Abstract
Background
The Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA-FS) is a 50-item, criterion-specified questionnaire that assesses a child’s adaptive skills in everyday context and can be used in high-risk follow-up settings to identify risk for adverse neurodevelopmental outcome. Our aim was to validate the WIDEA-FS by comparing a sample of typically developing children to children with special health needs and to compare results to the Capute Scales, which include domains of including both the Cognitive Adaptive Test (CAT) and the Clinical Linguistic and Auditory Milestone Scale (CLAMS).
Methods
Six hundred and sixty children (typically developing and having special healthcare needs) aged 0–36 months completed the WIDEA-FS, the CAT, and the CLAMS assessments.
Results
Children with special health needs scored significantly lower on the WIDEA than those with typical development. WIDEA-FS subscales were significantly associated with the CAT (WIDEA-FS self-care 0.87, social cognition 0.89) and the CLAMS (WIDEA-FS communication 0.96, social cognition 0.92) tests.
Conclusions
The WIDEA-FS has concurrent validity with the CAT and CLAMS and construct validity in that children with special health needs have significantly poorer performance on the WIDEA-FS than children with typical development.
Impact
-
The WIDEA-FS demonstrated both construct validity and concurrent validity with the Capute Scales, including the Cognitive Adaptive Test (CAT) and the Clinical Linguistic and Auditory Milestone Scale (CLAMS).
-
This is the first study to validate the use of the WIDEA-FS in children with typical development and children with special healthcare needs.
-
The WIDEA-FS is a quick and valid checklist that can be used to assess neurodevelopmental functioning during daily activities in typically developing children and those at risk for neurodevelopmental differences.
Similar content being viewed by others
Introduction
Major advances in pediatric medicine have resulted in the increased survival of infants born preterm, as well as children with complex genetic, neurological, cardiac, and oncological impairments.1,2,3 However, the majority of these children are at risk for a variety of developmental challenges in self-care, motor, communication, and social learning skills.3,4,5 In addition, a disproportionately large number of children at risk for developmental disability grow up in environments where poverty and family stressors are abundant but quality early childhood and habilitative experiences are scarce.6,7 In order to measure the effectiveness of intervention programs for children both at risk for and who have developmental delays, outcome assessment tools that describe daily activities are required.
Presently available outcome measures, such as the Vineland Adaptive Behavior Scales8 and the Bayley Scales of Infant and Toddler Development, Third Edition,9 are able to effectively discern subtleties in developmental delay in young children. The results of these standardized assessments can be used to identify children who would benefit from early intervention services. However, these tests come with a high cost for both families and healthcare centers because the tests require lengthy interviews, in-person visits, and administration conducted by trained examiners. Currently, tools for children younger than 3 years of age that are flexible for pediatric, early childhood, rehabilitation, and social work professionals require sequential use over time and are limited in their abilities to identify daily tasks that can enhance parental confidence and a child’s sense of competency.
Msall and colleagues developed the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA-FS) as a quick and low cost measure of functional abilities in early childhood.10 The WIDEA-FS is a multidisciplinary observation criterion scale designed to provide a checklist of emerging functional skills in children from birth to 36 months of age and includes the following 4 domains: (1) self-care in feeding, dressing, and diaper awareness, (2) mobility, (3) communication, and (4) social cognition. The WIDEA-FS was designed by a multi-disciplinary group of professionals whose goal was to measure criterion-specific activities, occurring during a young child’s daily routine. The individual items were selected based on their relationship to meaningful everyday tasks that parents could easily observe or participate in with the child. The WIDEA-FS has been used as an outcome measure in children with Krabbe disease,11 children with prenatal exposure to ZIKA virus,12 and in children with a history of moderate-to-severe encephalopathy.13,14 While this test has been used as an outcome measure in high-risk populations, it is important to validate the test in a normative sample. The goal of this study was to evaluate validity of the WIDEA-FS by comparing a sample of typically developing children to children with special health needs ages 0–36 months and to evaluate the concurrent validity between subscales of the WIDEA-FS to the Capute Scales15 consisting of the Cognitive Adaptive Test (CAT; a measure of visual motor problem solving) and the Clinical Linguistic and Auditory Milestone Scale (CLAMS; a measure of language).16
Methods
Participants
The subjects were 660 children (356 boys, 304 girls) between the ages 0 and 36 months. We prospectively recruited the following two cohorts of children: (1) children with typical development and (2) children with special healthcare needs (SHN). Children in the typically developing cohort were recruited after developmental screening by their pediatrician during well-child visit. Children were recruited in the SHN cohort if they met any of the following criteria: (1) at risk for health problems or developmental delays due to prematurity (birth weight <1500 g), small for gestational age, or had chronic medical conditions (e.g., seizures, congenital malformations requiring surgery); (2) children with physical disability (cerebral palsy); (3) children with developmental delay; and (4) children with genetic disorder (e.g., Trisomy 21, spina bifida).
Among the participants, 112 experienced SHN (74 boys, 38 girls; Supplemental Table 1). Subjects were recruited from the University of Chicago Comer and LaRabida Children’s Hospitals (Chicago, Illinois), the Women and Children’s Hospital of Buffalo (Buffalo, NY), UT Galveston (TX), and Child Developmental and Rehabilitation Center (Oregon Health & Science University). Full Institutional Review Board approval was obtained at all sites, and written parental consent was obtained for each participant.
All subjects were simultaneously assessed using the WIDEA-FS and CLAMS (Supplemental Table 1). A subset of the cohort of children with typical development and all children with SHN were also tested with the CAT (Supplemental Table 1). A member of the study team who was familiar with the Capute Scales and the WIDEA-FS administered the examinations.
Test instruments
Warner Initial Developmental Evaluation of Adaptive and Functional Skills
The WIDEA-FS was initially constructed using a Delphi consensus among a multidisciplinary team of experts, including developmental pediatricians, developmental psychologists, early childhood educators, physical therapists, occupational therapists, speech language pathologists, and nurse practitioners. Subjects were recruited for initial testing in several clinical scenarios including a well-child clinic, a neonatal intensive care unit follow-up clinic, an Early Intervention program, and a clinic devoted to surveillance of children with cerebral palsy, spina bifida, congenital malformations, and developmental delay. The test items were selected to represent meaningful functional behaviors which represented all domains of daily activities. Scoring was determined using criterion-specific areas so as to cover a meaningful Likert scale, using four response choices for each item. The WIDEA-FS consists of 50 individual items contained within the following domains: self-care (17 items), mobility (9 items), communication (13 items), and social cognition (11 items). Each item consists of an explicit operationally defined task that is part of an everyday activity and is rated on a scale of one (never performs task) to four (always performs task). Examples of test items from each subscale include: “chews solid food” (self-care), “maintains sitting without support” (mobility), “demonstrates two-syllable babbling” (communication), and “looks for an object dropped out of sight” (social cognition). The total score ranges from 50 to 200 points. Once a child achieves the maximum score in each domain, one can be assured that basic skills have been achieved.
The form can be completed in several ways: directly by the parents/caregiver, through a structured interview between parents/caregiver and the health professional, or via telephone interview. The WIDEA-FS takes approximately 10 min to complete and is available in both English and Spanish (Supplementary Material).
The Capute Scales
The Capute Scales are a neurodevelopmental assessment battery for children between birth and 36 months of age and consists of the CAT and the CLAMS15,16,17 sub-domains. The CAT measures visual motor and problem-solving skills. The CAT involves observation of the child in a structured problem-solving play situation with common children’s toys, including blocks, puzzles, and crayons. The CLAMS is a language assessment tool that measures expressive and receptive language skills in the first 36 months of life.16 This assessment consists of age-based language milestones, which are recorded through elicitation (orienting toward a bell, playing with blocks, picture cards, repetition of numbers, following prepositional commands) and parent interview.16
The Capute Scales, including the CAT and CLAMS, has been used to measure performance in children with typical development,18 children who were born prematurely,19 as well as in children with genetic,20 cardiac,21 or immunological disorder,22 or experienced cerebral palsy,19 intellectual disability,20 or autism.20
Statistical analysis
Analyses were conducted using the statistical computing package Stata Version 15. The mean, median, and standard deviation (SD), and several percentiles (5th, 10th, 25th, 50th, 75th, 95th) were calculated for each domain of the WIDEA-FS as well as the total score (sum of self-care, mobility, communication, social cognition domains) for the following age ranges of children with typical and SHN: 0–4.9, 5–5.9, 6–6.9, 7–7.9, 8–8.9, 9–9.9, 10–10.9, 11–11.9, 12–12.9, 13–15.9, 16–18.9, 19–21.9, 22–24.9, 25–30.9, and 31–36.9 months.
We compared WIDEA-FS scores between children with typical development and SHN using a linear regression model, with age at the time of WIDEA-FS examination as a covariate. In addition, the area under the receiver operating characteristic (aROC) curve was calculated to assess the ability of the WIDEA-FS to discriminate between children with typical development vs. those with SHN. For sensitivity and specificity, a cutpoint was chosen based on maximizing the Youden Index (sensitivity + specificity − 1).
In order to understand relationships between the WIDEA-FS subscales and the CAT and CLAMS tests, we calculated the Spearman rank correlation coefficient between (1) WIDEA-FS communication score and CLAMS raw score; (2) WIDEA-FS self-care score and CAT raw score; (3) WIDEA-FS social cognition and CLAMS raw score; (4) WIDEA-FS social cognition score to CAT raw score. In addition, we report 95% confidence intervals for the correlations, based on Fisher’s transformation. Partial correlations, adjusted for age, were also calculated based on rank values.
Results
There were 660 children concurrently tested with the WIDEA-FS and the CLAMS. Of these children, 548 were considered to have typical development (Table 1) and 112 children had SHN (Supplemental Table 2). A subgroup of children with typical development received the CAT (n = 318, 58%), while the majority of children with SHN (n = 111, 99%) completed both the CAT and CLAMS assessment (Supplemental Table 1). Demographic and clinical characteristics of the participants are listed in Supplemental Table 1. Mean and percentile scores (p5, p10, p25, p50, p75, p95) on the WIDEA-FS in children with typical development are listed by age group in Table 1 and Supplemental Table 3.
Children with SHN had lower birth weights and more male participants than typically developing children
Children in the SHN group were significantly older at time of the WIDEA-FS assessment and had significantly lower birth weights than children in the typically developing group (Supplemental Table 1). Additionally, the SHN group had a significantly larger proportion of males than the typically developing group. Social class as measured by Hollingshead Index (Hollingshead, A. B., 1975, Four factor index of social status, unpublished) did not differ significantly between groups (Supplemental Table 1).
WIDEA-FS total score and domain scores were significantly lower in children with SHN compared to typically developing children
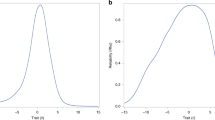
Children in the typically developing group had increasing total scores (Table 1) and domain scores (Supplemental Table 3) with age. The total WIDEA-FS score for children with SHN also increased with age, but for any given age, the SHN group had lower domain and total scores than in the typically developing children (Supplemental Tables 2 and 3). In fact, after controlling for age, WIDEA-FS scores were significantly lower in the group of children with SHN when compared to the children with typical development in total score and in each domain score (Fig. 1). When accounting for age, those children with SHN scored an average of 33 points less than those children with typical development (Table 2). Each WIDEA-FS subscale mean score was significantly less in the group with SHN, as compared to those with typical development (self-care, 10 points lower; mobility, 5 points lower; communication, 11 points lower; social cognition, 7 points lower; Table 2).
Interestingly there were some ceiling effects noted on subscales of the WIDEA-FS in typically developing children. The majority of typically developing children received the maximum score on the mobility subscale between 12 and 15 months, the communication subscale between 18 and 21 months, and the social cognition subscale between 25 and 30 months (Fig. 1). The self-care subscale did not have a similar ceiling effect for typically developing children before 3 years of age (Fig. 1).
Differentiation between children with typical development and children with SHN using the WIDEA-FS
The aROC, cutpoints (calculated using the Youden Index), and sensitivities/specificities for predicting SHN among the following age groups 22–24.9 months, 25–30.9 months, and 31–36 months of age are listed in Table 3. Of all the WIDEA-FS subscales, communication had the highest aROC curve for all the age groups.
WIDEA-FS scores are associated with the CAT and the CLAMS scores
There were significant associations between WIDEA-FS and CAT and CLAMS scores, with and without adjustments for age (Table 4). More specifically, the WIDEA-FS communication and social cognition subscales were each significantly related to the CLAMS test with a high correlation (communication 0.96; social cognition 0.92; Table 4). The WIDEA-FS self-care and WIDEA-FS social cognition were also significantly related to the CAT subscale (0.87 self-care; 0.89 social cognition; Table 4).
Discussion
In this prospective study of children with both typical development and children with SHN, we established construct validity of the WIDEA-FS in finding that children with SHN demonstrated significantly lower WIDEA-FS scores than children who were typically developing. While the WIDEA-FS scores were higher in typically developing children, scores in all the groups of children increased along with age indicating a measurement of emerging skill acquisition that parallels developmental maturation. We also established concurrent validity between the WIDEA-FS (communication and social cognition subscales) with the CLAMS as well as WIDEA-FS (self-care and social cognition) with the CAT.
The WIDEA-FS measures tasks that are functional activities and represent the everyday skills of young children. It is not surprising therefore that typically developing children had a significantly greater level of functioning than children with SHN (Table 2).
In a similar fashion, the age at which typically developing children were able to achieve the maximum scores on the WIDEA-FS follow that of developmental maturation; the earliest skills emerged in the mobility subscale, followed by language, and ending with self-care. This age-ordered performance on WIDEA-FS subscales mirror typically developing sequences of developmental maturation.23
Similar to the Capute Scales, the WIDEA-FS provides a short developmental catalog that can be completed in <15 min without special equipment and does not require the administrator to have advanced professional training. Many items on the WIDEA-FS communication subscale measure similar skills to those on the CLAMS. For example, both assessments measure how often or if the child uses gestures to communicate and if a child correctly understands the words “mama and dada.” Thus the high correlation seen between these two measures (Table 4) supports the idea that they measure similar constructs.
Interestingly, the items on the CAT and the WIDEA-FS self-care subscale do not overlap as directly, yet they are still significantly correlated (Table 4). The WIDEA-FS self-care scale measures the child’s ability to chew, independently feed using fingers, use a spoon and fork, and drink from a cup without a lid. The CAT measures items such as the ability to lift a cup, obtain a cube, and secure a pellet. While these items are different in their everyday context, the manipulative skills required to do each may represent enough similar tasks that the two tests are highly correlated.
While the WIDEA-FS subscale social cognition is a unique domain, we chose to compare it with the CLAMS because the items that are measured in social cognition are heavily dependent on language. Social skills measured in the social cognition domain like playing “peek-a-boo,” imitating another child, and pretend play require understanding of names of objects, people, and requests, gesturing language, and making sense of social communicative interactions. Unsurprisingly, we saw a significant correlation between WIDEA-FS social cognition and CLAMS scores.
Based on a similar rationale, we also chose to compare the WIDEA-FS social cognition to the CAT. Tasks on the social cognition subscale of the WIDEA-FS, like taking turns to roll a ball, turning pages in a book, and helping with household tasks require problem-solving skills, which require visual localization and manipulation of objects. These adaptive skills measured on the WIDEA require the same foundation of visual motor skills reflected in the items measured on the CAT. While both the CAT and CLAMS were significantly correlated to the WIDEA-FS social cognition subscale, the CLAMS had a slightly higher correlation with the social cognition WIDEA-FS subscale than with the CAT. In each comparison between tests, the CLAMS had the highest correlation to both WIDEA-FS subscales (Table 4).
While the three subscales we compared to the CAT and CLAMS were correlated, we did not compare the WIDEA-FS mobility subscale to the CAT and CLAMS. The CAT and CLAMS was designed as a measure of cognitive, linguistic, and adaptive abilities.24 The gross motor abilities tested in the WIDEA-FS mobility subscale are not reflected in the CAT or CLAMS tasks. Future studies should compare the WIDEA-FS mobility subscale to a motor-based developmental outcome measure to confirm concurrent validity.
Our study is limited in that children in the SHN group were significantly older at the time of WIDEA-FS assessment. Children with SHN tended to be recruited into the study later than typically developing peers, likely because they had more medical complexity and may have more often been hospitalized during earlier time points than their typically developing peers who were followed in outpatient clinics in the traditional follow-up sequence. For this reason, the WIDEA-FS appears to be more evidently valid in the SHN population after 18 months of age. Therefore, our results should be interpreted with some caution.
We chose to calculate cutpoints to indicate a differentiation or risk of delay at three time points in the second year of life (22–24.9 months, 25–30.9 months, and 31–36.9 months), because children in our SHN cohort tended to be older at the time of WIDEA-FS testing. If the goal of the clinician is to use the WIDEA-FS to screen children who will need to receive a more detailed, in-person neurodevelopmental assessment, we recommend that the clinician consider using the cutpoints listed in Table 3 for children between 22 and 36.9 months of age, especially in the self-care, communication, and social cognition domains. Because we found a ceiling affect at a younger age in the mobility domain of the WIDEA-FS domain, the 2-year cutpoints are less robust in distinguishing between children with typical and SHN. For this reason, we have included the tables with percentile scores of children with typical development at all ages (Table 1 and Supplemental Table 3) and encourage clinicians to use the 10th percentile scores to refer children at younger ages for more detailed assessment.
The results of this study suggest that the WIDEA-FS can be a useful tool for the description of functional status in everyday activities in children between birth and 36 months of age. It is important for clinicians working with infants and children at risk of delay to identify those children who would benefit from targeted interventions and supports. However, it is not always possible for families to complete traditional detailed standardized testing, which requires a visit with a skilled tester and participation of the child. Considering that the time it takes to complete the WIDEA-FS is much less than that of traditional observational and questionnaire inventories, it can be used easily as either a part of a battery of developmental tests or when other, more extensive testing is unavailable. This test may also be issued remotely and may be of benefit to families who have limited resources to travel to a pediatric medical center or are burdened by traveling a great distance to receive follow-up care.
We believe that the WIDEA-FS is an efficient and valid assessment that provides health professionals and educators a comprehensive overview of emerging functioning during daily routines. This can help professionals prioritize interventions that underly the motor, communicative, and social aspects of these routines.
References
Horbar, J. D. et al. Trends in mortality and morbidity for very low birth weight infants, 1991-1999. Pediatrics 110, 143–151 (2002).
Lemons, J. A. et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. Pediatrics 107, e1 (2001).
Doyle, L. W. & Victorian Infant Collaborative Study. Evaluation of neonatal intensive care for extremely low birth weight infants in Victoria over two decades: I. Effectiveness. Pediatrics 113, 505–509 (2004).
Marlow, N., Wolke, D., Bracewell, M. A., Samara, M. & Group, E. P. S. Neurologic and developmental disability at six years of age after extremely preterm birth. N. Engl. J. Med. 352, 9–19 (2005).
Vohr, B. R. & Allen, M. Extreme prematurity-the continuing dilemma. N. Engl. J. Med. 352, 71–72 (2005).
Wang, Q. Disability and American families: 2000. Bulletin 62, 21–30 (2005).
Msall, M. & Park, J. in Neurodevelopmental Disabilities: Clinical and Scientific Foundations (ed. Hart, H. M.) 27–42 (Mac Keith Press, 2009).
Sparrow, S. S., Cicchetti, D. & Balla, D. A. Vineland Adaptive Behavior Scales (Springer, 1984).
Bayley, N. Bayley Scales of Infant and Toddler Development (The Psychological Corporation, 2006).
Ottenbacher, K. J. et al. Functional assessment and care of children with neurodevelopmental disabilities. Am. J. Phys. Med. Rehabil. 79, 114–123 (2000).
Duffner, P. K. et al. Developmental and functional outcomes in children with a positive newborn screen for Krabbe disease: a pilot study of a phone-based interview surveillance technique. J. Pediatr. 161, 258.e1–263.e1 (2012).
Mulkey, S. B. et al. Neurodevelopmental abnormalities in children with in utero Zika virus exposure without congenital Zika syndrome. JAMA Pediatr. 174, 269–276 (2020).
Mulkey, S. B. et al. Erythropoietin and brain magnetic resonance imaging findings in hypoxic-ischemic encephalopathy: volume of acute brain injury and 1-year neurodevelopmental outcome. J. Pediatr. 186, 196–199 (2017).
Gonzalez, D. E. M., Juul, S. E., Mathur, A. M., Van Meurs, K. & McKinstry, R. C. Placental pathology and neonatal brain MRI in a randomized trial of erythropoietin for hypoxic-ischemic encephalopathy. Pediatr. Res. 493, 6 (2019).
Hoon, A. H. Jr, Pulsifer, M. B., Gopalan, R., Palmer, F. B. & Capute, A. J. Clinical adaptive test/clinical linguistic auditory milestone scale in early cognitive assessment. J. Pediatr. 123, S1–S8 (1993).
Capute, A. J., Shapiro, B. K., Wachtel, R. C., Gunther, V. A. & Palmer, F. B. The Clinical Linguistic and Auditory Milestone Scale (CLAMS). Identification of cognitive defects in motor-delayed children. Am. J. Dis. Child. 140, 694–698 (1986).
Msall, M. E., DiGaudio, K. M. & Duffy, L. C. Use of functional assessment in children with developmental disabilities. Phys. Med. Rehabil. North Am. Clinics 4, 517–527 (1993).
Voigt, R. G. et al. Concurrent and predictive validity of the cognitive adaptive test/clinical linguistic and auditory milestone scale (CAT/CLAMS) and the Mental Developmental Index of the Bayley Scales of Infant Development. Clin. Pediatr. 42, 427–432 (2003).
Rogers, B. et al. Cystic periventricular leukomalacia and type of cerebral palsy in preterm infants. J. Pediatr. 125, S1–S8 (1994).
Capone, G. T., Goyal, P., Grados, M., Smith, B. & Kammann, H. Risperidone use in children with Down syndrome, severe intellectual disability, and comorbid autistic spectrum disorders: a naturalistic study. J. Dev. Behav. Pediatr. 29, 106–116 (2008).
Rogers, B. T. et al. Neurodevelopmental outcome of infants with hypoplastic left heart syndrome. J. Pediatr. 126, 496–498 (1995).
Wachtel, R. C., Tepper, V. J., Houck, D., McGrath, C. J. & Thompson, C. Neurodevelopment in pediatric HIV infection. The use of CAT/CLAMS. Clinical Adaptive Test/Clinical Linguistic and Auditory Milestone Scale. Clin. Pediatr. 33, 416–420 (1994).
Hensch, T. K. & Bilimoria, P. M. Re-opening windows: manipulating critical periods for brain development. Cerebrum 2012, 11 (2012).
Capute, A. J. & Accardo, P. J. The infant neurodevelopmental assessment: a clinical interpretive manual for CAT-CLAMS in the first two years of life, part 1. Curr. Probl. Pediatr. 26, 238–257 (1996).
Acknowledgements
This project required a multidisciplinary network of developmental pediatricians, pediatric nurse practitioners, pediatric physical, occupational, and speech language therapists, early child educators, and community pediatricians. We are grateful to Nancy Lyon, Kim McKernan, and James Roistacher for community outreach and engagement. This study was supported by a grant from the Children’s Guild of Buffalo. M.E.M. is also funded in part by Leadership Education in Neurodevelopmental and Related Disorders Training Program (LEND)—Illinois T73 MC11047 HRSA/DHHS.
Author information
Authors and Affiliations
Consortia
Contributions
Each author has met the Pediatric Research author requirements. C.P., K.W., J.P., C.C., and M.E.M. contributed to conception and design, analysis and interpretation of data, and drafts of the manuscript. K.M., N.L., C.P.B., B.T.R., J.R., F.A.C., and M.E.M. contributed to acquisition of data. All the listed authors contributed to revising the article for intellectual content and all authors approved the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Informed consent was required for participation in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Peyton, C., Wroblewski, K., Park, J. et al. Validity of The Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA-FS): a daily activity criterion checklist for infants and toddlers. Pediatr Res 90, 1052–1057 (2021). https://doi.org/10.1038/s41390-020-01342-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01342-0