Abstract
Background
Administration of caffeine citrate can facilitate extubation. Our aim was to determine whether a loading dose of caffeine citrate given to ventilated, preterm infants affected the diaphragm electrical activity.
Methods
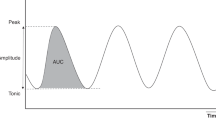
Infants <34 weeks of gestational age were recruited if requiring mechanical ventilation and prescribed a loading dose of caffeine citrate. Surface electrodes recorded the electrical activity of the diaphragm (dEMG) before and after administration of intravenous caffeine citrate. The mean amplitude of the EMG (dEMG) trace and the mean area under the EMG curve (aEMGc) were calculated.
Results
Thirty-two infants were assessed with a median gestational age of 29 (27–31) weeks. The dEMG amplitude increased, peaking at 25 min post administration (p = 0.006), and the increase in aEMGc (p = 0.004) peaked at 30 min; the differences were not significant after 60 min. At 20 min, there was an increase in minute volume (p = 0.034) and a reduction in the peak inspiratory pressure (p = 0.049).
Conclusions
We have demonstrated a transient increase in both electrical activity of the diaphragm and respiratory function following an intravenous loading dose of caffeine citrate.
Similar content being viewed by others
Introduction
Mechanical ventilation is frequently used to support very prematurely born infants who have immature, underdeveloped lungs and inadequate respiratory drive. Yet, prolonged ventilation is associated with complications, such as bronchopulmonary dysplasia and pulmonary interstitial emphysema,1,2 and hence, it is important to successfully extubate infants as soon as possible. Caffeine citrate is a methylxanthine and administration can facilitate successful extubation through a number of mechanisms.3 Caffeine citrate is a respiratory stimulant that acts centrally and antagonises inhibitory adenosine A1 receptors.4 It increases the ventilatory response to hypercapnia in preterm infants.5 Furthermore, administration of caffeine citrate can increase respiratory muscle strength and improve lung compliance.6 Intravenous caffeine citrate has also been shown to increase the diaphragmatic activity of spontaneously breathing preterm infants with a corresponding increase in tidal volume.7 Whether, however, the effects of caffeine citrate administration on diaphragm electrical activity are similar in ventilated, preterm infants is currently unknown.
Electromyography (EMG) is a global measure of the neural impulses that are translated into muscle fibre action potentials, with the processed signal giving the amplitude of electrical activity of a muscle.8 The amplitude of the electrical activity of the diaphragm (EAdi) is helpful in monitoring asynchrony and respiratory muscle loading of ventilated patients.8 The EAdi can also be used to assess neural respiratory drive;9,10 inspiratory drive has been shown to increase in response to an increased work of breathing.11 We hypothesised that administration of a loading dose of caffeine citrate to ventilated, prematurely born infants would result in an increase in the amplitude of the diaphragm electromyogram and improved respiratory function. Our aim was to test those hypotheses.
Methods
Study design and subjects
A prospective, observational cohort study took place between 01/09/2018 and 30/06/2019 at the two neonatal units within King’s College Hospital NHS Foundation Trust (KCH), London UK. This NHS Foundation Trust comprises of King’s College Hospital, London and the Princess Royal University Hospital, Orpington. The London Brent Research Ethics Committee approved the study and the parents gave written, informed consent for their infant to take part.
Infants born <34 weeks of completed gestational age (GA) who were prescribed a loading dose of caffeine citrate by the clinical team were eligible for recruitment into the study if they were receiving invasive mechanical ventilation. Infants with chromosomal or major congenital anomalies were excluded. Baseline demographic data were collected including gender, ethnicity, antenatal exposure to corticosteroids and magnesium sulphate, GA and mode of delivery, mode of ventilation prior to caffeine administration and use of postnatal surfactant.
At KCH, ventilatory support was delivered by an SLE 6000 ventilator (SLE limited, Croydon UK). Preterm infants were usually supported by patient-triggered ventilation with a targeted tidal volume. Targeted tidal volumes were set between 5 and 6 mL/kg. The clinical team routinely prescribed a 20-min loading dose caffeine citrate (20 mg/kg) to ventilated infants <34 weeks of GA as per Trust guidelines and in agreement with recent evidence showing the benefit of early therapy (before day 3 of postnatal life) in decreasing the composite outcome of bronchopulmonary dysplasia or all-cause mortality.12
Diaphragmatic electrical activity was measured continuously 15 min prior to the administration of a loading dose of caffeine citrate and until 180 min after the loading dose. The peak inspiratory pressure (PIP), positive end expiratory pressure, expired tidal volume, fraction of inspired oxygen, inspiratory time and mean airway pressure were recorded during the same time periods as the EMG analysis.
The activity of the diaphragm was measured via transcutaneous EMG of the diaphragm using surface electrodes. All infants were assessed in the supine position. The transcutaneous diaphragm EMG was monitored using a portable 16-channel digital physiological amplifier (Dipha-16; Inbiolab, Groningen, the Netherlands) and three surface electrodes (Kendall H59P cloth electrodes; Covidien, MA). Two electrodes were placed vertically in line with the nipples on the right and left chest wall at the costo-abdominal margin and one electrode placed at the centre of the sternum. The electrodes were connected to a portable physiological amplifier (DEMCON; Macawi Medical Systems, the Netherlands) that generated raw signals correlating to the diaphragm EMG at a sampling rate of 500 Hz. The physiological amplifier wirelessly transmitted to a bedside computer running Polybench (Applied Biosignals, Weener, Germany). Raw signals were filtered and processed automatically within the Polybench software including the gating technique. The method used to filter the cardiac electrical activity was similar to the gating technique described by O’Brien.13 EMG data were imported into MATLAB from Poly5 format using the TMSi MATLAB Interface (Twente Medical Systems International, Oldenzaal, the Netherlands). The complete recording of each infant was reviewed and points at which the infants was moving or being handled were identified by the presence of interference to the signal, these were excluded from analysis. EMG analyses of periods of 30-s artefact-free recordings were performed at set time intervals. Three sets of stable 30-s recordings in a time period beginning 5 min prior to administration of the loading dose of caffeine citrate and at 5-, 20-, 25-, 30-, 60-, 120- and 180-min time intervals after the start of the 20-min caffeine citrate loading dose infusion were analysed. For each artefact-free 30-s recording, the mean amplitude of the EMG (dEMG) trace and the mean area under the EMG curve (aEMGc)14,15 were calculated using MATLAB Statistics Toolbox Release 2015b (The MathWorks, Inc., Natick, MA, USA). At each time interval, the change from the baseline for each measurement was calculated with each infant acting as their own control.
Analysis
The data were tested for normality using Shapiro–Wilk test and found to be non-normally distributed. Therefore, data are presented as median (interquartile range) and differences assessed for statistical significance using Wilcoxon rank-sum test for paired changes post caffeine administration. Statistical analyses were undertaken using the SPSS software Version 25 (SPSS Inc., Chicago IL).
Sample size
A previous study found an increase in median peak electrical activity from 1.42 to 2.16 μV in non-ventilated infants following caffeine administration,7 therefore, using an estimated sample mean of 1.4 ± 0.6 μV, to detect a 30% difference in peak diaphragm EMG with 80% power at the 5% significance level, a sample of 32 infants was recruited.
Results
During the study period, 110 infants born <34 weeks of completed GA were admitted to the neonatal unit, and 32 were recruited (Fig. 1; Table 1). There were no significant differences in GA and birth weight (BW) between the included infants and those 15 infants who were eligible but not included (GA: 31.14 (25.0–32.71) weeks, p = 0.817; BW: 1.15 (0.73–1.91) kg, p = 0.71). In the included infants, the median time after birth to caffeine citrate administration was 288 (133–745) min (Table 1).
There was a significant increase in dEMG amplitude from baseline following the loading dose of caffeine citrate that peaked at 25 min post administration (p = 0.006) and a significant increase in aEMGc from baseline peaking at 30 min post administration of caffeine citrate (p = 0.004). By 60 min, the loading dose of caffeine citrate had no significant effect on the EAdi (Figs. 2 and 3). At 20 min, there was a significant increase in minute volume (p = 0.034) from baseline and significant reduction from baseline in the PIP (p = 0.049), and at 30 min, a significant increase in the respiratory rate (p = 0.021) from baseline. There were no significant changes in tidal volume post caffeine administration (Table 2).
Discussion
We have demonstrated that in preterm, ventilated infants there was a significant increase in both the dEMG amplitude and aEMGc, which peaked within the first hour following a loading dose of caffeine citrate. This transient increase in diaphragmatic electrical activity post administration of intravenous caffeine citrate is in agreement with a recent study in non-ventilated newborns.7 It may be explained by the initial high peak serum levels seen shortly after administration of the loading dose of caffeine. The timing of the increase in diaphragmatic activity was associated with improvements in lung function as shown by the increase in minute volume and decrease in the PIP.
The current study measured electrical activity and not contractions of the diaphragm. One in vivo study found, however, that administration of theophylline resulted in an increase in minute ventilation, which correlated with an increase in diaphragmatic contractility as well as inspiratory diaphragmatic neuromuscular output.16 What is unknown, however, is the underlying mechanism by which caffeine acts to enhance this contractile nature. One adult study showed an increase in trans-diaphragmatic pressure post caffeine therapy implying that caffeine does indeed enhance muscle contractility of the diaphragm.17 It has been suggested that caffeine acts centrally by rapidly crossing the blood–brain barrier18 and, through transmission of neural impulses, has subsequent effects on respiratory function resulting in increased diaphragmatic muscle activity.19 A further possibility is that caffeine increases sarcoplasmic reticulum calcium concentrations17,20 and hence enhances the activation of contractile proteins by increasing the affinity of calcium activation sites for calcium ions.21
A previous study described a significant increase in tidal volume post caffeine citrate administration in non-invasively ventilated infants, which was shown to correlate with the increase in dEMG amplitude.7 The majority of infants in the present study were supported with a predetermined targeted tidal volume, hence we would not have expected to see a change in the expiratory tidal volume. As lung mechanics change over time, the PIP required to achieve a target tidal volume will change. In this study, we observed a statistically significant decrease in PIP post caffeine administration with a corresponding increase in minute volume with an increase in respiratory rate demonstrating that the increase in diaphragmatic electrical activity favourably influenced respiratory function.
The elimination half-life of caffeine citrate is 101 h in infants,22 compared to the 3–6 h half-life observed in adults.4 It has been shown, however, that there is a high variation in the elimination half-life between neonates of relatively similar conceptional ages.23 Moreover, one study showed that peak concentrations of both oral and intravenous caffeine citrate are observed between 30 min and 2 h following administration.24 We speculate that the physiological effects of caffeine citrate in our study peaking within the first 1 h post administration are related to the time to peak effect (Tmax) at the peak concentration (Cmax) and not related to the maximum possible effect of the drug (Emax).25
Our study has strengths and some limitations. This study used non-invasive techniques for monitoring, with the use of surface electrodes, which were generally acceptable to parents with only two parents declining participation. There is ease and simplicity in using surface electrodes and these can be used for infants of all GAs.26 Diaphragm electromyogram recording by surface electrodes could potentially be susceptible to interference from surrounding muscle groups, such as intercostal and abdominal. On analysis of the traces, however, little interference was seen. This is in agreement with one previous study of diaphragm electrical recordings that showed little crosstalk of intercostal and abdominal muscles with diaphragmatic activity.27 Interventions such as neonatal procedures, nursing cares or position changes were not controlled for due to the acute setting and timing of the study, and these may have had some interference on the dEMG signal as movement artefacts; however; this limitation was accounted for by selecting the closest 30-s artefact-free period at each time interval studied. Overall, we saw a positive response in electrical activity following caffeine administration, but the response was variable. Our sample size, unfortunately, precludes sub-group analysis. A further limitation of this study was the non-randomisation of infants, but as caffeine has been shown to be beneficial to all premature infants,28,29 it would be unethical to randomise infants.
In conclusion, we have demonstrated that a loading dose of caffeine citrate in ventilated preterm infants had a transient increase in the EAdi and improvement in respiratory function. The transient nature of the effects we describe have implications for neonatal clinicians, that is if extubation is not soon after the loading dose of caffeine citrate has been administered, it may be less effective in facilitating extubation, but there is no evidence that this would impinge on its proven effects on improving neurodevelopmental outcome.30
References
Jensen, E. A. et al. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 169, 1011–1017 (2015).
Miller, J. D. & Carlo, W. A. Pulmonary complications of mechanical ventilation in neonates. Clin. Perinatol. 35, 273–281 (2008).
Steer, P. et al. High dose caffeine citrate for extubation of preterm infants: a randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 89, F499–F503 (2004).
Abdel-Hady, H. et al. Caffeine therapy in preterm infants. World J. Clin. Pediatr. 4, 81–93 (2015).
Rossor, T. et al. The effect of caffeine on the ventilatory response to hypercarbia in preterm infants. Pediatr. Res. 83, 1152–1157 (2018).
Kassim, Z., Greenough, A. & Rafferty, G. F. Effect of caffeine on respiratory muscle strength and lung function in prematurely born, ventilated infants. Eur. J. Pediatr. 168, 1491–1495 (2009).
Kraaijenga, J. V. et al. The effect of caffeine on diaphragmatic activity and tidal volume in preterm infants. J. Pediatr. 167, 70–75 (2015).
Doorduin, J. et al. Monitoring of the respiratory muscles in the critically ill. Am. J. Respir. Crit. Care Med. 187, 20–27 (2013).
Jeffreys, E. et al. Diaphragm electromyography results at different high flow nasal cannula flow rates. Eur. J. Pediatr. 178, 1237–1242 (2019).
Reilly, C. C. et al. Neural respiratory drive, pulmonary mechanics and breathlessness in patients with cystic fibrosis. Thorax 66, 240–246 (2011).
Oda, A. et al. Nasal high-flow therapy decreased electrical activity of the diaphragm in preterm infants during the weaning phase. Acta Paediatr. 108, 253–257 (2019).
Shenk, E. E. et al. Evaluation of timing and dosing of caffeine citrate in preterm neonates for the prevention of bronchopulmonary dysplasia. J. Pediatr. Pharm. Ther. 23, 139–145 (2018).
O’Brien, M., Van Eykern, L. & Prechtl, H. in Non-Invasive Physiological Measurements (ed. Rolfe, P.) 131–177 (Academic Press Inc, London, 1983).
Kanwade, A. B. & Bairagi, V. K. Feature extraction of EMG signals in time and frequency domain for myopathy, neuropathy and healthy muscle. 3rd International Conference on Electrical, Electronics, Engineering Trends, Communication, Optimisation and Sciences (EEECOS) (2016).
de Waal, C. G. et al. Electrical activity of the diaphragm during nCPAP and high flow nasal cannula. Arch. Dis. Child. Fetal Neonatal Ed. 102, F434–F438 (2017).
Aubier, M. et al. Increased ventilation caused by improved diaphragmatic efficiency during aminophylline infusion. Am. Rev. Respir. Dis. 127, 148–154 (1983).
Supinski, G. S., Deal, E. C. Jr & Kelsen, S. G. The effects of caffeine and theophylline on diaphragm contractility. Am. Rev. Respir. Dis. 130, 429–433 (1984).
Philip, R. K. et al. Caffeine treatment for apnea of prematurity and the influence on dose-dependent postnatal weight gain observed over 15 years. J. Caffeine Adenosine Res. 8, 99–106 (2018).
Bhatia, J. Current options in the management of apnea of prematurity. Clin. Pediatr. (Phila.) 39, 327–336 (2000).
Aubier, M. Pharmacotherapy of respiratory muscles. Clin. Chest Med. 9, 311–324 (1988).
Lamb, G. D., Cellini, M. A. & Stephenson, D. G. Different Ca2+ releasing action of caffeine and depolarisation in skeletal muscle fibres of the rat. J. Physiol. 531, 715–728 (2001).
Charles, B. G. et al. Caffeine citrate treatment for extremely premature infants with apnea: population pharmacokinetics, absolute bioavailability, and implications for therapeutic drug monitoring. Ther. Drug Monit. 30, 709–716 (2008).
Le Guennec, J. C., Billon, B. & Pare, C. Maturational changes of caffeine concentrations and disposition in infancy during maintenance therapy for apnea of prematurity: influence of gestational age, hepatic disease and breast-feeding. Pediatrics 76, 834–840 (1985).
Shrestha, B. & Jawa, G. Caffeine citrate - is it a silver bullet in neonatology? Pediatr. Neonatol. 58, 391–397 (2017).
MHRA. UKPAR Caffeine 5 mg/mL Solution for Injection. PL 20346/0002 (Medicines and Healthcare products Regulatory Agency, 2008)
American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am. J. Respir. Crit. Care Med. 166, 518–624 (2002).
Hutten, J. et al. Cross talk of respiratory muscles: it is possible to distinguish different muscle activity? Respir. Physiol. Neurobiol. 158, 1–2 (2007).
Schmidt, B. et al. Caffeine therapy for apnea of prematurity. N. Engl. J. Med. 354, 2112–2121 (2006).
Schmidt, B. et al. Long-term effects of caffeine therapy for apnea of prematurity. N. Engl. J. Med. 357, 1893–1902 (2007).
Schmidt, B. et al. Academic performance, motor function and behaviour 11 years after neonatal caffeine citrate therapy for apnea of prematurity: an 11 year follow up of the CAP randomised clinical trial. JAMA Pediatr. 171, 564–572 (2017).
Acknowledgements
We thank Dr Ian Hunt who supported analysis of the data. The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The EMG equipment was provided by SLE.
Author information
Authors and Affiliations
Contributions
A.G. and K.A.H. designed the study; E.E.W., K.A.H., J.J. and R.S.-R. collected the data; E.E.W., T.D. and A.G. analysed the data and produced the first draft. All authors were involved in revising it critically for important intellectual content and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
A.G. has a non-conditional educational grant from SLE to support her research on optimising neonatal ventilation. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Williams, E.E., Hunt, K.A., Jeyakara, J. et al. Electrical activity of the diaphragm following a loading dose of caffeine citrate in ventilated preterm infants. Pediatr Res 87, 740–744 (2020). https://doi.org/10.1038/s41390-019-0619-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0619-x
This article is cited by
-
Diaphragmatic electromyography in infants: an overview of possible clinical applications
Pediatric Research (2024)
-
Respiratory muscle function in the newborn: a narrative review
Pediatric Research (2022)