Abstract
Observational studies demonstrating reduced rates of infections, necrotizing enterocolitis (NEC), and mortality in preterm infants fed their own mother’s milk, as opposed to formula, have prompted endeavors to achieve similar effects with the right choice of food and food additives. In a systematic review of meta-analyses and randomized controlled trials (RCTs), we considered nutritional interventions aimed at reducing the rates of infections, NEC, or mortality in very preterm infants. The overall effects of particular interventions were presented as risk ratios with 95% confidence intervals. In RCTs, pasteurized human donor milk, as opposed to formula, reduced NEC but not infections or mortality. No differences emerged between infants receiving human or bovine milk-based fortifiers. Pooled data of small trials and a recent large RCT suggested that bovine lactoferrin reduced rates of fungal sepsis without impact on other infections, NEC, or mortality. Pooled data of RCTs assessing the use of prebiotic oligosaccharides found reduced infection but not mortality. Enteral L-glutamine (six RCTs) lowered infection rates, and enteral L-arginine (three RCTs) reduced NEC. A meta-analysis sensitivity approach found multiple-strain (but not single-strain) probiotics to be highly effective in reducing NEC and mortality. Thus, selected food components may help to improve outcomes in preterm infants.
Similar content being viewed by others
Background
Breastfeeding is recommended by the World Health Organization (WHO) for all infants, which in very preterm infants translates into pumped or expressed breast milk given via gavage. A multitude of observational studies indicate that mother’s own milk, as opposed to term or preterm formula, confers protection against invasive infection and necrotizing enterocolitis (NEC),1 and therefore lowers mortality. This protection afforded by mother’s milk appears to be little altered by pasteurization.2,3 These observations have fostered beliefs that food components actually do make a difference in the care of tiny preterm infants to prevent invasive infections and NEC. While availability of mother’s own milk cannot be studied by means of randomized controlled trials (RCT), other sources of milk and various food additives can and have been the subject of such trials. This review has been undertaken to summarize the evidence available, based on published meta-analyses and results of RCTs.
Methods
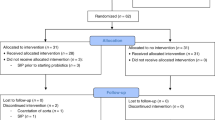
To identify RCTs that investigated nutritional interventions in premature infants aimed at reducing rates of invasive infections, NEC, or mortality in very preterm infants as primary or secondary endpoints, we performed a Medline search via PubMed (https://www.ncbi.nlm.nih.gov/pubmed/). A variety of search terms were applied (search concept: Premature infant AND (enteral OR oral OR nutrition) AND RCT). The detailed search strategy is available in Supplementary File 1. Only articles on RCTs or meta-analyses published in English were considered. The search yielded 2924 hits, of which 69 were relevant to this review. The overall effects of particular nutritional interventions on infection rate, NEC, and mortality were calculated by using the Mantel–Haenszel method for dichotomous outcomes, and were presented as risk ratios (RR) with 95% confidence intervals (CI), by using Epi Info, Stat Calc (Centers for Disease Control and Prevention, Atlanta, GA; https://www.cdc.gov/epiinfo/index.html). Registered trials were identified by the WHO International Clinical Trials Platform (World Health Organization, Geneva, Switzerland; http://apps.who.int/trialsearch/Default.aspx) and the trial registry of the National Library of Medicine (National Institutes of Health, Washington, DC; https://www.clinicaltrials.gov). Sample sizes were determined by using the ClinCalc online sample size calculator (Sean P. Kane, Rosalind Franklin University of Medicine and Science, North Chicago, IL; https://clincalc.com/stats/samplesize.aspx).
Milk and milk components
Colostrum
Colostrum contains a variety of glycoproteins that support the infant’s defense against microbes colonizing the mucous membranes after birth. Oropharyngeal administration of mother’s own fresh or frozen/thawed colostrum compared with water, saline, placebo, or no intervention has been investigated in eight trials. In six trials, colostrum was given within the first 48 h of life, in two trials up to 96 h of life. Two more trials investigated bovine colostrum administered enterally via gavage. Individually, the trials failed to demonstrate significantly reduced rates of infection, NEC, or mortality. The trials have been analyzed by three independently conducted meta-analyses4,5,6 that differed by inclusion of trials (by acceptance of unpublished data, time of administration, and source of colostrum). However, the meta-analyses agreed that there is no evidence from RCTs to suggest that colostrum reduced rates of NEC, infection, or mortality, as did calculations that combined all RCTs that had been included in at least one of the meta-analyses (Table 1). A subgroup analysis of the four trials included in all three meta-analyses likewise revealed similar rates of infection (9/80 [11.3%] vs 8/76 [10.5%], risk ratio (RR) [95% confidence interval (CI)] 1.07 [0.43–2.63]), NEC (7/80 [8.8%] vs 4/76 [5.3%], RR [95% CI] 1.66 [0.51–5.45]), and mortality (3/80 [3.8%] vs 1/76 [1.3%], RR [95% CI] 2.85 [0.30–26.81]).
Donor milk
In the absence of mother’s own milk, human donor milk is the most closely related source of nutrition and recommended by the World Health Organization, the European Society of Pediatric Gastroenterology, Hepatology, and Nutrition, and the American Academy of Pediatrics.7,8,9 The most recent Cochrane meta-analysis10 reviewing data from a total of 1879 preterm infants enrolled in 12 trials, found evidence that donor milk, as opposed to formula, significantly reduced rates of NEC but had no impact on invasive infections or mortality (Table 1). The overall methodological quality of the trials included was judged to be moderate. Protection against NEC was reported by the four trials published before 2000 that reported to use unfortified donor milk (RR [95% CI] 0.30 [0.10–0.90]) and the four trials published after 2000 that reported to use fortified donor milk (RR [95% CI] 0.61 [0.38–0.97]). All but one trial (published in 1983) used pasteurized donor milk. The results were not changed substantially by exclusion of this single trial that used unpasteurized donor milk.11 In addition to these 12 trials, there are several investigator-initiated RCTs randomizing preterm infants to donor milk or formula, which have already completed recruitment (Canada: ISRCTN3531714, target sample size n = 352; Argentina: NCT01390753, n = 300; England: NCT016868477, n = 66; United States: NCT01534481, n = 670, and NCT01232725, n = 121), are currently recruiting (Lithuania: ISRCTN64647571, n = 120; England: ISRCTN16799022, n = 100), or have been registered but are not recruiting yet (India: CTRI/2016/04/006855, n = 230; CTRI/2018/11/016480, n = 428). The results of these trials are expected to further refine our view on the merits of donor milk to reduce rates of infection, NEC, and mortality.
Human milk-based fortifier
As preterm infants growing along fetal trajectories gain weight at a much faster rate than term infants, human milk provides insufficient quantities of protein, calcium, and phosphate to allow for adequate growth of very preterm infants. Therefore, human milk—either own mother’s milk or donor milk—requires fortification to ensure that the enteral supply matches the demand of the growing infant. Fortifiers added are usually based on bovine milk but may be derived from human milk as well. A study that randomized preterm infants fed their own mother’s milk to fortification with a human milk-based fortifier and pasteurized donor milk if mother’s milk ceased to be available (n = 138), or bovine milk-based fortifier and preterm formula if no mother’s milk was available (n = 69), found significantly lower rates of NEC associated with human fortifier/donor milk versus bovine fortifier/formula,12 while there was no difference in rates of infection of mortality. A second study of the same group randomized 53 preterm infants with birth weights between 500 and 1250 g to donor milk fortified with a human milk-based fortifier or preterm formula.13 They found a trend toward reduced rates of NEC associated with exclusively human milk-based nutrition, as opposed to feeding preterm formula (thereby supporting the superiority of human milk, as opposed to formula). However, there was no effect in a head-to-head comparison between fortifiers based on human or bovine milk added to mother’s own milk or donor milk.14 A company-funded open-label RCT comparing a human milk-based and a bovine milk fortifier in preterm infants with a gestational age ≤28 weeks is set to recruit patients in northern Sweden (NCT03797157, target sample size n = 222).
Lactoferrin
Human and bovine milk, as well as tears, bile, and saliva, contain the glycoprotein lactoferrin that exhibits an array of antimicrobial activities in vitro. After acidic proteolysis in the stomach, lactoferrin yields a group of peptides called lactoferricins that also have antimicrobial properties. While lactoferrin is already present in milk, adding further lactoferrin has been hypothesized to be beneficial in preterm infants who are exceptionally prone to invasive infections originating in the gut. This hypothesis has been addressed by six trials involving a total of 886 preterm infants that were summarized in the last update of the Cochrane review published in 2017.15 Lactoferrin supplementation to enteral feeds was associated with a significant reduction of infections (36/432 [8.3%] vs 64/454 [14.1%], RR [95% CI] 0.59 [0.40–0.87]), but did not reduce mortality (19/527 [3.6%] vs 31/544 [5.7%], RR [95% CI] 0.65 [0.37–1.11]). Joint analysis of the four trials (750 participants) that also reported rates of NEC (≥stage 2) yielded evidence of reduced rates of NEC associated with lactoferrin (8/368 [2.2%] vs 22/382 [5.8%], RR [95% CI] 0.40 [0.18–0.86]). Quality of the trials was judged to be low because of risk of bias.15 All but one trial had used bovine lactoferrin. The results were not changed after exclusion of the single trial that employed human recombinant lactoferrin16 involving a total of 120 infants. A further meta-analysis published in 201817 included three additional trials that had been published in Chinese journals but were not listed by PubMed. This meta-analysis, however, yielded similar results (infection (9 trials): 41/629 [6.5%] vs 96/659 [14.6%], RR [95% CI] 0.47 [0.33–0.67], NEC (5 trials): 9/448 [2.0%] vs 26/462 [5.6%], RR [95% CI] 0.40 [0.18–0.86], and mortality (7 trials): 22/625 [3.5%] vs 35/647 [5.4%], RR [95% CI] 0.70 [0.38–1.30]).
This favorable view on lactoferrin changed after publication of the results of the ELFIN trial, the largest trial so far investigating the use of enteral lactoferrin to prevent infection for very preterm infants.18,19 Recruiting a total of 2203 preterm infants (2182 with primary outcome data available), the ELFIN trial enrolled more infants than all previous trials taken together. This trial found no difference for invasive infection (316/1093 [28.9%] vs 334/1089 [30.7%], RR [95% CI] 0.94 [0.83–1.07]), NEC (63/1085 [5.8%] vs 56/1084 [5.2%], RR [95% CI] 1.12 [0.71–1.77]), or mortality (71/1076 [6.6%] vs 68/1076 [6.3%], RR [95% CI] 1.04 [0.69–1.59]).
When combining the data from the ELFIN trial with those of the Cochrane analysis from 2017, there was no effect of lactoferrin on NEC or mortality (Table 1) while a trend remained for infections. A subgroup analysis revealed an effect of lactoferrin on rates of infection in infants not exclusively fed their own mother’s milk (222/990 [22.4%] vs 262/961 [27.3%], RR [95% CI] 0.82 [0.71–0.96]).20 Analyzed by pathogen, lactoferrin appeared to have no effect on Gram-positive (RR [95% CI] 0.87 [0.71–1.06]) or Gram-negative bacterial infections (RR [95% CI] 0.88 [0.63–1.21]), while the impact on fungal sepsis was statistically significant (RR [95% CI] 0.21 [0.07–0.63]). However, the overall rate of fungal infection was 15 times lower in the recent ELFIN trial (5/2182 [0.23%]) compared with the previous trials summarized in the Cochrane meta-analysis from 2017 (17/498 [3.4%]), and the ELFIN trial contributes only five cases to this sensitivity analysis. An array of interventions shown to decrease intestinal fungal colonization and rates of invasive fungal infections, such as probiotics,21 dietary medium-chain triglycerides,22 systemic (e.g., fluconazole), and topical chemoprophylaxis (such as nystatin)23,24 apparently act in concert to substantially decrease rates of fungal infection. The rates of fungal infections reported by the ELFIN investigators in the United Kingdom are similar to those of nosocomial infection surveillance data for preterm infants elsewhere.25 Two large randomized “Lactoferrin Infant Feeding Trials” (LIFT) currently recruit preterm infants in Australia (ISRCTN66482337, target sample size n = 1500) and Canada (NCT03367013, n = 500).
Amino acids
L-Arginine
Tissue hypoxia and ischemia may precipitate a cascade of events that ultimately result in NEC. Vasoconstrictive stimuli may be antagonized by nitric oxide produced by nitric oxide synthase from L-arginine and O2. Increasing the amount of substrate available to these enzymes may therefore enhance local perfusion by dilating constricted vessels. Three randomized controlled trials (from Canada, Greece, and Egypt) investigated the prophylactic use of oral L-arginine (1.5 mmol/kg/d) to prevent NEC in a total of 285 preterm infants.26 In one of the three trials, infants were first started on parenteral L-arginine and then switched to oral L-arginine once tolerating 40% enteral food.27 The trials were small but judged to be of good methodological quality. L-Arginine supplementation was associated with a significant reduction of NEC (stage 2 or more) without impacting on mortality (Table 1). No data were provided to allow for a meta-analysis of invasive infection rates. Despite the encouraging results, there are no new ongoing registered RCTs investigating the use of L-arginine in very preterm infants.
L-Glutamine
L-Glutamine is a conditionally essential amino acid that serves as a source of energy and to build nicotinamide adenine dinucleotide that is required to counteract oxidative stress. Combined results of six RCTs totaling 1095 infants28 suggest that enteral supplementation of L-glutamine reduced rates of invasive infection without impacting on rates of NEC and mortality (Table 1). The trials were judged to be of good methodological quality. In contrast, RCTs that investigated parenteral administration of L-glutamine (n = 5) failed to reveal any reduction in the rate of invasive bacterial infection. There are currently no newly registered RCTs investigating the use of enteral L-glutamine supplementation for preterm infants.
Trace elements
Selenium
Selenium is incorporated into selenoproteins that are important for an effective immune response, and inadequate selenium intake may thus impair the ability of a preterm infant to fend off pathogens.29 In geographically defined areas with low selenium concentrations, parenteral selenium supplementation has been reported to be associated with a lower proportion of infants having one or more episodes of infections,30 without impact on mortality. A single double-blind RCT conducted in India31 that randomized 90 preterm infants to oral selenium (10 µg/d) or placebo for 28 days also found lower rates of infections without impact on mortality (Table 1). No new trials have been registered addressing the effect of oral selenium supplementation in preterm infants.
Zinc
Zinc is a trace element with a multitude of functions in mammalian biology, and low zinc stores have been hypothesized to predispose preterm infants to NEC.32 Oral zinc supplementation has been investigated in a single RCT that increased the total zinc intake from 1.3 to 1.4 mg/d in placebo control infants to 9.7–10.7 mg/d in infants assigned to the experimental group.33 Additional zinc supplementation had no impact on the rate of infection but significantly reduced rates of NEC and mortality (Table 1). An open-label RCT is currently recruiting preterm infants <30 weeks of gestational age (target sample size, n = 126) to determine whether enteral zinc supplementation leads to improved growth in infants at risk for bronchopulmonary dysplasia (NCT03532555). The investigators’ hypothesis is that oral zinc supplementation in these infants will significantly improve growth compared with standard of care. Neither infection nor NEC are listed as secondary endpoints.
Non-digestible carbohydrates
Manufactured oligosaccharides
Human milk contains a large variety of linear and branched oligosaccharides that are metabolized in the gut lumen only by certain microbes such as bifidobacteria. By virtue of their influence on the human gut microbiome, such oligosaccharides are referred to as prebiotics. Composition and quantity of these human milk oligosaccharides (HMO) vary over time and from mother to mother, depending on the mother’s secretory status. Synthetic galacto-oligosaccharides (GOS) and fructo-oligosaccharides (FOS) from pharmaceutical sources supposed to mimic HMO have been tested in a series of RCTs.34 The results suggest that food supplementation with these oligosaccharides is associated with reduced rates of invasive infection but not NEC or mortality (Table 1). A company-sponsored double-blind RCT investigating the more typical human HMOs, 2′fucosyl-lactose and lacto-N-neotetraose, is currently recruiting patients (gestational age 27–31 weeks, birth weight ≤1500 g) in French hospitals (NCT03607942, target sample size n = 160).
Inulin
A single RCT from Turkey that randomized preterm infants to receive inulin, a dietary fiber consisting of β(2 → 1)-linked fructose moieties, reported significantly lower rates of invasive infection and mortality but no effect on NEC in infants receiving inulin, as compared with placebo (Table 1). The trial, employing a 2 × 2 factorial design, also assessed the effect of live Bifidobacterium lactis given as a single-strain bacterial probiotic.35 Protection afforded by inulin (900 mg/d) against invasive infection and death was not augmented further by Bifidobacterium lactis, while Bifidobacterium lactis itself reduced rates of NEC (6/200 [3%] vs 30/200 [15%], RR [95% CI] 0.02 [0.09–0.47]).
Lactulose
Lactulose is a disaccharide made of galactose and fructose with a β(1 → 4) link that cannot be metabolized by human digestive enzymes. A RCT from Israel investigated the use of lactulose in 28 preterm infants.36 Rates of invasive infections (2/15 [13%] vs 4/13 [31%]), NEC (1/15 [7%] vs 2/13 [15%]), and mortality (0/15 [0%] vs 1/13 [8%]) tended to be lower in lactulose-fed infants, as compared with controls, without reaching the level of statistical significance.
Probiotics
The intestinal microbiome of healthy breastfed infants displays an abundance of bifidobacteria and lactobacilli. They are thought to keep Gram-negative enterobacteriaceae at bay that have been identified as the responsible pathogen of most fatal invasive infections in preterm infants.25 Disturbing the balance of the preterm infant’s intestinal microbiome by systemic antibiotics is associated with increased rates of invasive infections, NEC, and mortality.37,38,39,40 A large number of RCTs have investigated the administration of live bacteria (probiotics) as a means to establish a presumably healthier gut microbiome, and several meta-analyses have confirmed that probiotics reduce rates of NEC and mortality.41,42,43,44,45,46 The effect on invasive infections appears to be limited to infants fed human milk.47,48,49 Protective effects observed in RCTs are widely mirrored in results of observational studies.50,51 There is wide variability in the type of probiotic bacteria studied, but bifidobacteria and lactobacilli appear to be most efficacious.52,53 The efficacy of single-strain probiotics, however, in reducing NEC is limited (Table 1), while probiotics composed of two or more different strains (such as a combination of lactobacilli plus bifidobacteria) are highly effective in reducing NEC and mortality45,54 and may furthermore reduce infections in human milk-fed infants.49 There is no effect of nonbacterial (yeast) probiotics.45,52
Other interventions
Oral immunoglobulin has been investigated in five trials, three of which were found to be eligible for a Cochrane meta-analysis.55 The oral administration of IgG or an IgG/IgA combination did not result in a significant reduction in the incidence of definite NEC (43/921 [4.7%] vs 51/191 [5.5%], RR (95% CI) 0.84 (0.57–1.25)), while data on infection and mortality were not reported.
Oral erythropoietin has been investigated in two trials recruiting a total of 110 infants. There was no effect on NEC rates (2/61 [3.3%] vs 3/49 [9.4%], RR (95% CI) 0.62 (0.15–2.69)) or any other outcome.56
Implementation and future research
The present evidence from RCTs suggests that rates of invasive infections, NEC, and mortality in preterm infants can be influenced by the choice of food, food components, and food additives. Selenium, inulin, GOS/FOS prebiotics, and enteral L-glutamine apparently are associated with diminished rates of invasive infections. Zinc, L-arginine, donor milk, and multiple-strain probiotics are associated with lower rates of NEC. Inulin, zinc, and multiple-strain probiotics are associated with reduced all-cause mortality (Fig. 1).
Presently, only donor milk7,8,9,57,58 and multiple-strain probiotics57,59 have been introduced into clinical routine in some countries. However, probiotic products for medical use with a robust quality control pertaining to manufacturing and transport are not available in many places. Preterm formula and breast milk fortifier contain zinc, albeit at low quantities. In contrast, promising low-cost interventions such as inulin, L-arginine, or L-glutamine are currently neither widely employed nor being pursued in further trials.
There are several potential reasons for the reluctance of the neonatological scientific community to change clinical practice. Application of evidence from RCTs and meta-analyses to local practice requires results not only to be robust but also based on background data that resemble those encountered by the physicians in charge. Some rather small trials with positive results feature high event rates in the placebo arm. The incidence of NEC has fallen substantially with increased use of mother’s milk, donor milk, and multiple-strain probiotics, and the current numbers may be quite different to those in RCTs that were conducted many years ago.
In the most recent RCT in very preterm infants born before 32 weeks’ gestation, the ELFIN trial, overall rates of NEC, and mortality were 5.5% and 6.5%, respectively.18,19 More than 3300 infants would need to be recruited to demonstrate a one-third reduction by an intervention in a RCT. Such a trial would necessitate huge collaborative efforts and pose considerable obstacles for logistics and funding, possibly involving public–private partnerships. Moreover, it would compete with other trials for patients. Interestingly, the large ELFIN trial allowed study participants to be enrolled in other RCTs simultaneously. Simultaneous enrolment of preterm infants is a contentious issue60 but might be a pivotal option to pave the avenue for further research into the health of limited-number patient groups.
The food additives found to reduce rates of infection, NEC, and mortality work by distinct but potentially synergistic modes of action. Simultaneous administration of prebiotics and probiotics has so far met with limited success.35 In the near future, it may be feasible to produce a combined formulation of L-arginine, L-glutamine, inulin, zinc, Bifidobacterium infantis, and Lactobacillus acidophilus as a single nutritional intervention for preterm infants, akin to the polypill approach employed as a prophylaxis for cardiovascular morbidity and mortality in the elderly.61,62 This option, however, is still awaiting to stand the test of large, well-conducted trials.
References
Miller, J. et al. A systematic review and meta-analysis of human milk feeding and morbidity in very low birth weight infants. Nutrients 10, 707 (2018).
Cossey, V. et al. Pasteurization of mother’s own milk for preterm infants does not reduce the incidence of late-onset sepsis. Neonatology 103, 170–6 (2013).
Dicky, O. et al. Policy of feeding very preterm infants with their mother’s own fresh expressed milk was associated with a reduced risk of bronchopulmonary dysplasia. Acta Pædiatr. 106, 755–762 (2017).
Nasuf, A. W. A., Ojha, S. & Dorling, J. Oropharyngeal colostrum in preventing mortality and morbidity in preterm infants. Cochrane Database Syst. Rev. 9, CD011921 (2018).
Sadeghirad, B. et al. Human and bovine colostrum for prevention of necrotizing enterocolitis: a meta-analysis. Pediatrics 142, e20180767 (2018).
Panchal, H., Athalye-Jape, G. & Patole, S. Oropharyngeal colostrum for preterm infants: a systematic review and meta-analysis. Adv. Nutr. (2019).
WHO. Guidelines on Optimal Feeding of Low Birth-weight Infants in Low- and Middle-income Countries. (World Health Organization, Geneva, 2011).
ESPGHAN Committee on Nutrition, Arslanoglu, S. et al. Donor human milk for preterm infants: current evidence and research directions. J. Pediatr. Gastroenterol. Nutr. 57, 535–542 (2013).
American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics 129, e827 (2012).
Quigley, M., Embleton, N. D. & McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 7, CD002971 (2019).
Tyson, J. E. et al. Growth, metabolic response, and development in very-low-birth-weight infants fed banked human milk or enriched formula. I. Neonatal findings. J. Pediatr. 103, 95–104 (1983).
Sullivan, S. et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J. Pediatr. 156, 562–567 (2010). e1.
Cristofalo, E. A. et al. Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants. J. Pediatr. 163, 1592–1595 (2013).
O’Connor, D. L. et al. Nutrient enrichment of human milk with human and bovine milk-based fortifiers for infants born weighing <1250 g: a randomized clinical trial. Am. J. Clin. Nutr. 108, 108–116 (2018).
Pammi, M. & Suresh, G. Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst. Rev. 6, CD007137 (2017).
Sherman, M. P. et al. Randomized controlled trial of talactoferrin oral solution in preterm infants. J. Pediatr. 175, 68–73 (2016).
He, Y., Cao, L. & Yu, J. Prophylactic lactoferrin for preventing late-onset sepsis and necrotizing enterocolitis in preterm infants: a PRISMA-compliant systematic review and meta-analysis. Med. (Baltim.) 97, e11976 (2018).
Griffiths, J. et al. Enteral lactoferrin to prevent infection for very preterm infants: the ELFIN RCT. Health Technol. Assess. 22, 1–60 (2018).
ELFIN trial investigators group. Enteral lactoferrin supplementation for very preterm infants: a randomised placebo-controlled trial. Lancet 393, 423–433 (2019).
Manzoni, P. et al. Is lactoferrin more effective in reducing late-onset sepsis in preterm neonates fed formula than in those receiving mother’s own milk? Secondary analyses of two multicenter randomized controlled trials. Am. J. Perinatol. 36, S120–S125 (2019).
Manzoni, P. et al. Oral supplementation with Lactobacillus casei subspecies rhamnosus prevents enteric colonization by Candida species in preterm neonates: a randomized study. Clin. Infect. Dis. 42, 1735–1742 (2006).
Arsenault, A. B. et al. Dietary supplementation with medium-chain triglycerides reduces candida gastrointestinal colonization in preterm infants. Pediatr. Infect. Dis. J. 38, 164–168 (2019).
Cleminson, J., Austin, N. & McGuire, W. Prophylactic systemic antifungal agents to prevent mortality and morbidity in very low birth weight infants. Cochrane Database Syst. Rev. CD003850 (2015).
Austin, N., Cleminson, J., Darlow, B. A. & McGuire, W. Prophylactic oral/topical non-absorbed antifungal agents to prevent invasive fungal infection in very low birth weight infants. Cochrane Database Syst. Rev. CD003478 (2015).
Piening, B. C., Geffers, C., Gastmeier, P. & Schwab, F. Pathogen-specific mortality in very low birth weight infants with primary bloodstream infection. PLoS One 12, e0180134 (2017).
Shah, P. S., Shah, V. S. & Kelly, L. E. Arginine supplementation for prevention of necrotising enterocolitis in preterm infants. Cochrane Database Syst. Rev. 4, CD004339 (2017).
Amin, H. J. et al. Arginine supplementation prevents necrotizing enterocolitis in the premature infant. J. Pediatr. 140, 425–431 (2002).
Moe-Byrne, T., Brown, J. V. & McGuire, W. Glutamine supplementation to prevent morbidity and mortality in preterm infants. Cochrane Database Syst. Rev. 4, CD001457 (2016).
Avery, J. C. & Hoffmann, P. R. Selenium, selenoproteins, and immunity. Nutrients 10, 1203 (2018).
Darlow, B. A. & Austin, N. C. Selenium supplementation to prevent short-term morbidity in preterm neonates. Cochrane Database Syst. Rev. CD003312 (2003).
Aggarwal, R., Gathwala, G., Yadav, S. & Kumar, P. Selenium supplementation for prevention of late-onset sepsis in very low birth weight preterm neonates. J. Trop. Pediatr. 62, 185–193 (2016).
Terrin, G. et al. Zinc in early life: a key element in the fetus and preterm neonate. Nutrients 7, 10427–10446 (2015).
Terrin, G. et al. Zinc supplementation reduces morbidity and mortality in very-low-birth-weight preterm neonates: a hospital-based randomized, placebo-controlled trial in an industrialized country. Am. J. Clin. Nutr. 98, 1468–1474 (2013).
Chi, C., Buys, N., Li, C., Sun, J. & Yin, C. Effects of prebiotics on sepsis, necrotizing enterocolitis, mortality, feeding intolerance, time to full enteral feeding, length of hospital stay, and stool frequency in preterm infants: a meta-analysis. Eur. J. Clin. Nutr. 73, 657–670 (2019).
Dilli, D. et al. The propre-save study: effects of probiotics and prebiotics alone or combined on necrotizing enterocolitis in very low birth weight infants. J. Pediatr. 166, 545–551 (2015). e1.
Riskin, A. et al. The effects of lactulose supplementation to enteral feedings in premature infants: a pilot study. J. Pediatr. 156, 209–214 (2010).
Cotton, C. M. Early, prolonged use of postnatal antibiotics increased the risk of necrotising enterocolitis. Arch. Dis. Child Educ. Pr. Ed. 95, 94 (2010).
Alexander, V. N., Northrup, V. & Bizzarro, M. J. Antibiotic exposure in the newborn intensive care unit and the risk of necrotizing enterocolitis. J. Pediatr. 159, 392–397 (2011).
Kuppala, V. S., Meinzen-Derr, J., Morrow, A. L. & Schibler, K. R. Prolonged initial empirical antibiotic treatment is associated with adverse outcomes in premature infants. J. Pediatr. 159, 720–725 (2011).
Ting, J. Y. et al. Association between antibiotic use and neonatal mortality and morbidities in very low-birth-weight infants without culture-proven sepsis or necrotizing enterocolitis. JAMA Pediatr. 170, 1181–1187 (2016).
AlFaleh, K. & Anabrees, J. Probiotics for prevention of necrotizing enterocolitis in preterm infants. Cochrane Database Syst. Rev. CD005496 (2014).
Lau, C. S. & Chamberlain, R. S. Probiotic administration can prevent necrotizing enterocolitis in preterm infants: A meta-analysis. J. Pediatr. Surg. 50, 1405–1412 (2015).
Sawh, S. C., Deshpande, S., Jansen, S., Reynaert, C. J. & Jones, P. M. Prevention of necrotizing enterocolitis with probiotics: a systematic review and meta-analysis. PeerJ 4, e2429 (2016).
Thomas, J. P., Raine, T., Reddy, S. & Belteki, G. Probiotics for the prevention of necrotising enterocolitis in very low-birth-weight infants: a meta-analysis and systematic review. Acta Pædiatr. 106, 1729–1741 (2017).
Chang, H. Y. et al. Multiple strains probiotics appear to be the most effective probiotics in the prevention of necrotizing enterocolitis and mortality: an updated meta-analysis. PLoS One 12, e0171579 (2017).
Sun, J. et al. Effects of probiotics on necrotizing enterocolitis, sepsis, intraventricular hemorrhage, mortality, length of hospital stay, and weight gain in very preterm infants: a meta-analysis. Adv. Nutr. 8, 749–763 (2017).
Zhang, G. Q., Hu, H. J., Liu, C. Y., Shakya, S. & Li, Z. Y. Probiotics for preventing late-onset sepsis in preterm neonates: a PRISMA-compliant systematic review and meta-analysis of randomized controlled trials. Med. (Baltim.) 95, e2581 (2016).
Rao, S. C., Athalye-Jape, G. K., Deshpande, G. C., Simmer, K. N. & Patole, S. K. Probiotic supplementation and late-onset sepsis in preterm infants: a meta-analysis. Pediatrics 137, e20153684 (2016).
Aceti, A. et al. Probiotics prevent late-onset sepsis in human milk-fed, very low birth weight preterm infants: systematic review and meta-analysis. Nutrients 9, 904 (2017).
Olsen, R., Greisen, G., Schrøder, M. & Brok, J. Prophylactic probiotics for preterm infants: a systematic review and meta-analysis of observational studies. Neonatology 109, 105–112 (2016).
Dermyshi, E. et al. The “golden age” of probiotics: a systematic review and meta-analysis of randomized and observational studies in preterm infants. Neonatology 112, 9–23 (2017).
van den Akker, C. H. P. et al. Probiotics for preterm infants: a strain-specific systematic review and network meta-analysis. J. Pediatr. Gastroenterol. Nutr. 67, 103–122 (2018).
Hagen, P. C. & Skelley, J. W. Efficacy of bifidobacterium species in prevention of necrotizing enterocolitis in very-low birth weight infants. A systematic review. J. Pediatr. Pharm. Ther. 24, 10–15 (2019).
Guthmann, F. & Bührer, C. Routine probiotics in preterm infants? Arch. Dis. Child Fetal Neonatal Ed. 96, F311–F312 (2011).
Foster, J. P., Seth, R. & Cole, M. J. Oral immunoglobulin for preventing necrotizing enterocolitis in preterm and low birth weight neonates. Cochrane Database Syst. Rev. 4, CD001816 (2016).
Ananthan, A., Balasubramanian, H., Rao, S. & Patole, S. Clinical outcomes related to the gastrointestinal trophic effects of erythropoietin in preterm neonates: a systematic review and meta-analysis. Adv. Nutr. 9, 238–246 (2018).
Sharpe, J., Way, M., Koorts, P. J. & Davies, M. W. The availability of probiotics and donor human milk is associated with improved survival in very preterm infants. World J. Pediatr. 14, 492–497 (2018).
Weaver, G. et al. Recommendations for the establishment and operation of human milk banks in Europe: a consensus statement from the European Milk Bank Association (EMBA). Front Pediatr. 7, 53 (2019).
Denkel, L. A. et al. Protective effect of dual-strain probiotics in preterm infants: a multi-center time series analysis. PLoS One 11, e0158136 (2016).
Davis, J. M. et al. Enrollment of neonates in more than one clinical trial. Clin. Ther. 39, 1959–1969 (2017).
Huffman, M. D., Xavier, D. & Perel, P. Uses of polypills for cardiovascular disease and evidence to date. Lancet 389, 1055–1065 (2017).
Selak, V. et al. Reaching cardiovascular prevention guideline targets with a polypill-based approach: a meta-analysis of randomised clinical trials. Heart 105, 42–48 (2019).
Acknowledgements
Preparation of the paper was supported in part by a grant from German Federal Department of Education and Research (FKZ 03ZZ0829B) within the framework of the NeoBiom project.
Author contributions
C.B., H.F. and S.W. formulated the questions to be addressed, designed the search strategy, and assessed the hits. Quantitative data were compiled by C.B. who prepared the first version of the paper. The paper was subsequently critically reviewed by H.F. and S.W. All three authors approved the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bührer, C., Fischer, H.S. & Wellmann, S. Nutritional interventions to reduce rates of infection, necrotizing enterocolitis and mortality in very preterm infants. Pediatr Res 87, 371–377 (2020). https://doi.org/10.1038/s41390-019-0630-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0630-2
This article is cited by
-
Glutamine inhibits inflammation, oxidative stress, and apoptosis and ameliorates hyperoxic lung injury
Journal of Physiology and Biochemistry (2023)
-
Per- und polyfluorierte Alkylsubstanzen (PFAS) und Stillen: Nutzen-Risiken-Abwägungen
Monatsschrift Kinderheilkunde (2022)
-
Evidence-Based Approaches to Minimize the Risk of Developing Necrotizing Enterocolitis in Premature Infants
Current Treatment Options in Pediatrics (2022)
-
Sachgerechte Reinigung von Milchpumpen
Monatsschrift Kinderheilkunde (2021)