Abstract
Background
With high survival rates for pediatric acute lymphoblastic leukemia (ALL), long-term quality of life is a prominent consideration in treatment. We concurrently evaluated cognition, behavior, and quality of life in child and adolescent ALL survivors and determined associations between them.
Methods
The sample included 83 controls (mean age: 12.5 years) and 71 ALL survivors (mean age: 11.9 years, mean age at diagnosis: 3.8 years). Participants completed measures of general intellectual abilities, math achievement, and fine motor skills. Parents and teachers completed a survey assessing child participants’ cognitive, behavioral, and emotional function. Parents additionally completed a survey about their child’s quality of life.
Results
Survivors had lower scores on measures of working memory, processing speed, timed math, and fine motor skills (effect size 0.5–1, p < 0.001). Parents identified more problems with executive function and learning in survivors than controls (effect size > 0.7, p < 0.001), and indicated a lower quality of life in all categories evaluated (effect size > 0.7, p < 10−4). Reduced quality of life was associated with lower math achievement scores and with inattention and executive function problems.
Conclusions
ALL survivors experience diffuse cognitive, behavioral, and motor impairments, which are associated with reduced quality of life. These findings underscore the need to address these challenges in ALL survivors.
Impact
-
Compared with cancer-free peers, parents of childhood acute lymphoblastic leukemia survivors treated with chemotherapy only reported reduced quality of life. Math difficulties and behavioral problems increased the risk for reduced quality of life.
-
Reduced quality of life is associated with mild cognitive and behavioral difficulties, suggesting that even relatively mild impairments have broad implications for ALL survivors.
-
Screening and early intervention targeting cognitive and behavioral function may enhance quality of life for ALL survivors.
Similar content being viewed by others
Introduction
Pediatric acute lymphoblastic leukemia (ALL), the most common childhood cancer, typically manifests between 2 and 5 years of age.1 Contemporary treatments involve combination chemotherapy administered in phases across 2–3 years, achieving 5-year survival rates that now exceed 90%.1 However, ALL survivors are at risk of developing difficulties in later life that affect cognitive function, such as impairments in working memory, processing speed, attention, executive function, and motor coordination.2,3,4,5,6,7,8 These difficulties may affect academic progress, and vocational and social success,9,10,11,12 and may have implications for quality of life.13
Health-related quality of life (HRQL)—the subjective perception of health and well-being—can be affected from the time of leukemia treatment through long-term survivorship. In their systematic review, Fardell et al.14 reported consensus across several studies showing that HRQL, encompassing physical, psychological, and social functioning, is significantly reduced in ALL patients during treatment. While HRQL for ALL patients has been reported to improve over the course of chemotherapy treatment, some reports suggest that low HRQL can continue into survivorship.14,15 Using the Pediatric Quality of Life Inventory (PedsQL), a widely used tool for evaluating HRQL in pediatric populations, Kunin-Batson et al.13 found that HRQL in survivors averaging 9 years since diagnosis was consistent with previously published population norms, but that problems with verbal cognitive abilities and visual-motor integration were associated with reduced physical and psychosocial HRQL. However, survivors in this study were treated on protocols administered between 1993 and 2000.16,17 Treatment protocols continue to evolve, and cognitive and behavioral outcomes may change as a function of these adjustments; ongoing evaluation of quality of life in survivors and associated outcomes is needed. Additionally, quality of life in previous work was compared to normative data ascertained a decade prior.13,18 Inclusion of contemporaneous typically developing peers enables comparison of quality of life among individuals in a similar societal context. Since interventions have the potential to alter cognitive and behavioral morbidities,19 elucidation of associations between cognitive difficulties and HRQL provides opportunities to improve long-term HRQL among ALL survivors.
The purpose of this study was to evaluate cognition, behavior, and HRQL concurrently in late childhood and adolescent ALL survivors and in a contemporaneous group of typically developing peers. We collected a variety of outcome measures to assess cognitive and behavioral function, including performance-based and proxy-rated measures. Our first goal was to compare functional abilities and HRQL of ALL survivors with typically developing peers and with published norms. The second goal was to examine associations between neuropsychological, proxy-reported, and HRQL outcomes.
Methods
Participants
ALL survivors were recruited for this study through a parent study, which was conducted at the Hospital for Sick Children to evaluate cognitive abilities, genetic variation, and nutrition in ALL survivors.3 Eligible survivors were recruited for the two studies simultaneously through contact in clinic during a follow-up visit or, for individuals who had previously participated in the parent study, approached through a mailed research invitation letter followed by a phone call. Measures common between studies included: performance-based assessments of intelligence, academic achievement and fine motor skills, as well as parent-rated assessments of behavior. Additional measures completed for this study, included assessment of HRQL, and teacher ratings of behavioral problems and learning deficits. For 89% of participants, all tests were completed on the same day. The remaining 11% completed all new assessments within a maximum of 12 months.
ALL participants were eligible to participate if they: (1) received a primary diagnosis of ALL between 1 and 10 years of age; (2) were treated with chemotherapy only (no cranial radiation or bone marrow transplant) at the Hospital for Sick Children; (3) had not received ALL treatment for a period of at least 2 years; (4) had not been diagnosed with Down syndrome; (5) were not currently taking psychoactive medication; (6) did not have a history of head trauma requiring a hospital stay; and (7) were 8–18 years old at evaluation. These criteria matched those of the parent study, except participants were additionally required to have no magnetic resonance imaging (MRI) contraindications due to neuroimaging analyses conducted as part of companion work.20 Figure 1 summarizes the selection of participants. To quantify chemotherapy exposure in ALL survivors, we conducted a complete chart review and extracted total cumulative dose for a number of chemotherapy agents. Complete dose data were available for 64 of 71 ALL participants (90%).
Survivors were drawn from a pool of participants initially enrolled in another study (N-PhenoGENICS). In companion work, we also planned neuroimaging for the same patients, so MRI contraindications were considered additional exclusion criteria. This resulted in a total of 155 individuals that were considered eligible for the present study. Recruitment was planned for approximately half of them.
A group of typically developing controls (CTL) was recruited by posting advertisements on hospital message boards. These participants and their caregivers completed the same performance-based and questionnaire measures as the ALL survivor group. CTL participants were eligible to participate if they had not been previously diagnosed with a neurodevelopmental disorder, had no history of serious head trauma, were not currently taking psychoactive medication, were between 8 and 18 years old, and had no MRI contraindications.
All procedures and study-related communications with participant families were conducted in accordance with a written protocol approved by the Hospital for Sick Children’s Research Ethics Board. Informed consent was obtained from all participants, and/or their parents/guardians. Assent was obtained from participants considered too young or otherwise unable to provide informed consent.
Demographics and clinical information
On the day of testing, parents of participants completed a brief survey about basic health and demographic information, including child date of birth (to calculate age), sex, and ethnicity. Ethnic background was determined based on the self-reported background of biological grandparents. To verify eligibility as determined at the time of screening, the survey also included items about history of mental health, head trauma, and current psychoactive medications. Clinical information specific to ALL, including date of diagnosis, treatment protocol, and cumulative dose of chemotherapy agents, were obtained by review of medical charts. A subset of participants also provided parent educational attainment and occupation information. Reported occupations were classified by the Canadian National Occupational Classification (NOC) system and subsequently used to generate NOC Income Scores, which are indicative of average income percentile for an occupation as measured against the Canadian population.21
Performance-based measurements
General cognitive abilities were assessed using the Wechsler Intelligence Scale for Children IV (WISC).22 Participants who were 17 or older (5 ALL, 6 CTL) completed the Wechsler Adult Intelligence Scale IV (WAIS).23 Age-adjusted standard scores for Verbal Comprehension, Perceptual Reasoning, Working Memory, and Processing Speed were compared across groups. Math was assessed using subtests of the Wechsler Individual Achievement Test III (WIAT),24 including numerical operations, math problem solving, addition fluency, subtraction fluency, and multiplication fluency.
Fine motor speed and dexterity were evaluated using the Grooved Pegboard Test,25 in which participants insert keyed pegs into slots (once each with the dominant and nondominant hand). Completion times, converted to z-scores, were taken as the primary outcome measure.
Parent- and teacher-rated measurements
Parents/guardians completed a series of questionnaires about participant’s behavior and perceived HRQL. Symptoms of inattention and hyperactivity were characterized using the Conners-3 parent-rating scale (Pearson).26 Parents/guardians were also given the Conners-3 teacher-rating questionnaire to be completed by the child’s teacher. HRQL was assessed using the PedsQL parent-proxy report (using the Generic Core Scales),18,27 which consists of 23 questions related to physical, emotional, social, and school functioning. PedsQL summary scores for each of these areas are produced by summing the Likert scale responses of associated questions. The discretized summed score is subsequently scaled to range between 0 (low HRQL) and 100 (high HRQL).27 Where utilized, predetermined cut-off scores for the PedsQL to categorize low versus normal HRQL were based on references established by other authors and were taken to be 63.28, 63.29, 62.07, and 56.75 for physical, emotional, social, and school scales, respectively.13,18
Statistical analysis
All statistical analyses were completed using the R statistical computing package (version 3.6).28 Demographic data were compared between groups based on a two-sample t test (for average age) and tests of equal proportions (for sex, ethnicity, and handedness). Cumulative dose of chemotherapy agents, where noted, were compared by a Mann−Whitney U test. For visualization in plots, confidence intervals were generated by bootstrap sampling, using minimum 500 draws and allowing replacement.
Linear regression models were used to fit WISC, WIAT, pegboard, and Conners outcome measures. Ordinal logistic regression was conducted to fit PedsQL outcome measures,29 taking the ordinal levels to be set by the discretization of each PedsQL scale (3.125 points for the Physical scale and 5 points for the Emotional, Social, and School scales). Explanatory variables for the models included age, age at diagnosis, sex, group assignment (e.g., CTL versus ALL), and age-group and sex-group interactions. The fixed effect for age was omitted for models where outcome variables were already standardized for age (i.e., WISC, WIAT). All statistical tests were two sided. The false discovery rate was applied to control false positives due to multiple comparisons. The computed q values were reported to convey significance.
To evaluate factors associated with impaired HRQL outcomes, cognitive and behavioral measures and their interactions with group assignment (CTL vs. ALL) were added as explanatory variables (in addition to those listed above) in the ordinal logistic regression models for PedsQL scores. In all analyses, results were considered statistically significant at p < 0.05 or q < 0.10.
Results
Study sample
The sample included 83 typically developing controls (CTL) and 71 ALL survivors (ALL; 46% of eligible population). Sample characteristics are summarized in Table 1. The average age at evaluation was 12.2 years (SD = 2.8 years, range 8.0–18.1 years). The groups did not differ significantly from each other on age at evaluation (p = 0.25), distribution of sex (p = 0.6), or ethnicity (p = 0.28). ALL survivors were on average 3.8 years old at diagnosis (SD = 1.7 years), and an average of 8.1 years (SD = 2.5 years) had elapsed between the time of diagnosis and time of evaluation. Cumulative chemotherapy exposures across ALL survivors were considered homogeneous, although sex differences were apparent. For example, cumulative dexamethasone and vincristine doses were higher in males (median [interquartile range] = 1280 [680] and 70 [21] mg/m2, respectively) than females (890 [615] and 52 [7.8] mg/m2) due to a longer treatment period (p = 0.00002 and 0.0003 by a Mann−Whitney U test). A complete summary of dose information is provided in Supplementary Materials (Supplementary Figs. 1 and 2).
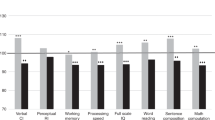
Cognitive function
Compared with the CTL group, the ALL survivor group scored significantly lower across all indices of the WISC/WAIS (Fig. 2a and Supplementary Table 1). The average score for the ALL group was considered within the normal limits for the Verbal Comprehension Index (VCI, mean = 102; 95% CI 100–106) and the Perceptual Reasoning Index (PRI, mean = 97, 95% CI 93–101). ALL mean scores for Working Memory Index (WMI, mean = 93, 95% CI 90–96) and Processing Speed Index (PSI, mean = 90, 95% CI 87–94) indicated poorer performance compared to average CTL scores, 101 (95% CI 98–104) and 105 (95% CI 103–108) respectively. The average WMI and PSI scores, though in the normal range for an individual, were also considered low compared to population norms (100 with standard deviation 15) for a group of this size. With reference to norms, the effect size was estimated to be −0.5 and −0.7 for WMI and PSI, respectively (represented as difference in means, in units of standard deviation). The WISC/WAIS scores were consistent with expectations from a previous report from the parent study.3
For each plot, group membership is shown on the x-axis and scores are listed on the y-axis. Mean scores are represented by a horizontal line and error bars represent 95% confidence limits for the means. Each circle represents results for an individual participant. WISC/WAIS indices (panel a) and WIAT subscales (panel b) are shown at the bottom of each plot. VCI Verbal Comprehension Index, PRI Perceptual Reasoning Index, WMI Working Memory Index, PSI Processing Speed Index, Num. op. Numerical Operations, Prob. solv. Math Problem Solving, Fl. add. Fluency: Addition, Fl. sub. Fluency: Subtraction, Fl. mul. Fluency: Multiplication.
Assessment of the WIAT math subscales also indicated poor performance in the ALL group relative to the CTL group (Fig. 2b and Supplementary Table 1), with the most extreme difference observed in Multiplication Fluency, ALL mean score = 89 (95% CI 85–92) versus CTL mean score = 102 (95% CI 100–105). The ALL group was significantly slower than the CTL group in completing the Grooved Pegboard task, indicating poorer fine motor skills (averaging 0.9 std. dev. less than CTL across both hands, q < 0.001, Supplementary Table 1).
Behavioral function
Parent-rated assessments of behavioral problems indicated elevated levels of inattention, learning problems, executive function problems, and difficulties in peer relations in the ALL group relative to CTL and to population norms (Fig. 3 and Supplementary Table 1), with attention deficits and learning problems most prominently elevated. Teacher forms were returned for 77% of the sample (118/154; 66 CTL and 52 ALL). When compared with population norms, teachers indicated that ALL survivors exhibited mild elevations across all categories but defiance-aggression. When compared with the CTL group, ALL teacher scores were statistically different only for learning problems/executive function (q < 0.1). Parent and teacher ratings were globally correlated within participants (Fig. 3c, d and Supplementary Fig. 3A, B), with the exception of the defiance-aggression and peer relations scales (Supplementary Fig. 3C, D). Parent scores showed greater deviation from population norms than corresponding teacher scores, similar to other observations.30,31
Proxy scores from parents (a) and teachers (b) are shown on the y-axis across groups (x-axis). Mean scores are represented by a horizontal line and error bars represent 95% confidence limits of the means. Each circle represents a single observation. Associations between parent ratings (x-axis) and teacher ratings (y-axis) for learning problems and executive function are shown in panels (c) and (d), respectively. Inatten. Inattention, Hyper. Imp. Hyperactivity/Impulsivity, Learn. Prob. Learning Problems, Exec. Func. Executive Functioning, Def.Agg. Defiance/Aggression, Peer Rel. Peer Relations, Learn. Exec. Learning Problems/Executive Functioning.
Health-related quality of life
ALL survivors were more likely to have low HRQL scores than CTL participants across all PedsQL items and categories (Fig. 4). Using previously defined cut-offs,13,18 the proportions of ALL participants with low HRQL were 29%, 37%, 26%, and 39% for the physical, emotional, social, and school scores, respectively (as compared to 2, 11, 2, and 6% in the CTL group). A total of 51% of ALL participants fell below threshold on at least one of the four scales (versus 17% in the CTL group). ALL survivor HRQL was not found to depend on parental educational attainment or NOC occupational income scores (Supplementary Figs. 4 and 5).
Panels show physical (a), emotional (b), social (c) and school (d) quality of life scores. PedsQL scores were binned for display (x-axis), including 5 possible scores per bin. The y-axis lists proportions of the group in each score range from 0 to 1. Within each panel, the distribution of scores is represented in bar graphs for the CTL group and the ALL survivor group separately. The third stacked bar graph shows the proportion of individuals (y-axis) across groups (x-axis) who had scores that were indicative of low QoL (dark gray) or normal/high QoL (light gray). Error bars indicate 95% confidence intervals obtained by bootstrap sampling.
Associations between cognition, behavior and HRQL
Conners-3 parent scores and performance-based WIAT math results were significantly associated with parent-rated HRQL. Elevated scores on all Conners-3 items, which indicates poorer performance, were significantly associated with lower HRQL score in each domain of the PedsQL (Fig. 5). Math performance, including problem solving, addition, subtraction, and multiplication, was positively associated with physical, social, and school HRQL.
Each plot shows odds ratios (x-axis) between cognitive/behavioral variables listed on the y-axis and each domain of the PedsQL (title bar). The vertical line marks an odds ratio of 1, i.e., no significant association. Error bars represent 95% confidence limits determined by bootstrap resampling. For display purposes, the scale was adjusted so that impairment on the predictor score (indicated in rows) was associated with a poorer QoL if the odds ratio was positive (independent of the original directionality). The odds ratio was derived from the ordinal logistic regression results, and is expressed for a one unit change in the predictor.
Discussion
As a group, ALL survivors treated with chemotherapy only exhibited mild, but numerous cognitive and behavioral impairments relative to cancer-free peers. They also experienced reduced HRQL, with approximately 50% of survivors falling below the threshold on at least one of the domains assessed as part of the PedsQL. HRQL was most affected in the domain of school function: over 40% of ALL survivor parents expressed a high level of concern over their child’s school HRQL, relative to <10% of parents of children without a history of cancer. Math performance and parent-rated behavioral problems, including inattention, executive dysfunction and difficulties with peer relations, increased risk for poor HRQL across domains. Thus, although deficits are relatively mild overall, it appears that their combination may have significant implications for HRQL among survivors.
Inattention, executive function, and math achievement exhibited the strongest associations with perceived HRQL in our school age sample. The link between behavioral problems and HRQL was particularly notable. The strength of this association must be viewed cautiously because it is likely attributable, at least in part, to ‘common source bias’ (i.e., both the Conners and PedsQL surveys were completed by the same parent). However, the parent ratings were corroborated by other results31: teachers identified more learning problems and executive dysfunction in ALL survivors relative to cancer-free peers, with correlations to parent ratings; and performance-based measures of math skills, processing speed, and working memory also identified difficulties, with correlations to parent ratings of cognitive/behavioral difficulties and associations with HRQL outcomes. Parent-proxy reports will remain an important source of information for evaluating abilities and HRQL in children and adolescents,32 and provide a different perspective of a child’s behavior based on environment and availability of peer comparisons.31 Overall, our results suggest that cognitive and behavioral problems in survivors may be linked with broadly impaired HRQL. This interpretation is in line with previous work in adult survivors of childhood cancer, which showed that cognitive impairment is associated with reduced social attainment.33,34
Consequently, ameliorating cognitive and neurobehavioral problems in ALL survivors may have a positive impact on HRQL. Potentially effective interventions to address cognitive and behavioral deficits include cognitive training programs targeted at strengthening working memory skills,19,35 or stimulant medication to address attention deficits.36 Several studies in childhood cancer survivors showed that individuals who completed a computerized training module exhibited better working memory and fewer behavioral problems than did individuals who did not complete training.19,37 Others showed that methylphenidate medication may be beneficial for addressing attention deficits in childhood cancer survivors.36,38,39 Further research is needed to determine whether cognitive/behavioral improvements also lead to corresponding improvements in HRQL.
There are several factors that may influence HRQL that we were not able to consider in our evaluations. First, socio-economic characteristics generally affect quality of life40 and prior research in ALL survivors showed that lower household income was associated with poor physical HRQL.13 Moreover, cancer diagnosis in children can significantly affect parental income,41 so that the interaction of socio-economic status and quality of life (or other outcome measures) is complex in children with significant health conditions such as childhood cancer. We did not evaluate household income or parental history of employment prior to ALL diagnosis. While we found no relationship between maternal and paternal educational attainment or NOC income scores and HRQL outcomes in ALL survivors, it will be important to understand the significance of parental employment/income changes on HRQL in future studies. Second, our analysis did not consider the potential impact of treatment characteristics on HRQL. While we did determine cumulative exposures for survivors with the intention of exploring this relationship, the distribution of doses was determined to be very homogeneous, precluding meaningful inferences about the impact of chemotherapy dose on other outcomes. A systematic review reported little impact of treatment factors on HRQL in ALL survivors.42 Larger samples that include a spectrum of treatment protocols would be required to elucidate the impact of treatment factors on long-term HRQL. Third, we did not obtain self-report measures of HRQL. In past work, the PedsQL 4.0 Generic Scale exhibited moderate to good agreement between parent-proxy and self-report scales for children between 5 and 16 years old.32 Overall, however, ALL survivors exhibited difficulties in performance-based, teacher-, and parent-rated measurements, boosting confidence in the HRQL ratings provided by parents. Fourth, while most participants completed all assessments in a single day, 11% of the survivor sample completed assessments over multiple hospital visits, which may affect study results and the associations reported. Fifth, generalization of our findings will need to be evaluated since survivors were recruited at a single institute and only sampled part of the survivor population. In this context, we highlight that our findings are in line with a previous study from Kunin-Batson et al.13 that included survivors from different sites. Finally, the cross-sectional nature of the study prevents us from drawing conclusions about how HRQL may change over time.
Conclusion
Cognitive, academic, and behavioral difficulties, while mild, are widespread among ALL survivors treated with chemotherapy only. These impairments appear to have broad implications for quality of life. Additional research on quality of life in survivors will require prospective, longitudinal studies to determine how HRQL evolves through survivorship and expanded consideration of the role of sociodemographic factors, including changes resulting from ALL diagnosis. Early detection of and intervention for cognitive and/or behavioral deficits may be imperative for ultimately improving HRQL outcomes in survivors.
References
Howlader, N. et al. National Cancer Institute SEER Cancer Statistics Review 1975−2014 (National Cancer Institute, Bethesda, MD, 2017).
Cheung, Y. T. & Krull, K. R. Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neurosci. Biobehav. Rev. 53, 108–120 (2015).
van der Plas, E. et al. Characterizing neurocognitive late effects in childhood leukemia survivors using a combination of neuropsychological and cognitive neuroscience measures. Child Neuropsychol. 24, 999–1014 (2018).
Iyer, N. S., Balsamo, L. M., Bracken, M. B. & Kadan-Lottick, N. S. Chemotherapy-only treatment effects on long-term neurocognitive functioning in childhood ALL survivors: a review and meta-analysis. Blood 126, 346–353 (2015).
Jacola, L. M. et al. Cognitive, behavior and academic functioning in adolescent and young adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. Lancet Psychiatry 3, 965–972 (2016).
Jacola, L. M. et al. Longitudinal assessment of neurocognitive outcomes in survivors of childhood acute lymphoblastic leukemia treated on a contemporary chemotherapy protocol. J. Clin. Oncol. 34, 1239–1247 (2016).
Liu, W. et al. Evolution of neurocognitive function in long-term survivors of childhood acute lymphoblastic leukemia treated with chemotherapy only. J. Cancer Surviv. 12, 398–406 (2018).
Godoy, P. B. G., Simionato, N. M., de Mello, C. B. & Suchecki, D. Assessment of executive functions after treatment of childhood acute lymphoid leukemia: a systematic review. Neuropsychol. Rev. 30, 386–406 (2020).
Lofstad, G. E., Reinfjell, T., Hestad, K. & Diseth, T. H. Cognitive outcome in children and adolescents treated for acute lymphoblastic leukaemia with chemotherapy only. Acta Paediatr. 98, 180–186 (2009).
Harshman, L. A. et al. Population-based exploration of academic achievement outcomes in pediatric acute lymphoblastic leukemia survivors. J. Pediatr. Psychol. 37, 458–466 (2012).
Bull, R. & Lee, K. Executive functioning and mathematics achievement. Child Dev. Perspect. 8, 36–41 (2014).
Kirchhoff, A. C. et al. Physical, mental and neurocognitive status and employment outcomes in the Childhood Cancer Survivor Study Cohort. Cancer Epidemiol. Biomark. Prev. 20, 1838–1849 (2011).
Kunin-Batson, A., Kadan-Lottick, N. & Neglia, J. P. The contribution of neurocognitive functioning to quality of life after childhood acute lymphoblastic leukemia. Psychooncology 23, 692–699 (2014).
Fardell, J. E. et al. Health-related quality of life of children on treatment for acute lymphoblastic leukemia: a systematic review. Pediatr. Blood Cancer 64, e26489 (2017).
Zheng, D. J. et al. Longitudinal analysis of quality-of-life outcomes in children during treatment for acute lymphoblastic leukemia: a report from the Children’s Oncology Group AALL0932 trial. Cancer 124, 571–579 (2018).
Gaynon, P. S. et al. Long-term results of the children’s cancer group studies for childhood acute lymphoblastic leukemia 1983-2002: a Children’s Oncology Group Report. Leukemia 24, 285–297 (2010).
Matloub, Y. et al. Intrathecal triple therapy decreases central nervous system relapse but fails to improve event-free survival when compared with intrathecal methotrexate: results of the Children’s Cancer Group (CCG) 1952 study for standard-risk acute lymphoblastic leukemia, reported by the Children’s Oncology Group. Blood 108, 1165–1173 (2006).
Varni, J. W., Burwinkle, T. M., Seid, M. & Skarr, D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul. Pediatr. 3, 329–341 (2003).
Conklin, H. M. et al. Computerized cognitive training for amelioration of cognitive late effects among childhood cancer survivors: a randomized controlled trial. J. Clin. Oncol. 33, 3894–3902 (2015).
van der Plas, E. et al. Quantitative MRI outcomes in child and adolescent leukemia survivors: evidence for global alterations in gray and white matter. NeuroImage: Clin. 28, 102428 (2020).
Boyd, M. A socioeconomic scale for Canada: measuring occupational status from the census. Can. Rev. Sociol./Rev. canadienne de. sociologie 45, 51–91 (2008).
Wechsler, D. The Wechsler Intelligence Scale for Children 4th edn (Pearson Assessment, London, 2004).
Wechsler, D. Wechsler Adult Intelligence Scale 4th edn (Pearson Assessment, San Antonio, TX, 2008).
Wechsler, D. Wechsler Individual Achievement Test—Third Edition (NCS Pearson, San Antonio, TX, 2009).
Gardner, R. A. & Broman, M. The Purdue pegboard: normative data on 1334 school children. J. Clin. Child Psychol. 8, 156–162 (1979).
Conners, C. Conners 3 Manual 3rd edn (Multi-Health Systems Inc., Toronto, ON, 2008).
Varni, J. W., Seid, M. & Kurtin, P. S. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med. Care 39, 800–812 (2001).
R Core Team. R: A Language and Environment for Statistical Computing [Internet] (R Foundation for Statistical Computing, Vienna, Austria) https://www.R-project.org/ (2020).
Panepinto, J. A. et al. Impact of family income and sickle cell disease on the health-related quality of life of children. Qual. Life Res. 18, 5–13 (2009).
Narad, M. E. et al. Parent-teacher agreement on ADHD symptoms across development. Psychol. Assess. 27, 239–248 (2015).
Willard, V. W. et al. Concordance of parent-, teacher- and self-report ratings on the Conners 3 in adolescent survivors of cancer. Psychol. Assess. 28, 1110–1118 (2016).
Varni, J. W., Limbers, C. A. & Burwinkle, T. M. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual. Life Outcomes 5, 2 (2007).
Kunin-Batson, A. et al. Predictors of independent living status in adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Pediatr. Blood Cancer 57, 1197–1203 (2011).
Ehrhardt, M. J. et al. Neurocognitive, psychosocial, and quality-of-life outcomes in adult survivors of childhood non-Hodgkin lymphoma. Cancer 124, 417–425 (2018).
Cox, L. E. et al. Feasibility and acceptability of a remotely administered computerized intervention to address cognitive late effects among childhood cancer survivors. Neurooncol Pr. 2, 78–87 (2015).
Conklin, H. M. et al. Long-term efficacy of methylphenidate in enhancing attention regulation, social skills, and academic abilities of childhood cancer survivors. J. Clin. Oncol. 28, 4465–4472 (2010).
Conklin, H. M. et al. Long-term efficacy of computerized cognitive training among survivors of childhood cancer: a single-blind randomized controlled trial. J. Pediatr. Psychol. 42, 220–231 (2017).
Smithson, E. F., Phillips, R., Harvey, D. W. & Morrall, M. C. H. J. The use of stimulant medication to improve neurocognitive and learning outcomes in children diagnosed with brain tumours: a systematic review. Eur. J. Cancer 49, 3029–3040 (2013).
Netson, K. L. et al. Parent and teacher ratings of attention during a year-long methylphenidate trial in children treated for cancer. J. Pediatr. Psychol. 36, 438–450 (2011).
Didsbury, M. S. et al. Socio-economic status and quality of life in children with chronic disease: a systematic review. J. Paediatr. Child Health 52, 1062–1069 (2016).
Hiyoshi, A., Montgomery, S., Bottai, M. & Hovén, E. I. Trajectories of income and social benefits for mothers and fathers of children with cancer: a national cohort study in Sweden. Cancer 124, 1492–1500 (2018).
Vetsch, J. et al. Health-related quality of life of survivors of childhood acute lymphoblastic leukemia: a systematic review. Qual. Life Res. 27, 1431–1443 (2018).
Acknowledgements
This work was supported by the Ontario Institute for Cancer Research through funding provided by the Government of Ontario (IA024), the Canadian Institutes of Health Research, and the Canadian Cancer Society (Grant #703558).
Author information
Authors and Affiliations
Contributions
L.G.-C., E.A.W., P.T., and L.H. contributed substantially to the acquisition of data. E.v.d.P., T.L.S.N., D.T.B., R.W., S.G., J.H., R.J.S., S.I., and B.J.N. contributed to the conception, design, analysis and/or interpretation of the data. E.v.d.P. and B.J.N. were primarily responsible for drafting and revising the manuscript. All authors provided final approval of the manuscript to be submitted for publication.
Corresponding author
Ethics declarations
Competing interests
R.J.S. has performed consulting work with Ironshore Pharmaceutic and Development, Inc., Purdue Pharma and Lilly Corp. He is the Toronto Dominion Bank Chair in Child and Adolescent Psychiatry. The other authors have no conflicts of interest to disclose.
Consent statement
All participants and/or their parents/guardians provided written, informed consent prior to participation in the study. Assent was obtained from participants too young or otherwise unable to provide informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
van der Plas, E., Spencer Noakes, T.L., Butcher, D.T. et al. Cognitive and behavioral risk factors for low quality of life in survivors of childhood acute lymphoblastic leukemia. Pediatr Res 90, 419–426 (2021). https://doi.org/10.1038/s41390-020-01230-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01230-7