Abstract
Our climate has significantly changed, exceeding what the world has experienced over the last 650,000 years, and has been cited as the most significant health threat of the twenty-first century. Climate change is impacting health in unprecedented ways. While everyone is vulnerable to the health impacts associated with climate change, children are disproportionately affected because of their physical and cognitive immaturity. Climate change impacts that include rising temperatures, extreme weather, rising sea levels, and increasing carbon dioxide levels are associated with a wide range of health issues in children such as asthma, allergies, vector-borne diseases, malnutrition, low birth weight, and post-traumatic stress disorder. Pediatric health providers play a critical role in advancing the science and translating findings to improve public understanding about the link between climate changes and children’s health, and establishing strategies to address these issues. This review will provide an overview of research exploring the impact of climate change on children’s health impacts, as well as provide recommendations for pediatric research moving forward.
Similar content being viewed by others
Introduction
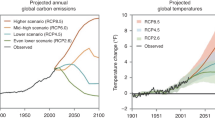
Our climate has significantly changed exceeding what the world has experienced over the last 650,000 years, and has been cited as the most significant health threat of the twenty-first century.1,2 The earth’s temperature is increasing, mainly as a result of human activity such as burning fossil fuel and greenhouse gas emissions. In 2019, record breaking heat waves have been reported globally—June was recorded as the warmest ever recorded in human history.3 All of these impacts affect human health worldwide.4
Health impacts can result from direct exposures patterns (e.g., heat waves, poor air quality), or indirectly (e.g., water availability, food quality). Figure 1 illustrates the most significant climate change impacts including rising temperatures, more extreme weather, rising sea levels, and increasing carbon dioxide levels, their effect on exposures, and the subsequent health outcomes that can result from these changes in exposures.5
Impact of climate change on human health From: Centers for Disease Control and Prevention https://www.cdc.gov/climateandhealth/effects/
Climate change can affect health by impacting the severity or frequency of health problems and by creating health issues where they have not previously occurred. Pre-existing health conditions, socioeconomic status, and life stage all contribute to vulnerability to climate-related and weather-related health effects. Social and behavioral factors that may influence health outcomes includes age, gender, race, ethnicity, poverty, housing, level of education, access to care, community health resources, and pre-existing health condition.6
Over the past decade, the number of scientific papers on health and climate change has more than tripled.4 This review will discuss the evidence to date on pediatric health outcomes from each of climate change such as rising temperatures as well as provide a roadmap for pediatric research moving forward.
Children’s vulnerability
While everyone is vulnerable to the health impacts associated with climate change, children are disproportionately affected because of their physical, physiologic, and cognitive immaturity.7 According to the World Health Organization, it is estimated that 88% of the existing global burden of disease attributable to climate change occurs in children less than 5 years old.8 Children in low-income countries that already experience a higher burden of disease and limited capability to adapt are even more affected by the harmful effects of climate change.8
Children are particularly vulnerable to detrimental health impacts from climate change. Exposures affecting the child begin before conception; thus, the parent’s environmental exposures have great importance.9 Throughout the life course, the environment needs to be safe. During the fetal period, the tissues and organs of embryos and fetuses are rapidly growing and developing. This time in development gives children unique periods of vulnerability. If an exposure occurs during these development phases, it can cause irreparable damage by interfering and manipulating the delicate and sensitive mechanisms in the body.7,10
Children have a higher exposure to air, food, and water per unit of body weight than adults.7 Unlike adults, due to immature detoxification systems and long lifespans, children do not have the biological capacity to adapt and respond, allowing these detrimental effects to stay with the child later on in life and the ability to impact future generations.9 Additionally, they are altogether dependent on their caregivers and cannot appropriately respond to threats.11 All of these factors have significant effects on physical, mental, and community health, placing children at direct risk of injury or death.
Health impacts: reproductive and children’s health
Children spend more time than adults outdoors, breathe more rapidly than adults, and are still developing their respiratory systems. While current research on the specific impacts on children have tended to focus on respiratory diseases as a result of climate change on air quality, emerging data are linking climate changes to a broader range of health issues, such as the impacts of extreme heat events to prematurity.12
Asthma, allergies, other respiratory diseases
Rising temperatures, increasing precipitation and atmospheric carbon dioxide, are expected to increase levels of airborne allergens, allergic illnesses and increases in asthma episodes.13,14 High levels of particulate matter, nitrogen oxides, sulfur oxides, and other pollutants affect the development of the children’s lungs regardless of any pre-existing illness or chronic condition. Nitrogen oxide, nitrogen dioxide, and PM2.5 have been associated with a worsening of lung function, as evidenced by a decrease in FEV1.15,16
Because children are more likely to play and spend more time outdoors, they are more likely to develop asthma when exposed to pollutants and airborne allergens. High temperatures increase the amount of pollen produced in some plants and the distribution of aeroallergens, which contributes to the prevalence and severity of asthma and other respiratory diseases.17,18,19
School absenteeism has been significantly linked to asthma. Rising temperatures with resulting reduction in air quality is impacting childhood asthma rates and success in school.20,21 Other extreme weather events that can impact respiratory disease in children includes heavy precipitation and sea level rise, coupled with flooding that can lead to mold in homes and schools, increasing risk for a variety of health issues.20,22,23
Additionally, climate change creates longer, warmer, and drier seasons increasing the frequency and intensity of wildfires. The smoke and air pollution from wildfire can exacerbate asthma symptoms and trigger attacks.24,25
Heat-related illness
Extreme heat events are becoming more prevalent around the globe and are the leading cause of environmental deaths in the United States.16 High temperature extremes compromise the body’s ability to regulate its internal temperature. Loss of control of internal temperature can lead to heat cramps, heat exhaustion, heatstroke, and hyperthermia.26 Children are especially vulnerable to extreme heat because they have a high surface area to mass ratio, and must divert more cardiac output to their skin to dissipate heat.27,28 The primary health effects from children exposed to heat waves are dehydration, electrolyte imbalance, fever, renal disease, and heat stress.29
During the summer months, children spend more time playing outside and participating in vigorous activity, putting them at increased risk of heat-related illnesses. Exertional heatstroke is the leading cause of death in youth sports.30,31 Socioeconomic disparities are also prominent, as those who can afford air-conditioning in homes suffer less from heat-related illnesses.32
Neurodevelopmental effects
As the temperature goes up, air quality goes down. Emerging research are findings associations to exposure to air pollutants (e.g., nitrogen dioxide, PM2.5) with impacts on brain development such as intelligence and memory.33,34,35 These findings of neurotoxic effects are consistent with laboratory studies finding air-pollution-induced neurological damage.36,37
Cardiovascular disease
Cardiovascular disease is the number one cause of death among adults in the United States and is also costing the U.S. health-care system billions of dollars. Strategies are targeted at prevention from birth to adolescent age. However, climate change has been shown to have negative cardiovascular consequences to the fetus and to young children. Multiple studies report an association between maternal heat exposure during early pregnancy and in increased odds of congenital heart defects. Exposure increases are potentially larger in the spring and summer seasons due to the increased frequency and intensity of heat waves.38,39,40
Vector-borne disease
Rising temperatures and increased precipitation are impacting the burden of infectious diseases transmitted by insect vectors and through contaminated water. Increased precipitation creates environments that promote vector breeding. Rising temperatures have led to increases in the geographical range and transmission of vector-borne diseases such as Lyme disease, West Nile, Malaria, and Zika.41
Vector-borne diseases can result in serious, long-term health impacts. West Nile Virus has been linked to an increased rate of clinical depression even 8 years after initial infection.42 In addition, chronic Lyme disease, a tickborne illness, has been associated with neuropsychiatric symptoms, such as alterations in affect, behavior, cognition, and perception.43 Congenital Zika virus infection has been associated with microcephaly and birth defects. Children with evidence of Zika had at least one adverse outcome such as feeding difficulties, vision and hearing challenges.44 Asymptomatic children infected by Zika may be at risk for health problems later in life and should be monitored clinically.45
Waterborne infectious disease
Rising sea temperature, excess precipitation, and flooding contribute to increases of waterborne infectious disease. Waterborne diseases are caused by a variety of contaminants such as bacteria (e.g., Vibrio), biotoxins (e.g., algal blooms), and toxic chemicals (e.g., petrochemicals), which can lead to morbidity and mortality. It is predicted that rising sea temperatures will increase the growth and spread of bacteria and the number of people impacted by diseases caused by Vibrio bacteria such as cholera.41,46
Another concern is that extreme weather events, such as flooding can contaminate water with metals, chemicals, and toxicants released into the environment (e.g., Hurricane Harvey) increasing apprehension about long-term health impacts, particularly for children.41,47
Malnutrition
Climate has major consequences for changes in nutrition and food security, food production systems, food safety and safe drinking water.48,49 It is estimated that 600 million are sickened annually by consuming contaminated food and 420,00 of them die each year.50 This number is anticipated to continue to grow as the changing climate brings changes to the agricultural environment, pest, animal and human behaviors.49
Climate change will impact both the quantity and quality of the food produced globally as well as its equitable distribution.48,51,52 Climate change is associated with rising temperatures, as well as periods of drought and flooding altering the ability to grow traditional crops. All of these changes alter relationships among crops, pests that prey on them, and pathogens. Additionally, climate change exacerbates declining trends in pollinating insects, rising ground-level ozone concentrations, and declines in fishing yield particularly in regions with limited capacity to adapt to these variations.51,53,54
Altered rainfall patterns and increases in extreme weather events will impact the occurrence and persistence of bacteria, viruses, parasites, harmful algae, fungi and their vectors, and the patterns of their corresponding water and food-borne diseases and risk of toxic contamination. In addition, climate changes will result in greater risk of food contamination from persistent organic pollutants and heavy metals from changes in soils, variety of crops under cultivation, methods of cultivation, redistribution of sediments and long-range atmospheric transport.49
Maternal malnutrition can lead to low birth weight, morbidity, and mortality.10 Climate change is predicted to worsen malnutrition in the developing world. Extreme weather events and changes in temperature and precipitation patterns can directly damage or destroy crops and other food supplies. This may happen seasonally but is anticipated to become a chronic problem under changing climate conditions especially in sub-Saharan Africa and South Asia, where most of today’s food insecure live.52 Food availability will be compromised by projected yield declines across the crop, livestock and fisheries sectors.52
Globally, 76% of the population derive the majority of their daily protein from plants.55 This population is most vulnerable as climate change impacts are felt beyond yield and availability. Rising CO2 levels are already altering the nutritional composition of crops. Elevated atmospheric CO2 is anticipated to widen the disparity in protein intake within countries, with plant-based diets being the most valuable.56 Staple food crops such as potatoes, barley, rice, and wheat that are primary sources of dietary protein for many countries, result in reduced protein content when cultivated at elevated CO2 levels.57
By 2050, assuming today’s diets and levels of income inequality, an additional 148.4 million of the world’s population may be placed at risk of protein deficiency because of CO2. In India, an additional 53 million people may become at risk.56
It is predicted that by the end of the twenty-first century one half of the world’s population could face severe food shortages due to the impact of rising temperatures on staple food crops.58 This will add to upward pressure on international food prices, in a time where global food supply needs are projected to increase by 60% from 2006 to 2050 to meet the needs of a growing population and changing diets.48,52
The world population grows by approximately 83 million people annually, despite declining fertility levels, and is anticipated to continue over time.59 This continued population growth, in combination with climate change, may overwhelm global crop production. It is anticipated that food security and nutritional adequacy, in the context of the rapidly evolving conditions that result from climate change, will be a major determinant of the next century’s global burden of disease.51
Mental health impacts
Climate change-driven events not only threaten physical health but also take a significant toll on mental health and wellbeing. Children living in geographic regions most vulnerable to the impacts of climate change, with less resilient infrastructure and/or with fewer supports, are most at-risk. The children anticipated to be most adversely impacted by climate change are the 85% of the world’s children who live in developing countries, children living in poverty, and some communities of color.60,61
The potential mental health consequences of climate change range from stress and distress symptoms to clinical disorders, e.g., anxiety, depression, post-traumatic stress, and suicidality. These consequences can be the result of either exposures to short-lived or prolonged climate- or weather-related events and their health consequences. These mental health impacts can interact with other health, social, and environmental stressors to diminish an individual’s wellbeing.62 Children and adolescents, in particular, are more susceptible to traumatic events that may result in long-term negative effects on health, social, and behavioral outcomes.11,61
It is predicted that the primary way in which children’s mental health will be impacted is through extreme weather events. Exposure to extreme weather events and climate-related disasters and ensuing family stress,63 displacement64 and interruption in their social support system,65 and are at risk for the development of post-traumatic stress disorder (PTSD) and other mental health problems including anxiety, sleep disorders, depression, panic, phobias anxiety, phobias and panic, substance abuse and attachment disorders.63,66,67,68,69,70 While prevalence of PTSD following climate-related disasters is typically in the range of 15–30%,71 in a study of primary school students in Thailand it was reported to be as high as 57.3% in the aftermath of the Asian tsunami.72
Children may suffer other psychological effects from traumatic exposures of climate-related disasters. The accompanying disruptions in their environment and family and social support may include adverse impacts on their capacity to regulate emotions, behavioral or adjustment problems, increased cognitive deficits, impaired language development and learning problems.64,68,69,73,74 Mental health services must be part of the disaster planning to meet the needs of children.
In an analysis of the 2017 Atlantic hurricane season which brought Hurricanes Maria, Harvey, and Irma, researchers identified several factors that increased the likelihood of severe mental health consequences. Several risk factors including minimal warning period, no options for evacuation, extended power outages, personal loss, displacement, and death of others, placing survivors at higher risk for psychopathologies.75 Domestic abuse, including child abuse, often increases in young families who have experienced extreme-weather events and climate-related disasters, such as Hurricane Katrina.76,77,78,79 Finally, repeated and sustained stressful early life events which might be anticipated in the context of climate change, can predispose children to adverse mental health outcomes later in life.80
Reproductive health
As temperatures continue to increase in many regions of the world, consideration of its impact on birth outcomes is critical.80,81 While the study of the potential influences on pregnancy and prenatal complications related to climate change is an emerging area of research, there is strong evidence that extreme heat and air pollution can lead to preterm birth and low birth weight.82,83,84 Exposure to air pollution during pregnancy has also been linked to decreased lung function in infancy and childhood and asthma.85 Other health outcomes that have been linked to extreme heat include congenital cataracts86 and sudden infant death.87
Pregnant women are less able to regulate the temperature of their bodies.88 It is believed that stress from a rising body temperature could also trigger an inflammatory response that constricts a pregnant woman’s vasculature, making it harder for blood carrying oxygen to reach the placenta and which can compromise the fetus.89 The dehydration that is associated with overheating may also be significant because it decreased the amount of amniotic fluid which is associated with fetal death. Temperature-sensitive proteins in the vessels may play a role through vasodilation in the placenta which in turn decreases blood pressure and therefore blood supply to the fetus. Associations between extreme heat and preterm delivery have been supported in a number of studies.90,91,92,93
Conclusions
Pediatric health providers have an important role in advancing the science and implementing approaches to helping children, families and society cope with its impacts. Evidence indicates that the health and wellbeing of children are already being affected by climate change. These changes highlight the critical need for us to consider the consequences of these environmental changes on health, particularly in children whose developing systems are more vulnerable to these extreme exposures and dependent upon adults to protect them from these hazards. Projections of continued global warming and associated health impacts underscore the urgency to enact proactive policies that reduce greenhouse gases. There is strong consensus that thousands of lives in the U.S. could be saved and hundreds of billions of dollars in health-related economic benefits gained each year with strong policies that lower greenhouse gas emissions.41,62
Despite progress in research exploring pediatric health outcomes associated with climate changes, there remain gaps in our understanding of (1) long-term health impacts (including physical and mental health), (2) best practices for addressing emerging health issues, and (3) methods for mitigating risk. It has been suggested that a consortium of global experts be established to develop research agendas to identify and address the specific needs of children worldwide.11 There is a critical need for researchers to employ new methodologies to improve the attribution of climate change to pediatric health impacts with a consideration of the complex array of societal modifiers such as socioeconomic status.4
Specific areas where gaps exist in the science include surveillance of the long-term effects of exposure to climate changes, especially mental health impacts. Research needs to explore how psychological stress acts synergistically with other forms of environmental exposures to cause adverse mental health effects and incorporating key mental health outcomes in health impacts assessments under a variety of climate change scenarios.94
In addition to studying direct health impacts, research efforts are needed to study impacts from indirect effects such as reductions in the security and quality of food and water that are anticipated, and will surely impact children’s growth and development and health in general.48
Another important research focus is the impact of climate changes on children’s health and school attendance. We know that school attendance is aligned with future success in adulthood, yet rising temperatures, poor air quality, mold and other environmental exposures from climate changes can negatively impact children’s health increasing absenteeism.20,29 Studies exploring outdoor air quality, the implementation of the Environmental Protection Agency’s (EPA’s) Air Quality Flag program (designed to alert communities about poor air quality), and its impact on reducing school absenteeism from respiratory diseases are currently underway. The use of programs such as the EPA Air Quality Flag program to educate and empower school personnel, children, and communities about the association between air quality and respiratory health, along with ways to adapt school activities (such as recess, sports) to reduce illness, are important to protecting children’s health. The cost-effectiveness of these and other measures to protect children will be necessary to justify future programs.
There is also a need to identify communities that are most vulnerable to detrimental health impacts of climate change, where resources are limited and risks are high. Research that explores best practices for enhancing public health and health-care infrastructures are needed, along with improving risk communication and public health education about potential health risks. Efforts to improve early-warning systems and public education to create a greater awareness of risks by the public may translate to more successful mitigation and adaptation strategies.94
It is essential that the health-care sector reframe climate change as a health issue, advocating for health as a cross-cutting theme for overall adaptation strategies. It must also advocate for increased awareness and a better understanding of the relationship between climate and health, while integrating evidence into both policy and practice. Research aimed at improving the capabilities of health-care and emergency services to address disasters is needed to ensure that risks are understood and that best practices are identified, communicated, and implemented. Building resiliency in health-care settings must go beyond planning for the delivery of clinical services, but also include an evaluation of climate risks and community vulnerability combined with resilience planning.94
Low-carbon and resilience strategies for the health-care sector are offered in the report Climate Smart Health Care. Over time, research has shown improvements in lowering carbon footprints, employee and patient health, and community benefits when health-care systems adopt low-carbon strategies. In many cases, a reduction in operating costs is also realized. Pediatric health providers can become involved in promoting these efforts in their institutions.95
Pediatric health providers play a critical role in advancing the science and translating findings to improve public understanding about the link between climate changes and children’s health, and establishing strategies to address these issues.
Disclaimer
The ATSDR and EPA did not play any role in the design of this study; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the manuscript for publication. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
Costello, A. et al. Managing the health effects of climate change. Lancet 373, 1693–1733 (2009).
Parry, M. L., Canziani, O. F., Palutikof, J. P., van der Linden, P.J., & Hanson, C.E. (eds). Climate Change 2007: Impacts, Adaptation and Vulnerability, 1st edn (Cambridge University Press, Cambridge, 2007).
Copernicus Climate Change Service. Another exceptional month for global average temperatures [Internet]. https://climate.copernicus.eu/another-exceptional-month-global-average-temperatures (2019).
Watts, N. et al. The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet 391, 581–630 (2018).
Centers for Disease Control and Prevention. Climate effects on health [Internet]. https://www.cdc.gov/climateandhealth/effects/default.htm (2014).
U.S. Global Change Research Program. The impacts of climate change on human health in the United States: a scientific assessment [Internet]. https://health2016.globalchange.gov/ (2016).
Etzel, R. A. & Balk, S. J. Pediatric Environmental Health, 4th edn (American Academy of Pediatrics, 2018).
United Nations International Children’s Emergency Fund. Unless we act now: the impact of climate change on children [Internet]. https://www.unicef.org/publications/index_86337.html (2015).
Sheffield, P. E. & Landrigan, P. J. Global climate change and children’s health: threats and strategies for prevention. Environ. Health Perspect. 119, 291–298 (2011).
Rylander, C., Øyvind Odland, J. & Manning Sandanger, T. Climate change and the potential effects on maternal and pregnancy outcomes: an assessment of the most vulnerable-the mother, fetus, and newborn child. Glob. Health Action 6, 19538 (2013).
Stanberry, L. R., Thomson, M. C. & James, W. Prioritizing the needs of children in a changing climate. PLoS Med. 15, e1002627 (2018).
Ahdoot, S. & Pacheco, S. E. Global climate change and children’s health. Pediatrics 136, e1468–e1484 (2015).
D’Amato, G., Vitale, C., Lanza, M., Molino, A. & D’Amato, M. Climate change, air pollution, and allergic respiratory diseases: an update. Curr. Opin. Allergy Clin. Immunol. 16, 434–440 (2016).
Demain, J. G. Climate change and the impact on respiratory and allergic disease: 2018. Curr. Allergy Asthma Rep. 18, 22 (2018).
McGeachie, M. J. et al. Patterns of growth and decline in lung function in persistent childhood asthma. N. Engl. J. Med. 374, 1842–1852 (2016).
Payne-Sturges, D. C. et al. Healthy air, healthy brains: advancing air pollution policy to protect children’s health. Am. J. Public Health 109, 550–554 (2019).
Ariano, R., Canonica, G. W. & Passalacqua, G. Possible role of climate changes in variations in pollen seasons and allergic sensitizations during 27 years. Ann. Allergy Asthma Immunol. 104, 215–222 (2010).
Patz, J. A., Frumkin, H., Holloway, T., Vimont, D. J. & Haines, A. Climate change: challenges and opportunities for global health. JAMA 312, 1565–1580 (2014).
Ziska, L. et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc. Natl. Acad. Sci. USA 108, 4248–4251 (2011).
Chalupka, S. & Anderko, L. Climate change and schools: implications for children’s health and safety. Creat Nurs. 25, 249–257 (2019).
Park, J. Temperature, test scores, and human capital production [Internet]. Mimeo. http://scholar.harvard.edu/files/jisungpark/files/temperature_test_scores_and_human_capital_production_-_j_park_-_1-18-17.pdf (2017).
Casas, L., Espinosa, A. & Pekkanen, J. et al. School attendance and daily respiratory symptoms in children: influence of moisture damage. Indoor Air 27, 303–310 (2017).
Baldacci, S. et al. Allergy and asthma: effects of the exposure to particulate matter and biological allergens. Respir. Med. 109, 1089–1104 (2015).
NASA Global Climate Change. Lightning sparking more boreal forest fires [Internet]. https://climate.nasa.gov/news/2602/lightning-sparking-more-boreal-forest-fires/ (2017).
United States Environmental Protection Agency. Wildfire smoke: a guide for Public Health Officials [Internet]. https://www3.epa.gov/airnow/wildfire_may2016.pdf (2016).
Sarofim, M. C. et al. Ch. 2: Temperature-Related Death and Illness. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment (US Global Change Research Program, Washington, DC, 2016).
Falk, B. & Dotan, R. Child-adult differences in the recovery from high-intensity exercise. Exerc Sport Sci. Rev. 34, 107–112 (2006).
Landrigan, P. J. et al. The Lancet Commission on pollution and health. Lancet 391, 462–512 (2018).
Xu, Z. et al. The impact of heat waves on children’s health: a systematic review. Int. J. Biometeorol. 58, 239–247 (2014).
Centers for Disease Control and Prevention. Heat illness among high school athletes—United States, 2005−2009 [Internet]. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5932a1.htm (2010).
Bergeron, M. F. Reducing sports heat illness risk. Pediatr. Rev. 34, 270–279 (2013).
Schmeltz, M. T., Petkova, E. P. & Gamble, J. L. Economic burden of hospitalizations for heat-related illnesses in the United States, 2001–2010. Int. J. Environ. Res. Public Health 13, 894 (2016).
Clifford, A., Lang, L., Chen, R., Anstey, K. J. & Seaton, A. Exposure to air pollution and cognitive functioning across the life course-a systematic literature review. Environ. Res. 147, 383–398 (2016).
Xu, X., Ha, S. U. & Basnet, R. A review of epidemiological research on adverse neurological effects of exposure to ambient air pollution. Front. Public Health 4, 157 (2016).
Brockmeyer, S. & D’Angiulli, A. How air pollution alters brain development: the role of neuroinflammation. Transl. Neurosci. 7, 24–30 (2016).
Allen, J. L. et al. Developmental neurotoxicity of inhaled ambient ultrafine particle air pollution: parallels with neuropathological and behavioral features of autism and other neurodevelopmental disorders. Neurotoxicology 59, 140–154 (2017).
Bolton, J. L. et al. Prenatal air pollution exposure induces neuroinflammation and predisposes offspring to weight gain in adulthood in a sex-specific manner. FASEB J. 26, 4743–4754 (2012).
Auger, N., Fraser, W. D., Sauve, R., Bilodeau-Bertrand, M. & Kosatsky, T. Risk of congenital heart defects after ambient heat exposure early in pregnancy. Environ. Health Perspect. 125, 8–14 (2017).
Lin, S. et al. Maternal ambient heat exposure during early pregnancy in summer and spring and congenital heart defects—a large US population-based, case-control study. Environ. Int. 118, 211–221 (2018).
Zhang, W. et al. Projected changes in maternal heat exposure during early pregnancy and the associated congenital heart defect burden in the United States. J. Am. Heart Assoc. 8, e010995 (2019).
U.S. Global Change Research Program. The impacts of climate change on human health in the United States: a scientific assessment [Internet]. https://health2016.globalchange.gov/ (2016).
Nolan, M. S., Hause, A. M. & Murray, K. O. Findings of long-term depression up to 8 years post infection from West Nile virus. J. Clin. Psychol. 68, 801–808 (2012).
Gerstenblith, T. A. & Stern, T. A. Lyme disease: a review of its epidemiology, evaluation, and treatment. Psychosomatics 55, 421–429 (2014).
Satterfield-Nash, A. et al. Health and development at age 19−24 months of 19 children who were born with microcephaly and laboratory evidence of congenital Zika virus infection during the 2015 Zika virus outbreak—Brazil, 2017. Morb. Mortal Wkly. Rep. 66, 1347–1351 (2017).
Kapogiannis, B. G., Chakhtoura, N., Hazra, R. & Spong, C. Y. Bridging knowledge gaps to understand how Zika virus exposure and infection affect child development. JAMA Pediatr. 171, 478–485 (2017).
Semenza, J. C. et al. Environmental suitability of vibrio infections in a warming climate: an early warning system. Environ. Health Perspect. 125, 107004 (2017).
Environmental Integrity Project. Preparing for the next storm: learning from the man-made environmental disasters that followed Hurricane Harvey [Internet]. https://www.environmentalintegrity.org/wp-content/uploads/2018/08/Hurricane-Harvey-Report-Final.pdf (2018).
Intergovernmental Panel on Climate Change. Climate change and land: an IPCC special report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems [Internet]. https://www.ipcc.ch/srccl-report-download-page/ (2019).
World Health Organization. Food safety: Climate change and the role of WHO [Internet]. https://www.who.int/foodsafety/publications/all/climate_change/en/ (2019).
World Health Organization. WHO estimates of the global burden of foodborne diseases [Internet]. http://apps.who.int/iris/bitstream/handle/10665/199350/9789241565165_eng.pdf?sequence=1 (2015).
Myers, S. S. et al. Climate change and global food systems: potential impacts on food security and undernutrtion. Annu. Rev. Public Health 38, 259–277 (2017).
Food and Agriculture Organization of the United Nations. FAO strategy on climate change [Internet]. http://www.fao.org/3/a-i7175e.pdf (2017).
Burke, M. & Lobell, D. Climate effects on food security: an overview. Clim. Change Food Security Adv. Glob. Change Res. 37, 13–30 (2010).
Muller, C., Cramer, W., Hare, W. & Lotze-Campen, H. Climate change risks for African agriculture. Proc. Natl. Acad. Sci. USA 108, 4313–4315 (2011).
Food and Agriculture Organization of the United Nations. Food balance sheets, 1970−2011 [Internet]. http://www.fao.org/faostat/en/#data/FBS/visualize (2014).
Medek, D. E., Schwartz, J. & Myers, S. S. Estimated effects of future atmospheric CO2 concentrations on protein intake and the risk of protein deficiency by country and region. Environ. Health Perspect. 125, 087002 (2017).
Myers, S. et al. Increasing CO2 threatens human nutrition. Nature 510, 139–142 (2014).
Battisti, D. S. & Naylor, R. L. Historical warnings of future food insecurity with unprecedented seasonal heat. Science 323, 240–244 (2009).
United Nations Department of Social Economic and Social Affairs. The world population prospects: 2017 Revision [Internet]. https://www.un.org/development/desa/publications/world-population-prospects-the-2017-revision.html (2017).
Burke, S. E. L., Sanson, A. V. & Van Hoom, J. The psychological effects of climate change on children. Curr. Psychiatry Rep. 20, 35 (2018).
Trombly, J., Chalupka, S. & Anderko, L. Climate change and mental health. Am. J. Nurs. 114, 44–52 (2017).
U.S. Global Change Research Program. Fourth National Climate Assessment Volume II: impacts, risks, and adaptation in the United States [Internet]. https://nca2018.globalchange.gov/ (2018).
Simpson, D. M., Weissbecker, I. & Sephton, S. E. Extreme weather-related events: implications for mental health and well-being. In Climate Change and Human Well-Being: Global Challenges and Opportunities (ed. Weissbecker, I.) 57−78 (Springer, New York, 2011).
Pfefferbaum, B., Jacobs, A. K., Jones, R. T., Reyes, G. & Wyche, K. F. A skill set for supporting displaced children in psychological recovery after disasters. Curr. Psychiatry Rep. 19, 60 (2017).
Banks, D. M. & Weems, C. F. Family and peer social support and their links to psychological distress among hurricane-exposed minority youth. Am. J. Orthop. 84, 341–352 (2014).
Norris, F. H. et al. 60,000 disaster victims speak: part I. An empirical review of empirical literature,1981−2001. Psychiatry Interpers. Biol. Process 65, 207–239 (2002).
Council on Environmental Health. Global climate change and children’s health. Pediatrics 136, 992–997 (2015).
Dean, J. G. & Stain, H. J. Mental health impact for adolescents living with prolonged drought. Aust. J. Rural Health 18, 32–37 (2010).
Garcia, D. M. & Sheehan, M. C. Extreme weather-driven disasters and children’s health. Int. J. Health Serv. 46, 79–105 (2016).
Goldmann, E. & Galea, S. Mental health consequences of disasters. Annu. Rev. Public Health 35, 169–183 (2014).
Alisic, E. et al. Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. Br. J. Psychiatry 204, 335–340 (2014).
Piyasil, V. et al. Post-traumatic stress disorder in children after the tsunami disaster in Thailand: a 5-year follow up. J. Med. Assoc. Thail. 94, 138–144 (2011).
Clayton, S., Manning, C., Krygsman, K. & Speiser, M. Mental health and our changing climate: impacts, implications, and guidance [Internet]. http://ecoamerica.org/wp-content/uploads/2017/03/ea-apapsych-report-web.pdf (2017).
Fairbank, J.A., Putnam, F. W. & Harris, W. W. Child traumatic stress: prevalence, trends, risk, and impact. In Handbook of PTSD: Science and Practice. 2nd edn, 121−145 (Guilford Press, New York, NY, 2014).
Espinel, Z. & Shultz, J. Lessons from the 2017 Atlantic Hurricanes Predict Increasing Risks for Psychopathology from Extreme Storms throughout the 21st Century”. APA 2019; Abstract: 4−149.
Fritze, J., Blashki, G. A., Burke, S. & Wiseman, J. Hope, despair and transformation: climate change and the promotion of mental health and well-being. Int. J. Ment. Health Syst. 2, 13 (2008).
Harville, E., Taylor, C., Tesfai, H., Xiong, X. & Buekens, P. Experience of Hurricane Katrina and reported intimate partner violence. J. Interpers. Violence 26, 833–845 (2011).
Keenan, H., Marshall, S., Nocera, M. A. & Runyan, D. Increased incidence of inflicted traumatic brain injury in children after a natural disaster. Am. J. Preventative Med. 26, 189–193 (2004).
Yun, K., Lurie, N. & Hyde, P. S. Moving mental health into the disaster-preparedness spotlight. New Engl. J. Med. 363, 1193–1194 (2010).
Faravelli, C., Lo Sauro, C. & Godini, L. Childhood stressful events, HPA axis and anxiety disorders. World J. Psychiatry 2, 13–25 (2012).
Anderko, L., Schenk, B., Huffing, K. & Chalupka, S. Climate Change, Health, and Nursing: A Call to Action (Alliance of Nurses for Healthy Environments [Internet], Mount Rainier, MD, 2016). https://envirn.org/climate-change/cover-climate-change-health-and-nursing/.
Stieb, D. M., Chen, L., Eshoul, M. & Judek, S. Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ. Res. 117, 100–111 (2012).
Lamichhane, D. K., Leem, J.-H., Lee, J.-Y. & Kim, H.-C. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ. Health Toxicol. 30, e2015011 (2015).
Zhang, Y., Yu, C. & Wang, L. Temperature exposure during pregnancy and birth outcomes: An updated systematic review of epidemiological evidence. Environ. Pollut. 225, 700–712 (2017).
Korten, I., Ramsey, K. & Latzin, P. Air pollution during pregnancy and lung development in the child. Paediatr. Respir. Rev. 21, 38–46 (2017).
Van Zutphen, A. R., Lin, S., Fletcher, B. A. & Hwang, S.-A. A population-based case-control study of extreme summer temperature and birth defects. Environ. Health Perspect. 120, 1443–1449 (2012).
Auger, N., Fraser, W. D., Smargiassi, A. & Kosatsky, T. Ambient heat and sudden infant death: a case-crossover study spanning 30 years in Montreal, Canada. Environ. Health Perspect. 123, 712–716 (2015).
Poursafa, P., Keikha, M. & Kelishadi, R. Systematic review on adverse birth outcomes of climate change. J. Res. Med. Sci. 20, 397–402 (2015).
Kuehn, L. & McCormick, S. Heat exposure and maternal health in the face of climate change. Int. J. Environ. Res. Public Health [Internet] 14, https://doi.org/10.3390/ijerph14080853 (2017).
Carolan-Olah, M. & Frankowska, D. High environmental temperature and preterm birth: a review of the evidence. Midwifery 30, 50–59 (2014).
He, J.-R. et al. Ambient temperature and the risk of preterm birth in Guangzhou, China (2001–2011). Environ. Health Perspect. 124, 1100–1106 (2016).
Kloog, I., Melly, S. J., Coull, B. A., Nordio, F. & Schwartz, J. D. Using satellite-based spatiotemporal resolved air temperature exposure to study the association between ambient air temperature and birth outcomes in Massachusetts. Environ. Health Perspect. 123, 1053–1058 (2015).
Schifano, P. et al. Heat and air pollution exposure as triggers of delivery: a survival analysis of population-based pregnancy cohorts in Rome and Barcelona. Environ. Int. 88, 153–159. (2016).
Portier, C. J. et al. A Human Health Perspective on Climate Change: A Report Outlining the Research Needs on the Human Health Effects of Climate Change (Environmental Health Perspectives/National Institute of Environmental Health Sciences [Internet], Research Triangle Park, NC, 2010). www.niehs.nih.gov/climatereport.
Bouley, T. et al. Climate-smart Healthcare: Low-Carbon and Resilience Strategies for the Health Sector (Washington, DC: World Bank Group [Internet], Washington, DC, 2017). http://documents.worldbank.org/curated/en/322251495434571418/pdf/113572-WP-PUBLIC-FINAL-WB;hkG-Climate-smart-Healthcare-002.pdf.
Acknowledgements
Many thanks to Madison Schinstock for providing expert technical assistance in the preparation of the paper. This study was supported by the Agency for Toxic Substances and Disease Registry (ATSDR), cooperative agreement award number 1U61TS000238-05 (to the Mid-Atlantic Center for Children’s Health and the Environment and the Region 1 New England Pediatric Environmental Health Specialty Unit). The contents of this manuscript are the responsibility of the authors and do not necessarily represent the official views of ATSDR. The U.S. Environmental Protection Agency (EPA) supports the Pediatric Environmental Health Specialty Units (PEHSU) by providing funds to ATSDR under Inter-Agency Agreement number DW-75-92301-05. Neither EPA nor ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications.
Author information
Authors and Affiliations
Contributions
All named authors have agreed to the submission; Submission is not currently being considered for publication by another journal, and will not be published in any form without the consent of publishers. All have made substantial contributions to the development of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anderko, L., Chalupka, S., Du, M. et al. Climate changes reproductive and children’s health: a review of risks, exposures, and impacts. Pediatr Res 87, 414–419 (2020). https://doi.org/10.1038/s41390-019-0654-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0654-7
This article is cited by
-
Strategies to strengthen a climate-resilient health system: a scoping review
Globalization and Health (2023)
-
An efficient vector-borne disease prediction using SS optimization-based hybrid support vector random forest model
Signal, Image and Video Processing (2023)
-
Climate change-related health hazards in daycare centers in Munich, Germany: risk perception and adaptation measures
Regional Environmental Change (2023)
-
ALIMUS—We are feeding! Study protocol of a multi-center, cluster-randomized controlled trial on the effects of a home garden and nutrition counseling intervention to reduce child undernutrition in rural Burkina Faso and Kenya
Trials (2022)
-
Feature extraction and classification of climate change risks: a bibliometric analysis
Environmental Monitoring and Assessment (2022)