Abstract
Background
Oxygenation instability is not quantified or documented despite being common and correlated with neonatal morbidities, retinopathy of prematurity, and adverse 18-month outcomes.
Methods
We developed a five-type SpO2 histogram classification system based on the SpO2 difference within the 10–90th cumulative time percentile (A) and the time percentage with SpO2 ≤80% (B). In type 1, A is <5% and in type 5, A and B are ≥10%. We then studied consecutive 12-h SpO2 frequency histograms in all infants ≤34 weeks gestation receiving respiratory support on day 1, over 6 months.
Results
Six thousand and sixteen histograms were obtained in 73 infants, 28.9 ± 3.0 weeks gestation, and birth weight (BW) 1318.5 ± 495 g. All types were common and did not overlap. Type 3–5 (“unstable”) histograms were more common in oxygen or any intubated support. Time in SpO2 <85% and <80% progressively increased in types 3–5. Among histograms in oxygen, the mean (±SD) of SpO2 medians was 92.8 ± 1.9. Infants ≤28 weeks exhibited three phases of SpO2 instability (stable–unstable–stable). Those developing unstable histograms during the first week received longer ventilatory support (median [IQR], 101 [66] vs. 62 [28] days) and supplemental oxygen (62.5 [72] vs. 40.5 [40] days), and more were on ventilatory support at 40 weeks (7/15 vs. 0/10).
Conclusions
Classified SpO2 histograms quantify and document SpO2 instability and identify early infants at risk of prolonged respiratory support, while median SpO2 does not.
Similar content being viewed by others
Introduction
Oxygen saturation (SpO2) instability is common among premature infants, with an average of over 100 hypoxemic events per day in the first 8 weeks of life.1 In a mouse model of bronchopulmonary dysplasia (BPD), intermittent hypoxic stress during induction of BPD potentiated oxidative stress in lung tissue, exacerbated alveolar developmental arrest2 and was associated with delay in cerebral growth and neurodegeneration.3 Furthermore, simulation of intermittent hypoxemia in neonatal mice resulted in permanent sensorimotor deficit and cerebral hypomyelination.4 In premature infants, the incidence of intermittent hypoxemia has been related to retinopathy of prematurity requiring laser therapy,1 BPD,5,6 and adverse 18-month outcomes.7 Various interventions such as change in ventilation mode,8 change in position,9 and RBC transfusion10 have decreased the incidence of hypoxemic events in premature infants; however, the day-to-day clinical evaluation, quantification, and documentation of SpO2 instability in the neonatal intensive care unit (NICU) is hampered by the lack of an objective tool and language.
SpO2 histograms reveal the median SpO2 and the presence and magnitude of SpO2 instability over chosen periods of time ranging from the previous 30 min to 24 h.
In this manuscript, we describe a new SpO2 histogram classification system and use it to describe the prevalence, magnitude, and natural history of SpO2 instability in a busy level III NICU in a cross-sectional observational study.
Materials and methods
Study design and patients
This was a two-phase observational study conducted in the 60-bed, level III NICU at BC Women’s Hospital (Vancouver, BC, Canada).
In phase 1, we developed and piloted an SpO2 histogram classification system in a convenience sample of 29 premature infants ≤34 weeks gestation receiving respiratory support, such as continuous positive airway pressure (CPAP), non-invasive ventilation, or intubated respiratory support, during a period of 8 consecutive days. This proof-of-concept pilot was conducted to verify that five distinct histogram types, pre-defined by the study team, covered the spectrum of histograms seen and did not overlap. By the end of this phase, we made adjustments to the piloted classification system in order to simplify how each histogram type was defined (Fig. 1).
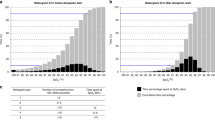
The histogram classification system. a A sample SpO2 histogram. SpO2 histograms are classified by counting the number of gray bars between the 10th and 90th percentage of time and the percentage of time with SpO2 ≤80%. The values obtained are entered into the classification table in b. c Examples of type 1–5 SpO2 histograms
During phase 2 we prospectively applied the updated classification system to a sample consisting of all premature infants admitted between June and November of 2015 at ≤34 weeks gestation with the need for invasive or non-invasive respiratory support on day 1. Infants with congenital diaphragmatic hernia, hypoxic ischemic encephalopathy, congenital heart defect, or major congenital anomalies incompatible with life were excluded. The observation period started on the day of admission and continued until the date of discharge with participants receiving continuous pulse oximetry monitoring for the duration. Data were analyzed cross-sectionally and longitudinally. Cross-sectionally we determined the prevalence of each histogram type overall and in relation to the type of respiratory support being administered, and the mean (±SD) of the median time spent in SpO2 ≤80%, <85%, 88–92%, 85–95%, 90–95%, and >95% for each histogram type. Longitudinally we studied the natural history of oxygenation instability among premature infants as measured by histogram type from day 1 to discharge or transfer to a level II NICU.
During the time of the study, the target SpO2 range was 88–92%, and the alarm limits were set at 86–94% in infants where the fraction of inspired oxygen (FiO2) was >0.21 or 86–100% in infants with FiO2 = 0.21.
This was a pre-planned analysis of data obtained during a PDSA (Plan, Do, Study, Act—The W. Edwards Deming Institute, Ketchum, ID) audit aimed at increasing histogram use in the NICU, and was approved by the Institutional Review Board of our center with informed consent waived.
SpO2 and histograms
SpO2 was obtained continuously using pulse oximetry on the normal sensitivity setting, with a 0.5 Hz sampling rate (Radical; Masimo, Irvine, CA, USA) and was displayed with a 10-s averaging time. We used real-time 12-h histograms built with a 1-s real-time sampling rate, available as a standard option in Software Revision J.10.26, from the Phillips Intellivue MX800 monitors.
In this pragmatic study, we intended to create and use a common approach and language to document, communicate, and better understand individual oximetry data in the NICU. The pulse oximeter probe limb sitting was not standardized; the site was chosen by nursing based on nursing considerations, and nursing was responsible to obtain the best possible oximeter signal at all times. Furthermore, there were no SpO2 validation rules, and we did not exclude areas of data dropout (SpO2 = 0 and pulse rate = 0) or areas of excessive variability or consider the variables related to signal quality such as Signal IQ- signal identification and quality indicator, Signal IP- signal perfusion index, or pulse rate to heart rate correlation.
Histogram classification
In every SpO2 histogram (Fig. 1a), the horizontal axis shows the range of the displayed SpO2; we set the SpO2 range from 81 to 100% and the unit width at 1%. The vertical axis shows the percentage of time. The bars in the foreground (black) show that the percentage-of-time SpO2 values fall into each unit on the scale. The bars in the background (gray) show the cumulative percentage-of-time value, which results from adding each of the foreground bars to the sum of those to its left. The percentage of time with SpO2 below 81% is shown as a single percentage-of-time cumulative frequency bar to the left of the 81% bar. The median SpO2 in each histogram is the interpolated SpO2 of the cumulative bar(s) with percentage-of-time value of 50%.
We classified SpO2 histograms based on the number of cumulative (background) bars with percentage-of-time value >10% and <90%, and the percentage-of-time value of the cumulative frequency bar to the left of 81% (the ≤80% bar). In type 1 histograms, the number of background bars with value >10% and <90% is <5, in type 2 histograms it is 5–9, and in type 3–5 histograms it is ≥10. Type 3–5 histograms are differentiated by the height of the ≤80% bar: in type 3 it is <5%, in type 4 it is 5–9%, and in type 5 it is ≥10% (Fig. 1b, c).
Study procedure
SpO2 histograms were printed twice daily at pre-set times for all participating infants from the first day of life until the infant was discharged home or transferred to a different NICU.
For each histogram, the respiratory support and oxygen supplementation for the previous 12-h period were documented. Non-intubated respiratory support included heated humidified high flow by nasal cannula, CPAP, and bi-level CPAP. Intubated respiratory support included conventional ventilation, high-frequency oscillatory ventilation, and high-frequency jet ventilation. When a change in support type was made during a recorded period, the highest support given during that period was assigned.
In type 1 and 2 histograms, SpO2 remains within a relatively narrow range, so we broadly called them Stable, while in type 3–5 histograms, SpO2 swings more widely, so we called these Unstable histograms.
Statistical analysis
Statistical analysis was performed with the SPSS v25.0 package (IBM, Armonk, NY).
Patient demographics are shown as mean ± standard deviation (SD). Statistical analysis for the cross-sectional pathway began with simple counts to construct a frequency table of histogram types and obtain the mean (±SD) median saturation in each type. For each of six different SpO2 ranges, graphs of the mean (±SD) percentage of time spent in the specific range were plotted, to compare histogram types. Confidence intervals (CIs) of 95% were calculated for the 85–95% range and 90–95% range.
Continuous variables were compared using Student’s t test and categorical variables using the χ2 and Fisher’s exact tests, as appropriate. Differences were considered significant when p value was <0.05.
Results
One hundred and sixteen infants ≤34 weeks gestation were admitted to our NICU over the 264 days of observation. Eighty nine infants needed respiratory support on day 1 of life and 16 were excluded for congenital anomalies or technical difficulties, so that 73 infants with BW 1318.5 ± 495 g and gestational age (GA) 28.9 ± 3.0 weeks were studied. We obtained and analyzed 6016 consecutive histograms, 82 ± 78 histograms per infant, over a per-patient average of 46 ± 44 days. Figure 2 shows the prevalence of each histogram type overall and in relation to the type of respiratory support being administered. The absolute and relative incidence of each histogram type is shown for each category of interest. All histogram types were common, but their prevalence was different (p < 0.00001). The histogram type distribution in extubated vs. intubated respiratory support was different both during periods when in FiO2 = 0.21 and >0.21 (p < 0.00001).
Histogram prevalence study. Prevalence of each histogram type, for infants in FiO2 = 0.21, FiO2 >0.21, and by form of respiratory support. The mean ± SD of the SpO2 medians was the same in histogram Types 2–5. GA and BW are expressed as mean ± SD and age at entry as median (IQR). Supplemental oxygen by itself was not considered as respiratory support
In histograms obtained in FiO2 >0.21, the overall mean (±SD) of SpO2 medians was 92.8 ± 1.9% and was similar to that in types 2–5 histograms. This median SpO2 lies within the alarm limits range of 86–94% used in our NICU and within the now recommended SpO2 target of 90– 95%, but was higher than our NICU SpO2 targets of 88–92%.
Only 56 (2%) of 2811 histograms in FiO2 >0.21 were type 1 with a mean (±SD) of SpO2 medians of 95.1 ± 2.6%, but in 23 of these type 1 histograms the median SpO2 was >95% and the mean (SD) SpO2 medians was 97.9 (0.9)%, and in 33 type 1 histograms the median SpO2 was ≤95% and the mean (SD) SpO2 medians was 92.9 (1.1)%.
The time spent within different saturation ranges for histograms obtained in FiO2 >0.21 is illustrated in Fig. 3. The mean time spent in our then SpO2 target zone 88–92% was 26 ± 11% and was similar for all histogram types, and the mean time spent in the SpO2 85–95% alarm zone and in the 90–95% zone was 65 ± 18% and 50 ± 15%. The higher the histogram type, the more time was spent in the SpO2 <85 and <80% zones (p <0.01). The mean difference in time >95% between type 1 vs. types 2–5 was 24% (95% confidence interval (CI) 20–28).
Histograms remained stable throughout hospital stay in 39 infants with GA 31.3 ± 1.1 and BW 1633 ± 375.5 g, whereas in 34 infants with GA 26.4 ± 2.1 and BW 957 ± 345.1 g, histograms showed an initial stable phase with only type 1 and 2 histograms, followed by an unstable phase with type 3–5 histograms and then a final stable (resolution) phase when the histogram types returned to stable.
The median (IQR) duration of the initial stable phase was 6.3 (4.1) days and the duration of the unstable phase was 49.5 (35) days. All studied infants returned to a stable (resolution) phase prior to discharge, with the exception of two infants who died during the unstable phase. In addition, one infant was transferred to a different level III NICU during the unstable phase and lost to follow-up.
Table 1 presents the respiratory outcomes of all infants born at ≤28 weeks gestation, who entered the unstable phase during the first week of life (n = 18), compared to infants who did not enter the unstable phase during the first week of life (n = 10).
Discussion
The SpO2 histogram classification system provides the clarity of a common language and reveals the presence and magnitude of SpO2 instability, as well as the natural history among premature infants. It also shows that SpO2 instability is common and distinct from the SpO2 median. Further, because it is the SpO2 median that is being targeted during clinical care, the SpO2 median is insensitive to the degree of SpO2 instability. Thus, our data show that for periods in FiO2 >0.21, the overall mean (±SD) of SpO2 medians was 92.8 ± 1.9%, and was similar to that in types 2–5 histograms. As such, the degree of SpO2 instability needs to be documented separately and in addition to the SpO2 median.
Our study is the first to describe and classify SpO2 histograms in the NICU in support of clinical care. Other studies have reported on how hypoxemic events impact clinical outcomes. Poets et al.7 in a post hoc analysis of the COT trial11 has reported that hypoxemic events were associated with death or disability in 56.5% in the highest decile vs. 36.9% in the lowest decile of hypoxemic exposure. However, the effect of cumulative hypoxemia on death or disability was not examined. Others have shown that oxygen desaturation events are associated with the development of BPD5 and that infants diagnosed with BPD had increased frequency and duration of intermittent hypoxemia episodes during the first 26 days of life as well as lower baseline SpO2.6
We here show that unstable histograms during that first 7 days of life among extremely low gestational age newborns (ELGAN) identify infants at risk of longer ventilatory support and need for supplemental oxygen, and at increased risk of being on ventilatory support at 40 weeks.
Prospective data on how to safely and effectively decrease intermittent hypoxemia is limited partly due to the fact that these events are poorly documented and quantified. These events, observed in the presence and absence of assisted ventilation, are distinct from those due solely to immature respiratory control. Hypoxemic events in mechanically ventilated premature infants are triggered by forced exhalations that produce a decrease in lung volume with a subsequent increase in airway resistance and a drop in lung compliance.12 While it is not yet known if newer ventilatory strategies will be able to lessen prolonged cumulative hypoxemia as detected by type 3–5 histograms, histogram type documentation should be considered an important outcome variable in trials aimed at improving respiratory support and/or automatically regulating oxygen administration in infants.
The main limitation of our study is that we did not systematically track periods with motion artifact that potentially might have altered histogram type, but because the Masimo signal extraction technology minimizes the occurrence of artifact-based low values,13 and because we used histograms summarizing 12 h rather than shorter periods, we think that motion artifact should have a small effect on our results. Also, our study was a descriptive study and was not powered to look for the correlation between histogram types and GA, respiratory support, and neonatal morbidities.
Displaying, describing, and documenting SpO2 instability is now possible. If we are to improve oxygen targeting, more clinical attention needs to be paid to infants with unstable histograms. Research aimed at decreasing the prevalence of type 3–5 histograms and cumulative time in the hypoxic range is likely to improve neurodevelopmental outcomes.
References
Di Fiore, J. M. et al. A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J. Pediatr. 157, 69–73 (2010).
Ratner, V. et al. Hypoxic stress exacerbates hyperoxia induced lung injury in a neonatal mouse model of bronchopulmonary dysplasia. Neonatology 95, 299–305 (2009).
Ratner, V. et al. The contribution of intermittent hypoxemia to late neurological handicap in mice with hyperoxia-induced lung injury. Neonatology 92, 50–58 (2007).
Juliano, C. et al. Mild intermittent hypoxemia in neonatal mice causes permanent neurofunctional deficit and white matter hypomyelination. Exp. Neurol. 264, 33–42 (2015).
Fairchild, K. D., Nagraj, V. P., Sullivan, B. A., Moorman, J. R. & Lake, D. E. Oxygen desaturations in the early neonatal period predict development of bronchopulmonary dysplasia. Pediatr. Res. 85, 987–993 (2019).
Raffay, T. M. et al. Neonatal intermittent hypoxemia events are associated with diagnosis of bronchopulmonary dysplasia at 36 weeks postmenstrual age. Pediatr. Res. 85, 318–323 (2019).
Poets, C. F. et al., Canadian Oxygen Trial Investigators. Association between intermittent hypoxemia or bradycardia and late death or disability in extremely preterm infants. JAMA 314, 595–603 (2015).
Jain, D., Claure, N., D’Ugard, C., Bello, J. & Bancalari, E. Volume guarantee ventilation: effect on preterm infants with frequent hypoxemia episodes. Neonatology 110, 129–134 (2016).
McEvoy, C. et al. Prone positioning decreases episodes of hypoxemia in extremely low birth weight infants (1000 grams or less) with chronic lung disease. J. Pediatr. 130, 305–309 (1997).
Abu Jawdeh, E. G., Martin, R. J., Dick, T. E., Walsh, M. C. & Di Fiore, J. M. The effect of red blood cell transfusion on intermittent hypoxemia in ELBW infants. J. Perinatol. 34, 921–925 (2014).
Schmidt, B. et al., Canadian Oxygen Trial (COT) Group. Effects of targeting higher vs lower arterial oxygen saturations on death or disability in extremely preterm infants: a randomized clinical trial. JAMA 309, 2111–2120 (2013).
Bolivar, J. M. et al. Mechanisms for episodes of hypoxemia in preterm infants undergoing mechanical ventilation. J. Pediatr. 127, 767–773 (1995).
Sahni, R., Gupta, A., Ohira-Kist, K. & Rosen, T. S. Motion-resistant pulse oximetry in neonates. Arch. Dis. Child Fetal Neonatal Ed. 88, F505–F508 (2003).
Author information
Authors and Affiliations
Contributions
All authors take responsibility for the reported findings and have participated in the concept and design, analysis and interpretation of data, drafting or revising, and approval of this manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borenstein-Levin, L., Konikoff, L. & Solimano, A. Clinical quantification of SpO2 instability using a new histogram classification system: a clinical study. Pediatr Res 87, 716–720 (2020). https://doi.org/10.1038/s41390-019-0566-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0566-6
This article is cited by
-
The effect of changing respiratory rate settings on CO2 levels during nasal intermittent positive pressure ventilation (NIPPV) in premature infants
Journal of Perinatology (2023)
-
Oxygen saturation histogram classification system to evaluate response to doxapram treatment in preterm infants
Pediatric Research (2023)
-
Oxygenation in the NICU: there is more to it than meets the eye
Pediatric Research (2023)
-
Histogram analysis for bedside respiratory monitoring in not critically ill preterm neonates: a proposal for a new way to look at the monitoring data
European Journal of Pediatrics (2021)
-
Oxygen saturation histograms predict nasal continuous positive airway pressure-weaning success in preterm infants
Pediatric Research (2020)