Abstract
Background
Tissue oximeters are not interchangeable. Two instruments with sensors dedicated to preterm infants—INVOS 5100C and Nonin SenSmart X-100—have not yet been compared.
Methods
By measuring cerebral oxygenation in ten preterm infants with spontaneous apneic episodes defined by pulse oximeter readings (SpO2) below 80%, as well as tissue oxygenation during vascular occlusion on the forearm of ten adults, simultaneously we compared performance in the hypoxic range.
Results
We found the mean conversion equations to be StO2,SenSmart X-100 = 0.34 × StO2,INVOS 5100C + 44.8% during apnea in infants and StO2,SenSmart X-100 = 0.59 × StO2,INVOS 5100C + 34.4% during vascular occlusion. The individual regressions displayed large and statistically significant variations in both infants and adults. In three infants the INVOS sensor showed very little reaction to decreases in SpO2.
Conclusions
These findings confirm that different NIRS devices give very different estimates when the oxygenation is low. The large variation when compared to SpO2 suggest that the sensor placement is very important in preterm infants.
Similar content being viewed by others
Introduction
Near-infrared spectroscopy (NIRS) can be used to estimate the oxygen saturation of hemoglobin in tissue. The thin skull and scalp of infants is in theory well suited for NIRS measurements of the brain tissue, which has fueled the promise for neonatologists that NIRS-based cerebral oximetry could be an important step forward in patient monitoring. The clinical benefits of monitoring cerebral oxygenation in newborn infants have yet to be determined. The SafeBoosC study (Safeguarding the Brain of our smallest Children), a phase II randomized clinical trial including 166 extremely preterm infants, found that the use of cerebral NIRS could reduce the hypoxic burden, when used in combination with a dedicated treatment guideline.1 A phase III trial powered to detect differences in clinically relevant outcomes is under way.
The absolute values and dynamic responses to changes in oxygen saturation have been shown to differ among both devices and sensors.2,3 This implicates that the clinician will need to know the performance of their specific device and sensor in terms of normal ranges and intervention thresholds in order to use it competently, e.g., the intervention thresholds of SafeBoosC were originally determined using the INVOS 5100C with an adult sensor and to implement the treatment guideline of that trial using another NIRS instrument one needs to know how the absolute numbers compare between the devices. In that respect it is a challenge that no reference standard exists for calibration of the instruments.4
The tissue oxygenation is a volume-weighted measure, weighted by the relative arterial and venous contribution to the tissue blood pool. This distribution cannot readily be determined in vivo, which may be one of the reasons for the differences between the available NIRS devices as different manufacturers assume different arterial to venous volume ratios (AVR). Another may be that the devices use slightly different technologies, such as sensor geometry and wavelengths. And lastly the algorithms that are used to calculate the tissue oxygen saturation are most likely also not identical.
In order to establish a simple way of calibrating and comparing NIRS devices for use in neonatal care, optical phantoms mimicking the infant head have been used.5,6,7 The liquid phantom consists of a container with a blood−lipid solution that can be deoxygenated by either yeast or O2/N2 gas mixtures. NIRS measurements are performed through silicone windows. The optical properties of both windows and liquid can be adjusted to match the desired tissue. The experimental setup is fairly simple and allows simultaneous and reproducible comparison of multiple devices with a high signal-to-noise ratio in the complete range of saturations.
Our group has previously suggested vascular occlusion tests on the extremities of adults as a way to compare NIRS devices for infant use. The ischemic hypoxia induced by occlusion can be tolerated long enough to cover the relevant range and is easy to perform. However, using forearm muscles as a surrogate tissue for the infant head may be problematic given the differences in optical properties and has been shown not to compare well with the term infants head.8
With the current study we therefore aimed to compare two NIRS devices intended for preterm neonatal use by a new approach. Taking advantage of the recurrent spontaneous desaturations, commonly occurring in preterm infants with apneic episodes, we have compared two devices in the hypoxic range. Additionally, we performed vascular occlusion tests and repositions on the forearm of adults in order to test how this compares to the preterm infant head and the results from the previous phantom studies.
Materials and methods
The clinical investigation was approved by the regional Ethics Committee (jour. no. H-1-2012-011) and conducted at the Copenhagen University Hospital—Rigshospitalet, Denmark. Written informed consent was obtained from the participants or their legal guardian prior to inclusion.
Investigated NIRS devices
The INVOS™ 5100C (Medtronic, Minneapolis, MN) with the neonatal OxyAlert™ NIRSensor is supplied with a two-wavelength LED source (730 and 810 nm) and two photodiode detectors with source-detector-separations of 30 and 40 mm.
The SenSmart™ Model X-100 (Nonin Medical Inc., Plymouth, MN) with the neonatal/pediatric EQUANOX™ Advance 8004CB NA sensor is supplied with two four-wavelength LED sources (730, 760, 810 and 880 nm) and two photodiode detectors in a symmetric dual-architecture with source-detector separations of 12.5 and 25 mm for the short and long distances, respectively. Thus, a total of four light paths are achieved.
Both systems use spatially resolved spectroscopy for absolute measurements and allegedly “subtract” the short, and consequently more shallow, light path(s) from the long, in order to increase sensitivity to deeper lying tissue. In addition, SenSmart™ uses Dynamic Compensation™ in which the measured light attenuation is used as a proxy for age to correct for developmental changes in tissue optical properties, e.g. due to myelination.
It should be stressed that the INVOS system is marketed as a trend monitor. In the current study, the absolute readings are used. It is not possible, however, to establish a safe baseline in neonatal care as the sickest and smallest newborns are born in a state of hemodynamic and respiratory compromise. It is thus important to test the reliability of the absolute readings in this patient group.
It is noteworthy that the AVR used for INVOS is 25:75, while it is 30:70 for the SenSmart.
Data collection
Real-time simultaneous data from oximeters, as well as pulse oximetry and ECG, were collected using ixTrend Express 2.0 (ixellence GmbH, Wildau, Germany) acquisition software on a laptop connected to the patient monitor (IntelliVue MP70, Philips Medizinsysteme, Boeblingen GmbH, Boeblingen, Germany). The serial ports of the oximeters were connected to the patient monitor using VueLink modules (Philips Medizinsysteme, Boeblingen GmbH, Boeblingen, Germany). All data were acquired at 1 Hz.
Measurements in infants with apnea
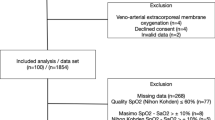
Infants born preterm (gestational age <32 + 0 weeks) and admitted to the department were recruited when more than three spontaneous desaturations (SpO2 < 80%) had occurred during the past 6 h. Dense dark hair or head size preventing simultaneous placement of sensors with at least 6 cm distance between light sources were exclusion criteria.
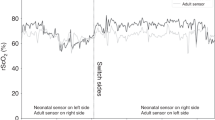
A sensor from each oximeter was placed on the fronto-parietal region, such that they measured on opposite cerebral hemispheres. The INVOS sensor was always positioned so that the cable was running backwards/dorsal, while the cable of the SenSmart was always running upwards against the vertex of the head. In addition to standard patient monitoring, an additional pulse oximeter (Masimo SET IntelliVue Module, Masimo Corp., Irvine, CA, USA) was equipped. Data were continuously collected for 4 h, after which the sensors switched position, and additionally 4 h of data were collected.
During the measurement period, the infant was left as undisturbed as allowed by daily routine care. The trial personnel were not involved in patient care or treatment.
Measurements on the adult forearm
Volunteers were recruited through local advertisement. Eligible for inclusion in the study were healthy adults (age ≥ 18 years) with a skinfold thickness of less than 10 mm on the forearm as measured by the Haperden caliper. Local skin disease or dense dark hair in the measurement area, hypertension (systolic blood pressure > 160 mmHg), active implants (e.g. a pacemaker), and pregnancy were exclusion criteria.
All measurements were performed with the participant sitting upright with the arm resting supported at heart level. The sensors were positioned on the upper anteromedial and -lateral forearm, avoiding large visible veins, and kept in place by a self-adhesive bandage. A minimum distance of 6 cm was kept between sensors to avoid cross-talk. The positions were marked with a pencil for later repositioning.
Two sensors from the same oximeter were positioned on the forearm as described above. Once steady state was established, ten 60-s measurements were performed. One sensor was removed and repositioned between each measurement in the same position, while the other served as a reference. The procedure was performed for both oximeters on each subject.
Vascular occlusion test
A sensor from each oximeter was positioned on the forearm as described above. After 1 min of measurement during steady state, a cuff on the upper arm was inflated to a pressure of 250 mmHg in order to prevent both arterial and venous circulation in the forearm. The pressure was kept for 6 min of ischemic hypoxia before the pressure was released. Once reflow ceased and a new steady state was established after approximately 5 min, the procedure was repeated to a total of six measurements. After the first three measurements the positions of the sensors were switched, using the center of the sensors for alignment. The sequence of sensor positions was arranged so that each sensor would be first on the anteromedial site five times each.
Data processing
All time series were acquired at 1 Hz and binned in 5-s intervals. Since the INVOS™ 5100C only display values between 15 and 95%, only time points with values inside this range (16% ≤ StO2,INVOS ≤ 94%) were included in analysis, to avoid possible bias. Time points with poor signal quality as indicated by error codes (e.g. excessive light) were excluded from analysis. There have been no attempts to remove noise or artifacts.
Statistical analysis
The a priori null hypothesis was that the instruments are interchangeable, i.e., they measure comparable absolute values independent of measurement value. Sample size for the paired oximetry data was estimated for both parts of the investigation to have a power of 80% (1 − β) to detect a 5-percentage point difference between absolute values. Precisions were set to 5% based on previous experience.8,9 P values below 0.05 were considered significant. Statistical tests were conducted in R.10
Measurement during apnea
The performance of the two oximeters was compared using Deming regression as both measures contain measurement error. From the time-series data, oximetry value pairs during hypoxemia (SpO2 < 80%) due to apnea were used for further analysis in order to select data more likely to reflect real physiologic change and obtain a more even distribution throughout the measurement range. The error ratio between measurement methods was estimated using time-series data without apnea (SpO2 > 80%). Unweighted Deming regression was used as the error ratio appeared to be relatively constant throughout the measurement range. The regression including all infants used a grand average error ratio, while the regressions by subject use individual error ratios. The Deming regression slope determined for each subject−sensor combination was pooled in a meta-analysis to generate a weighted average slope.11 A fixed effect model was used for the meta-analysis as all subject−sensor combinations in the two groups represent the same population, assuming that the true slope does not differ among individuals and/or between sensor positions.
Measurement during vascular occlusion
Only data acquired during cuff occlusion was used for comparison by unweighted Deming regression. Error ratio between methods was estimated from the steady-state measurement just prior to occlusion. The regression including all volunteers used a grand average error ratio, while the regressions by subject used individual error ratios. As with the infants a fixed effect meta-analysis was done.
Measurement during repositioning
To account for the spontaneous fluctuations, the precision was determined by subtracting the StO2 estimates of the reference sensor from the repositioned sensor. The mean of each 60-s measurement was calculated. Reposition precision was defined as the within-subject standard deviation (root mean square error Sw) by one-way ANOVA with subject as random factor, to account for the nonconstant nature of StO2 between instances.12 Confidence intervals and repeatability coefficients were calculated as by Bland and Altman for comparison studies with repeated measurements.13 The repeatability coefficient is defined as 2 × 1.96Sw or 2.77Sw. Two readings by the same method will be within the repeatability coefficient for 95% of subjects. It has been shown to be inversely related to the dynamic sensitivity,9,14 so the repeatability coefficients were corrected by the regression coefficient from the vascular occlusion test. As the SenSmart Model X-100 is approved for absolute readings, it was used as the reference and the INVOS 5100C readings corrected accordingly.
Results
Ten preterm infants (6 male/4 female) born at median gestational age 26 + 4 weeks (range 25 + 1–31 + 0 weeks) were recruited within the neonatal period while they exhibited spontaneous apnea (median corrected gestational age 32 + 6 weeks (range 29 + 0–34 + 5 weeks) at time of measurement). Apart from the periods with apnea, and accompanying desaturation and bradycardia, all infants were hemodynamically stable, treated with nasal continuous positive airway pressure, and had a mean weight of 1281 g (SD ± 288 g) and a mean hemoglobin concentration of 7.4 mM (SD ± 1.7 mM) at the time of measurement.
Ten healthy adults (8 male/2 female) with a median age of 29 years (range 24–36 years) and a mean skinfold of 7.3 mm (SD ± 0.9 mm) were recruited.
We did not experience drop-outs or adverse events. No infants or adults were excluded from analysis.
Comparison during apnea
The grand mean SpO2 during periods of apnea was 70.0%, while grand mean StO2 was 57.7% and 64.0% as measured by INVOS 5100C and SenSmart X-100, respectively. Figure 1 illustrates a representative time-series plot of SpO2 and the two StO2 measures in an infant with noticeable apnea. The baseline difference in StO2 between INVOS 5100C and SenSmart X-100 is more pronounced than usual in the sample but helps separate the two traces in the figure.
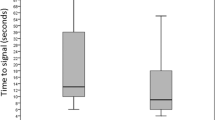
The simultaneous estimates of StO2 by INVOS 5100C and SenSmart X-100 during apnea differed significantly (P < 0.0001) with a conversion equation determined by Deming regression for all data points during apnea of StO2,SenSmart X-100 = 0.34 (CI 0.31–0.37) × StO2,INVOS 5100C + 44.8% (CI 43.2–46.6%) and a correlation coefficient (r2) of 0.458 (Figs. 2 and 3). The meta-analysis of the slopes per sensor position gave a mean slope of 0.45 (CI 0.44–0.47) (Fig. 3). There was significant heterogeneity between the positions/infants (P < 0.0001).
Comparison during vascular occlusion test
The grand mean StO2 were 83.9% (range 72–92%) and 84.0% (range 62–92%) during steady state prior to vascular occlusion when measured by INVOS 5100C and SenSmart X-100, respectively. The mean range was 23–92% for INVOS 5100C and 44–92% for SenSmart X-100 during vascular occlusions. Figure 4 illustrates a representative time-series plot of the two StO2 measures during a series of vascular occlusion tests on the adult forearm.
The simultaneous estimates of StO2 by INVOS 5100C and SenSmart X-100 during the period of occlusion differed significantly (P < 0.0001) with a conversion equation determined by Deming regression of StO2,SenSmart X-100 = 0.59 (CI 0.58–0.59) × StO2,INVOS 5100C + 34.4% (CI 34.0–34.8%) and a correlation coefficient (r2) of 0.95 (Fig. 4). The meta-analysis of the slopes per sensor position gave a mean slope of 0.56 (CI 0.557–0.562) (Fig. 5). There was significant heterogeneity among the 20 subject–sensor combinations (P < 0.0001). Furthermore, the association between the instruments was slightly different between the two positions on the arm (meta-analysis regression coefficients of 0.54 and 0.57, P < 0.0001, Fig. 6).
Precision
For the difference between the reference and repositioned sensor, the precision of the ten repeated measurements on the arm was 1.8% (CI 1.5–2.0%) and 1.5% (CI 1.3–1.7%) with INVOS 5100C and SenSmart X-100, respectively. This corresponds to a repeatability coefficient of 4.9% for INVOS 5100C and 4.1% for SenSmart X-100. If the regression coefficient (0.59) from the vascular occlusion tests is used for this correction, the repeatability coefficient of INVOSC becomes 2.9%. Table 1 compiles the repeatability precision of the repositioned and reference sensor, as well as their difference, for both devices.
Discussion
The main finding of our study is that the StO2 estimate by INVOS neonatal OxyAlert™ NIRSensor changed more than the simultaneous estimate by NONIN SenSmart™ Model X-100 during both apnea in preterm infants and during vascular occlusion on the forearm of adults. The difference was more marked in the preterm neonatal head than for the adult forearm. Overall, the difference during apnea was close to what could be expected from in vitro comparison between the same devices in a blood–lipid dynamic phantom.15 There was, however, also evidence of substantial variability in this difference depending on subject–sensor combinations, in particular on the preterm infant head.
This is to our knowledge the first study comparing different NIRS instruments on preterm infants focusing on periods of hypoxia. This has clinical relevance as cerebral hypoxia is a threat to the brain, as most of the recorded out-of-range cerebral oxygenation in preterm infants are hypoxic,1 and as most interventions prompted by StO2 in the SafeBoosC II trial were indeed in response to low values.16 The strength of this approach is that it covers a wide range of cerebral oxygenation, which enables a more robust statistical analysis. Periods of steady-state normoxia constitute the majority of collected data, but are liable to random noise. Selecting data from objective criteria with a real change in oxygenation, i.e. the hypoxic periods (SpO2 < 80%) due to apnea, increases the signal-to-noise ratio and reduce the influence of regression attenuation. Alternatively, visual inspection could be applied to select only high-quality signals, but such procedure is prone to introduce bias. In addition, we used Deming regression, which differ from simple linear regression, as it accounts for errors of measurement in both variables. Neglecting the measurement error on the independent observations will bias the regression coefficient towards 0 in a simple linear regression. Deming regression is most relevant when the correlation coefficient is low,17 i.e. the effect is most pronounced in the regression of the infant data (r2infants = 0.458 compared to r2adults = 0.954), as this will augment the effects of a possible difference in measurement error (error ratio ≠ 1). This makes Deming regression more sensitive to the estimate of the error ratio.
Inspecting the Forest plot (Fig. 3) suggests that in one of the ten infants (I), the slope in both positions was very close to unity, while in three infants, each in one position, the slope was significantly above unity, while in the remaining infants and positions the slope was significantly below unity. In the three cases when the slope was above unity, the apparent reason was that the INVOS device responded less than expected from the degree of desaturation measured by pulse oximetry. The observation suggests that in some positions on the preterm newborn head a tissue oximeter may be significantly undersensitive to desaturations. One possible physical explanation could be that the probe was placed over a collection of cerebrospinal fluid (e.g. over an open sylvian fissure) or over a collection of subarachnoid blood. That this can indeed lead to a markedly reduced reactivity to desaturation is supported by results from Monte-Carlo simulation of photon migration in an MRI-based model of the neonatal head. Here a collection of CSV under the sensor lead to a significant reduced response to increased absorption coefficient in the brain compartment.5 When placing and replacing the sensors, we did not attempt to put exactly in the same place, which would not be possible anyway due to the differences in source–detector distances in the two devices. Furthermore, we did not precisely record the positioning of the probes, nor did we attempt any brain imaging to measure the distance from skin to brain surface or to obtain evidence of normal brain structure below the sensor. Another explanation could simply be poor skin contact of the probe or hair in the light path, which the signal quality system incorporated in the device failed to detect.
It is well established that NIRS instruments differ and the present study is yet another confirmation of that. It also shows that comparing instruments on these small infants is not without problems. We have previously suggested that NIRS instruments could be compared in a simple setup of vascular occlusion test on the adult arm.9,14 The data we present here do not support that hypothesis. As mentioned, another approach is to use a liquid blood–lipid phantom where changes in oxygenation are induced. In such a phantom the conversion equation was StO2,SenSmart X-100 = 0.38 × StO2,INVOS 5100C + 42.7% compared to StO2,SenSmart X-100 = 0.34 × StO2,INVOS 5100C + 44.8% found in the present study.6 The agreement with the results obtained here suggests that the liquid phantom model might be a way forward, albeit the precision of the instruments in a clinical setting cannot be estimated using phantoms. The often-used breath down method is appealing, because it constitutes a clinical validation setup,7,18,19,20,21,22 much like the standard for validation of pulse oximeters.23 Usually, a fixed (AVR) is used to calculate a weighted reference from arterial and venous blood samples. The assumed AVR differ among instruments and it is thus not surprising that the instruments do not agree. Moreover, the venous samples of blood are collected from the jugular vein and do not solely represent drainage from the cerebral cortex. Furthermore, the assumption of a fixed AVR may also be challenged, as the normal response to hypoxia is to compensate by increasing blood flow, gradually changing the distribution between the vascular volumes.24,25 A specific problem with this model using hypoxemic hypoxia is that the ability to detect cerebral ischemic hypoxia not tested. Low SpO2 in a healthy adult will in most cases result in an increased cerebral blood flow.26,27 This comes about by a dilation of the arterial side and the AVR increases. Conversely, during ischemia, SpO2 is normal but blood flow is too low to meet the oxygen demands. In such cases the AVR is less predictable, and may in fact be decreased in the frontal regions of the preterm infant.28 The literature contains many examples of such validation studies and the results are conflicting and heterogeneous. It is therefore time to abandon this method of calibration/validation for use of cerebral oximetry in neonates and possibly also for other patient groups.
Our study has several limitations. First of all, we did not account for possible changes in blood flow, which could influence the instruments differently. During bradycardia, which often is associated with apnea during recurrent apneic spells in preterm infants, it is likely that the blood flow in the skin decrease more than the cerebral blood flow that to an extent is kept constant by cerebral autoregulation. The SenSmart sensor has source−detector separations of 12.5 and 25 mm compared to the 30 and 40 mm of the OxyAlert NIRsensor. This means, in theory, that the SenSmart samples more superficial tissue and is therefore perhaps more influenced by the tissue oxygenation of the skin and scalp. The effect of this would be that the real difference between the two devices as regard the estimate of cerebral oxygenation is underestimated. Secondly, the tissue deoxygenation happening during an apnea is different from the deoxygenation in the ischemic muscle. The vascular occlusion may lower the A:V ratio as the venous vessels are compressed first and therefore expanded distal to the occlusion from the still ongoing inflow of blood through the arteries. In contrast the cerebral arteries dilate in response to deoxygenated blood which should move the A:V ratio in the opposite direction. Thirdly, the measurements on the infants were occasionally disturbed by the routine care of the infants including tactile stimulation during some apneic episodes. This may have increased the variation. Lastly, we found that the rStO2 estimates from the two positions on the arm differed slightly. It also to some extent violates the assumption that one sensor can be used as reference during repeated measurements with a second in an adjacent area.
The precision of repeated measurements after repositioning of the sensor is also clinically relevant in neonatology. During care of a preterm infant the NIRS sensors have to be repositioned to avoid pressure sores and heat burns.1 We found better repeatability than previously reported. A possible explanation is our longer measurement periods of 60 s and our correction for the spontaneous fluctuations by keeping a second sensor positioned during all the repeated measurements and subtracting this reference from the repositioned StO2 estimate. This enables a differentiation between real variation in oxygenation and error in measurements. This is seldom done in similar studies, but gives a better impression of the signal-to-noise ratio.
In spite of these weaknesses, we conclude that the INVOS 5100C with OxyAlert NIRsensor and NONIN SenSmart Model X-100 cannot be used interchangeably unless the absolute numbers are adjusted. As both sensors are designed for the neonatal population, it is surprising that the difference is so large. The sensors have different emitter-detector geometry that, as mentioned above, could be a factor. In theory, a deeper light path should result in less StO2 decline during apnea, desaturation and bradycardia, but this is not what we observed. It is reasonable to assume that the sensors were calibrated differently, and it is as previously stated known that the assumptions of AVR are different. In theory a calibration with an AVR of 25:75 compared to 30:70 will result in lower reference rStO2 values throughout the range, but more so when the venous saturation is low compared to the arterial. If the arterial-venous difference is constant, the effect of different AVR assumptions result only in an oxygenation-level independent offset in reference rStO2 estimates. Either way the magnitude of the effect of 25:75 versus 30:70 cannot explain the difference between INVOS and Sensmart in the present study.
In the SafeBoosC II trial the thresholds for intervention were StO2 below 55% and above 85%. This range was defined by the INVOS adult sensor.29 Neither of the sensors used here agree with that sensor,3,15 but a range of 55–85% with the OxyAlert NIRSensor would correspond to a range of 64–74% with the SenSmart. Thus, our results are important in the effort to include both instruments in such a trial aiming at testing the effects of NIRS monitoring on clinical outcomes and for any clinical use that depends on absolute values. Furthermore, the large variation in slopes and the fact that the INVOS sensor in three infants failed to detect decreases in SpO2 suggest that the placement of the NIRS sensor on the infant head must be done meticulously and perhaps with a standard procedure for fast clinical assessment of the correlation between the NIRS readings and SpO2 to decrease the likelihood of false normal estimates of the cerebral oxygenation. False reassurance could be harmful for the infants and perhaps cancel out any benefits of cerebral NIRS monitoring in the preterm infant population.
Conclusion
INVOS neonatal OxyAlert™ NIRSensor and NONIN SenSmart™ Model X-100 show significant differences in cerebral StO2 dynamics during apnea in preterm infants as well as during vascular occlusion on the forearm of adults. The estimate of the difference in response between the sensors varied between sensor positions in the study subjects, especially on the infants’ heads.
Change history
02 April 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41390-020-0869-7
References
Hyttel-Sørensen, S. et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase II randomised clinical trial. BMJ 350, g7635 (2015).
Hessel, T. W., Hyttel-Sørensen, S. & Greisen, G. Cerebral oxygenation after birth—a comparison of INVOS ®and FORE-SIGHT™ near-infrared spectroscopy oximeters. Acta Paediatr. 103, 488–493 (2014).
Dix, L. M. L., van Bel, F., Baerts, W. & Lemmers, P. M. A. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr. Res. 74, 557–563 (2013).
Wolf, M., Naulaers, G., van Bel, F., Kleiser, S. & Greisen, G. A review of near infrared spectroscopy for term and preterm newborns. J. Infrared Spectrosc. 20, 43–55 (2012).
Dehaes, M. et al. Assessment of the frequency-domain multi-distance method to evaluate the brain optical properties: Monte Carlo simulations from neonate to adult. Biomed. Opt. Express 2, 552–567 (2011).
Kleiser, S. et al. Comparison of tissue oximeters on a liquid phantom with adjustable optical properties: an extension. Biomed. Opt. Express 9, 86–101 (2018).
Bickler, P. E., Feiner, J. R. & Rollins, M. D. Factors affecting the performance of 5 cerebral oximeters during hypoxia in healthy volunteers. Anesth. Analg. 117, 813–823 (2013).
Hyttel-Sørensen, S., Hessel, T. W., la Cour, A. & Greisen, G. A comparison between two NIRS oximeters (INVOS, OxyPrem) using measurement on the arm of adults and head of infants after caesarean section. Biomed. Opt. Express 5, 3671 (2014).
Hyttel-Sørensen, S., Sorensen, L. C., Riera, J. & Greisen, G. Tissue oximetry: a comparison of mean values of regional tissue saturation, reproducibility and dynamic range of four NIRS-instruments on the human forearm. Biomed. Opt. Express 2, 3047–3057 (2011).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, Austria, 2013).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 7, 177–188 (1986).
Bland, J. M. & Altman, D. G. Agreement between methods of measurement with multiple observations per individual. J. Biopharm. Stat. 17, 571–582 (2007).
Bland, J. M. & Altman, D. G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 8, 135–160 (1999).
Hyttel-Sørensen, S., Hessel, T. W. & Greisen, G. Peripheral tissue oximetry: comparing three commercial near-infrared spectroscopy oximeters on the forearm. J. Clin. Monit. Comput. 28, 149–155 (2014).
Kleiser, S., Nasseri, N., Andresen, B., Greisen, G. & Wolf, M. Comparison of tissue oximeters on a liquid phantom with adjustable optical properties. Biomed. Opt. Express 7, 2973–2992 (2016).
Riera, J. et al. The SafeBoosC phase II clinical trial: an analysis of the interventions related with the oximeter readings. Arch. Dis. Child Fetal Neonatal Ed. 101, F333–F338 (2015).
Linnet, K. Performance of Deming regression analysis in case of misspecified analytical error ratio in method comparison studies. Clin. Chem. 44, 1024–1031 (1998).
Rasmussen, P. et al. Capillary-oxygenation-level-dependent near-infrared spectrometry in frontal lobe of humans. J. Cereb. Blood Flow Metab. 27, 1082–1093 (2007).
Pollard, V. et al. Validation in volunteers of a near-infrared spectroscope for monitoring brain oxygenation in vivo. Anesth. Analg. 82, 269–277 (1996).
MacLeod, D. B. et al. Development and validation of a cerebral oximeter capable of absolute accuracy. J. Cardiothorac. Vasc. Anesth. 26, 1007–1014 (2012).
Benni, P. B. A validation method for near-infrared spectroscopy based tissue oximeters for cerebral and somatic tissue oxygen saturation measurements. J. Clin. Monit. Comput. 0, 0–0 (2017).
Henson, L. C., Calalang, C., Temp, J. A. & Ward, D. S. Accuracy of a cerebral oximeter in healthy volunteers under conditions of isocapnic hypoxia. Anesthesiology 88, 58–65 (1998).
ISO. 80601-2-61:2011 Medical Electrical Equipment—Part 2-61: Particular requirements for basic safety and essential performance of pulse oximeter equipment (2017).
Rasmussen, M. B., Eriksen, V. R., Andresen, B., Hyttel-Sørensen, S. & Greisen, G. Quantifying cerebral hypoxia by near-infrared spectroscopy tissue oximetry: the role of arterial-to-venous blood volume ratio. J. Biomed. Opt. 22, 25001 (2017).
Watzman, H. M. et al. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology 93, 947–953 (2000).
Xu, F., Liu, P., Pascual, J. M., Xiao, G. & Lu, H. Effect of hypoxia and hyperoxia on cerebral blood flow, blood oxygenation, and oxidative metabolism. J. Cereb. Blood Flow Metab. 32, 1909–1918 (2012).
Nöth, U., Kotajima, F., Deichmann, R., Turner, R. & Corfield, D. R. Mapping of the cerebral vascular response to hypoxia and hypercapnia using quantitative perfusion MRI at 3 T. NMR Biomed. 21, 464–472 (2008).
Noori, S., Stavroudis, T. A,. & Seri, I. Systemic and cerebral hemodynamics during the transitional period after premature birth. Clin. Perinatol. 36, 723–36–v (2009).
Hyttel-Sørensen, S. et al. A phase II randomized clinical trial on cerebral near-infrared spectroscopy plus a treatment guideline versus treatment as usual for extremely preterm infants during the first three days of life (SafeBoosC): study protocol for a randomized controlled trial. Trials 14, 120 (2013).
Acknowledgements
We are thankful for the parents of the infants who decided to participate in the clinical investigation.
Author information
Authors and Affiliations
Contributions
B.A. conceptualized and designed the study, performed data collection and analysis, drafted and revised the manuscript, and approved the final manuscript as submitted. G.G. conceptualized and designed the study, performed data analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted. S.H.-S. conceptualized and designed the study, performed data analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andresen, B., Greisen, G. & Hyttel-Sorensen, S. Comparison of INVOS 5100C and Nonin SenSmart X-100 oximeter performance in preterm infants with spontaneous apnea. Pediatr Res 87, 1244–1250 (2020). https://doi.org/10.1038/s41390-020-0752-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0752-6
This article is cited by
-
Cerebral oxygen saturation in neonates: a bedside comparison between neonatal and adult NIRS sensors
Pediatric Research (2023)
-
Preterm infants variability in cerebral near-infrared spectroscopy measurements in the first 72-h after birth
Pediatric Research (2023)
-
Neuromonitoring in neonatal critical care part II: extremely premature infants and critically ill neonates
Pediatric Research (2023)