-fits-all” initiative. Our data highlight the importance of encouraging and normalizing self-care practices, and of listening to what physicians articulate about their needs. Pre-implementation needs assessment allows a “bottom-up” approach where physician voices can be heard.
Similar content being viewed by others
Introduction
The importance of physician well-being has moved to the forefront of national dialogue about healthcare.1,2,3,4 The impact of burnout, secondary traumatic stress, compassion fatigue, and moral distress on the personal and professional lives of US physicians can no longer be ignored.4,5,6,7 Institutions and healthcare systems have begun implementing physician “wellness initiatives” for students, trainees, and faculty.8,9 A working definition of physician wellness has been suggested to include not merely the “absence of ill-being,” but “physical and mental well-being that allows physicians to develop their full potentials across personal and work-life domains.”3 To that end, the Triple Aim (enhanced patient experiences, population health, and health cost reduction) has expanded to a Quadruple Aim that incorporates the importance of collective well-being of the patient care team to achieve desired healthcare objectives.10,11
Despite the inherent difficulties, the most stressful and emotionally challenging elements in physicians’ lives may also be the activities from which the greatest satisfaction is derived.12 Therefore, it is critical to better understand what drives work-related distress and satisfaction and whether there are ways to support one while minimizing the other. Although personal self-care strategies and institution-sponsored programs are both essential for physician well-being, workplace initiatives likely have greater impact in reducing burnout.8,13 Although some institution-sponsored programs may be effective, little is known about who uses them and how likely they are to be utilized.8 Of particular importance is understanding which programs/services physicians wish they had available, as this may help target interventions to specific physician audiences and suggest new possibilities to explore.
To date, academic pediatric subspecialists’ opinions on existing and desired workplace wellness interventions have not been examined. In our current study, we conducted a cross-sectional national survey of physicians in five pediatric subspecialties (neonatology, critical care, palliative care, emergency medicine, and hematology-oncology) to: (1) characterize existing institution -sponsored wellness offerings; (2) determine utilization of available institution -sponsored wellness activities; and (3) identify interventions physicians wish were available to them. We hypothesize that desired interventions will be influenced by subspecialty as well as by individual personality characteristics, and that there is a disconnect between wellness programming that is offered to pediatric subspecialists and what they themselves truly desire.
Methods
Participants
Email addresses for pediatric subspecialists in neonatology (NICU), palliative care (PC), critical care (CC), emergency medicine (EM), and hematology-oncology (HO) acquired as part of our prior studies of compassion fatigue, burnout, and compassion satisfaction14,15,16,17,18 were utilized as sources of potential subjects for the current study. This project was designated as exempt human research by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Instrument
A 15-item questionnaire of personal and professional characteristics (including the “Big Five Personality Factors”19,20) as well as perceptions about, and availability and personal utilization of institutional “wellness” activities, was distributed electronically and anonymously to pediatric subspecialty providers nationally. A brief description of the study, with a hyperlink to the questionnaire, was distributed via SurveyMonkey® to all potential study participants. The invitation to participate was resent to non-responders at 2-week intervals for a total of three attempts.
Data analysis
Individual survey responses were downloaded, coded, and entered into SPSS Statistics Version 23 (IBM, Armonk, NY). Qualitative content analysis was performed for free-text answers to “What programs/support systems would you create to help you cope with compassion fatigue and burnout?” Descriptive statistics were calculated for all other survey responses. Bivariate analyses were performed using χ2 tests or independent t tests as appropriate. Multivariable logistic regression models for categories of institutional programming as a function of potential predictors of program utilization were constructed.
Results
Of the 7907 surveys delivered by SurveyMonkey®, 652 responses were returned (8.3% response rate). Of these, two individuals declined to participate and 16 participants returned a blank survey. Eighteen surveys were excluded because the participant had not completed availability and personal utilization questions, and thus the study questions could not be addressed. Twenty-six surveys were excluded because the participant was not currently a NICU, PC, CC, EM, or HO provider. This left a final study population of 590 individuals (Fig. 1).
Characteristics of the study population are shown in Table 1, Supplementary Table S1, and Supplementary Fig. S1. Of the five subspecialties included in the study, the largest number of responses came from CC and EM physicians (31.9% and 31.2% of participants, respectively). The majority of participants were female, were mid-career or senior level practitioners, and had worked at their present institution for more than 5 years. NICU and PC respondents had been in practice and employed at their current institutions longer than CC, EM, and HO participants (P < 0.01). While almost two-thirds of respondents had some education about burnout, less than half had education about compassion fatigue, and 4% were entirely unfamiliar with the concept. NICU and HO physicians were less likely than PC and EM providers to have had education about compassion fatigue (P < 0.01) and were also less likely to have received education about burnout when compared with EM (P < 0.01).
Personal self-care
Virtually all participants engaged in one or more self-care activities outside the workplace. Time spent with family/friends/pets, conversations about work-related distress, and exercise were the most frequently reported personal wellness activities (Table 1). EM and CC physicians were significantly more likely to exercise than HO (P < 0.004 and P < 0.01, respectively). EM physicians were significantly more likely to talk about work-related distress than CC, HO, or NICU physicians (Supplementary Table S1; P < 0.001, P < 0.008, and P < 0.001, respectively). PC physicians were significantly more likely to socialize, explore creative arts as a therapeutic outlet, participate in holistic practices, and utilize mental healthcare services than the other subspecialists (Supplementary Table S1), and were the least likely to engage in “negative behaviors” (e.g., self-designated excessive food or alcohol consumption, recreation drug abuse; Supplementary Table S1). NICU physicians were the least likely to talk about work-related distress, socialize with friends/family, engage in creative arts, or utilize mental healthcare as part of personal wellness regimens (Supplementary Table S1). Female study participants were significantly more likely than male participants to use social connections and holistic practices as self-care (P < 0.001). In addition, participants who self-identified with the personality trait “extroversion” were significantly more likely to exercise (P < 0.008) and to socialize (P < 0.000) as part of personal self-care, whereas individuals who identified with the trait “openness” were more likely to utilize creative arts (P < 0.000), and subjects who identified with “neuroticism” were more likely to cope using “negative habits” (P < 0.005) and mental health services (P < 0.01).
Institution-sponsored self-care
Approximately 60% of respondents reported that they participated in institutionally offered wellness opportunities (Table 1). The most frequently cited barriers to participation were the (in)convenience of scheduling (45.3%), time constraints (27.2%), the preference of participants to “handle things on my own” (34.1%), and the sentiment that partaking in the activity would not be helpful (21.9%). Sixteen percent of participants had “no idea” what programs their institution offered for physician wellness, with HO physicians the least aware and PC providers the most aware of available activities (Supplementary Table S2, P < 0.006). Impediments to participation were independent of subspecialty (Supplementary Table S1). While female study participants were significantly more likely than male participants to report “inconvenience” of institutionally sponsored wellness programs as a barrier (51.6% vs. 35%, P < 0.01), male physicians were more likely to prefer to “handle things on their own” (46% vs. 26.1%, P < 0.001) and to assume that wellness interventions would not be helpful (30% vs. 17%, P < 0.02). Participants who self-identified with “extroversion” or “agreeableness” were less skeptical of the potential personal value of attending institution-sponsored wellness activities (P < 0.05), while those who identified as “conscientious”’ were more likely to find events “too time-consuming” (P < 0.04).
Scheduled debriefs/critical incident management, Schwartz Center Rounds, and professional counseling/support groups were the institutionally sponsored wellness activities that were most available to study participants (Table 2). Availability of debriefs/critical incident management, Schwartz Center Rounds, pet therapy, and organized team building events were significantly different across subspecialties (Supplementary Table S2). Debriefs/critical incident management were least available to HO physicians, and Schwartz Center Rounds were most available to PC providers, when compared with the other subspecialists surveyed (P < 0.007 and P < 0.02, respectively). Pet therapy was most available to PC and least available to NICU physicians (P < 0.003). Organized team building events were more available to PC and EM physicians when compared with HO and NICU physicians (P < 0.02).
There were significant differences in utilization of almost all institution-sponsored wellness activities across pediatric subspecialties (Supplementary Table S2). PC providers were more likely to take advantage of all institution-sponsored wellness programs (with the exception of organized team building activities) than any of the other subspecialists surveyed (P < 0.000). NICU physicians were least likely to utilize pet therapy or institution-sponsored mental health services, while EM physicians were least likely to attend Schwartz Rounds or holistic programs, and CC physicians were least likely to participate in debriefs/critical incident management or partake of peer-to-peer support programs. Utilization of institution-sponsored wellness activities was not affected by sex nor by personal self-care activities. Individuals who self-identified with the personality trait “openness” were significantly more likely to attend institution-sponsored holistic programs (P < 0.02) and those who self-identified with “agreeableness” were more likely to attend Schwartz Rounds (P < 0.02).
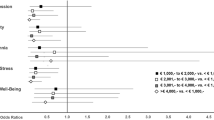
Wish lists for institution-sponsored physician wellness activities
Respondents’ free-text responses (Fig. 2) for “wish lists” for specific institutional supports to combat compassion fatigue and burnout were coded into four main categories: social/emotional support, improvements to leadership, organizational support, and modifications to the physical work environment. The categories of social/emotional support and organizational support were further parsed as shown in Table 3 and Fig. 3. There were no significant differences across subspecialties for any “wish list” items (Supplementary Table S3). For the four main categories of “wish lists,” there were no significant differences between male and female physicians; however, female physicians were significantly more likely to desire greater social/emotional support as it related specifically to enhanced opportunities for debriefing and patient connection (25% vs. 13%, P < 0.006). Self-identified “extroverts” were significantly more likely to desire modifications of their physical work environments (P < 0.04), while those who identified with “conscientiousness” were more likely to want organizational support (P < 0.05) and less likely to want social/emotional support in the form of enhanced team building (P < 0.01). Individuals who identified with “agreeableness” were also significantly less likely to request greater social/emotional support in the form of enhanced team building (P < 0.007), as well as less likely to want increased general administrative support (P < 0.03).
Institutional supports were coded into four main categories: social/emotional support, improvements to leadership, organizational support, and modifications to the physical work environment. The categories of social/emotional support and organizational support were further parsed as shown. NICU neonatology, PC palliative care, CC critical care, EM emergency medicine, HO, hematology–oncology.
Discussion
Compassion fatigue, moral distress, and burnout, alone or in combination, take their toll on the physical and emotional health of physicians.4,5,6,7 In this cross-sectional national survey of pediatric subspecialists, we present the first comprehensive evaluation of availability and utilization of institution-sponsored physician wellness activities. We also present the first investigation into the workplace wellness interventions that pediatric subspecialists wish were available to them.
Because compassion fatigue, moral distress, and burnout are interrelated phenomena that negatively impact well-being and professional performance, physicians may be unable to pinpoint a specific cause of their emotional distress.21,22 Being able to “name it to tame it”23 may well apply to physician distress. In our study population, nearly two-thirds of participants had some education about burnout, whereas less than half had received education about compassion fatigue. Greater knowledge about the prevalence of these phenomena, as well as their signs and sequelae, may help pediatric subspecialists recognize the importance of integrating self-care routines into their daily lives. We identified differences in personal self-care practices based on subspecialty, sex, and personality characteristics. While it is perhaps not surprising that PC providers were the most engaged in self-care outside of the workplace,24 it was unexpected and concerning that NICU physicians in our sample were less involved than the other subspecialists in activities that strengthen social/emotional connections in private life. That female study participants were more likely to utilize social/emotional liaisons for self-care is also not surprising, given what is understood about differences in relational styles between men and women.25 Similarly, that “extroverts” participated in activities with greater social/emotional connection and that “neurotics” were more likely to engage in “negative” habits and utilize mental health services was notable but not entirely unexpected.26,27
In recent years, many institutions and healthcare organizations around the country have embarked on wellness initiatives to address the widespread problem of physician distress and burnout.8,9 The cost of investing in institutional programs to promote physician well-being and retention is far less that the cost of replacing a “burned-out” physician.28 In our study population, the range of available institution-sponsored physician wellness activities differed across pediatric subspecialties. This raises important questions about how institutions determine which wellness interventions to provide. Are pre-implementation needs assessments being performed?29 Or are less systematic smatterings of activities simply put in place to “check the box” of providing physician wellness opportunities? Availability of an institution-sponsored wellness intervention in no way guarantees that the target audience of physicians knows it exists, uses it, or finds it effective in easing compassion fatigue or burnout. In our cohort, nearly 20% of participants reported having “no idea” what institution-sponsored self-care activities were available to them. Because it can be extremely difficult for a distressed or “burned-out” physician to seek support, it is disheartening that dissemination of this information may be so variable and/or inadequate. That barriers to participation differed by sex and personality traits speaks to the importance of providing more than a “one-size-fits-all” approach to what is offered. In our population, while there were significant differences in utilization of institution-sponsored wellness activities across subspecialties, the overall utilization rate was ~60%. While this level of involvement in self-care at work is somewhat encouraging, it does not in any way speak to the effectiveness of these interventions. Given the current alarming levels of burnout and dissatisfaction among physicians nationally, some institution-sponsored wellness activities may not be as beneficial as intended.8
In our study cohort, scheduled team debriefings, Schwartz Center Rounds, mental health services, and organized team building events were the most available institution-sponsored wellness activities, whereas debriefs, organized team building, Schwartz Center Rounds, and pet therapy were the most frequently utilized programs. Interestingly, while professional counseling/support groups were available to 43% of participants, only 17% utilized the intervention. This is in contrast to team building events and pet therapy, which while less available (40% and 18%, respectively), had greater participation (60% and 45%, respectively). It is possible that participants perceive less stigma associated with these activities.30 This underscores the importance of an institutional culture that views a physician’s receipt of mental healthcare as self-care rather than frailty.
When our study population was queried about specific institution-sponsored wellness programs they lacked but desired, the majority sought greater social/emotional support. Free-text responses (Fig. 2) included desire for “more social events within the group to deepen relationships and build camaraderie” and “social gathering to share difficult situations and debrief about them.” This is aligned with the most commonly utilized institutional offerings. Coworker relationships impact overall job satisfaction, and work-related distress arising from coworker conflict has been associated with burnout in some pediatric subspecialists.14,15,16,17,18 In specific, participants sought increased opportunities for “real-time debriefing sessions for difficult cases… either after a death or even during care of a critically ill patient.” Debriefs/critical incident management has been shown to provide a sense of support and community, and may improve resilience.31 The knowledge that peers face similar struggles can serve as a source of relief. However, successful critical incident management requires skill and sensitivity in order to avoid causing additional traumatic stress.32
There are several limitations to our study. Our survey response rate was low, which raises reasonable concerns about non-response bias. Response rates to physician surveys have declined steeply in recent years, with job demands and email/survey fatigue as the most commonly cited reasons.33,34 There is no scientifically validated, minimally acceptable survey response rate, and a low response rate, in and of itself, is not an indicator of response bias.35 Survey response rates are not strongly associated with survey quality.36 That said, we acknowledge that our response rate (at <10% in this pilot study) may introduce a greater degree of non-response bias. It is not possible to compare variables between those who responded to the survey and those who did not. However, because pediatric academic subspecialists share similar attitudes and behaviors, it is possible that responders and non-responders have comparable characteristics and thus provide similar responses. Contact information for some study participants may have been outdated; thus, our response rate may actually have been higher than our calculation.37 We did not query participants about feelings of distress or well-being on the day of survey, but either of these sentiments may have impacted participation and/or responses. The generalizability of our findings may be limited by the sample size and by the fact that participants were largely female and mid-career and senior level faculty. Our study was not designed to evaluate the impact or effectiveness of any interventions described by participants.
Conclusions
It is encouraging that physician wellness is now a benchmark worthy of consideration alongside improvements in patient care experiences and population health, and diminution in healthcare costs. However, actualization of physician wellness requires more than simply implementing a “one-size-fits-all” wellness initiative. Institutional leadership must continue to work diligently and thoughtfully to change the current pervasive culture that contributes to physician distress.38 Our data highlight the importance of providing better education to pediatric subspecialists about sources and sequelae of work-related distress, of encouraging and normalizing physician self-care practices both at home and in the workplace, and of listening and responding to what physicians articulate about their own needs. Thus, pre-implementation needs assessment allows a “bottom-up” approach where physician voices can be heard and, hopefully, answered.
References
Shanafelt, T. D., Sloan, J. A. & Habermann, T. M. The well-being of physicians. Am. J. Med. 114, 513–519 (2003).
Wallace, J. E., Lemaire, J. B. & Ghali, W. A. Physician wellness: a missing quality indicator. Lancet 374, 1714–1721 (2009).
Brady, K. J. S. et al. What do we mean by physician wellness? A systematic review of its definition and measurement. Acad. Psychiatry 42, 94–108 (2018).
Schwenk, T. L. & Gold, K. J. Physician burnout-a serious symptom, but of what? JAMA 320, 1109–1110 (2018).
Williams, E. S., Rathert, C. & Buttigieg, S. C. The personal and professional consequences of physician burnout: a systematic review of the literature. Med. Care Res. Rev. https://doi.org/10.1177/1077558719856787. (2019).
Talbot, S. G. & Dean, W. Physicians aren’t ‘burning out’ they’re suffering from moral injury. https://www.statnews.com/2018/07/26/physicians-not-burning-out-they-are-suffering-moral-injury/. Accessed 10 Jul 2019.
Jha, A. K. et al. A crisis in health care: a call to action on physician burnout. Massachusetts Medical Society. http://www.massmed.org/News-and-Publications/MMS-News-Releases/Physician-Burnout-Report-2018/. Accessed 15 Jul 2019.
West, C. P., Dyrbye, L. N., Erwin, P. J. & Shanafelt, T. D. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 388, 2272–2281 (2016).
Thomas, L. R. et al. Evidence-based interventions for medical student, trainee, and practicing physician well-being: a CHARM annotated bibliography for the Collaborative for Healing and Renewal in Medicine (CHARM) Best Practices Subgroup. https://www.semanticscholar.org/paper/Evidence-Based-Interventions-for-Medical-Student%2C-A-Thomas-Harry/bab46c61c7c879108c56c76c00cb2a1c3be39529 (2017). Accessed 10 Jul 2019.
West, C. P. Physician well-being: expanding the Triple Aim. J. Gen. Intern. Med. 31, 458–459 (2016).
Bodenheimer, T. & Sinsky, S. From Triple to Quadruple Aim: care of the patient requires care of the provider. Ann. Fam. Med. 12, 576–576 (2014).
Taylor, J. & Aldridge, J. Exploring the rewards and challenges of paediatric palliative care work. BMC Palliat. Care 16, 73 (2017).
Lemaire, J. B. & Wallace, J. E. Not all coping strategies are created equal: a mixed methods study exploring physicians’ self-reported coping strategies. BMC Health Serv. Res. 10, 208–218 (2010).
Weintraub, A. S., Geithner, E. M. & Waldman, E. D. Compassion fatigue, burnout, and compassion satisfaction in neonatologists in the U.S. J. Perinatol. 36, 1021–1026 (2016).
Kase, S. M., Waldman, E. D. & Weintraub, A. S. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric palliative care providers in the United States. Palliat. Support Care. 17, 269–275 (2019).
Gribben, J. L., Kase, S. M., Waldman, E. D. & Weintraub, A. S. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric critical care physicians in the United States. Pediatr. Crit. Care Med. 20, 213–222 (2019).
Gribben, J. L., MacLean, S. A., Pour, T., Waldman, E. D. & Weintraub, A. S. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric emergency medicine physicians in the United States. Acad. Emerg. Med. 26, 732–743 (2019).
Weintraub, A. S., Sarosi, A., Goldberg, E. & Waldman, E. D. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric hematology-oncology physicians in the United States. J. Pediatr. Hematol. Oncol. 42, e50–e55 (2020).
John, O. P. & Srivastava S. in Handbook of Personality: Theory and Research (eds Pervin, L. A. & John, O. P.) 102–138 (Guilford Press, New York, 1999).
Donellan, M. B., Oswald, F. L., Baird, B. M. & Lucas, R. E. The Mini-IPIP Scales: tiny-yet-effective measures of the Big Five Factors of personality. Psychol. Assess. 18, 192–203 (2006).
Figley, C. R. in Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized (ed. Figley, C. R.) 1–20 (Taylor & Francis Group, New York, 1995).
Fumis, R. R. L., Junqueira Amarante, G. A., de Fatima Nascimento, A. & Vieira Junior, J. M. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann. Intensive Care. 7, 71 (2017).
Siegel, D. J. Mindsight: The New Science of Personal Transformation (The Random House Publishing Group, New York, 2010).
Sanchez-Reilly, S. et al. Caring for oneself to care for others: physicians and their self-care. J. Support Oncol. 11, 75–81 (2013).
Maltz, D. N. & Borker, R. in Language and Social Identity (ed. Gumpertz, J. J.) 196–216 (Cambridge University Press, Cambridge, 1982).
Lemaire, J. B. & Wallace, J. E. How physicians identify with predetermined personalities and links to perceived performance and wellness outcomes: a cross-sectional study. BMC Health Serv. Res. 14, 616 (2014).
Bakker, A. R., Van Der Zee, K. I., Lewig, K. A. & Dollard, M. F. The relationship between the Big Five Personality Factors and burnout: a study among volunteer counselors. J. Soc. Psychol. 146, 31–50 (2006).
Han, S. et al. Estimating the attributable cost of physician burnout in the United States. Ann. Intern. Med. 170, 784–789 (2019).
Shanafelt, T. D. et al. Building a program on well-being: key design considerations to meet the unique needs of each organization. Acad. Med. 94, 156–161 (2019).
Dyrbye, L. N. et al. The impact of stigma and personal experiences on the help-seeking behaviors of medical students with burnout. Acad. Med. 90, 961–969 (2015).
Osta, A. D., King, M. A., Serwint, J. R. & Bostwick, S. B. Implementing emotional debriefing in pediatric clinical education. Acad. Pediatr. 19, 278–282 (2019).
Everly, G. S. A primer on critical incident stress management: what’s really in a name? Int. J. Emerg. Ment. Health 1, 77–79 (1999).
Rolstad, S., Adler, J. & Ryden, A. Response burden and questionnaire length: is shorter better? A review and meta-analysis. Value Health 14, 1101–1108 (2011).
Berman, D. M., Tan, L. J. & Cheng, T. L. Surveys and response rates. Pediatr. Rev. 36, 364–366 (2015).
McFarlane, E., Olmstead, M. G., Murphy, J. & Hill, C. A. Nonresponse bias in a mail survey of physicians. Eval. Health Prof. 30, 170–185 (2007).
Johnson, T. P. & Wislar, J. S. Response rates and nonresponse errors in surveys. JAMA 307, 1805–1806 (2012).
Cunningham, C. T. et al. Exploring physician specialist response rates to web-based surveys. BMC Med. Res. Methodol. 15, 32–40 (2015).
Shanafelt, T. D. et al. Healing the professional culture of medicine. Mayo Clin. Proc. 94, 1556–1566 (2019).
Acknowledgements
We thank Ni-ka Ford, Academic Medical Illustrator at the Icahn School of Medicine at Mount Sinai, for her assistance with Fig. 2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kase, S.M., Gribben, J.L., Waldman, E.D. et al. A pilot study exploring interventions for physician distress in pediatric subspecialists. Pediatr Res 88, 398–403 (2020). https://doi.org/10.1038/s41390-020-0805-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0805-x