Abstract
Background
Secondhand smoke (SHS) exposure at home and fetal SHS exposure during pregnancy are a major cause of disease among children. The aim of this study is quantifying the burden of disease due to SHS exposure in children and in pregnancy in 2006–2017 for the 28 European Union (EU) countries.
Methods
Exposure to SHS was estimated using a multiple imputation procedure based on the Eurobarometer surveys, and SHS exposure burden was estimated with the comparative risk assessment method using meta-analytical relative risks. Data on deaths and disability-adjusted life years (DALYs) were collected from National statistics and from the Global Burden of Disease Study.
Results
Exposure to SHS and its attributable burden stalled in 2006–2017; in pregnant women, SHS exposure was 19.8% in 2006, 19.1% in 2010, and 21.0% in 2017; in children it was 10.1% in 2006, 9.6% in 2010, and 12.1% in 2017. In 2017, 35,633 DALYs among children were attributable to SHS exposure in the EU, mainly due to low birth weight.
Conclusions
Comprehensive smoking bans up to 2010 contributed to reduce SHS exposure and its burden in children immediately after their implementation; however, SHS exposure still occurs, and in 2017, its burden in children was still relevant.
Impact
-
Exposure to secondhand smoke at home and in pregnancy is a major cause of disease among children.
-
Smoking legislation produced the adoption of voluntary smoking bans in homes; however, secondhand smoke exposure at home still occurs and its burden is substantial.
-
In 2017, the number of deaths and disability-adjusted life years in children attributable to exposure to secondhand smoke in the European Union countries were, respectively, 335 and 35,633.
-
Low birth weight caused by secondhand smoke exposure in pregnancy showed the largest burden.
-
Eastern European Union countries showed the highest burden.
Similar content being viewed by others
Introduction
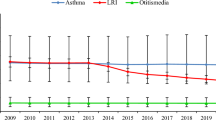
Exposure to secondhand smoke (SHS) is a major cause of disease among children, and there is no safe level of SHS exposure.1,2 It has been shown to be associated with many adverse health effects among children, and the diseases with the strongest evidence of a causal link with SHS exposure in children are asthma, lower respiratory tract infections (LRI), otitis media (OM), and sudden infant death syndrome (SIDS).2,3 Moreover, exposure to SHS during pregnancy are detrimental to fetal growth and development, leading to adverse birth outcomes such as preterm birth, low birth weight (LBW), being small for gestational age, and perinatal and infant mortality.2,3
Children are involuntarily exposed to SHS from their parents smoking at home. However, in the past 20 years in many countries worldwide, the implementation of smoking bans in workplaces, including the hospitality sector, following Article 8 of the World Health Organization (WHO) Framework Convention for Tobacco Control, have had, in the early years, an indirect effect of increasing voluntary smoking bans in homes, which may also result from increases in cessation rates in household members.4,5,6 For example, smoke-free homes increased from 72% in 2008 to 78% in 2012 in Italy,7,8 from 16% in 1998 to almost 50% in 2008 in smokers’ houses in England,9 by 50% in Scotland,10 and SHS exposure at home declined from 29.2% in 2006 to 12.7% in 2011 in Spain.11 Moreover, the introduction of smoke-free legislation in Scotland showed a 39% reduction in salivary cotinine concentration among children.12
As a consequence of the adoption of smoke-free houses, smoking bans had further indirect effect of reducing the diseases in children due to SHS exposure mainly at home and in newborns due to SHS exposure among pregnant women in any setting. A recent meta-analysis that included 41 studies, among which 16 were from Europe, showed an association between the implementation of smoke-free legislation and reductions in the rates of hospitalization from asthma exacerbations (−9.8%, 95% confidence intervals [CIs]: −16.6%, −3.0%), LRI (−18.5%, 95% CI: −32.8%, −4.2%), and LBW (−2.8%, 95% CI: −4.4%, −1.2%) in children.13 In Scotland, smoke-free legislation was associated with a gradual decrease in acute LRI events14 and in the rate of asthma admissions in children.15 In Hungary, the strengthening of smoking bans improved the probability of live births,16 and the introduction of national smoke-free legislation in England was associated with fewer hospital admissions per year for respiratory tract infection and asthma in children.17,18
Despite the increase of smoke-free homes in the early years after smoking legislation with subsequent increase in children’s health, many children and pregnant women were still exposed to SHS in European Union (EU) countries in recent years. As an example, in 2010 in Italy, 54% of youths were exposed to SHS in any setting,19 and in 2016, 72% of children aged <12 years were exposed in any setting in Spain.20 Moreover, in a Spanish birth cohort, 30% of pregnant women were exposed to SHS during 1997–2008,21 in Poland the prevalence in pregnant women was estimated as 13% in 2008,22 and recently, in a sample of Slovak pregnant women 28% of them lived with a smoking partner.23
As a consequence, the burden of disease due to SHS exposure in children should be still considerable.
A full understanding of the exposure to SHS at home in children and the consequent burden of diseases for the whole EU population of children and newborns in the past decade is lacking. The aim of this study, conducted within the TackSHS Project,24 is to quantify the burden of disease due to SHS exposure at home among children and to SHS exposure in pregnancy in the past 10 years in 28 EU countries.
Methods
Burden of disease from SHS exposure
The burden of disease from exposure to SHS in children was estimated for each country using the comparative risk assessment methodology.25 In brief, we selected the diseases for which there is evidence of a causal relationship with SHS exposure and for which there is sufficient quantitative information.25 Then for each SHS-related disease (LBW, SIDS, LRI, OM, and asthma exacerbation), the country-specific mortality and morbidity attributable to exposure to SHS was calculated by first estimating the SHS attributable fraction (AFSHS) for each age group using the Levin’s formula26
where p is the prevalence of exposure to SHS (by age groups in each country) and RR is the corresponding relative risk of death or disease from the SHS-related disease for children exposed to SHS compared to not exposed.
For each disease and country, the population AFSHS (PAF) was then obtained as a weighted sum of age-specific AFSHS with the proportion of cases in each stratum as weight. The PAF represents the reduction in the population burden of disease that would occur if exposure to SHS was removed. The age groups included in the analysis varied depending on the disease under study. The number of deaths attributable to SHS exposure was obtained by multiplying the age-specific number of deaths for the corresponding AFSHS and summing over ages. The number of disability-adjusted life years (DALYs) was similarly computed.
For each estimate of deaths and DALYs attributable to SHS exposure, an uncertainty interval (UI) was obtained with a Monte Carlo procedure, which deal simultaneously with uncertainty arising from estimates of SHS exposure, RR, and deaths or DALYs25 (see Supplementary Material).
Exposure to SHS
We used data from the Eurobarometer surveys carried out in 2006, 2010, 2014, and 2017, which are regular face-to-face interviews with approximately 1000 subjects in each EU country (see Supplementary Material). We excluded the 2008 and 2012 surveys in order to contain the amount of data (and missing data) and to maintain a 3–4-year interval between surveys. Since SHS exposure was not uniformly asked in all surveys, we used a multiple imputation procedure to estimate SHS exposure at home for the missing years (see Supplementary Material).27
In detail, we created a new dataset including socio-demographic, smoking, and SHS exposure variables from all the surveys,28 and we replaced each missing value with a plausible one M times (creating M complete datasets), choosing M according to the rule of thumb based on the average percentage rate of missingness.29 This step was carried out with the Multivariate Imputation by Chained Equations procedure, which involves specifying a posterior distribution for all incomplete variables and required a preliminary step consisting in the selection of a set of predictors to be included in the regressions.27,30 The predictors included socio-demographic individual variables, such as gender, age, marital status, and survey’s specific variables, such as country, year, and survey weight. The regressions used varied according to the nature of the variables (logistic or polytomous logistic regressions and proportional odds models). Each of the M complete datasets was then analyzed with standard statistical methods and the results were then pooled to obtain a final point estimate and a measure of precision, which accounts for uncertainty due to missing information.27 Our data presented two different patterns of missing values. The first one is systematically missing data, which are those variables completely missing in some surveys. The second type of missing values, i.e., sporadically missing data, is partly and randomly missing in some surveys. We took into account for the clustered structure of the data coming from different surveys by forcing the survey year to be a predictor.28,31
The final SHS exposure for children used in the burden estimation represents the proportion of people with children who allow smoking in their house and were specific for age groups 0–9 and 10–14 years. Exposure among pregnant women was defined as the proportion of women aged 25–44 years being ever exposed to SHS in any setting (house, workplace, car, or public places). The age class 25–44 was chosen in order to take into account for the average age of women at childbirth in EU countries, which, in 2017, varied between 26 years of age in Bulgaria and 31 years of age in Italy, with an average of 29 years in EU.32 Both SHS exposure measures were estimated taking into account for the survey weights ensuring that each country is represented in proportion to its population size and to its sample composition (see Supplementary material).
Data
The RRs of death or incidence from LBW, SIDS, LRI, OM, and asthma exacerbation for children exposed to SHS in comparison to not exposed were estimated from the most recent meta-analyses. In Table 1, the selected RRs values with the referring age groups, SHS exposure definition, and references are reported.
For years 2006, 2010, and 2014, the age-specific number of deaths from each disease for each country was extracted from the Eurostat (http://ec.europa.eu/eurostat/data/database/) and WHO (http://data.euro.who.int/dmdb/) databases that report observed data from EU Members States’ National Statistical Institutes. For year 2017, the number of deaths was extracted from the Global Health Data Exchange of the Global Burden of Disease (GBD) study, an international project that annually quantifies and globally compares the health loss due to diseases, accidents, and risk factors by age, sex, and geographical area and is compliant with the Guidelines for Accurate and Transparent Health Estimates Reporting.39,40
For years 2006, 2010, and 2014, the country- and age-specific DALY from each disease were computed by first estimating the years of life lost (by applying the life expectancy extracted from Eurostat to the number of deaths collected from the Eurostat/WHO databases) and then summing them to the years lived with disability estimated within the GBD study. For 2017, the DALY estimates of GBD were used.
In Supplemental Table S4 of the Supplementary Material, the list of International Classification of Diseases X codes used to select the diseases from the WHO/Eurostat databases and from the GBD study is presented. While the same classification was used to identify deaths and DALYs from SIDS and asthma from WHO/Eurostat and GBD, some differences were observed in the codes for LBW, LRI, and OM (see Supplementary Material).
Results
The multiple imputation procedure was run with M = 80 imputations. Exposure to SHS at home in the overall EU among children stalled from 2006 to 2017 with values of 10.1% in 2006 (95% CI: 4.1–16.1%), 9.6% (95% CI: 1.8–17.9%) in 2010, 10.8% (95% CI: 1.9–20.2%) in 2014, and 12.1% (95% CI: 3.3–21.4%) in 2017. Exposure to SHS for pregnant women in the overall EU stalled from 2006 to 2017 with values of 19.8% in 2006 (95% CI: 12.6–27.1%), 19.1% (95% CI: 8.8–29.4%) in 2010, 20.4% (95% CI: 9.2–31.7%) in 2014, and 21.0% (95% CI: 8.7–33.4%) in 2017. Prevalence estimates were largely uncertain due to the large amount of missing data taken into account in the multiple imputation procedure, and by visual inspection of CIs, we can conclude that differences in prevalence were not significant.
As a consequence of the trend in SHS prevalence, the SHS-PAF in the EU countries were stable for all the diseases (Table 2).
In 2017, the number of deaths and DALYs attributable to SHS exposure were, respectively, 335 (UI: 88–772) and 35,633 (UI: 11,141–78,176). The proportion of deaths and DALYs attributable to SHS exposure on the total number of deaths and DALYs among children in the EU was, respectively, 1.4% and 0.7%. The proportion of DALYs varied between values >1.5% in Malta, Slovakia, Bulgaria, Poland, and Romania and values <0.4% in Finland, The Netherlands, Belgium, and Luxembourg (Fig. 1).
AT: Austria, BE: Belgium, BG: Bulgaria, CY: Cyprus, CZ: Czech Republic, HR: Croatia, DK: Denmark, EE: Estonia, FI: Finland, FR: France, DE: Germany, GR: Greece, HU: Hungary, IE: Ireland, IT: Italy, LV: Latvia, LT: Lithuania, LU: Luxembourg, MT: Malta, NL: Netherlands, PL: Poland, PT: Portugal, RO: Romania, SK: Slovakia, SI: Slovenia, ES: Spain, SE: Sweden, UK: United Kingdom.
In 2017, LBW caused most part of both deaths and years of healthy life lost due to prenatal SHS exposure, with a proportion of DALYs of 0.4% in all the EU countries, reaching a maximum of 1.1% in Poland. LBW was followed by LRI, asthma, SIDS, and finally by OM, with around 0.1% DALYs attributable to SHS on the overall DALYs (Fig. 2). In Eastern EU countries such as Poland, Bulgaria, Slovakia, and also Malta, DALYs due to SHS exposure were mainly from LBW with a proportion up to 1.1% in Poland, whereas in Romania and Bulgaria a high proportion of SHS-related DALYs was from LRI (Fig. 2).
Discussion
This study provides evidence indicating a stall in SHS household exposure in children and in SHS exposure among pregnant women in all settings and, consequently, in PAF estimates.
In the first period, from 2006 to 2010, slightly lower values of SHS exposure in children and pregnant women were estimated, and this may be in part due to the implementation of smoking bans in 16 out of 28 EU countries (Luxembourg, Belgium, the UK, Spain, Finland, Slovenia, Lithuania, Denmark, France, Portugal, Croatia, Slovakia, Latvia, Cyprus, Greece, Germany). Other 6 EU countries implemented nation-wide smoking bans maximum 2 years before 2006, i.e., in 2004–2005 (Ireland, Sweden, Malta, Italy, Estonia, The Netherlands), whereas after 2010, only 6 EU countries developed smoking bans (Poland, Hungary, Bulgaria, Romania, Czechia, Austria). The stall in SHS prevalence estimates from 2010 to 2017 suggests that comprehensive smoking bans had less influence in the adoption of smoke-free homes in the long run. In this period, other tobacco control measures were implemented in EU countries with no significant impact on SHS exposure at home. Specifically, in the whole period tax increases and anti-tobacco mass-media campaigns were implemented in some countries; pictorial warnings in tobacco packages was implemented in all EU countries in 2016 and smoking bans in cars with children or pregnant women was applied in some countries in 2015–2017, e.g., in UK, France, and Italy. Thus smoking bans could have an immediate effect in slightly reducing smoking at home, but SHS exposure still occurs and its burden is substantial in the long run.
A recent systematic review showed findings from 26 studies evaluating the burden of disease due to SHS exposure in children for different countries worldwide, with PAF estimates that largely varied among studies. PAF estimates, mainly associated with incidence, except for SIDS, ranged between 0.9% and 22.4% for OM, 6.7–43.6% for SIDS, 2.0–31.9% for LRI, 0.8–35% for asthma, and 2.1–23.5% for LBW,3 since they are dependent on the prevalence of exposure to SHS, which largely varies across countries.25 The PAFs estimated in this study are in line with the lower ranges of those estimated in the systematic review, whereas a recent study estimated that PAF attributable to SHS exposure for OM, asthma, and LRI for 2015 in Spain was slightly lower in comparison to our estimates, probably due to a higher estimate of SHS exposure, defined by the existence of at least one smoker among household members.41
In 2017, the GBD study, which provides a comprehensive assessment of risk factor exposure and attributable burden of disease, estimated, for the EU countries, a total of 186 deaths and 20,870 DALYs attributable to SHS exposure in children aged <14 years, substantially less than our estimate of 335 deaths and 35,633 DALYs.39 This is likely due to the exclusion of LBW, SIDS, and asthma from the burden quantification of GBD estimates, and we showed that LBW was one of the diseases that mainly contributed to the burden from SHS exposure in children, especially in Eastern EU countries, determined from SHS exposure in pregnancy.
Our results show that in 2017 the burden was lower in Northern European countries, such as Luxembourg, Belgium, The Netherlands, Finland, Estonia, and Sweden, and higher in Eastern countries, such as Romania, Poland, Bulgaria, and Slovakia. Part of the countries with a lower SHS burden are those that implemented a smoking ban earlier. Thus the distribution of the burden due to SHS exposure by disease is not uniform in EU countries. Among those countries with a larger burden, Romania and Bulgaria showed a high proportion of DALYs attributable to SHS exposure from LRI, whereas Poland, Slovakia, Malta, and Bulgaria showed a high proportion in DALYs from LBW reaching a proportion of DALYs attributable to prenatal SHS exposure on total DALYs of 1.1% in Poland. LBW resulted the diseases with the highest proportion of both deaths and years of healthy life lost due to SHS exposure, suggesting a notable problem of SHS exposure in pregnancy, especially in Eastern EU countries.
There are several surveys that investigated SHS exposure in the EU countries, but SHS exposure in public places was the main studied outcome because of the evaluation of smoking bans (i.e., Global Tobacco Surveillance System and Eurobarometer surveys), whereas SHS household exposure, which is the main source of exposure in children, was not recently evaluated. The main strength of this study is that it provides a quantification of the burden due to SHS exposure at home among children in the past 10 years for the 28 EU countries, even if the estimates were largely uncertain due to the large amount of missing values taken into account in the imputation procedure. Moreover, few studies quantified the burden form SHS exposure in pregnancy in EU or in high-income countries,42 and to our knowledge, this is the first study that provides a quantification of this burden estimating deaths and DALYs from LBW. Another strength is in the data sources: first, Eurobarometer surveys allow estimating household SHS exposure with uniform data for all the EU countries; second, mortality data for 2006, 2010, and 2014 are observed and not estimated data and are available for all the diseases of interest, reducing the uncertainty that could arise from death estimates. The DALY estimates combine an observed (years of life lost) with an estimated (years lived with disability) part, reducing the uncertainty that could arise form an estimation of the total DALYs. Moreover, another strength of this study is to use a direct question for SHS home exposure estimates, whereas, within the GBD study, household SHS prevalence was indirectly estimated using data on household composition and smoking habits.39
This study has, however, some limitations. A first limitation is that, given the exposure definition, changes in prevalence refer to changes in the proportion of people with children who adopt smoking rules in home and proportion of women in fertile age being ever exposed, independently from the amount (hours) of exposure, that cannot be quantified using our data without generating further excessive uncertainty. A more precise estimation of SHS exposure taking into account for the effective quantification of exposure could improve results, but this information is not available for all the EU countries.
A second limitation comes from the age classes of SHS exposure that are not always aligned to those of the diseases under study. For example, SIDS refer to children aged <1 year, and the burden was studied with the SHS exposure estimated for children of age 0–9 years. We can, however, reasonably assume that rules on smoke-free houses do not vary with the children age. Another limitation is that the quality of the meta-analysis used to select RR was not assessed, but these were chosen only on the basis of being most recent, even if some of them included old studies. A final limitation arises from the imputation procedure used to estimate SHS exposure that was used to impute data from several sample surveys by imputing the data in the combined data matrix from all surveys. This approach assumes that the relationship between SHS exposure and its explicative variables found in 2006 and 2010 remains unchanged also for years 2014 and 2017. Moreover, our imputation approach does not account for differences between the surveys, for example, if they were conducted at different times or if different sampling methodologies were used or if they were carried out by different organizations. A more appropriate approach is to carry out a hierarchical multiple imputation taking into account for the multilevel structure of the data given by four independent surveys.28,31,43 Hierarchical multiple imputation procedures that have already been developed in the literature, however, only take into account multilevel continuous and binary data and could not be applied to the factor variables of our data. However, literature results show that valid inferences form hierarchal multiple imputation methods can only be obtained if the dataset gathers a large number of clusters, and in our study we are working with only four clusters.28,43 Moreover, the main feature of the multilevel modeling are to take into account for differences between surveys and to include covariates at survey level. In our analysis, however, the pooled surveys were carried out by the same organization using the same sampling design, and the only survey-level variable available was the year in which it was carried out that was included among the predictors in our imputation model.28
In conclusion, in the past decade, despite that smoke-free homes initially increased, presumably as a result of the implementation of smoking bans,44 our results show that, in the long run, the diseases caused by SHS exposure in children are still not negligible. This suggests that household SHS exposure in children and among pregnant women are still high. Up to 1.6% of total DALYs could be avoided eliminating SHS exposure in children and pregnancy. Preventing exposure of children to SHS in home and prenatal exposure to maternal SHS exposure in the EU therefore still requires great and for sure coordinated efforts.
References
US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General (US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta, GA, 2006).
Öberg, M., Jaakkola, M. S., Woodward, A., Peruga, A. & Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 377, 139–146 (2011).
Carreras, G. et al. Burden of disease attributable to second-hand smoke exposure: a systematic review. Prev. Med. 129, 105833 (2019).
Cheng, K. W., Glantz, S. A. & Lightwood, J. M. Association between smokefree laws and voluntary smokefree-homes rules. Am. J. Prev. Med. 41, 566–572 (2011).
Martínez-Sánchez, J. M. et al. Do smoke-free policies in work and public places increase smoking in private venues? Tob. Control 23, 204–207 (2014).
Monson, E. & Arsenault, N. Effects of enactment of legislative (public) smoking bans on voluntary home smoking restrictions: a review. Nicotine Tob. Res. 19, 141–148 (2017).
Minardi, V. et al. Compliance with the smoking ban in Italy 8 years after its application. Int. J. Public Health 59, 549–554 (2014).
Gallus, S. et al. Voluntary home smoking ban: prevalence, trend and determinants in Italy. Eur. J. Public Health 26, 841–844 (2016).
Jarvis, M. J., Sims, M., Gilmore, A. & Mindell, J. Impact of smoke-free legislation on children’s exposure to secondhand smoke: cotinine data from the Health Survey for England. Tob. Control 21, 18–23 (2012).
Akhtar, P. C. et al. Smoking restrictions in the home and secondhand smoke exposure among primary schoolchildren before and after introduction of the Scottish smoke-free legislation. Tob. Control 18, 409–415 (2009).
Fernández, E. et al. Changes in secondhand smoke exposure after smoke-free legislation (Spain, 2006–2011). Nicotine Tob. Res. 19, 1390–1394 (2017).
Akhtar, P. C., Currie, D. B., Currie, C. E. & Haw, S. J. Changes in Child Exposure to Environmental Tobacco Smoke (CHETS) study after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ 335, 545 (2007).
Faber, T. et al. Effect of tobacco control policies on perinatal and child health: a systematic review and meta-analysis. Lancet Public Health 2, e420–e437 (2017).
Been, J. V. et al. Smoke-free legislation and paediatric hospitalisations for acute respiratory tract infections: national quasi-experimental study with unexpected findings and important methodological implications. Tob. Control 27, e160–e166 (2018).
Mackay, D., Haw, S., Ayres, J. G., Fischbacher, C. & Pell, J. P. Smoke-free legislation and hospitalizations for childhood asthma. N. Engl. J. Med. 363, 1139–1145 (2010).
Hajdu, T. & Hajdu, G. Smoking ban and health at birth: evidence from Hungary. Econ. Hum. Biol. 30, 37–47 (2018).
Been, J. V., Millett, C., Lee, J. T., van Schayck, C. P. & Sheikh, A. Smoke-free legislation and childhood hospitalisations for respiratory tract infections. Eur. Respir. J. 46, 697–706 (2015).
Millett, C., Lee, J. T., Laverty, A. A., Glantz, S. A. & Majeed, A. Hospital admissions for childhood asthma after smoke-free legislation in England. Pediatrics 131, e495–e501 (2013).
Martínez-Sánchez, J. M. et al. Exposure to secondhand smoke in Italian non-smokers 5 years after the Italian smoking ban. Eur. J. Public Health 22, 707–712 (2012).
López, M. J. et al. Social inequalities in secondhand smoke exposure in children in Spain. Tob. Induc. Dis. 16, 14 (2018).
Robinson, O. et al. The association between passive and active tobacco smoke exposure and child weight status among Spanish children. Obesity 24, 1767–1777 (2016).
Wdowiak, A., Wiktor, H. & Wdowiak, L. Maternal passive smoking during pregnancy and neonatal health. Ann. Agric. Environ. Med. 16, 309–312 (2009).
Argalášová, L. et al. Determinants of ETS exposure in a sample of Slovak pregnant women. Rev. Environ. Health 32, 201–205 (2017).
Fernández, E. et al. Tackling second-hand exposure to tobacco smoke and aerosols of electronic cigarettes: the TackSHS Project Protocol. Gac. Sanit. 34, 77–82 (2020).
Öberg, M., Jaakkola, M. S., Prüss-Üstün, A., Schweizer, C. & Woodward, A. Second-Hand Smoke: Assessing the Environmental Burden of Disease at National and Local Levels (World Health Organization, Geneva, 2010).
Levin, M. The occurrence of lung cancer in man. Acta Unio Int. Contra Cancrum 9, 531–541 (1953).
Rubin, D. B. Multiple Imputation for Nonresponse in Surveys (Wiley, New York, 1987).
Gelman, A., King, G. & Liu, C. Not asked and not answered: multiple imputation for multiple surveys. JASA 93, 846–857 (1999).
White, I. R., Royston, P. & Wood, A. M. Multiple imputation using chained equations: issues and guidance for practice. Stat. Med. 30, 377–399 (2011).
Raghunathan, T. E., Lepkowski, J. M., van Hoewyk, J. & Solenberger, P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv. Methodol. 27, 85–95 (2001).
Resche-Rigon, M. & White, I. R. Multiple imputation by chained equations for systematically and sporadically missing multilevel data. Stat. Methods Med. Res. 27, 1634–1649 (2018).
Eurostat. Fertility statistics. Mean age of women at childbirth across EU regions. https://ec.europa.eu/eurostat/statistics-explained/index.php/Fertility_statistics (2020) Accessed 29 Sep 2020.
Leonardi-Bee, J., Smyth, A., Britton, J. & Coleman, T. Environmental tobacco smoke and fetal health: systematic review and meta-analysis. Arch. Dis. Child. Fetal Neonatal Ed. 93, F351–F361 (2008).
Royal College of Physicians. Passive Smoking and Children. A Report by the Tobacco Advisory Group (RCP, London, 2010).
Jones, L. et al. Parental and household smoking and the increased risk of bronchitis, bronchiolitis and other lower respiratory infection in infancy: systematic review and meta-analysis. Respir. Res. 12, 5 (2011).
Li, J. S., Peat, J. K., Xuan, W. & Berry, G. Meta-analysis on the association between environmental tobacco smoke (ETS) exposure and the prevalence of lower respiratory tract infection in early childhood. Pediatr. Pulmonol. 27, 5–13 (1999).
Tinuoye, O., Pell, J. P. & Mackay, D. Meta-analysis of the association between secondhand smoke exposure and physician-diagnosed childhood asthma. Nicotine Tob. Res. 15, 1475–1483 (2013).
Jones, L., Hassanien, A., Cook, D., Britton, J. & Leonardi-Bee, J. Parental smoking and the risk of middle ear disease in children. Arch. Pediatr. Adolesc. Med. 166, 18–27 (2012).
GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1345–1422 (2017).
Stevens, G. A. et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet 388, e19–e23 (2016).
Continente, X. et al. Burden of respiratory disease attributable to secondhand smoke exposure at home in children in Spain (2015). Prev. Med. 123, 34–40 (2019).
Reece, S. et al. Secondhand smoke exposure during pregnancy: a cross-sectional analysis of data from Demographic and Health Survey from 30 low-income and middle-income countries. Tob. Control 28, 420–426 (2019).
Audigier, V. et al. Multiple imputation for multilevel data with continuous and binary variables. Stat. Sci. 33, 160–183 (2018).
Behbod, B., Sharma, M., Baxi, R., Roseby, R. & Webster, P. Family and carer smoking control programmes for reducing children’s exposure to environmental tobacco smoke. Cochrane Database Syst. Rev. 1, CD001746 (2018).
Acknowledgements
E.F. thanks CERCA Programme/Generalitat de Catalunya for institutional support. This work was supported by the European Union’s Horizon 2020 research and innovation program [grant number 681040]; the 2017 Italian Health Ministry CCM Programme Project “Choosing health priorities and selecting effective interventions to prevent the burden of chronic non-communicable diseases” (http://www.ccm-network.it/progetto.jsp?id=node/1977&idP=740); the Ministry of Research and Universities from the Government of Catalonia to EF [grant number 2017SGR319]; the Instituto Carlos III and co-funded by the European Regional Development Fund, FEDER [INT16/00211 and INT17/00103], Government of Spain to E.F. and the Italian League Against Cancer (Milan) to S.G. This manuscript was prepared by the TackSHS Project Consortium and does not necessarily reflect the views of the European Commission. The European Commission is not responsible for any use that may be made of the information that contains in this manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
G.C., A.L., B.C., S.G., E.F., and G.G. made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; M.J.L., A.L.N., A.L., M.T.P., J.B.S., and E.F. contributed in drafting the article or revising it critically for important intellectual content; G.C., A.L., B.C., S.G., M.J.L., A.L.N., A.L., M.T.P., J.B.S., E.F., and G.G. gave the final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent statement
Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Carreras, G., Lachi, A., Cortini, B. et al. Burden of disease from exposure to secondhand smoke in children in Europe. Pediatr Res 90, 216–222 (2021). https://doi.org/10.1038/s41390-020-01223-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01223-6
This article is cited by
-
A selective review of smoking cessation interventions in the emergency department
Emergency Cancer Care (2022)
-
European progress in working towards a tobacco-free generation
European Journal of Pediatrics (2021)