Abstract
Background
The impact of pediatric chronic kidney disease (pCKD) on the brain remains poorly defined. The objective of this study was to compare brain morphometry between children with early-stage pCKD and typically developing peers using structural magnetic resonance imaging (MRI).
Methods
The sample age range was 6–16 years. A total of 18 children with a diagnosis of pCKD (CKD stages 1–3) due to congenital anomalies of the kidney and urinary tract and 24 typically developing peers were included. Volumetric data from MRI and neurocognitive testing were compared using linear models including pCKD status, age, maternal education level, and socioeconomic status.
Results
Cerebellar gray matter volume was significantly smaller in pCKD, t(38) = −2.71, p = 0.01. In contrast, cerebral gray matter volume was increased in pCKD, t(38) = 2.08, p = 0.04. Reduced cerebellum gray matter volume was associated with disease severity, operationalized as estimated glomerular filtration rate (eGFR), t(14) = 2.21, p = 0.04 and predicted lower verbal fluency scores in the pCKD sample. Enlarged cerebral gray matter in the pCKD sample predicted lower scores on mathematics assessment.
Conclusions
This study provides preliminary evidence for a morphometric underpinning to the cognitive deficits observed in pCKD.
Impact
-
The impact of pediatric chronic kidney disease (CKD) on the brain remains poorly defined, with no data linking brain morphometry and observed cognitive deficits noted in this population.
-
We explored the relationship between brain morphometry (using structural magnetic resonance imaging), cognition, and markers of CKD.
-
Cerebellar and cerebral gray matter volumes are different in early CKD. Volumetric decreases in cerebellar gray matter are predicted by lower eGFR, suggesting a link between disease and brain morphometry.
-
Reduced cerebellar gray matter predicted lower verbal fluency for those with pCKD. Enlarged cerebral gray matter in the pCKD sample predicted lower mathematics performance.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) describes the progression of decline in kidney function leading to end-stage kidney disease (ESKD). Over 50% of all pediatric cases are due to congenital, non-glomerular anomalies,1 resulting in a life-long burden that requires routine care. Neurocognitive dysfunction is a well-established comorbidity in children and adults with both CKD and ESKD. Although intelligence (IQ) is generally within the normal range in early pediatric CKD (pCKD)2,3,4 there is evidence for impairment on tasks of executive function (EF) even in mild to moderate kidney disease, suggesting that EF declines may exist in parallel with duration and progression of disease.5,6
Despite recognition of neurocognitive comorbidity in the setting of early pCKD, there is a paucity of data exploring the neurobiology of these cognitive deficits. This gap in research is in part due to the low incidence of pCKD (15–74.7 cases per million children7) making implementation of comprehensive neuroimaging studies challenging. Existing neuroimaging studies in pCKD have included heterogeneous patient populations with a wide variety of disease etiologies and simultaneous inclusion of ESKD and renal transplant patients in parallel to early-stage CKD populations,8,9 limiting our ability to make inferences about the effects of early-stage pCKD on brain structure and function. Furthermore, research linking brain morphometry with the observed neurocognitive deficits in pCKD is lacking.
The present pilot study sought to addressed these gaps in the literature by using quantitative structural magnetic resonance imaging (sMRI) to compare neuroanatomical features between children with mild to moderate pCKD due to congenital anomalies of the kidney and urinary tract (CAKUT) and typically developing healthy controls. In addition, we explored the association between brain morphometry, disease status, and performance on neurocognitive assessment.
Methods
Study design and population
This study was conducted at the University of Iowa Stead Family Children’s Hospital and approved by the Institutional Review Board. The pilot sample was composed of male children aged 6–16 years with pCKD due to CAKUT and healthy male controls of the same age range. We limited pilot participation to males only for two reasons: (1) CAKUT is 2–3 times more prevalent in males than in females1 and there are known sex-based developmental differences in the brain that are difficult to account for in a small- to moderate-sized sample that includes both males and females.10 Informed consent and/or assent, as applicable, was obtained from participants and legal guardians at the time of participation. Parents and participants were informed that the results of the study, including sMRI, were collected for study purposes only and that results would not be disclosed.
We compared the pCKD cohort to a sample of healthy control participants from the surrounding community. Our inclusion and exclusion criteria were designed to recruit a homogeneous pCKD cohort given that previously published data suggest a lack of observed effect due to heterogeneity in recruited CKD samples.9 Potentially eligible pCKD participants were identified through electronic medical records by querying for a diagnosis code of CKD and specified age parameters. The research team then utilized the electronic medical record to confirm (1) accuracy of age and clinical diagnosis of CKD within the medical record, (2) estimated glomerular filtration rate (eGFR) between 30 and 90 ml/min/1.73 m2 within 6 months of study participation using the Bedside Schwartz calculation,11 and (3) etiology of pCKD due to CAKUT. Exclusion criteria for the pCKD sample included female gender, current dialysis requirement or history of chronic dialysis (defined as more than 6 weeks dialysis therapy), history of renal transplant, history of very preterm to extreme prematurity (<30 weeks estimated gestational age), history of seizures on antiepileptic medications, central nervous system anomalies (e.g., ventriculoperitoneal shunts, spina bifida), known chromosomal anomalies, congenital cardiac disease, diagnosed intellectual disability, traumatic brain injury that required hospitalization, and/or contraindication to MRI including presence of metal implants.
Caregivers of pCKD patients who met the study inclusion criteria received a letter of study invitation seeking voluntary study participation. Exclusion criteria, as defined above, were confirmed via the medical record and a phone interview with the caregiver prior to participation.
Unaffected, healthy controls aged 6–16 years were recruited from the local community via electronic advertisements with the intention to match with pCKD participants based on age as closely as possible. This group was enrolled in the study to represent a spectrum of both normal, healthy brain development and presumed normal kidney function. Exclusion criteria were as per the pCKD group.
Study procedures
Participants completed a neurocognitive assessment and sMRI on the day of research visit. Anthropometric data including height, weight, head circumference, and blood pressure were obtained. A blood sample was obtained to calculate eGFR using the Bedside Schwartz11 equation (0.413 × (height in centimeters))/serum creatinine [mg/dl]).
During the study visit, parents/caregivers completed measures to obtain demographic information, participant medical history (including birth history, other medical diagnoses, and medications), and family medical history. Additional data were provided by the parent regarding the child’s participation in educational assistance programs, birth history, and a family history of renal or psychiatric disease.
Study data were collected and managed using REDCap (Research Electronic Data Capture) hosted at the University of Iowa Hospitals & Clinics. REDCap is a secure, web-based software platform designed to support data capture for research studies.12,13
Neurocognitive assessments
All participants completed age-appropriate, standardized neurocognitive assessments with a focus on EF measures. This included assessment of intelligence (Wechsler Intelligence Scale for Children-IV [WISC-IV]), executive functioning (Behavior Rating Inventory of Executive Function—2nd edition [BRIEF] and Delis–Kaplan Executive Function System), memory (Children’s Memory Scale), dexterity (Grooved Pegboard Assessment), verbal fluency (Delis–Kaplan Executive Function System [DKEFS]), attention (Conners’ Continuous Performance Test II) and overall academic skills (Wide Range Achievement Test 4 [WRAT-4]). The BRIEF is a parent-report measure. All other tests were administered by a trained examiner and supervised by a licensed psychologist (A.L.C.).
Disease-related parameters
All participants were invited to provide a blood sample to estimate glomerular filtration rate (eGFR [ml/min/1.73m2]). Data were abstracted from the pCKD participants’ medical record to quantify illness duration as well as serum bicarbonate level (meq/l), hemoglobin (g/dl), and level of proteinuria in the 6 months prior to assessment (Table 2). Given that all pCKD participants had etiology of disease due to identified CAKUT, the disease start date was considered patient date of birth. A comprehensive medication and disease-related history was obtained for all participants. Within the pCKD sample, six (33%) were prescribed antihypertensive agents two participants (11%) were receiving growth hormone, one participant (5.5%) required alkalinizing agent therapy due to a history of metabolic acidosis, and no participants were on erythropoietin-stimulating agents at the time of assessment. No healthy controls were receiving any of these medications.
Neuroimaging
Participants underwent a non-sedated, noncontrast-enhanced MRI of the brain after MRI safety screening. sMRI scans obtained after June 2016 were acquired on a GE Discovery 750 W 3 Tesla (T) scanner (n = 39). Participants who were assessed before June 2016 completed scans on a Siemens TrioTim 3T scanner (n = 7). Both scans were equipped with a 32-channel head coil. Anatomical T1-weighted were acquired as follows for GE (Siemens parameters in parentheses): coronal BRAVO (MPRAGE), TR = 8.392 (2300) ms, TE = 3.184 (2.82) ms, TI = 450 (900) ms, flip angle = 12 (10)°, FOV = 282 × 282 × 264 mm, matrix = 256 × 256 × 240. Parameters for T2-weighted were: coronal, TR = 3000 (4800) ms, TE = 85.925 (430) ms, FOV = 256 × 256 × 224 mm, matrix = 256 × 256 × 160. A prospective motion correction (PROMO) sequence was used to prospectively correct motion artifacts.14 Following completion of the scan, all images were processed and visually inspected by a trained neuroimaging specialist. Scans were flagged and removed from analysis if there was too much artifact to produce reliable data (n = 4: 2 pCKD scans and 2 healthy control scans were removed prior to analysis).
sMRI images were processed using the BRAINSAutoWorkup pipeline that optimizes tissue classification through an iterative framework, producing robust parcellation of brain regions results in a multi-scanner setting.15 BRAINSAutoWorkup labels brain regions using a multi-atlas, similarity-weighted, majority-vote procedure (joint label fusion),16 using a set of expert-segmented templates adapted from the Desikan–Killiany atlas.17 Brain regions included cortical and subcortical regions, separated by hemispheres and tissue type (gray or white matter) where appropriate. The BRAINSAutoWorkup pipeline automatically derives volumes for brain structures. Inter-scanner variation was harmonized using an empirical Baysian approach (COMBAT harmonization) as implemented by the ez.combat toolbox in Rstudio.18,19,20 We confirmed that scanner did not predict ROI. Analyses were performed on harmonized data.
Statistical analysis
Neuroanatomical regions of interest (ROIs) vary with intracranial volume (ICV). Relationships between ROIs and ICV follow the power law principle, i.e., ROI = α × ICVβ, where α is the constant and β represents the scaling component of the power function. Effective de-trending of the relationship between ROI and ICV requires the use of the power proportion (PPM).21
PPM was calculated as follows:
Each ratio was subsequently standardized by subtracting out the grand mean and dividing by standard deviation. The efficacy of de-trending was verified with linear regression models with ICV as the predictor variable and PPMs as the dependent variables. None of the estimates for ICV were statistically significant (Supplementary Fig. 1), demonstrating effective de-trending. The outcome measures in the analysis represent power-adjusted ROIs as the primary dependent variables.
The primary analysis compared brain volumes between participants with pCKD and healthy controls. We examined 17 brain ROIs defined a priori representing major regions across the brain. We employed separate linear regression models on each ROI with group, age, parental socioeconomic status (SES), and maternal education as predictor variables. The impact of pertinent disease-related variables on brain morphometry were explored in ad hoc analyses limited to the pCKD group only.
We additionally compared groups on neurocognitive measures with specific attention to executive functioning. Standard scores and T-scores derived from standardized measures were used for statistical analyses. Parental SES and maternal education were added as predictor variables (note that the outcome scores of cognitive tests are age adjusted).
Ad hoc structure–function analyses were then performed for brain regions identified from the primary analysis as being significantly different between groups. These analyses were limited to the pCKD group only and included linear regressions to quantify the relationship between brain ROIs (independent variable) and neurocognitive outcomes (dependent variable).
Analyses were performed using RStudio version 3.5.1 (Feather Spray). Given that this was a pilot study, there was no correction for multiple comparisons, and results were considered significant if the unadjusted p value was less than 0.05.
Results
Sample
The final sample analyzed was dictated by the number of available and eligible pCKD patients from our center during the timeframe of the pilot study with complete neuroimaging data and included 18 males with pCKD and 24 healthy control males. Baseline demographics for the sample are outlined in Table 1. All participants in the final sample had both structural MRI data and neurocognitive data for analysis. Briefly, the average age of the sample was 12.0 years old (SD = 3 years). Mean age was not statistically different between groups, t(35.6) = −0.07, p = 0.9. Parental SES was similar across groups, X2(3) = 4.5, p = 0.2. Due to the potential impact of elevated blood pressure on cognition, we evaluated blood pressure at or above the 90th percentile for age between the pCKD and control samples.22 Elevated blood pressure was found to occur similarly in both cases and controls (X2(1) = 0.7, p = 0.4). Table 2 displays disease-related variables for the pCKD group.
Neuroanatomy
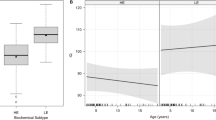
Figure 1a shows the standardized beta estimates of the difference between the groups for all investigated brain volumes (summary statistics for the standardized group estimates for each ROI can be found in Supplementary Table 1). Mean cerebellar gray matter volume was lower in the pCKD group relative to controls, t(38) = −2.71, p = 0.01. In contrast, mean cerebral gray matter was larger in the pCKD group than in controls, t(38) = 2.08, p = 0.04.
Panel a shows the standardized group estimates (x-axis) and 95% confidence limits of the estimates for each of the regions of interest (ROIs) included in the analysis (y-axis). Estimates are adjusted for age, socioeconomic status, and maternal education. The red (vertical) line marks 0, or no significant effect of group on ROI. Red circles mark significant group estimates. Panel b shows the relationship between estimated glomerular filtration rate, eGFR, (x-axis) and standardized cerebellum gray matter volume (y-axis) in the pCKD group.
Cerebellar and cerebral gray matter were, therefore, investigated for the secondary and ad hoc analyses exploring disease-related and functional correlates. eGFR was a significant predictor of cerebellar gray matter volume in pCDK, t(14) = 2.21, p = 0.04, where participants with lower eGFR exhibited lower cerebellar gray matter volume (Fig. 1b). Cerebrum gray matter volume was not associated with eGFR however (t(16) = −0.38, p = 0.71). There was no relationship between proteinuria, anemia, or acidosis and cerebellar or cerebral morphometry.
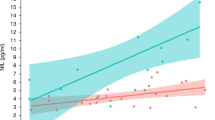
Structure–function relationships
Group differences on cognitive tasks are summarized in Table 3. Significant associations are shown in Fig. 2a, b. There was a significant, positive association between cerebellar gray volume and standardized verbal fluency scores for the category fluency task on the DKEFS assessments, with higher cerebellar volume associated with better performance in the pCKD group (t(12) = 2.5, p = 0.03) (Fig. 2a). Likewise, a significant negative relationship was observed between cerebral gray matter volume and mathematics in the pCKD group whereby higher cerebral gray matter was associated with reduced mathematics performance (t(12) = −2.9, p = 0.01) (Fig. 2b).
Discussion
Within this pilot study, we provide evidence for structural brain differences in patients with pCKD compared to healthy controls. Evaluation of brain morphometry demonstrated that cerebellar gray matter was disproportionately smaller in the pCKD cohort. Conversely, the pCKD cohort had increased cerebral gray matter volumes compared to healthy controls. Among disease-related variables, diminished renal function (eGFR) predicted lower cerebellar gray matter volumes, suggesting that renal disease may be a contributor to differences in brain morphometry. No disease-related variables, including duration of disease, were associated with the comparatively increased cerebral gray matter volume in the pCKD group.
In contrast to adult CKD, pediatric CKD is largely due to congenital causes with disease onset and progression coinciding with crucial stages in brain development.23 Previously published data details the presence of EF deficits in the pCKD population. The Chronic Kidney Disease in Childhood Study (CKiD)24 has provided a robust source of neurocognitive data focused on mild to moderate pCKD.2,5 Within the CKiD sample, up to 40% of children with pCKD were found to be at-risk for lower overall EF as per parental report from the Behavior Rating Inventory of Executive Function, which was more than double the normative expectation.2 Lower verbal fluency, as assessed by the Delis Kaplan Executive Function System (DKEFS) “category switching” task, has been linked with poorer blood pressure control in the pCKD population.25 Here, we performed a broad, standardized assessment of cognition and found very similar themes to published data with deficits primarily on tests of EF and evidence for potentially worsened performance on generalized tests of intelligence. Our results extend previously published neurocognitive findings by linking focused cognitive deficits to abnormal brain morphometry in a sample of children with pCKD.
Nineteen studies have been published utilizing neuroimaging in the pCKD population between 1977 and as of this writing.8 No previous studies have established a link between brain morphometry and neurocognitive assessment in pCKD. In contrast to published data, our study utilized well-defined inclusion and exclusion criteria to minimize heterogeneity in a relatively small sample size that may be introduced from a wide variety of disease etiologies. In doing so, we optimized the power to evaluate the effect of CKD on brain morphometry and neurocognition. Furthermore, by focusing on children early in the course of the disease—free from the complications of ESKD—we have an opportunity to identify the earliest signs of brain abnormality in relationship to cognition and clinical biomarkers of renal disease (e.g., eGFR, proteinuria, acidosis, anemia). Unfortunately, due to the nature of our pilot sample size we are underpowered to detect any effect of clinical renal disease biomarkers on cognition—this must be a focus of future research.
Brain development in the typically developing child involves an intricate process of dendritic pruning within the gray matter. Here, we described decreased cerebellar gray matter volumes and paradoxically increased cerebral gray matter volumes in children with CKD that are associated with diminished performance on tasks of verbal fluency and mathematics, respectively. Whether enlarged cerebral gray matter occurs as a failure of normal development or as a compensatory mechanism to maintain total brain volume in pCKD is unclear. Of interest, the pattern of increased cerebral gray matter in the pCKD population shows parallel themes to the cortical gray matter differences observed using neuroimaging in the autism/autism spectrum population.26,27 Further analysis is required utilizing both regional brain metabolic sequences and white matter connectivity to better inform the neurodevelopmental trajectory in pCKD.
Limitations to this study exist. pCKD can be considered a somewhat rare childhood disease, and as such we were limited in the number of participants recruited from a single center pilot study who met the stringent inclusion and exclusion criteria. Similarly, CKD—particularly in adulthood—is often considered a silent disease with prolonged asymptomatic progression. Despite thorough history taking, it is possible that we could have unknowingly included control patients with mild asymptomatic CKD as evidenced by several in our study with eGFR ranging between 80 and 90 ml/min/1.73 m2 as calculated using the serum creatinine level. eGFR using serum creatinine is highly influenced by hydration status and muscle mass; thus, inclusion of cystatin C to corroborate serum creatinine values of eGFR is warranted in future studies.
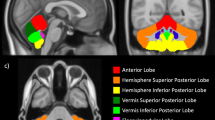
Multi-center expansion to this study is needed to further evaluate the effect of potential confounders such as SES and preterm birth that may be underrepresented due to the nature of the pilot sample. It is possible that we have underestimated the impact of preterm birth in the pCKD sample, particularly given that existing data suggest prematurity may be a risk factor for both CKD presence and lower cognitive outcomes.28,29,30 However, existing studies in late preterm infants have shown evidence of lower cerebral gray matter volumes among late preterm infants, which is in direct contrast to our finding of increased cortical volumes in the pCKD group.29 To further support pCKD as a driver for abnormal cerebellar gray matter development, post hoc analyses were performed. Figure 3 shows the case and control distribution of term and preterm participants and corresponding cerebellar gray matter volume distribution. We subsequently removed the preterm participants from the analysis and re-ran regional statistical analysis. Cerebellar gray matter volume remained significantly smaller for the pCKD sample in post hoc analyses and still controlling for age, SES, and maternal education (p = 0.021).
We are currently unable to fully disentangle the contributions of disease progression versus developmental diathesis on brain morphometry in this population. Our results within this small sample do suggest that differences in brain morphometry between groups are at least in part associated with decreased renal function. Verbitsky et al.31 provide evidence for worsened performance on tasks of EF in children who have identifiable genomic variants that are associated with the child’s underlying kidney disease. Future investigation should integrate evaluation of disease-causing genomic variants with both brain morphometry and cognition. Lastly, it is possible that the neurocognitive procedures from our study could be influenced by subtle interviewer and recall bias. Interviewer bias is a risk in a pilot study such as this; however, a standardized interview and assessment process as well as a double-score and double-data entry methodology performed by two trained psychometricians was established to further minimize the risk for interviewer bias. Although our psychometricians were not blinded to case/control status, the level of pCKD severity was not revealed to the team member(s) performing cognitive assessment. Lastly, recall bias is a risk when utilizing parent-report forms; thus, we sought to utilize objective (quantitative) data sources whenever possible and to corroborate parent-report forms with both the medical record and interviewer-derived objective data.
Our data provides key insight to the previously unrecognized differences in brain morphometry among patients pCKD and corresponding neurocognitive implications. These data highlight an opportunity for significant future research including use of longitudinal follow-up to more fully understand the brain developmental trajectories in pCKD—particularly in the pediatric to adult transition. Future studies should seek to examine nontraditional biomarkers of disease that may influence neurodevelopment in pCKD such as genomic drivers of kidney disease and the potential influence of chronic inflammation (e.g., altered cytokine expression) occurring in parallel with progression of CKD. The volumetric brain differences described here underscore that our understanding of pCKD progression and multisystem sequelae may be complicated by the developmental origins of CKD itself. The results herein should provide a catalyst for replication in a larger, longitudinal study with inclusion of younger pCKD patients to capture brain morphometry even earlier in the disease process. Given the life-long nature of pCKD, it behooves us to expand the currently limited understanding of this emerging kidney–brain relationship to better inform clinical care and ensure that pediatric patients with kidney disease enjoy a similar quality of life as their unaffected peers.
References
The North American Pediatric Renal Trials and Collaborative Studies 2014 Annual Report. Available at: https://web.emmes.com/study/ped/annlrept/annlrept.html. Accessed 10 Jan 2020.
Hooper, S. R. et al. Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin. J. Am. Soc. Nephrol. 6, 1824–1830 (2011).
Gerson, A. C. et al. Neurocognitive outcomes in children with chronic kidney disease: current findings and contemporary endeavors. Ment. Retard Dev. Disabil. Res. Rev. 12, 208–215 (2006).
Ruebner, R. L. et al. Neurocognitive dysfunction in children, adolescents, and young adults with CKD. Am. J. Kidney Dis. 67, 567–575 (2016).
Mendley, S. R. et al. Duration of chronic kidney disease reduces attention and executive function in pediatric patients. Kidney Int. 87, 800–806 (2015).
Hooper, S. R. et al. Executive functioning in children, adolescents, and young adults with chronic kidney disease. J. Dev. Behav. Pediatr. 36, 734–742 (2015).
Warady, B. A. & Chadha, V. Chronic kidney disease in children: the global perspective. Pediatr. Nephrol. 22, 1999–2009 (2007).
Moodalbail, D. G. et al. Systematic review of structural and functional neuroimaging findings in children and adults with CKD. Clin. J. Am. Soc. Nephrol. 8, 1429–1448 (2013).
Hartung, E. A. et al. Brain magnetic resonance imaging findings in children and young adults with CKD. Am. J. Kidney Dis. 72, 349–359 (2018).
Lenroot, R. K. et al. Sexual dimorphism of brain developmental trajectories during childhood and adolescence. Neuroimage 36, 1065–1073 (2007).
Schwartz, G. J. et al. Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int. 82, 445–453 (2012).
Harris, P. A. et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inf. 95, 103208 (2019).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 42, 377–381 (2009).
White, N. et al. PROMO: real-time prospective motion correction in MRI using image-based tracking. Magn. Reson. Med. 63, 91–105 (2010).
Pierson, R. et al. Fully automated analysis using BRAINS: AutoWorkup. Neuroimage 54, 328–336 (2011).
Wang, H. et al. Multi-Atlas segmentation with joint label fusion. IEEE Trans. Pattern Anal. Mach. Intell. 35, 611–623 (2013).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31, 968–980 (2006).
Fortin, J. P. et al. Harmonization of cortical thickness measurements across scanners and sites. Neuroimage 167, 104–120 (2018).
Johnson, W. E., Li, C. & Rabinovic, A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 8, 118–127 (2007).
Koscik, T. R. ez.combat. www.github.com/TKosik/ez.combat (2018).
Liu, D. et al. The power-proportion method for intracranial volume correction in volumetric imaging analysis. Front. Neurosci. 8, 356 (2014).
Flynn, J. T., et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Brown, T. T. & Jernigan, T. L. Brain development during the preschool years. Neuropsychol. Rev. 22, 313–333 (2012).
Furth, S. L. et al. Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin. J. Am. Soc. Nephrol. 1, 1006–1015 (2006).
Lande, M. B. et al. Association of blood pressure variability and neurocognition in children with chronic kidney disease. Pediatr. Nephrol. 31, 2137–2144 (2016).
Amaral, D. G., Schumann, C. M. & Nordahl, C. W. Neuroanatomy of autism. Trends Neurosci. 31, 137–145 (2008).
Foster, N. E. et al. Structural gray matter differences during childhood development in autism spectrum disorder: a multimetric approach. Pediatr. Neurol. 53, 350–359 (2015).
Crump, C. et al. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ 365, l1346 (2019).
Brumbaugh, J. E. et al. Altered brain function, structure, and developmental trajectory in children born late preterm. Pediatr. Res. 80, 197–203 (2016).
Adams-Chapman, I. et al. Neurodevelopmental impairment among extremely preterm infants in the neonatal research network. Pediatrics 141, e20173091 (2018).
Verbitsky, M. et al. Genomic disorders and neurocognitive impairment in pediatric CKD. J. Am. Soc. Nephrol. 28, 2303–2309 (2017).
Acknowledgements
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (K23DK110443 to L.A.H.).
Author information
Authors and Affiliations
Contributions
Research idea and study design: L.A.H., P.D.B., S.L.F., and P.C.N.; data acquisition: M.S., M.N., T.R.K., L.A.H.; data analysis/interpretation: M.S., L.A.H., K.E.L., E.v.P., T.R.K., J.L.S., A.L.C., P.C.N.; supervision or mentorship: L.A.H., P.C.N., P.D.B., and S.L.F. Primary responsibility to drafting the paper: M.S., L.A.H., E.v.P., J.L.S., M.N., P.C.N., P.D.B., and S.L.F. All authors contributed important intellectual content during iterative manuscript drafts or revisions, accepts personal accountability for the author’s own contributions, reviewed the document submitted for review, and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent and/or assent, as applicable, was obtained from participants and legal guardians at the time of participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Solomon, M.A., van der Plas, E., Langbehn, K.E. et al. Early pediatric chronic kidney disease is associated with brain volumetric gray matter abnormalities. Pediatr Res 89, 526–532 (2021). https://doi.org/10.1038/s41390-020-01203-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01203-w
This article is cited by
-
Self-concept and academic achievement in children with chronic kidney disease
Pediatric Nephrology (2024)
-
Common mental health conditions and considerations in pediatric chronic kidney disease
Pediatric Nephrology (2024)
-
Risk factors for neurocognitive impairment and the relation with structural brain abnormality in children and young adults with severe chronic kidney disease
Pediatric Nephrology (2023)
-
Associations between neurofilament light-chain protein, brain structure, and chronic kidney disease
Pediatric Research (2022)
-
Leveraging neuroimaging to understand the impact of chronic kidney disease on the brain
Pediatric Nephrology (2022)