Abstract
Central pulse wave velocity (cPWV) is a biomarker for cardiovascular (CV) risk and a predictor for CV events in adulthood. Alterations of arterial stiffness have also been associated with CV risk in childhood. The study aimed to systematically review and meta-analyze the association of blood pressure (BP), body mass index (BMI), and cardiorespiratory fitness (CRF) with cPWV in children. Literature search was through the databases PubMed, Web of Science, Embase and the Cochrane Register of Controlled Trials. Twenty-two articles were included in the systematic review and eight articles in the meta-analysis. Higher systolic and diastolic BP were associated with higher cPWV (pooled estimated effect size (ES) 0.02 (95% CI: 0.012−0.027; P < 0.001), and ES 0.02 (95% CI: 0.011−0.029; P < 0.001); respectively). Higher BMI correlated with higher cPWV (ES 0.025 (95% CI: 0.013−0.038; P < 0.001)). CRF was inversely associated with cPWV (ES −0.033 (95% CI: −0.055 to −0.011; P = 0.002)). In children, higher BP and BMI are already related to increased cPWV, and enhanced CRF may be a preventive strategy to counteract development of CV disease later in life.
Impact
-
This meta-analysis suggests that elevated blood pressure and body mass index in childhood correlate with increased central pulse wave velocity.
-
Children with higher cardiorespiratory fitness appear to have favorably lower arterial stiffening.
-
Elevated blood pressure and altered arterial stiffness originate early in life and childhood risk stratification as well as timely initiation of exercise treatment may help counteract development of manifest cardiovascular disease later in life.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is a growing burden in adult life,1 but has its origin early in life.2,3 Cardiovascular (CV) risk factors are linked to premature structural and functional alterations of the arterial wall in childhood.4,5,6 Endothelial dysfunction and pre-arteriosclerosis manifests in childhood and may lead to clinical events such as myocardial infarction, stroke and sudden death in adulthood.3,7
The global age-standardized prevalence of obesity increased to 5.6% in boys and 7.8 % in girls over the last 40 years.8 The risk of having high blood pressure (BP) is more than three times higher with an increased body mass index (BMI) compared to children with normal weight.9 One kg/m2 greater BMI is associated with 1.4 mmHg higher systolic blood pressure (SBP) in prepubertal children.10 A major contributor for the development of CV risk factors in childhood is physical inactivity.11 Only 4.6% of the girls and 16.8% of the boys fulfill the recommendation of 60 min of moderate to vigorous physical activity (PA) per day.12 At the age of 10–12 years, 60% of the total waking hours are spent sedentary.13 Both physical inactivity and sedentary time are independent factors for the development of chronic diseases.14,15,16 These lifestyle-associated risk factors in childhood track into adulthood17,18 and are predictive for the development of future CV risk factors and manifest CVDs.3,4
The vascular tree consists of two functional components with different structural characteristics: the large central elastic arteries (aorta, carotid and femoral arteries) and the peripheral muscular arteries.19 Measurement of arterial stiffness is a promising surrogate macrovascular biomarker for CV risk with a reclassification rate of about 13% for future CV events and mortality in adults.20 An increase of 1 m/s of central pulse wave velocity (cPWV) results in a 15% higher risk of CV events and mortality, adjusted for age, sex and risk factors.20 The measurement of PWV in central segments, such as the often-used carotid-femoral segment, has the highest correlation with CVDs compared to measurements of peripheral segments, such as femoral-ankle or brachial-radial PWV.21,22 cPWV increases with age and has a strong linear and bivariate correlation with BP in adults. A recent meta-analysis in adults demonstrated that individuals with overweight or obesity exhibit a significant higher cPWV.23 Higher PA as well as cardiorespiratory fitness (CRF) have been associated with lower arterial stiffness in young adults independent of BMI.24 The findings on the association of classic and lifestyle-associated CV risk factors with central arterial stiffness in children are inconsistent. Furthermore, it is not known whether cPWV is a sensitive biomarker for macrovascular health in children and whether it is suitable for CV risk stratification and implementation in primary prevention strategies, as is the case in adults. We therefore conducted a first systematic review and meta-analysis on the association of BP, BMI, and CRF with cPWV in a childhood population.
Methods
This systematic review and meta-analysis is based on a systematic search conducted using the Guidelines for Preferred Reporting Items for systematic reviews and meta-analyses (PRISMA).25 The protocol was registered (CRD42018108286) on the international prospective register of systematic reviews (PROSPERO, www.crd.york.ac.uk/prospero) after preliminary searches.26
Inclusion and exclusion criteria
The inclusion criteria included the availability of full texts and the use of the English language. Studies were included if the associations of cPWV measured by tono- or oscillometric device, with BP, BMI, and/or CRF/PA were investigated. Objective measures of physical fitness were limited to aerobic performance. Evaluation of PA comprised subjective and objective measures. Studies that assessed acute effects or resistance training were excluded. The population of interest were children and adolescents aged 3−18 years without medication for CV risk factors and across all BP levels. Children were excluded if they were older than 18 years or had a history of treated or CV risk factors. School- and population-related cross-sectional data and baseline data of longitudinal studies were included if available.
Data source and study selection
A first electronic search through the databases of Pubmed, Web of Science, Embase and the Cochrane Register for Controlled Trials was conducted in July 2018 followed by a second search, 6 months later in January 2019. The search was based on a systematic search string. This consisted of keywords for the target population, which were combined with characteristic search terms of the predictors (BMI, BP, CRF). These were then paired with the descriptor search term being cPWV. The complete search string for the database PubMed and detailed review process can be found in the supplementary material (S1, S2). For each database, specific adjustments were made, without restrictions, based on the following search term:
(vascular stiffness OR arterial stiffness* OR vascular stiffness* OR aortic stiffness* OR pulse wave velocity) AND (child OR child* OR schoolchild* OR youth* OR adolescen* OR infant OR young people OR young OR teenage*) AND (obesity OR overweight OR BMI OR body mass index OR waist-to-hip ratio OR waist circumference OR body fat OR exercise OR physical fitness OR physical activity OR sport* OR physical education OR television viewing OR physical inactivity OR sedentary OR tv viewing OR fitness OR physical fitness OR cardiorespiratory fitness OR CV fitness OR training OR walking OR hypertension OR prehypertension OR blood pressure OR high blood pressure OR high-normal blood pressure OR pre-hyperten* OR hyperten*).
Data extraction form
The extraction form contained general information about the studies. Author, year of publication, country (city) in which the study was carried out and, if mentioned, the ethnicity of the participants. The number of subjects who underwent a valid cPWV measurement and the percentage of male sex were noted. In addition, the method of cPWV assessment was listed. For better structure and clarity, the studies were divided into groups on the basis of predictors (BP, BMI, CRF). Most importantly, the effects of the predictors on cPWV were also listed.
Quality and risk-of-bias assessment
The critical appraisal tool for cross-sectional studies (AXIS) was used to assess the risk of bias and quality. It consists of 20 questions with three possible answers (yes, no or don’t know).27 Two reviewers independently assessed the quality of each included study. In case of discrepancies, the discussion continued until a consensus was reached.
Statistical analysis
For the meta-analysis we extracted the unstandardized β coefficients of the linear regression models in which cPWV served as outcome and BMI, BP, CRF as predictors. The standard errors (SE) of the β coefficients were calculated by the standard deviations. If this information was not available, we assessed the SE through p values or confidence intervals (CI). Data with standardized β coefficients and SEs were back-transformed to the original scale. We used a random effects meta-analysis model for each cPWV measure. Heterogeneity between studies was assessed with standard χ2 tests and quantified using I2.29 Additionally, we calculated the predictive intervals, which describes the range of the predicted true treatment effect in a new study based on the included studies.30 A meta-regression was conducted to explain potential heterogeneity between the studies with BMI, SBP or DBP as predictor. A p value of 0.05 or lower was considered as statistically significant. All statistical analyses were performed using Stata Version 15.1.
Results
Meta-regression and heterogeneity
High heterogeneity was found for the studies on the association of cPWV and BMI (I2 = 89.2%), SBP (I2 = 82.1%), DBP (I2 = 86.1%), and CRF (I2 = 67%). Therefore, a meta-regression was conducted to evaluate inconsistency between the studies with BMI, SBP and DBP as well as CRF as predictors. We included age, percentage of boys, and sample size in the model to investigate heterogeneity. No association was found and thus heterogeneity was unexplained for remaining outcomes.
Quality and risk-of-bias assessment
The results of the quality and risk-of-bias assessment are shown in the last column of Tables 1–3. The detailed results are presented in supplementary material (S3). Data concerning the selection procedure of the subjects were inconsistent.30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50 The handling of nonresponders was not completely explained and the response rate as well as information on the nonresponders remained unclear.30,31,32,33,34,35,36,37,38,39,40,41,43,44,45,46,47,48,49,50,51 The overall rating of κ for the risk of bias between the raters was 0.92 (agreement of 95.91%).
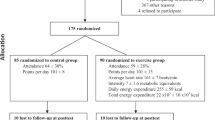
Study selection
The flowchart (Fig. 1) shows the detailed study selection. Twenty-two studies were included in the systematic review, 15 of them measured cPWV tonometrically (Compilor, SphygmoCor and PulseTrace) and seven by oscillometer (Mobil-O-Graph, Vicorder and Arteriograph). Of the 22 studies included in the systematic review,28,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51 eight reported a β coefficient for data pooling and were included in the meta-analysis.28,31,32,33,34,35,36,51 An overview of the included studies and participants is shown in Tables 1–3.
Blood pressure and central pulse wave velocity
Ten studies analyzed the association of SBP on cPWV. The sample size ranged from 81 to 1171. Eight studies reported that higher SBP was associated with higher cPWV (Table 1(a)).31,34,35,36,37,46,50,51 Six studies with a total of 2753 children and adolescents reported a β coefficient for the relationship of SBP with cPWV and were included in the meta-analysis.28,31,34,35,36,51 The pooled estimated ES of the association between SBP and cPWV was 0.02 (95% CI: 0.012−0.027, P < 0.001; predictive interval: −0.00 to 0.04; heterogeneity (I2) = 82.1%) (Fig. 2). To examine whether studies of low quality have influenced our result, we have excluded McCloskey et al.34 (AXIS 12/20) from the calculations, which did not change the results in terms of ES (∆ = +0.003) and heterogeneity (∆ = +2%).
The association of diastolic blood pressure (DBP) with cPWV was investigated in six studies (Table 1(b)).28,33,34,35,37,51 The sample size ranged from 138 to 1171 children and adolescents. Four studies found a positive correlation between DBP and cPWV.33,34,35,51 A total of five studies reported a β coefficient and were included in the meta-analysis.28,33,34,35,51 The association of DBP and cPWV resulted in a pooled estimated ES of 0.02 (95% CI: 0.01−0.03, P < 0.001; predictive interval: −0.01 to 0.05; heterogeneity (I2) = 86.1%) (Fig. 3). The recalculations without McCloskey et al. and Batista et al.33,34 showed no marked changes in effect (∆ < 0.01) size and heterogeneity (∆ = +4%).
Three of the studies included in the systematic review focused on 24-h-blood pressure and assessed group differences. Therefore, these three studies are listed separately in Table 1(c).
Litwin et al. analyzed the association between 24-h-BP and cPWV in children with high blood pressure. Children with a normal 24-h-BP had significantly lower cPWV compared to the group with severe hypertension. No differences between the pre-hypertensive, hypertensive and the control group with normal blood pressure were found.47 Tokgöz et al.49 revealed in their study that children with hypertension had an impaired cPWV compared to the control group. Wójtowicz et al. compared healthy controls to children with overweight and with overweight and hypertension. Both risk groups had significantly higher cPWV compared to the healthy pears, whereas the group with overweight and hypertension had the highest cPWV values.48
Body mass index and central pulse wave velocity
Thirteen studies with a total of 4854 participants investigated the relationship between BMI and cPWV in children and adolescents.28,32,33,34,35,36,38,39,40,41,42,43,51 The number of participants ranged from 19 to 1171. Seven studies showed that increased BMI was associated with increased cPWV (Table 2).32,33,35,40,42,43,51
Five studies with a total of 2767 children and adolescents reported a β coefficient for the association between BMI and cPWV and could be included in the meta-analysis.32,33,34,35,51 The pooled estimated ES of the association between BMI and cPWV was 0.025 (95% CI: 0.013−0.038, P < 0.001; predictive interval: −0.02 to 0.07; heterogeneity (I2) = 89.2%) (Fig. 4). No further analysis between the studies regarding quality differences was performed due to a limited number of included studies.
Cardiorespiratory fitness and central pulse wave velocity
Five studies investigated the association of objectively measured CRF and cPWV (Table 3).34,35,44,45,51 Three studies showed a significant inverse association of CRF with arterial stiffness,35,44,51 whereas two studies reported conflicting results45 and one study showed no evidence.34
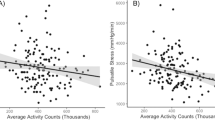
Only one study investigated the association of objectively measured daily PA (pedometer counts) with arterial stiffness. The number of counts correlated inversely with cPWV.35 One other study assessed the association of PA behavior with cPWV using subjective measures by use of a questionnaire. Köchli et al.51 found an association of physical inactivity (screen time) with cPWV which was, however, not independent of BMI and BP.
Only two of the above studies reported a β coefficient for the association of shuttle run stages with arterial stiffness and were included in the meta-analysis.35,51 The large differences in the method chosen to record CRF minimized comparability between the other studies. The pooled estimated ES for the association of CRF with cPWV in the above two studies was −0.033 (95% CI: −0.055 to −0.011, P = 0.002; heterogeneity (I2) = 67%). Since only two studies had the same outcome measure and were pooled, we refrained from performing forest plots for these.
Discussion
Our results imply that children with higher BP or BMI are characterized by increased arterial stiffness compared to children with normal BP and normal weight. Of note, children with higher CRF present with a favorably lower cPWV. Overall, the effect sizes may appear small; however, these findings are in young children with little lifetime exposure to CV risk.
We found a linear association of cPWV with SBP and DBP in children. The association of BP and cPWV in adults is a complex interaction between hemodynamic and mechanical patterns.52,53 It must be considered even more complex in children, where growth and childhood development as well as pubertal stages affect vascular structure and function. Nonetheless, in more than 2000 children aged 6–18 years included in the meta-analyses, we found that higher systolic and diastolic BP are significantly associated with a higher cPWV. Elevated BP has been shown to track into adulthood18 and childhood BP is considered an independent predictor for cPWV in adulthood.54,55 Most importantly, cPWV is considered an independent predictor for the longitudinal increase of SBP and incident hypertension.56,57 In the Cardiovascular Risk In Young Finns Study, individuals with persistently elevated BP from childhood to adulthood, and in those with normal child but elevated adult BP, have been shown to have increased risk of high arterial stiffness in adulthood.58 In conjunction with the findings of our meta-analysis, it appears to be of utmost importance to screen and control BP early in childhood as a primary prevention strategy to prevent manifestation of CVD later in life.
We also found a significant linear association between BMI and cPWV. In a previous meta-analysis in children and adolescents with obesity, Hudson et al.59 found moderate evidence for a higher cPWV in children with obesity compared to lean peers. Mean differences in cPWV were assessed in different arterial segments and variations between the regions were detected. Stiffer arteries in children with obesity were found specifically in central arteries such as the carotids and the aorta. The recently published follow-up of the ALSPAC Study assessed cPWV in late puberty. High-fat mass was independently associated with higher arterial stiffness during adolescence. No association between BMI and cPWV was found in the cross-sectional design. However, in the longitudinal follow-up, BMI and cPWV were significantly related and mostly explained by metabolic abnormalities.60 In our meta-analysis, findings on the association of BMI with cPWV are inconsistent, with moderate evidence for a linear association as indicated by the predictive interval. A potential explanation for the inconsistency of the association may be the assumption of an overall vasodilating effect as an adaptive mechanism of the vasculature to childhood obesity.60 Moreover, a premature nadir of arterial stiffness has been suggested due to accelerated growth and early onset of puberty.61 This may also explain the overall moderate evidence for our main finding on the association of BP with cPWV in children. Interestingly, our previous meta-analysis on the association of BP and BMI with retinal microvascular diameters in children showed strong evidence for a significant inverse correlation.62 Whether or not the microvascular bed may be more sensitive to changes in BP and BMI remains to be elucidated in future studies.
CRF and PA play a key role in child development and in the prevention of CV risk in childhood. Using pedometer counts as an objective measure of PA, Sakuragi et al.35 found that higher PA was associated with lower arterial stiffness. Objective measures of PA are likely to be more accurate in determining the association with arterial stiffening since questionnaire-based surveys suffer from under- as well as over-reporting. Five studies assessed the association of objectively measured CRF with cPWV.34,35,44,45,51 Two of the studies in the systematic review showed a significant association and one indicated a significant correlation of higher CRF with lower arterial stiffness.35,44,51 Meyer et al. found a positive association between the distance covered in 6 min and cPWV. Possible reasons for the divergent findings could be the method used to determine CRF and the age range (11–18 years) of the participants.45 Childhood growth and development during different stages of puberty and adolescence are dynamic and complex and are likely to affect vascular structure and function and associations with risk factors. From young adulthood onwards, there seems to be a significant and clearer association of higher CRF with lower arterial stiffness.63 In summary, the systematic review suggests an inverse association of CRF with arterial stiffness in younger, prepubertal children. These conclusions are supported by the meta-regression of two studies with the same outcome. An inverse correlation between CRF and cPWV is reported, with lower cPWV in fitter children. However, the results of Sakuragi et al.35 and Köchli et al.51 show that this association is not independent of BMI. Prospective long-term studies are warranted to investigate the efficacy of exercise interventions to improve vascular wall properties in children with high BP and BMI during childhood development.
Mechanisms for the early development of large artery stiffening include high-BP-induced mechanical stress inducing fragmentation of elastic lamellae and deposition of augmented collagen fibers in the vascular wall.64 The increased amount of collagen fibers in the tunica media and adventitia induces stiffening of the arteries and further increase in BP, which may evolve in a vicious cycle. It remains controversial which of the two, BP or arterial stiffening, is “chicken or egg”. In adults, there is some evidence that arterial stiffening may begin prior to the onset of hypertension.57 Some of the potential explanations for increased arterial stiffness in children with high BP also apply for children with obesity. Increased activity of the sympathetic nervous system in individuals with high BP and/or obesity alters the vascular tone and regulation of the arterial tree. The stimulation of the autonomic nervous system results in impaired arterial stiffness and elevated BP, although the exact underlying mechanism of how increased sympathetic nervous activity impairs arterial stiffening remain unexplained.65,66,67 Both, hypertension and obesity, are associated with a reduced bioavailability of nitric oxide (NO).68,69 Reduced NO availability is a precursor of endothelial dysfunction and may contribute to worsening of arterial stiffening.68 Most studies of this systematic review have differentiated between the associations of systolic and diastolic BP with cPWV. While these are, first and foremost, epidemiological findings, differential mechanisms may be debated. SBP represents peak mechanical stress in a pulsatile form, whereas DBP represents an underlying baseline stress for the vascular wall. Both, elevation of SBP and DBP, induce the above-mentioned mechanism whereby fragmentation of elastic lamellae and deposition of augmented collagen fibers in the vasculature are triggered. Isolated increased SBP leads to an increase in central pulse pressure (cPP), which is a key trigger for increased mechanical stress and vascular wall remodeling, and has been shown to increase the risk of CV events.20 Isolated increased DBP, on the other hand, lowers cPP and represents a lower pulsatile peak mechanical stress, however, at the cost of an increased underlying baseline stress.
The natural development of arterial stiffness during childhood also has to be taken into account. In children, a steady rise of PWV with age70 has been demonstrated, although a plateau in early childhood has been described.71 Regular physical activity lowers BP and thus reduces mechanical stress on the vascular system.72 Furthermore, PA and higher CRF mediate improved bioavailability of NO through repetitive higher shear stress,73,74 leading to improved endothelial function and lower peripheral resistance. Finally, regular PA and higher CRF have anti-inflammatory properties, with beneficial effects on vascular wall integrity.75,76
Our systematic review and meta-analysis have limitations. We included studies, which subjectively or objectively assessed PA behavior. Both methods have their advantages and disadvantages. Among others, subjectively assessed PA by questionnaires entail the risk of response and recall bias. On the other hand, objectively assessed PA by accelerometry does not provide standardized cutoff-values for children. Some of the studies of the systematic review included participants from an infantile age up to late adolescence.30,31,36,38,39,40,41,45,46 This wide age range makes it difficult to elaborate the association of arterial stiffness and CV risk factors in the different stages of child development. Age differences may be an explanation for the presence of high heterogeneity in our meta-analysis. A subgroup analysis could not be carried out due to the limited number of studies.77 We were not able to test funnel plot asymmetry because of insufficient test power to distinguish chance from asymmetry.78 Differences in the method and calibration of the devices used to assess central PWV, as well as the method used to determine the distance between carotid and femoral artery are additional reasons for the high heterogeneity between the studies and may further influence the accuracy of our results. All devices used in the studies were validated in adults against devices which have been used in prospective trials showing an independent prognostic value of cPWV (SphygmoCor) or against invasive stiffness assessment79 as recommended by the AHA80 and the Artery Society81 guidelines. The results of the conducted meta-analysis are of high value for primary prevention strategies of CVD but must be interpreted with caution due to differences in quality, pubertal stage, and high heterogeneity. There are several research gaps with respect to the clinical relevance of assessing arterial stiffness in children. The lack of validated devices for the determination of cPWV in children and insufficient normative and longitudinal data make it difficult to relate the prognostic value of cPWV to intermediate target organ endpoints in children. Moreover, there is an ongoing debate whether tonometric measurements of cPWV should be preferred over oscillometric measurements in adults. As can be seen from our systematic review in children, this debate also applies for measurements in children. In order to refurbish this debate and transfer it to childhood applications, more research is warranted. More high-quality studies, with more participants, standardized methods of measurement both with oscillometric and tonometric devices, taking into account potential cofounders and specific age categories, will strengthen our knowledge on the association of arterial stiffness and cardiovascular risk factors in childhood and will help to fill this gap.
This is the first meta-analysis providing an extensive overview on the association of cPWV with the three main childhood risk factors for the development of CVD later in life. Although the effect sizes are small, we showed that higher BP and BMI in children are already associated with impaired vascular wall integrity, as evident by an elevated cPWV. PA is associated with favorable vascular health and may be considered for future preventive intervention strategies in children with increased BP and BMI. Future research is warranted to elucidate whether cPWV is a potential vascular biomarker to improve CV risk stratification in children with predictive value for incidence CVD manifestation in adulthood.
References
World Health Organization. Global Status Report on Noncommunicable Diseases 2014 (WHO, Geneva, 2014).
Lavie, C. J., Milani, R. V. & Ventura, H. O. Obesity and cardiovascular disease. J. Am. Coll. Cardiol. 53, 1925–1932 (2009).
Berenson, G. Childhood risk factors predict adult risk associated with subclinical cardiovascular disease. The Bogalusa Heart Study. Am. J. Cardiol. 90, 3L–7L (2002).
Franks, P. W. & Bennett, P. H. Childhood obesity, other cardiovascular risk factors, and premature death. N. Engl. J. Med. 362, 485–493 (2010).
Bibbins-Domingo, K., Pletcher, M. J. & Goldman, L. Adolescent overweight and future adult coronary heart disease. N. Engl. J. Med. 357, 2371–2379 (2007).
Aggoun, Y. et al. Impaired endothelial and smooth muscle functions and arterial stiffness appear before puberty in obese children and are associated with elevated ambulatory blood pressure. Eur. Heart J. 29, 792–799 (2008).
Turoni, J. et al. Arterial stiffness and endothelial function in obese children and adolescents and its relationship with cardiovascular risk factors. Horm. Res. Paediatr. 80, 281–286 (2013).
NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
Sorof, J. M., Lai, D., Turner, J., Poffenbarger, T. & Portman, R. J. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics 113, 475–482 (2004).
Falaschetti, E. et al. Adiposity and cardiovascular risk factors in a large contemporary population of pre-pubertal children. Eur. Heart J. 31, 3063–3072 (2010).
Raitakan, O. T. et al. Effects of persistent physical activity and inactivity on coronary risk factors in children and young adults: The Cardiovascular Risk in Young Finns Study. Am. J. Epidemiol. 140, 195–205 (1994).
Verloigne, M. et al. Levels of physical activity and sedentary time among 10- to 12-year-old boys and girls across 5 European countries using accelerometers: an observational study within the ENERGY-project. Int. J. Behav. Nutr. Phys. Act. 9, 34 (2012).
Verloigne, M. et al. Patterns of objectively measured sedentary time in 10- to 12-year-old Belgian children: an observational study within the ENERGY-project. BMC Pediatr. 17, 147 (2017).
Ekelund, U. et al. TV viewing and physical activity are independently associated with metabolic risk in children: the European Youth Heart Study. PLoS Med. 3, e488 (2006).
Salmon, J., Dunstan, D. & Owen, N. Should we be concerned about children spending extended periods of time in sedentary pursuits even among the highly active? Int. J. Pediatr. Obes. 3, 66–68 (2008).
Janssen, I. & Leblanc, A. G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 7, 40 (2010).
Simmonds, M., Llewellyn, A., Owen, C. G. & Woolacott, N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis: adult obesity from childhood obesity. Obes. Rev. 17, 95–107 (2016).
Chen, X. & Wang, Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117, 3171–3180 (2008).
Kim, H.-L. & Kim, S.-H. Pulse wave velocity in atherosclerosis. Front. Cardiovasc. Med. 6, 41 (2019).
Vlachopoulos, C., Aznaouridis, K. & Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness. J. Am. Coll. Cardiol. 55, 1318–1327 (2010).
Tsuchikura, S. et al. Central versus peripheral arterial stiffness in association with coronary, cerebral and peripheral arterial disease. Atherosclerosis 211, 480–485 (2010).
Endes, S. et al. Associations of novel and traditional vascular biomarkers of arterial stiffness: results of the SAPALDIA 3 Cohort Study. PLoS ONE 11, e0163844 (2016).
Li, P., Wang, L. & Liu, C. Overweightness, obesity and arterial stiffness in healthy subjects: a systematic review and meta-analysis of literature studies. Postgrad. Med. 129, 224–230 (2017).
Fernberg, U., Fernström, M. & Hurtig-Wennlöf, A. Arterial stiffness is associated to cardiorespiratory fitness and body mass index in young Swedish adults: the Lifestyle, Biomarkers, and Atherosclerosis study. Eur. J. Prev. Cardiol. 24, 1809–1818 (2017).
PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4, 1 (2015).
Davies, S. The importance of PROSPERO to the National Institute for Health Research. Syst. Rev. 1, 5 (2012).
Downes, M. J., Brennan, M. L., Williams, H. C. & Dean, R. S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 6, e011458 (2016).
Stabouli, S. et al. Arterial stiffness and SBP variability in children and adolescents. J. Hypertens. 33, 88–95 (2015).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Egger, M., Smith, G. D. & Altman D. Systematic Reviews in Health Care Meta-Analysis in Context (John Wiley & Sons, New York, NY, 2013).
Stergiou, G. S. et al. Relationship of home blood pressure with target-organ damage in children and adolescents. Hypertens. Res. 34, 640–644 (2011).
Montero López, M. P. et al. Arterial stiffness and blood pressure in a multicultural child sample (Angola, Brazil, and Spain). Am. J. Hypertens. 32, 265–271 (2019).
Batista, M. S., Mill, J. G., Pereira, T. S. S., Fernandes, C. D. R. & Molina del, M. C. B. Factors associated with arterial stiffness in children aged 9-10 years. Rev. Saúde. Pública 49, 23 (2015).
McCloskey, K. et al. The effect of known cardiovascular risk factors on carotid-femoral pulse wave velocity in school-aged children: a population based twin study. J. Dev. Orig. Health Dis. 5, 307–313 (2014).
Sakuragi, S. et al. Influence of adiposity and physical activity on arterial stiffness in healthy children: the lifestyle of our kids study. Hypertension 53, 611–616 (2009).
Lurbe, E. et al. Blood pressure and obesity exert independent influences on pulse wave velocity in youth. Hypertension 60, 550–555 (2012).
Hvidt, K. N., Olsen, M. H., Holm, J.-C. & Ibsen, H. Obese children and adolescents have elevated nighttime blood pressure independent of insulin resistance and arterial stiffness. Am. J. Hypertens. 27, 1408–1415 (2014).
Garcia-Espinosa, V. et al. Peripheral and central aortic pressure, wave-derived reflection parameters, local and regional arterial stiffness and structural parameters in children and adolescents: impact of body mass index variations. High. Blood Press. Cardiovasc. Prev. 25, 267–280 (2018).
Caterini, J. E. et al. Magnetic resonance imaging reveals elevated aortic pulse wave velocity in obese and overweight adolescents: MRI assessment of vascular function in obesity. Clin. Obes. 7, 360–367 (2017).
Kulsum-Mecci, N. et al. Effects of obesity and hypertension on pulse wave velocity in children. J. Clin. Hypertens. 19, 221–226 (2017).
Hacıhamdioğlu, B. et al. Preperitoneal fat tissue may be associated with arterial stiffness in obese adolescents. Ultrasound Med. Biol. 40, 871–876 (2014).
Correia-Costa et al. Determinants of carotid-femoral pulse wave velocity in prepubertal children. Int. J. Cardiol. 218, 37–42 (2016).
Pierce, G. L. et al. Arterial stiffness and pulse-pressure amplification in overweight/obese African-American adolescents: relation with higher systolic and pulse pressure. Am. J. Hypertens. 26, 20–26 (2013).
Vogrin, B., Slak Rupnik, M. & Mičetić-Turk, D. Increased augmentation index and central systolic arterial pressure are associated with lower school and motor performance in young adolescents. J. Int. Med. Res. 45, 1892–1900 (2017).
Meyer, J., Elmenhorst, J., Giegerich, T., Oberhoffer, R. & Müller, J. Controversies in the association of cardiorespiratory fitness and arterial stiffness in children and adolescents. Hypertens. Res. 40, 675–678 (2017).
Lurbe, E., Torro, M. I., Alvarez-Pitti, J., Redon, P. & Redon, J. Central blood pressure and pulse wave amplification across the spectrum of peripheral blood pressure in overweight and obese youth. J. Hypertens. 34, 1389–1395 (2016).
Litwin, M., Obrycki, Ł., Niemirska, A., Sarnecki, J. & Kułaga, Z. Central systolic blood pressure and central pulse pressure predict left ventricular hypertrophy in hypertensive children. Pediatr. Nephrol. 34, 703–712 (2019).
Wójtowicz, J. et al. Central aortic pressure, arterial stiffness and echocardiographic parametersof children with overweight/obesity and arterial hypertension. Adv. Clin. Exp. Med. 26, 1399–1404 (2017).
Tokgöz, S. T., Yılmaz, D., Tokgöz, Y., Çelik, B. & Bulut, Y. The evaluation of arterial stiffness of essential hypertension and white coat hypertension in children: a case-control study. Cardiol. Young-. 28, 403–408 (2018).
Mir, S. M. et al. Cardiovascular functional and structural changes in children with primary hypertension. Minerva Pediatr. 68, 27–35 (2016).
Köchli, S. et al. Obesity, high blood pressure, and physical activity determine vascular phenotype in young children: the EXAMIN YOUTH study. Hypertension 73, 153–161 (2019).
AlGhatrif, M. & Lakatta, E. G. The conundrum of arterial stiffness, elevated blood pressure, and aging. Curr. Hypertens. Rep. 17, 12 (2015).
Mitchell, G. F. Arterial stiffness and hypertension: chicken or egg? Hypertension 64, 210–214 (2014).
Li, S., Chen, W., Srinivasan, S. R. & Berenson, G. S. Childhood blood pressure as a predictor of arterial stiffness in young adults: the Bogalusa Heart study. Hypertension 43, 541–546 (2004).
Aatola, H. et al. Lifetime risk factors and arterial pulse wave velocity in adulthood: the Cardiovascular Risk in Young Finns study. Hypertension 55, 806–811 (2010).
Najjar, S. S. et al. Pulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the Baltimore Longitudinal Study of Aging. J. Am. Coll. Cardiol. 51, 1377–1383 (2008).
Kaess, B. M. et al. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 308, 875 (2012).
Aatola, H. et al. Influence of child and adult elevated blood pressure on adult arterial stiffness: the Cardiovascular Risk in Young Finns Study. Hypertension 70, 531–536 (2017).
Hudson, L. D., Rapala, A., Khan, T., Williams, B. & Viner, R. M. Evidence for contemporary arterial stiffening in obese children and adolescents using pulse wave velocity: a systematic review and meta-analysis. Atherosclerosis 241, 376–386 (2015).
Dangardt, F. et al. Association between fat mass through adolescence and arterial stiffness: a population-based study from The Avon Longitudinal Study of Parents and Children. Lancet Child Adolesc. Health 3, 474–481 (2019).
Tryggestad, J. B., Thompson, D. M., Copeland, K. C. & Short, K. R. Obese children have higher arterial elasticity without a difference in endothelial function: the role of body composition. Obesity 20, 165–171 (2012).
Köchli, S., Endes, K., Infanger, D., Zahner, L. & Hanssen, H. Obesity, blood pressure, and retinal vessels: a meta-analysis. Pediatrics 141, e20174090 (2018).
Boreham, C. et al. Cardiorespiratory fitness, physical activity, and arterial stiffness. Hypertension 44, 721–726 (2004).
Chirinos, J. A., Segers, P., Hughes, T. & Townsend, R. Large-artery stiffness in health and disease. J. Am. Coll. Cardiol. 74, 1237–1263 (2019).
Aroor, A. R., Jia, G. & Sowers, J. R. Cellular mechanisms underlying obesity-induced arterial stiffness. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 314, R387–R398 (2018).
Thorp, A. A. & Schlaich, M. P. Relevance of sympathetic nervous system activation in obesity and metabolic syndrome. J. Diabetes Res. 2015, 1–11 (2015).
DeMarco, V. G., Aroor, A. R. & Sowers, J. R. The pathophysiology of hypertension in patients with obesity. Nat. Rev. Endocrinol. 10, 364–376 (2014).
Hermann, M., Flammer, A. & Lscher, T. F. Nitric oxide in hypertension. J. Clin. Hypertens. 8, 17–29 (2006).
Montero, D., Walther, G., Perez-Martin, A., Roche, E. & Vinet, A. Endothelial dysfunction, inflammation, and oxidative stress in obese children and adolescents: markers and effect of lifestyle intervention: endothelial dysfunction in childhood obesity. Obes. Rev. 13, 441–455 (2012).
Elmenhorst, J. et al. Percentiles for central blood pressure and pulse wave velocity in children and adolescents recorded with an oscillometric device. Atherosclerosis 238, 9–16 (2015).
Hidvégi, E. V. et al. Reference values of aortic pulse wave velocity in a large healthy population aged between 3 and 18 years. J. Hypertens. 30, 2314–2321 (2012).
Whelton, S. P., Chin, A., Xin, X. & He, J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 136, 493–503 (2002).
Ashor, A. W., Lara, J., Siervo, M., Celis-Morales, C. & Mathers, J. C. Effects of exercise modalities on arterial stiffness and wave reflection: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE 9, e110034 (2014).
Schuler, G., Adams, V. & Goto, Y. Role of exercise in the prevention of cardiovascular disease: results, mechanisms, and new perspectives. Eur. Heart J. 34, 1790–1799 (2013).
Kasapis, C. & Thompson, P. D. The effects of physical activity on serum C-reactive protein and inflammatory markers: a systematic review. J. Am. Coll. Cardiol. 45, 1563–1569 (2005).
Montero, D., Walther, G., Perez-Martin, A., Roche, E. & Vinet, A. Endothelial dysfunction, inflammation, and oxidative stress in obese children and adolescents: markers and effect of lifestyle intervention. Obes. Rev. J. Int. Assoc. Study Obes. 13, 441–455 (2012).
Fu, R. et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the Effective Health Care Program. J. Clin. Epidemiol. 64, 1187–1197 (2011).
Sterne, J. A. C. et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343, d4002 (2011).
Milan, A. et al. Current assessment of pulse wave velocity: comprehensive review of validation studies. J. Hypertens. 37, 1547–1557 (2019).
Townsend, R. R. et al. Recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement from the American Heart Association. Hypertension 66, 698–722 (2015).
Wilkinson IB et al. ARTERY Society guidelines for validation of non-invasive haemodynamic measurement devices: Part 1, arterial pulse wave velocity. Artery Res. 4, 34 (2010).
Author information
Authors and Affiliations
Contributions
G.L., C.H., S.K., D.I., K.E. and H.H. made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. G.L., C.H., A.S.-T. and H.H. drafted the article or revising it critically for important intellectual content. H.H. approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lona, G., Hauser, C., Köchli, S. et al. Association of blood pressure, obesity and physical activity with arterial stiffness in children: a systematic review and meta-analysis. Pediatr Res 91, 502–512 (2022). https://doi.org/10.1038/s41390-020-01278-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01278-5
This article is cited by
-
Relationship between adiponectin and blood pressure in obese Latino adolescent boys with a family history of type 2 diabetes
BMC Pediatrics (2023)
-
Blood pressure parameters affecting ventricular repolarization in obese children
Pediatric Nephrology (2023)