Abstract
Background
Photobiomodulation by 670 nm red light in animal models reduced severity of ROP and improved survival. This pilot randomised controlled trial aimed to provide data on 670 nm red light exposure for prevention of ROP and survival for a larger randomised trial.
Methods
Neonates <30 weeks gestation or <1150 g at birth were randomised to receive 670 nm for 15 min (9 J/cm2) daily until 34 weeks corrected age. Data collected: placental pathology, growth, days of respiratory support and oxygen, bronchopulmonary dysplasia, patent ductus arteriosus, necrotising enterocolitis, sepsis, worst stage of ROP, need for laser treatment, and survival.
Results
Eighty-six neonates enrolled—45 no red light; 41 red light. There was no difference in severity of ROP (<27 weeks—p = 0.463; ≥27 weeks—p = 0.558) or requirement for laser treatment (<27 weeks—p = 1.00; ≥27 weeks—no laser treatment in either group). Survival in 670 nm red light treatment group was 100% (41/41) vs 89% (40/45) in untreated infants (p = 0.057).
Conclusion
Randomisation to receive 670 nm red light within 24–48 h after birth is feasible. Although no improvement in ROP or survivability was observed, further testing into the dosage and delivery for this potential therapy are required.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) is a vaso-proliferative disorder of the retina affecting extremely preterm or low birth weight infants. The most devastating consequence of ROP is retinal detachment and blindness, which in most developed countries is reduced by careful screening and early treatment with either laser photocoagulation of avascular retina or intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) agents. However, ROP remains the leading cause of visual loss in children.1 In less severe cases, ROP will regress spontaneously, but in more severe cases invasive treatment with laser photocoagulation or intravitreal anti-VEGF injections is required to prevent retinal detachment.2 Despite regression of vascular changes, other abnormalities in vision still occur, including reduced visual acuity,3 reduced visual fields,4 reduced contrast sensitivity,5 refractive errors6 and strabismus.7 Guidelines have been developed for screening and treatment of ROP in premature and low birth weight infants.8,9 Use of these guidelines significantly reduces the risk of blindness and significant visual loss but does not prevent the disease from occurring nor all of the long-term visual consequences.10
Exposure to hyperoxia is considered to be one of the principle underlying causes for ROP. The in utero environment is relatively hypoxic (PaO2 25–35 mm Hg) compared to the ex utero environment (PaO2 60–100 mm Hg). This hyperoxic environment interferes with normal retinal vascular development, which eventually results in retinal hypoxia, fibrovascular proliferation and, in the worst cases, retinal detachment. Despite a number of clinical studies aimed at optimising pulse oximetry levels, ROP still persists.11,12 Given that the ex utero environment results in the developing retina being exposed to a higher PaO2, no matter how well controlled the pulse oximetry, other interventions need to be considered to prevent ROP from occurring.
Photobiomodulation using 670 nm red light might provide a novel treatment strategy to reduce the hyperoxic stage of ROP by reducing the harmful effects of reactive oxygen species (ROS) and restoring normal vessel development. Photobiomodulation light has been shown to promote wound healing in skin and oral mucosa13 and when delivered transcranially reduces cerebral pathology in animal models of brain damage and in human ischaemic stroke.14,15 Specifically in the retina, photobiomodulation using 670 nm red light-emitting diode (LED) light has been shown to protect photoreceptors from toxins and light-induced damage and reduce laser-induced retinal scarring,16,17,18,19,20,21 whether delivered to the eye directly or from the whole-body exposure. 670 nm red light has been shown to be absorbed by cytochrome c oxidase, the rate-limiting enzyme in the terminal phosphorylation of the mitochondria, and is proposed to act partly by repairing mitochondrial function and to increase the efficacy of ATP production and to reduce the creation of harmful by-products of ROS.22,23 This therapy might counteract the harmful effects of a hyperoxic environment, which is the initial phase of ROP development.
Photobiomodulation using 670 nm red LED light in oxygen-induced retinopathy animal models (which mimics facets of ROP including neovascularisation and photoreceptor cell death) reduced the extent of oxygen-induced retinal neovascularisation, decreased pulmonary haemorrhage and improved survival.24,25 We have previously shown that 670 nm red LED light is safe in preterm neonates, when delivered from a distance of 25 cm at a concentration of 9 J/cm2 for 15 min/day.26
Preliminary data to use for optimising dosage strategies prior to a large randomised controlled trial (RCT) are required. The aim of this pilot RCT were to provide data on treatment with 670 nm red LED light at a distance of 25 cm providing 9 J/cm2 in very premature neonates on reducing ROP and improving survival to be utilised for a larger RCT. The hypothesis of the study is that 670 nm red light commenced within 48 h after birth until 34 weeks postmenstrual age in very preterm neonates would reduce severe ROP and improve survival at the time of discharge from hospital.
Methods
Research design
A prospective randomised controlled study was performed in the Neonatal Intensive Care Unit (NICU) at the Canberra Hospital, Australia. The study was approved by the ACT Health Human Research Ethics Committee (eth.7.14.160) and is registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12619000371190).
Study population
Inclusion criteria
Neonates admitted to the NICU at <30 weeks gestation or <1150 g birth weight, whose parents provided informed consent, and 670 nm red light could be commenced within 48 h of birth were recruited.
Exclusion criteria
Neonates with chromosomal or significant congenital anomalies were excluded. Other exclusion criteria included inability to obtain consent within 48 h of birth or neonate considered too clinically unstable for 670 nm red light treatment in the first 48 h of life.
Neonates were randomised to intervention or control using a computer-generated randomisation protocol. Each neonate was given a study number and was entered into a commercially available trial data management program, Treonic (www.treonic.com). Research nurses and medical staff allocated to the study enrolled and entered participants. To ensure that equal numbers of extremely premature infants were randomised to intervention or control, the computer program stratified the randomisation by infant’s gestation (gestation ≤26 and >26 weeks) using randomisation blocks of 4. Infant’s allocation was revealed at time of enrollment. Masking of treatment allocation to the ophthalmologist performing the assessments for ROP occurred, but not of the clinical staff and researchers because of the nature of the intervention. Neonates >30 weeks gestation but with birth weight <1150 g were included in the 27–29 completed weeks group. Data were maintained on a password-protected database.
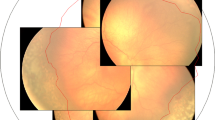
670 nm red light treatment was commenced on the day of entry into the study. A 670 nm LED was placed on the isolette 20–25 cm above the baby (in a similar fashion to phototherapy treatment) and was provided for 15 min each day (15 min provided 9 J/cm2 using a Warp 75 LED device, Quantum Devices, Inc., WI, USA) until 34 weeks corrected gestational age or until transfer to another level 2 unit. Neonates were dressed only in a nappy while receiving 670 nm red light. 670 nm red light is absorbed through the skin and acts at the cellular level, repairing mitochondrial function and increasing the efficacy of ATP production and reducing the creation of harmful by-products of ROS in the circulation to which the developing retina is exposed. Thus neonates do not have to have their eyes open to receive the effect of the 670 nm red light treatment. Neonates were treated with standard care for all other aspect of their care while in the NICU (Fig. 1) including maintaining oxygen saturations between 90% and 95%. While data were not formally collected, the unit practice was for nursing staff to have graphical representation of oxygen saturations on their monitor screen with the goal to be within this range 85% of the time over an 8–12 h shift. Patent ductus arteriosus (PDA) was managed using a physiological guideline. Initial treatment of a haemodynamically significant duct was with ibuprofen and surgical ligation utilised only after medical treatment failure and ongoing respiratory support with ventilation or continuous positive airway pressure required.
Babies who required phototherapy treatment for jaundice had blue light treatment suspended for 15 min in each 24-h period to administer 670 nm red light treatment.
Ophthalmological assessment was per the international standardised method,7 commencing at 32 weeks corrected gestational age and occurring weekly to fortnightly as required from a clinical perspective. Ophthalmological assessment was performed by qualified Ophthalmologists with the Royal Australasian College of Ophthalmologists who are well versed in the assessment of ROP. The Opthalmologists assessing the babies were masked to the treatment being received. The majority of assessments were performed by one Ophthalmologist (R.W.E.), with two other Ophthalmologists used when he was on leave.
Weight, length and head circumference data were collected weekly to assess growth. Data were collected on duration of oxygen requirement, incidence of chronic lung disease (oxygen requirement at 36 weeks postconceptional age), presence and treatment of a PDA, definite necrotising enterocolitis and number of septic episodes.
Placental pathology
Placenta were assessed prospectively as part of routine patient care with no knowledge of the neonates’ involvement in the study. In utero exposures to different pathologies has the potential to influence neonatal outcomes. Placental examination was included to exclude in utero experience as an independent influence on 670 nm red light treatment. In each case, a standard macroscopic description and sampling was performed according to current guidelines.27 The placentas were reassessed histologically by a perinatal pathologist masked to the study group but provided with gestational age. The assessment was comprehensive but specifically included the presence or absence of maternal or foetal inflammatory response to ascending intrauterine infection, evidence of maternal or foetal vascular malperfusion, delayed villous maturation, evidence of chronic villitis, chronic intervillositis or maternal floor infarction using established definitions.27
The commencement of this RCT was a precursor for a multicentre randomised controlled study with the following power calculation. ANZNN data from 2009 indicated that 31% of all infants <30 weeks gestation had any stage of ROP and 12.5% received laser treatment for ROP.28 For a reduction of any stage ROP from 31% to 20% and ROP requiring surgery from 12.5% to 7% with a two-sided significance level (1 − alpha) of 95 and power (1 − beta, %chance of detecting) of 90, the sample size required would be 700 per arm with a 6% loss to follow-up rate. For our institution with 100 patients in 2 years, we would expect 32 patients with any stage of ROP without treatment and 20 patients with any stage ROP with 670 nm red light treatment. This pilot study received local funding for 2 years and recruited 86 patients.
Statistical analyses were carried out using IBM SPSS Statistics (version 24.0.0.1; SPSS: SPSS, Inc., an IBM Company, Somers, NY, USA, 2016). Data are displayed as frequency and percentage (%) or median and inter-quartile range (IQR). Chi-square test and Mann–Whitney test are used where appropriate. Cox regression was performed to demonstrate independent influence of RED light on survival and ROP stage 3–4 after adjusting for antenatal steroid, gestational age, birth weight and gender. All p values were two-sided, and values <0.05 were considered statistically significant.
Results
Eighty-six neonates were enrolled in the study between March 2015 and January 2017. The trial ended at the end of 2 years of funding, with recruitment of 86 patients. Five neonates were not enrolled owing to inability to obtain parental consent within 48 h due to mother being in intensive care (Fig. 2). No parents declined the study. The neonates were block randomised into two gestation groups: 24–26 weeks gestation (n = 25; 14 no 670 nm red light; 11 670 nm red light) and 27–29 weeks gestation or birth weight <1150 g with gestation >29 weeks (n = 61; 30 no 670 nm red light; 31 670 nm red light). There were no adverse effects noted with the group receiving 670 nm red light.
The demographics for those enrolled in the study are shown in Table 1. Those not receiving red light were less likely to receive a complete course of antenatal steroids (p = 0.026). There were no differences between the weight, length and head circumference growth from birth to 34 weeks corrected gestational age in those neonates who received red light treatment and those who did not (Table 1).
The results of retinopathy of prematurity assessment and survival are shown in Table 2. Any stage of retinopathy in the untreated group was 31% (14/45) and in 26.8% (11/41) in the 670 nm red light group (p = 0.46). Survival in the 670 nm red light treatment group was 100% (41/41) vs 89% (40/45) in untreated infants (p = 0.057). There were no observed differences in survival between the study groups when separated into different gestational age groups. There was also no observed difference in the severity of ROP, need for laser treatment and survival when separated into different gestational age groups. These results did not change after adjusting for antenatal steroid, gestational age, birth weight and gender. The time to ROP stage 3–4 or death was not statistically different between the study groups (Figs. 3 and 4).
There were no significant differences between the placental findings between the neonates who received and did not receive red light treatment. There was a significant increase in stage 3–4 ROP related to acute chorioamnionitis (maternal inflammatory response), acute vasculitis/funisitis (foetal inflammatory response) and maternal vascular malperfusion (accelerated villous maturation) (p = 0.005, 0.034 and 0.037, respectively) (Table 3).
Discussion
This is the first randomised controlled study in premature neonates assessing the use of 670 nm red light. This pilot RCT was performed to determine feasibility and whether the distance and dose in animal studies provided similar results in reducing ROP and survivability. A study of 700 neonates in each arm is required to show a reduction in severe ROP. This small pilot study did not show a difference in severity of ROP but may indicate an improvement in survival and, as with our previous study,26 that 670 nm had no adverse effects on the treated neonates.
A number of clinical treatments and RCTs are being developed using wavelengths that are near the infrared spectrum including 670 nm.29 These RCTs are registered with the World Health Organisation International Clinical Trials Registry including studies treating back pain, stroke and traumatic brain injury. Near-infrared therapy has been used in a number of smaller studies with no adverse effects and most recently has been shown to increase peripheral blood flow,30 reduce osteoarthritis in knee joints31 and improve wound healing in chronic diabetic foot ulcers.32
Acute chorioamnionitis (maternal inflammatory response) and acute vasculitis/funisitis (foetal inflammatory response) were associated with an increased risk of ROP in our study. The literature associating ROP and inflammatory conditions of the placenta is varied with some reporting an association and others no association.33,34 A large multicentre study should include placental pathology to aid in answering whether inflammatory conditions of the placenta have an influence on the development of ROP.
This study has not looked at the long-term neurological or visual outcomes of the neonates enrolled in this study. Follow-up of very low birth weight infants is predominantly focussed on neurological development with blindness being the main factor assessed, rather than other subtle degrees of visual impairment. While resolution of ROP is frequently spontaneous, it can be associated with decreased visual acuity and an increased incidence of myopia, strabismus and amblyopia. Assessments of these visual findings are difficult in the neonatal period but can be more reliably done in pre-school age children with current screening tools.35,36 In a large multicentre trial, long-term neurological assessment as well as visual acuity should be included.
This study was funded as a pilot randomised trial to obtain preliminary data for a large multicentre RCT. There are a number of limitations to the study to aid in planning a large multicentre study. The length of time exposed to 670 nm red light due to the cut-off time of 34 weeks postmenstrual gestation may have influenced the results. This decision was based on the physiological principle that during the hyperoxic phase in the first weeks after birth the production of ROS would potentially be at its highest and that the 670 nm red light treatment would reduce the amount of ROS exposure. The dose of red light treatment administered to the neonates was based on original animal studies.24,25 However, the exact treatment times and distance from the light source was modified in this pilot study due to the need for neonates to be nursed in humidified isolettes. In the original animal study,24,25 red light was applied for 3 min at a distance of 2.5 cm providing 9 J/cm2 focussed mainly on the head of the animal. As a consequence of the neonates being in humidified isolettes, access to close treatment strategy was not possible. In order to maintain dosage at 9 J/cm2, a longer duration (15 min) and distance to treatment (~25 cm) was required. It is unclear if this more distant longer treatment strategy is as effective as the previously used close source treatment strategy. Further studies in both animal models and neonates is required to assess the validity of this modification in treatment strategy. Further, a conservative amount of 9 J/cm2 was used for this study, with others showing that exposures up to 50 J/cm2 caused no adverse effects in adults.29 Further studies examining distance, dosage and timing of dosage are required to aid in the future design of a multicentre clinical trial.
This study has shown the low prevalence of severe ROP in neonates >26 weeks gestation in an Australian NICU. Future modelling for a RCT should base the number of neonates to be included in the study on those <27 weeks gestation to minimise the number of neonates unnecessarily involved in an RCT.
Conclusions
This pilot RCT of 670 nm red light provides preliminary data for a larger randomised trial, indicating that future studies should focus on neonates born <27 weeks gestation. While this study was not powered adequately for ROP or survivability, the findings support further testing into the dosage and delivery methods of 670 nm red light in a clinical setting.
References
Haddad, M. A. O., Sei, M., Sampaio, M. W. & Kara-Jose, N. Causes of visual impairment in children: a study of 3210 cases. J. Pediatr. Ophthalmol. Strabismus 44, 232–240 (2007).
Early Treatment for Retinopathy of Prematurity Cooperative Group et al.Final visual acuity results in the early treatment for retinopathy of prematurity study. Arch. Ophthalmol. 128, 663–671 (2010).
Larsson, E. K., Rydberg, A. C. & Holstrom, G. E. A population-based study on the visual outcome in 10 year-old preterm and full-term children. Arch. Ophthalmol. 123, 825–832 (2005).
Larsson, E., Martin, L. & Holmstrom, G. E. Peripheral and central visual fields in 11-year old children who had been born prematurely and at term. J. Pediatr. Ophthalmol. Strabismus 41, 39–45 (2004).
Larsson, E., Rydberg, A. & Holmstrom, G. E. Contrast sensitivity in 10 year old preterm and full term children: a population based study. Br. J. Ophthalmol. 90, 87–90 (2006).
Larsson, E. K., Rydberg, A. C. & Holmstrom, G. E. A population-based study of the refractive outcome in 10-year-old preterm and full-term children. Arch. Ophthalmol. 121, 430–436 (2003).
O’Connor, A. R. et al. Strabismus in children of birth weight less than 1701 g. Arch. Ophthalmol. 120, 767–773 (2002).
Section on Ophthalmology, American Academy of Pediatrics, American Academy of Ophthalmology, American Association for Pediatric ophthalmology and Strabismus. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 117, 572–576 (2006).
Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for treatment of retinopathy or prematurity: results of the Early Treatment for Retinopathy of Prematurity Randomized Trial. Arch. Ophthalmol. 121, 1684–1696 (2003).
Dobson, V. et al. Visual acuity at 10 years in Cryotherapy for Retinopathy of Prematurity (CRYO-ROP) study eyes: effect of retinal residua of retinopathy of prematurity. Arch. Ophthalmol. 124, 199–202 (2006).
SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network. Target ranges of oxygen saturation in extremely preterm infants. N. Engl. J. Med. 362, 1959–1969 (2010).
Askie, L. M. et al. NeOProM: Neonatal Oxygenation Prospective Meta-analysis Collaboration study protocol. BMC Pediatr. 11, 6 (2011).
Eells, J. T. et al. Mitochondrial signal transduction in accelerated wound and retinal healing by near-infrared light therapy. Mitochondrion 4, 559–567 (2004).
Oron, A. et al. Low-level laser therapy applied transcranially to rats after induction of stroke significantly reduces long-term neurological deficits. Stroke 37, 2620–2624 (2006).
Lampl, Y. et al. Infrared laser therapy for ischemic stroke: a new treatment strategy. Results of the NeuroThera Effectiveness and Safety Trial-1 (NEST-1). Stroke 38, 1843–1849 (2007).
Eells, J. T. et al. Therapeutic photobiomodulation for methanol-induced retinal toxicity. Proc. Natl Acad. Sci. USA 100, 3439–3444 (2003).
Albarracin, R., Eells, J. & Valter, K. Photobiomodulation protects the retina from light-induced photoreceptor degeneration. Invest. Ophthalmol. Vis. Sci. 52, 3582–3592 (2011).
Albarracin, R. & Valter, K. Treatment with 670-nm light protects the cone photorecptors from white light-induced degeneration. Adv. Exp. Med. Biol. 723, 121–128 (2012).
Albarracin, R. & Valter, K. 670 nm red light preconditioning supports Muller cell function: evidence from the white light-induced damage model in the rat retina. Photochem. Photobiol. 88, 1418–1427 (2012).
Qu, C., Cao, W., Fan, Y. & Lin, Y. Near-infrared light protects the photoreceptor from light-induced damage in rats. Adv. Exp. Med. Biol. 664, 365–374 (2010).
Eells, J. et al. Photobiomodulation for the treatment of retinal injury and retinal degenerative diseases. In Proc. Light Activated Tissue Regeneration and Therapy Conference. Lecture Notes in Electrical Engineering, Vol. 12 (eds Waynant, R. & Tata, D.) 39–51 (Springer, Boston, MA, 2008).
Liang, H. L. et al. Photobiomodulation partially rescues visual cortical neurons from cyanide-induced apoptosis. Neuroscience 139, 639–649 (2006).
Tafur, J. & Mills, P. J. Low-intensity light therapy: exploring the role of redox mechanisms. Photomed. Laser Surg. 26, 323–328 (2008).
Natoli, R. et al. 670nm photobiomodulation as a novel protection against retinopathy of prematurity: evidence from oxygen induced retinopathy models. PLoS ONE 8, e72135 (2013).
Albarracin, R. et al. 670 nm light mitigates oxygen-induced degeneration in C57BL/6J mouse retina. BMC Neurosci. 14, 125 (2013).
Kent, A. L. et al. A safety and feasibility study of the use of 670nm red light in premature neonates. J. Perinatol. 35, 493–496 (2015).
Khong, Y. T. et al. Sampling and definitions of placental lesions. Amsterdam Placental Workshop Group Consensus Statement. Arch. Pathol. Lab. Med. 140, 698–713 (2016).
ANZNN (Australia and New Zealand Neonatal Network). Report of the Australian and New Zealand Network 2008 and 2009 (ANZNN, Sydney, 2012). https://npesu.unsw.edu.au/sites/default/files/npesu/data_collection/Report%20of%20the%20Australian%20and%20New%20Zealand%20Neonatal%20Network%202012.pdf
Fitzgerald, M. et al. Red/near-infrared irradiation therapy for treatment of central nervous system injuries and disorders. Rev. Neurosci. 24, 205–226 (2013).
Mitchell, U. H. & Mack, G. L. Low-level laser treatment with near-infrared light increases venous nitric oxide levels acutely: a single-blind, randomized clinical trial of efficacy. Am. J. Phys. Med. Rehabil. 92, 151–156 (2013).
Al Rashoud, A. S., Abboud, R. J., Wang, W. & Wigderowitz, C. Efficacy of low-level laser therapy applied at acupuncture points in knee osteoarthritis: a randomised double-blind comparative trial. Physiotherapy 15, 242–248 (2014).
Kajagar, B. M., Godhi, A. S., Pandit, A. & Khatri, S. Efficacy of low level laser therapy on wound healing in patients with chronic diabetic foot ulcers—a randomised control trial. Indian J. Surg. 74, 359–363 (2012).
Mitra, S., Aune, D., Speer, C. P. & Saugstad, O. D. Chorioamnionitis as a risk factor for retrinopathy of prematurity: a systematic review and meta-analysis. Neonatology 105, 189–199 (2014).
Kim, C. Y. et al. Chronic placental inflammation as a risk factor of severe retinopathy of prematurity. J. Pathol. Transl. Med. 52, 290–297 (2018).
Ciner, E. B. et al. Stereoacuity of preschool children with and without vision disorders. Optom. Vis. Sci. 91, 351–358 (2014).
Ying, G. S. Sensitivity of screening tests for detecting vision in preschoolers-targeted vision disorders when specificity is 94%. Optom. Vis. Sci 82, 432–438 (2005).
Acknowledgements
This study was funded by the Canberra Hospital Private Practice Fund.
Author information
Authors and Affiliations
Contributions
A.K. conceived, developed and managed the study; analysed the results and prepared and finalised the manuscript; M.E.A.-L., B.S. and R.N. was involved in the conception of the study, analysed the results and approved the final manuscript; T.C. helped conceive the study, analysed the results and approved the final manuscript; MB was involved in the conception of the study, managed the study and approved the final manuscript; J.E.D. was involved in the conception of the study, assessed the placentas, analysed the results and approved the final manuscript; R.W.E. was involved in the conception of the study, performed the eye examinations, analysed the results and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
The mother of the patient gave consent for publication of Fig. 1.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kent, A.L., Abdel-Latif, M.E., Cochrane, T. et al. A pilot randomised clinical trial of 670 nm red light for reducing retinopathy of prematurity. Pediatr Res 87, 131–136 (2020). https://doi.org/10.1038/s41390-019-0520-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0520-7