Abstract
Background
Insulin-like growth factors (IGFs), and their binding proteins (IGFBPs), play a significant role in cardiovascular function and may influence the pathobiology of PAH. We determined the diagnostic and prognostic value of IGF1 and IGFBP2 in pediatric PAH.
Methods
Serum was analyzed by ELISA for IGF1 and IGFBP2 in pediatric PAH subjects from the NHLBI PAH Biobank (PAHB, n = 175) and a cohort of asthmatic subjects (n = 46, age 0–21 years) as a chronic pediatric pulmonary disease control. Biomarkers were analyzed with demographic and clinical variables for PAH severity.
Results
Serum IGF1 was significantly lower in PAH compared to controls, while IGFBP2 was elevated in PAH subjects compared to controls. In the PAHB, IGF1 was negatively associated with mPAP and PVR, while IGFBP2 was positively associated with PVR and negatively associated with cardiac output and 6-min walk distance. Higher IGFBP2 levels were associated with use of prostacyclin therapy. IGFBP2 was associated with death, transplant, or palliative shunt with a Cox proportional hazard ratio of 8.8 (p < 0.001) but not IGF1 (p = 0.13).
Conclusions
Circulating IGFBP2 is a novel marker for pediatric PAH, which is associated with worse functional status, and survival. IGF axis dysregulation may be an important mechanistic target in pediatric pulmonary arterial hypertension.
Impact
-
Pediatric pulmonary hypertension is a severe disease, with poorly understood pathobiology.
-
There are few studies looking at the pathobiology of pulmonary hypertension only in children.
-
The IGF axis is dysregulated in pediatric pulmonary arterial hypertension.
-
IGF axis dysregulation, with increased IGFBP2, is associated with worse clinical outcomes in pediatric pulmonary artery hypertension.
-
IGF axis dysregulation gives new insight into the disease process and may be a mechanistic or therapeutic target.
Similar content being viewed by others
Introduction
Pulmonary arterial hypertension (PAH) in children is a progressive and almost uniformly fatal disease characterized by sustained elevation of pulmonary arterial pressures and death from right ventricular failure.1 Pediatric PAH (World Symposium on Pulmonary Hypertension (WSPH) group 1) is a heterogeneous disease, which may be idiopathic (IPAH), familial or heritable (HPAH), or associated with congenital heart disease, infection, portal hypertension, and pulmonary venous/capillary diseases.2 The distribution of disease associations is different in children with a higher incidence of IPAH, HPAH, and congenital heart disease rather than connective tissue disease or infection.1,3,4
The growth and metabolic regulation of the pulmonary vasculature and right ventricle in PAH is incompletely understood but is characterized by perivascular infiltration of inflammatory cells and loss of small arteries and capillary beds.5 Insulin-ike growth factors (IGF1/IGF2) are essential in the growth of endothelium and smooth muscle, development of vascular networks, and cardiomyocyte development and function.6 IGF actions are mediated by the IGF1/IGF2 receptors; in turn, IGF receptor interactions are modulated by a family of seven high-affinity IGF-binding proteins (IGFBP1–7).7 While IGF1 is the primary mediator, most IGF1 is bound to and stabilized by the IGFBPs that facilitate transport and interaction of IGF with the IGF receptor and act as a reservoir for IGF1 in the circulation.8 Of the IGFBPs, IGFBP2 has non-IGF-mediated functions, including translocation to the nucleus, affecting gene expression, with cell growth and developmental effects.9,10
IGFBP2 has also been implicated in cardiopulmonary disease. Circulating IGFBP2 was associated with pulmonary fibrosis and with a treatment response.11 IGFBP2 has also shown promise differentiating heart failure severity, with additional diagnostic benefit above standard biomarkers.12 The role of IGFBP2 is poorly understood in PAH, but its IGF-independent actions are well described in angiogenesis. In diseases such as cancer, IGFBP2 has been shown to have a pro-angiogenic and mitogenic effect contributing to disordered vascular growth, a mechanism that may have relevance in PAH.9
Elevation of circulating IGFBP2 was identified in a proteomic analysis of adult PAH subjects against controls.13 Given the activity of IGFBP2 in abnormal vascular growth, the role of IGF1 in cardiomyocyte function, and the elevated IGFBP2 in adult PAH subjects, this study examines the relationship of IGFBP2 and IGF1 as predictors of pediatric PAH severity.
Methods
In this multicenter cross-sectional study of pediatric PAH, we determined and analyzed IGF1 and IGFBP2 concentrations from a cohort of pediatric subjects with WSPH group 1 PAH and a cohort of children with asthma as chronic lung disease controls.
Study cohorts
NHLBI PAH Biobank (PAHB) enrollment protocol and informed consent was approved by the Cincinnati Children’s Hospital Medical Center Institutional Review Board (IRB). Control samples from Johns Hopkins Hospital were collected after informed consent or, with waiver of consent, by Johns Hopkins investigators. All cohorts have been approved by the Johns Hopkins University IRB.
Pulmonary hypertension enrollees
NHLBI PAH Biobank
The PAHB is an NHLBI (HL105333) funded resource of biological samples and genetic and clinical data for the PAH research community, with five pediatric enrolling centers (www.pahbiobank.org). De-identified biological samples and clinical data on enrollees (n = 175, age <21 years, Table 1) were available for analysis. The PAHB collects subject clinical parameters at enrollment, demographics and comorbidities, New York Heart Association/WSPH functional class, 6-min walk distance (6MWD), drug therapy, and right heart catheterization data. A subset of the PAHB cohort had right heart catheterizations within 6 months of enrollment (n = 29) and were used for invasive cardiac hemodynamic analysis. Mortality, transplant, and palliative shunt (Pott’s shunt or atrial septostomy) was collected prospectively and analyzed for the entire cohort.
Pediatric asthma subjects
A cohort of asthmatic pediatric subjects was used as a chronic pediatric pulmonary disease (n = 46, 5–17 years, Table 1) cohort. Random participants with moderate-to-severe asthma were enrolled in Environmental Control as Add-on Therapy in Childhood Asthma (NCT02251379), a randomized clinical trial comparing controller medication alone to controller medication plus home-based environmental intervention. All subjects had moderate-to-severe persistent asthma and were on stepwise chronic medical therapy (mean step 5 corresponding to inhaled corticosteroid and long-acting beta agonist).14 Samples were collected with Johns Hopkins IRB approval with informed consent and with subject assent where appropriate.
Methods
Laboratory methods
Serum samples were assayed for total IGF1 and IGFBP2 using commercial enzyme-linked immunosorbent assays (R & D Systems, Minneapolis, MN; Cat # DGB200, Human IGFBP-2; Cat # DG100, Human IGF1). Samples were assayed according to the manufacturer’s instructions, in the same laboratory and by the same technician. Assays were analyzed using KC4 (Bio-Tek Instruments, Winooski, VT). All assays were blinded to clinical outcomes and only unblinded for statistical analysis.
Statistical analysis
Total IGF1 and IGFBP2 concentrations are presented as median and interquartile range (IQR). There are normative values for IGF1 based on age and sex; thus IGF1 values were converted to Z-scores to compare the PAHB to a healthy population and to compare the asthmatic subject to the PAHB. Normative values are not available for IGFBP2. Biomarkers were natural log transformed for regression analysis in order to normalize distribution. Demographic and functional data are presented as median and IQR or median, percent, and range as appropriate. The results from receiver operating characteristic (ROC) curves and Youden analysis were used to determine the sensitivity and specificity of IGF1 and IGFBP2 at discriminating PAH from controls. Differences in categorical variables were assessed using Wilcoxon signed-rank test or, for continuous variables, Spearman’s rank correlation. In the PAHB, a subset of subjects (n = 29) had hemodynamic data collected within 6 months of the enrollment blood sample; this subset was used to analyze hemodynamic data against biomarker levels. Regression analysis was performed, adjusted for age and sex, using linear and logistic regression for continuous and categorical variables, respectively. Kaplan–Meier analysis was performed to evaluate time to a composite clinical worsening outcome of death, transplant, or palliative shunt (Pott’s shunt or atrial septostomy) with biomarkers dichotomized at the median and follow-up time of 60 months. Cox proportional hazard model, adjusted for age, sex, and PAH subtype was used to assess risk of the composite clinical worsening outcome based on biomarker level. A p value <0.05 was considered statistically significant. Statistical analysis was performed using Stata (Version 15.1; 2018; StataCorp, LLC, College Station, TX).
Results
Subject demographics
All PAHB subjects were diagnosed with WSPH group 1 PAH, with serum samples collected at enrollment. There were 175 PAHB and 46 asthmatic controls available for analysis. The demographic characteristics of the PAHB cohort and the control cohort are shown in Table 1. Anthropometric data are presented for those with clinical evaluation within 6 months of enrollment (n = 29) to correspond with hemodynamic and functional data. The PAHB subjects had a median age of 12 years, with 59% female subjects. The median age and gender were not significantly different between the PAHB and the controls. The PAHB subjects were comprised of 48% IPAH and 46% with associated PAH (APAH). The APAH group was predominantly congenital heart disease (40%), with no shunt (14%), unrepaired shunt (6%), and repaired shunt (20%).
Hemodynamic and functional measures are shown in Table 1. The PAHB subjects with cardiac hemodynamics within 6 months of enrollment (n = 29) had a mean pulmonary arterial pressure (mPAP) of 45 mmHg and a median pulmonary vascular resistance index (PVRi) of 10.7 Wood units × m2, consistent with severe pulmonary hypertension. Functionally, within 6 months of enrollment, a 6MWD was available for 80 subjects aged >8 years with a mean of 422 m. In all, 34% of the PAHB cohort were treated with a prostacyclin analog (PCA) as another measure of disease severity.
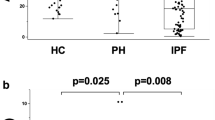
Serum IGF proteins in pediatric PAH
The lower limits of detection for the IGF1 and IGFBP2 assays were 18.2 and 4.4 ng/ml, respectively, with inter-plate coefficients of variation of 5% for IGF1 and 3.6% for IGFBP2. IGF1 values in the control cohort were consistent with the normal clinical IGF1 concentration range (IQR 100–600 ng/mL)15 and was confirmed by calculating Z-scores for the IGF1 value for each subject (Supplementary Fig. 1). The results of the serum IGF1 and IGFBP2 concentrations are detailed in Fig. 1a, b and Table 1 for both the PAHB and asthmatic control (median and IQR) cohorts (Fig. 1a, b). IGF1 was significantly lower in the PAHB compared with pulmonary disease controls (Table 1 and Fig. 1a, p < 0.0001). The Z-score distribution of IGF1 was lower in the PAHB compared to a normal distribution and was significantly lower in the PAHB compared to asthmatic subjects (p < 0.001, Supplementary Fig. 1). IGFBP2 was significantly elevated in the PAHB cohort compared with the pulmonary disease controls (Table 1 and Fig. 1b, p < 0.0001). Within PAH subtypes, IPAH subjects had a slightly higher IGF1 (131 ng/mL, 87–183, p = 0.014). There were no significant differences in IGF1 or IGFBP2 between other disease subtypes, although the cohorts were too small to draw conclusions. There was no significant difference in IGF1 and IGFBP2 between congenital heart disease subjects with a shunt, a repaired shunt, or no shunt (Supplementary Table 1).
IGFBP2 discriminates PAH from pulmonary disease controls
To determine whether IGF1 and IGFBP2 could discriminate PAH from controls, we used IGF1 and IGFBP2 values in the PAHB and the control cohort to generate the ROC curves (Fig. 2a, b). Serum IGF1 was able to identify the presence of PAH versus controls with an area under the curve (AUC) of 0.82 (p < 0.001), with the optimal cutoff established by Youden analysis of 177.3 ng/mL. This IGF1 threshold had a sensitivity of 73.9% and a specificity of 78.3%. IGFBP2 was able to identify the presence of PAH from the controls with an AUC of 0.80 (p < 0.001), with the optimal cutoff established by Youden analysis of 185 ng/mL. This IGFBP2 threshold had a sensitivity of 72.2% and a specificity of 80.4%.
a ROC curve of IGF1 in PAH Biobank subjects versus controls. AUC 0.82. Cut point for IGF1 of 177 ng/mL gives a sensitivity of 73.9% and a specificity of 78.3%. b ROC curve of IGFBP2 in PAH Biobank subjects versus controls. AUC 0.80. Cut point for IGFBP2 of 185 ng/mL gives a sensitivity of 72.2% and a specificity of 80.4%.
IGF1 and IGFBP2 correlate with hemodynamic severity
We evaluated the correlation of IGF1 and IGFBP2 with major hemodynamic variables in the PAHB. Spearman Rho values are shown in Table 2 for PAHB subjects with cardiac catheterization within 6 months (n = 29, Table 2) of enrollment. IGF1 was positively correlated with cardiac output (CO) and negatively correlated with mPAP, PVR, and PVRi, whereas IGFBP2 was strongly negatively correlated with CO and positively correlated with PVR and PVRi.
When linear regressions were adjusted for age and sex (Table 2, n = 29), IGF1 was negatively associated with mean right arterial pressure (mRAP), mPAP, pulmonary capillary wedge pressure (PCWP), and PVR. IGFBP2 was positively associated with PVR and negatively associated with CO but had no significant association with either mPAP, mRAP, or PCWP.
IGFBP2 concentration correlates with prostacyclin use
Continuous infusion/inhalation prostacyclin therapy (IV/SQ PCA) was used as a marker of more severe disease. We explored the relationship of serum IGFBP2 levels and IV/SQ PCA therapy compared with any other combination of enteral therapies (Fig. 3a). In all, 49% of PAH subjects (n = 85) were treated with PCA, with 34% (n = 59) receiving IV/SQ PCA. Only 1 subject was treated exclusively with a PCA. Serum median IGFBP2 concentration was significantly higher in the IV/SQ PCA administration groups compared to any other therapies without PCA (Fig. 3b).
a IGFBP2 concentration in PAH subjects on a PDE5 inhibitor, a PDE5 inhibitor and an ERA, a PDE5 inhibitor and IV/SQ PCA, or a combination of PDE5 inhibitor, ERA, and IV/SQ PCA. b IGFBP2 concentrations in PAH subjects on an IV/SQ PCA and any other therapy versus subject not on IV/SQ PCA and any other therapy.
Serum IGFBP2 concentrations were associated with functional outcomes and mortality
As shown in Table 2, using a linear regression model adjusted for age and sex, higher IGFBP2 was significantly associated with shorter 6MWD. For every 2.5-fold increase in IGFBP2 (1 natural log unit), subjects had a 140-m shorter 6MWD (p = 0.008). IGF1 was positively associated with 6MWD with subjects walking 130 m more for every natural log increase in IGF1 (p = 0.017).
IGFBP2 was positively associated with mortality with a log-odds of 1.193 (p = 0.016). Thus the odds ratio of death with 1 natural log unit higher IGFBP2 was 6.78. The median IGFBP2 concentration in subjects who died was 540 ng/mL compared with 262 ng/mL in survivors (p = 0.009). For subjects with an IGFBP2 concentration in the top quartile (>379 ng/mL), the relative risk of death was 12.4 (p = 0.023, 95% confidence interval (CI) 1.4–107; number needed to treat [harm] 11.6) compared with subjects with an IGFBP2 concentration in the bottom 3 quartiles. Analysis of the composite clinical worsening outcome (death, transplant, palliative shunt) was conducted using a Cox proportional hazard model, adjusted for age, sex, and PAH subtype (Supplementary Table 2). For every 2.5-fold increase in IGFBP2, the hazard ratio for death, transplant, or shunt was 8.8, (Supplementary Table 2, 95% CI 2.7–28.6; p < 0.001) indicating that IGFBP2 was independently and strongly predictive of clinical worsening over time. The Cox proportional hazard model was not significant for IGF1 (hazard ratio 0.45 95% CI 0.16–1.3, p = 0.13). In Kaplan–Meier analysis (Fig. 4), IGFBP2 above the median was associated with time to death, transplant, or palliative shunt (p = 0.02).
Discussion
PAH is a severe disease with an extremely high burden of morbidity and mortality. We sought to find new circulating biomarkers that may lead to a better understanding of PAH pathobiology. IGFs are an interesting target because of their essential roles in myocardial function and metabolism and smooth muscle and endothelial cell growth.8 This study demonstrates, for the first time, dysregulation of IGF1 and IGFBP2 in pediatric PAH and that IGFBP2 is elevated in pediatric PAH, with a significant association with disease severity and death.
IGF1 is a ubiquitous protein expressed as part of the pituitary growth hormone axis6,16 where growth hormone stimulates release of IGF1 from the liver.6 IGF1 is mediated by binding the cell surface IGFR1 tyrosine kinase coupled receptor, triggering a signaling cascade influencing growth.6 IGF1 exerts particular effects in the heart; IGF1 is necessary for fetal/neonatal cardiomyocyte proliferation and maturation, upregulation of IGF1 is seen in animal models of ventricular hypertrophy, and increased pressure or volume overload, while IGF1 deficiency results in heart failure and death.6,17,18 Equally important, IGF1 modulates vascular tone and nitric oxide production, which, when abnormal, contribute to pulmonary hypertension.16 In this study, lower IGF1 was associated with higher pulmonary artery pressures and lower CO, reflecting the previously described essential role for IGF1 in the cardiovascular system.8
While IGF1 is essential for cardiac function and growth, IGFBPs have been shown to have an evolving IGF1-independent role in adverse growth and cellular remodeling of the heart and worse outcomes after cardiovascular events.19 In normal physiology, IGFBP2 has been shown to be mostly growth inhibitory, binding IGF1 that is mitogenic for vascular growth. In disease, however, IGFBP2 expression and regulation may be very altered, with increased IGF1-independent effects on vascular growth and function.20 For example, IGFBP2 plays a role in dysregulated vascular growth in aggressive cancers. In human neuroblastoma cells, IGFBP2 overexpression upregulated vascular endothelial growth factor transcription, while in vitro studies have shown increased levels of IGFBP2-activating integrin receptors and promoting cell migration required for new vessel growth.20,21,22 Other studies show regulation of IGFBP2 in response to hypoxia-inducible factor (HIF)-1α, causing upregulation of IGFBP2,9 while an in silico model suggested that upregulation of IGFBP2 potentiated HIF-1α expression levels, further driving vascular growth.23
In this study, we demonstrate that IGF1 is decreased and IGFBP2 is elevated in pediatric PAH subjects compared with subjects with another chronic pulmonary disease and that IGFBP2 is significantly associated with markers of disease severity (6MWD, PVR, CO, use of continuous infusion therapy, mortality). The etiology of PAH-mediated IGFBP2 elevation is currently unknown. But the pattern seen in these subjects is clear; in PAH, there is an elevated IGFBP2 concentration and a lower available IGF concentration. IGFBP2’s hemodynamic and functional associations may also be independent of IGF concentration, a pattern of vascular dysfunction seen in patients with pulmonary fibrosis as well as multiple cancers.9,11 Although IGFBP2 has been shown to drive abnormal vascular growth in cancer, it has not been evaluated in pulmonary hypertension. However, the same mechanisms of endothelial and vascular smooth muscle dysfunction may be relevant, namely, abnormal pulmonary vascular development, metabolic dysregulation, abnormal vascular tone, and, in PAH, resultant right ventricular failure.6,13,16 Thus there may be a twofold insult from IGFBP2-mediated dysregulated vascular function and a relative deficiency of IGF from increased IGFBP2 binding, causing hemodynamic compromise with increased PVR and decreased CO. The reciprocal associations of functional outcomes of IGF1 and IGFBP2 suggest that dysregulation of this axis, with increased IGFBP2, and resultant worsening IGF availability in PAH may be a mechanism of worsening disease. Taken together, the IGF axis is essential for normal cardiopulmonary development and function and is dysregulated in pediatric PAH with strong associations with severity and survival.
This study is the first to explore IGF1 and IGFBP2 in pediatric PAH. While the overall size of the cohort is large for a pediatric PAH study, limitations include the diverse nature of pediatric PAH, as well as the limited number of subjects with contemporaneous hemodynamic and functional data. Further, this has not yet been validated in an independent cohort. The study is cross-sectional, with subjects enrolled at different phases of disease and blood samples collected only at enrollment. Thus it is not possible to associate IGFBP2 longitudinal changes with response to treatment. There were six deaths in the PAHB group limiting the power to assess mortality, although the study was well powered for the composite outcome. There was still a significant association with mortality in the PAHB, which mirrors the pattern seen in adult studies. Future studies should focus on a longitudinal analysis of IGF1 and IGFBP2 in pulmonary hypertension to validate this model, assess response to treatment, and to develop a better prognostic model for outcomes.
Given the essential function of IGF1 and IGFBP2 in vascular and cardiomyocyte growth, maturation, and function, these proteins may play a key role in the pathogenesis of PAH. IGFBP2 may be a useful prognostic biomarker of pediatric PAH and have the potential as the focus for development of new therapeutic targets.
References
Frank, B. S. & Ivy, D. D. Diagnosis, evaluation and treatment of pulmonary arterial hypertension in children. Children 5, 44 (2018).
Galie, N., McLaughlin, V. V., Rubin, L. J. & Simonneau, G. An overview of the 6th World Symposium on Pulmonary Hypertension. Eur. Respir. J. 53, 1802148 (2019).
Tuder, R. M. et al. Relevant issues in the pathology and pathobiology of pulmonary hypertension. J. Am. Coll. Cardiol. 62(25 Suppl), D4–D12 (2013).
Tuder, R. M. & Voelkel, N. F. Angiogenesis and pulmonary hypertension: a unique process in a unique disease. Antioxid. Redox Signal. 4, 833–843 (2002).
Archer, S. L., Fang, Y. H., Ryan, J. J. & Piao, L. Metabolism and bioenergetics in the right ventricle and pulmonary vasculature in pulmonary hypertension. Pulm. Circ. 3, 144–152 (2013).
Delafontaine, P. Insulin-like growth factor I and its binding proteins in the cardiovascular system. Cardiovasc. Res. 30, 825–834 (1995).
Forbes, B. E., McCarthy, P. & Norton, R. S. Insulin-like growth factor binding proteins: a structural perspective. Front. Endocrinol. 3, 38 (2012).
Delafontaine, P. Insulin-like growth factor I and its binding proteins in the cardiovascular system. Cardiovasc. Res. 30, 825–834 (1995).
Yau, S. W., Azar, W. J., Sabin, M. A., Werther, G. A. & Russo, V. C. IGFBP-2 - taking the lead in growth, metabolism and cancer. J. Cell Commun. Signal. 9, 125–142 (2015).
Besnard, V. et al. Distinct patterns of insulin-like growth factor binding protein (IGFBP)-2 and IGFBP3 expression in oxidant exposed lung epithelial cells. Biochim. Biophys. Acta 1538, 47–58 (2001).
Guiot, J., Bondue, B., Henket, M., Corhay, J. L. & Louis, R. Raised serum levels of IGFBP-1 and IGFBP-2 in idiopathic pulmonary fibrosis. BMC Pulm. Med. 16, 86 (2016).
Berry, M. et al. Proteomics analysis reveals IGFBP2 as a candidate diagnostic biomarker for heart failure. IJC Metab. Endocr. 6, 5–12 (2015).
Hemnes, A. R. et al. Human PAH is characterized by a pattern of lipid-related insulin resistance. JCI Insight 4, e123611 (2019).
National Asthma Education and Prevention Program & Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma (National Heart Lung and Blood Institute, Bethesda, MD, 2007).
Insulin-Like Growth Factor 1 (IGF1), LC-MS and Insulin-Like Growth Factor-Binding Protein 3 (IGFBP3) Growth Panel, Serum. Edited by Mayo Clinic Laboratories, https://www.mayocliniclabs.com/test-catalog/Clinical+and+Interpretive/36365.
Delafontaine, P., Song, Y. H. & Li, Y. Expression, regulation, and function of IGF-1, IGF-1R, and IGF-1 binding proteins in blood vessels. Arterioscler. Thromb. Vasc. Biol. 24, 435–444 (2003).
Wood, A. W., Schlueter, P. J. & Duan, C. Targeted knockdown of insulin-like growth factor binding protein-2 disrupts cardiovascular development in zebrafish embryos. Mol. Endocrinol. 19, 1024–1034 (2005).
Ren, J., Samson, W. K. & Sowers, J. R. Insulin-like growth factor I as a cardiac hormone: physiological and pathophysiological implications in heart disease. J. Mol. Cell. Cardiol. 31, 2049–2061 (1999).
Motiwala, S. R. et al. Measurement of novel biomarkers to predict chronic heart failure outcomes and left ventricular remodeling. J. Cardiovasc. Transl. Res. 7, 250–261 (2014).
Pickard, A. & McCance, D. J. IGF-binding protein 2 - oncogene or tumor suppressor? Front. Endocrinol. 6, 25 (2015).
Azar, W. J. et al. IGFBP-2 enhances VEGF gene promoter activity and consequent promotion of angiogenesis by neuroblastoma cells. Endocrinology 152, 3332–3342 (2011).
McMullen, J. R. Role of insulin-like growth factor 1 and phosphoinositide 3-kinase in a setting of heart disease. Clin. Exp. Pharmacol. Physiol. 35, 349–354 (2008).
Lin, K. W., Liao, A. & Qutub, A. A. Simulation predicts IGFBP2-HIF1alpha interaction drives glioblastoma growth. PLoS Comput. Biol. 11, e1004169 (2015).
Acknowledgements
This study was supported by the National Institutes of Health/National Heart, Lung, and Blood Institute awards R01HL135114 and R01 HL150070 (to A.D.E., M.N., J.Y., R.D., D.V., W.C.N., D.I., and E.D.A.), R24 HL105333 (to W.C.N., M.W.P., D.I., and E.D.A.). Serum/tissue samples were provided by PHBI under the Pulmonary Hypertension Breakthrough Initiative (PHBI). Funding for the PHBI is provided under an NHLBI R24 grant, #R24HL123767 (to A.D.E.). M.G. was supported by the Pediatric Scientist Development Program. The Pediatric Scientist Development Program is supported by Award Number K12-HD000850 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. M.N was supported by The Matthew and Michael Wojciechowski Pulmonary Hypertension Pediatric Proof-of-Concept Grant (Dr. Robyn J. Barst Pediatric PH Research and Mentoring Fund Grant).
Author information
Authors and Affiliations
Contributions
M.G., J.Y., M.N., and A.D.E. planned the project, analyzed the data, and wrote the manuscript; M.G., S.B., and J.Y. performed the experiments and interpreted the results; M.G., R.D., and J.Y. performed statistical analysis; M.N., M.W., E.C.M., T.G., R.D., D.I., E.D.A., W.C.N., M.W.P., K.L., E.B.R., R.H., D.Y., and A.D.E. recruited subjects and performed research; all authors reviewed, revised, and approved the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All samples and clinical data have been collected with informed consent and assent where appropriate. All cohorts have been approved by the Institutional Review Board at their respective institution and by the Johns Hopkins University Institutional Review Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Griffiths, M., Yang, J., Nies, M. et al. Pediatric pulmonary hypertension: insulin-like growth factor-binding protein 2 is a novel marker associated with disease severity and survival. Pediatr Res 88, 850–856 (2020). https://doi.org/10.1038/s41390-020-01113-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01113-x