Abstract
Background
Outcomes of infants with congenital diaphragmatic hernia (CDH) are primarily dependent on the severity of pulmonary hypoplasia. It is previously unknown whether postnatal lung growth in infants with CDH represents true parenchymal lung growth or merely an expansion in volume of the existing tissue. We hypothesized that lung volume growth in CDH infants will be accompanied by an increase in lung mass and that CDH infants will demonstrate accelerated catch-up growth of the more hypoplastic lung.
Methods
We used fetal and post-CDH repair MRI of 12 infants to measure lung volume and density, which was used to calculate lung mass.
Results
The average increase in right lung mass was 1.1 ± 1.1 g/week (p = 0.003) and the average increase in left lung mass was 1.8 ± 0.7 g/week (p < 0.001). When the ratio of left-to-right lung mass of the prenatal MRI was compared to post-repair MRI, the ratio significantly increased in all infants with average prenatal and post-repair ratios of 0.30 and 0.73, respectively (p = 0.002).
Conclusion
Lung growth in infants with CDH is indeed growth in lung mass (i.e. parenchyma), and the lungs demonstrate catch-up growth (i.e., increased rate of growth in the more hypoplastic ipsilateral lung).
Similar content being viewed by others
Introduction
Although the primary defect in infants with congenital diaphragmatic hernia (CDH) is a hole in the diaphragm, the outcome in these infants is primarily dependent on the severity of the pulmonary hypoplasia.1,2,3,4,5,6,7,8,9,10,11 Several studies have evaluated pulmonary hypoplasia during the prenatal period and developed a variety of markers of severity, including total lung volume (TLV), lung area-to-head circumference ratio (LHR), observed-to-expected LHR (O:E LHR), and percent predicted lung volume (PPLV).7,12,13,14,15,16,17 All of these studies have demonstrated a correlation between these prenatal markers, CDH severity, and postnatal outcomes. However, our knowledge of postnatal lung growth in this population is limited. Our previous work by Schopper et al. utilized conventional magnetic resonance imaging (MRI) techniques to measure postnatal lung volumes in CDH infants following diaphragmatic hernia repair and demonstrated that postnatal lung volumes increased, with the contralateral lung volume growing faster than the ipsilateral lung in most patients.18 Importantly, they demonstrated that postnatal lung volume growth was faster in the more severe CDH patients, suggesting the potential for catch-up lung volume growth. Comparisons between lung volume growth and weight gain in their population demonstrated that catch-up lung volume growth was increased in infants who had greater prenatal and postnatal weight gain.
Because the fetal lung is filled with fluid and subjected to minimal inflation pressures, and thus the fetal lungs have approximately constant density, it is generally accepted that prenatal lung volume correlates reliably with lung mass and is therefore a proxy for lung growth. In contrast, the postnatal lung is air-filled, with overall lung density influenced by inflation pressures of mechanical ventilation or normal respiration.19,20 Since the postnatal MRI sequences used by Schopper et al. could only detect lung volume and not density, this previous work could not measure any longitudinal changes in lung mass. Therefore, it is uncertain whether the lung volume growth observed in Schopper et al. represented true lung growth (i.e., increase in lung tissue mass) or merely an expansion in volume of the existing lung tissue. Following the study by Schopper et al., our group (Higano et al.) demonstrated that ultrashort echo time (UTE) MRI can accurately measure lung density in neonates on a range of respiratory supports (room air to mechanical ventilation), with density results similar to computed tomography (the current gold standard).21,22,23 In the current study, we used postnatal UTE MRI to determine lung volume, density, and mass in CDH infants following diaphragmatic hernia repair. We hypothesized that lung volume growth in CDH infants will be accompanied by an increase in lung mass and that CDH infants will demonstrate accelerated catch-up growth of the more hypoplastic lung. This novel lung mass measurement allows us to evaluate postnatal lung growth in CDH infants, differentiating increases in lung volume from actual growth of lung parenchymal mass.
Methods
This study was approved by the Cincinnati Children’s Hospital Medical Center Institutional Review Board. The study population included all infants with CDH admitted to Cincinnati Children’s Hospital Medical Center from January 1, 2015 to December 31, 2017. One infant was also included in the study by Schopper et al.18 Infants were excluded if they were diagnosed with CDH postnatally, were not viable at birth, had a right-sided diaphragmatic defect, had a diagnosis of congenital heart disease or other congenital malformations affecting life expectancy or cardiopulmonary development, had contraindication for MRI, were not clinically stable enough to undergo MRI, had weight >4.5 kg at the time of postnatal MRI (due to size constraints of our neonatal MRI scanner), or had insufficient image quality for data analysis (i.e., motion artifacts). Infants received no prenatal intervention.
Fetal pulmonary MRI was obtained as part of the normal clinical evaluation and performed in early (20–26 weeks) and late (30–34 weeks) gestation using a 1.5-T scanner without maternal or fetal sedation.3,24 The fetal MRIs were reviewed and analyzed for measurement of total lung volumes by staff radiologist experienced in interpreting fetal MRIs. Sonographically measured O:E LHR was obtained as part of the normal clinical evaluation and was used to prenatally determine CDH severity (mild disease: O:E >45, moderate disease: O:E 25–45, severe disease: O:E <25).17
All infants were managed by a team of CDH specialists at our institution following standard treatment protocols. After birth, the infants were intubated and stabilized with gentle ventilation and nitric oxide. The timing of the diaphragm repair was determined by the clinical team.
When the clinical team determined the infant was stable (following repair of the diaphragmatic defect), the infants underwent a tidal-breathing pulmonary MRI. The MRI was obtained using a small-footprint, neonatal-sized 1.5 T orthopedic MRI scanner adapted for use within our neonatal intensive care unit.25,26,27 Three-dimensional radial UTE images were acquired in all patients (repetition time/echo time ~5/0.2 ms; 5° flip angle; 18 cm field of view; ~0.7 mm resolution in each direction; ~10–16 min scan time; and ~120,000–200,000 radial projections).21,22,23 Using previously published methods, images were retrospectively respiratory-gated to end-expiration using UTE MR raw data with an acceptance window of 50%, allowing for accurate measurement of pulmonary density in infants on a wide range of support levels. No sedation or intravenous contrast was administered for the MRI procedure, unless sedation was a part of the patient’s ongoing clinical care. Patients were fed, swaddled, and equipped with ear protection before MRI. Respiratory support during MRI ranged from comfortably breathing on room air to nasal cannula oxygen to full ventilator support (see Table 1).
The following MRI parameters were measured at prenatal and postnatal periods from MRI analysis: TLV, right lung volume (RLV), left lung volume (LLV), total lung mass, right lung mass, and left lung mass. The fetal MRIs were reviewed and analyzed for the measurement of TLV, RLV, and LLV by a staff radiologist experienced in interpreting fetal MRIs. When both early and late prenatal scans were collected, the late scan was used. Previous autopsy studies have demonstrated a consistent fetal lung density of 1.15 g/cm3, therefore for the prenatal MRI, fetal lung mass was determined by multiplying the lung volume by this density value.19 The postnatal MRIs were analyzed using AMIRA (FEI Visualization Sciences Group, Hillsboro, Oregon); TLV, RLV, and LLV were determined via semi-automatic segmentation of the lungs (excluding major pulmonary vasculature) from the UTE images. Since UTE MRI was acquired in the proton-density regime as previously described,21 the lung density in g/cm3 was determined by measuring mean lung parenchymal signal and normalizing to the mean muscle signal. This density was multiplied by the lung volume to provide a measurement of lung mass.
The primary outcome measures were the total lung mass, right lung mass, and left lung mass determined from prenatal and postnatal post-repair MRI. The total, right, and left lung mass rates of growth were also calculated by dividing change in lung mass between prenatal and postnatal scans by the difference in gestational age at prenatal and postnatal scans. Clinical data gathered included gestational age at fetal MRI (weeks), corrected gestational age at postnatal MRI (weeks), birth weight (g), weight at the time of postnatal MRI (g), and CDH severity. The rate of weight gain (g/week) was calculated as weight gain from birth to time of post-repair MRI divided by the number of intervening weeks and was compared to the lung mass rate of growth.
Total, left, and right lung mass were compared between prenatal and post-repair scans using a paired Student’s t test. The differences between the left lung mass and the right lung mass at prenatal and post-repair scans were compared using a paired Student’s t test. The O:E LHR was used as a measure of severity, which was compared to the rate of lung growth using Pearson’s correlation. The rate of lung growth was compared with the rate of weight gain using Pearson’s correlation. For all tests, a p value of <0.05 was considered statistically significant.
Results
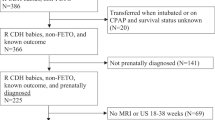
A total of 51 CDH babies were identified during the study period. One infant was excluded because of congenital malformations. Eight infants were excluded because they had no prenatal diagnosis of CDH, two infants had right-sided CDH, and five infants were excluded because they weighed >4.5 kg prior to reaching clinical stability. Fourteen infants were deceased prior to reaching clinical stability. Of the remaining 21 infants who met all of the inclusion/exclusion criteria, 19 consented for the study. Twelve infants had images of sufficient quality for data analysis. The demographic information and neonatal information are presented in Table 1.
All included infants had left-sided CDH. One infant had mild severity, 11 moderate, and no infants had severe CDH severity. There was a 10.4-week median interval between the prenatal and post-repair imaging studies, with 5.1 weeks prenatal and 4.7 weeks postnatal. The post-repair MRI occurred at a median of 3.2 weeks after surgical repair of the diaphragm.
The post-repair lung volume and density was measured in our study population, and the resulting lung mass was compared to prenatal lung mass derived from prenatal MRI lung volume. Total lung mass significantly increased in all infants with an average increase of 3.0 ± 1.3 g/week (p < 0.001; Fig. 1a). The average increase in contralateral (i.e., right) lung mass was 1.1 ± 1.1 g/week (p = 0.003; Fig. 1b), and the average increase in ipsilateral (i.e., left) lung mass was 1.8 ± 0.7 g/week (p < 0.001; Fig. 1c).
Prenatal and post-repair magnetic resonance imaging lung mass measurements in infants with mild (empty squares) and moderate (filled circles) congenital diaphragmatic hernia. Lung masses were calculated for the total lung (a), right lung (b), and left lung (c). Total lung mass significantly increased in all infants with an average increase of 3.0 ± 1.3 g/week (p < 0.001) (Total). The average increase in contralateral (right) lung mass was 1.1 ± 1.1 g/week (p = 0.003), and the average increase in ipsilateral (left) lung mass was 1.8 ± 0.7 g/week (p < 0.001)
To determine whether there was catch-up growth of the ipsilateral lung mass, the ratio of ipsilateral-to-contralateral lung mass at the time of prenatal versus post-repair MRI was compared. The ratios of ipsilateral-to-contralateral lung mass significantly increased between prenatal and post-repair MRI in all infants, with average prenatal and post-repair ratios of 0.30 ± 0.10 and 0.73 ± 0.34, respectively (p = 0.002; Fig. 2). There was a positive but non-significant correlation between the O:E LHR and the change in total (r = 0.554, p = 0.077), ipsilateral (r = 0.332, p = 0.319), and contralateral lung mass (r = 0.428, p = 0.190), normalized by birth weight, such that the change in lung mass/birth weight was lower in the patients with a lower O:E LHR and more severe CDH (Fig. 3a). However, when severity was compared to the difference in growth of the ipsilateral lung versus the contralateral lung, there was a negative trend between the O:E LHR and the difference in mass growth rate but this trend was not significant (r = −0.215, p = 0.526; Fig. 3b).
Ratio of left (ipsilateral) lung mass to right (contralateral) lung mass at prenatal and post congenital diaphragmatic hernia (CDH) repair time points in infants with mild (empty squares) and moderate (filled circles) CDH. The ratio significantly increased in all infants with average prenatal and post-repair ratios of 0.30 ± 0.10 and 0.73 ± 0.34, respectively (p = 0.002)
a Correlation of severity (observed-to-expected lung area-to-head circumference ratio (O:E LHR)) and rate of growth of total (blue circles), right (orange squares), and left (gray triangles) lung mass (g/week/birth weight). The change in total lung mass normalized to birth weight was lower in the patients with a lower O:E LHR and more severe congenital diaphragmatic hernia (total lung mass, Pearson’s r = 0.554, p = 0.077). b Comparison of severity (O:E LHR) and difference in mass growth rate of the ipsilateral (left) lung versus the contralateral lung (right)
Schopper et al. suggested that increased weight gain improved volume growth of the ipsilateral lung relative to the contralateral lung.18 Therefore, the impact of weight gain on the growth of the ipsilateral and contralateral lung mass was evaluated. While there was no correlation between weight gain and the mass growth of the contralateral lung normalized by birth weight (r = 0.091, p = 0.778), there was a positive but non-significant correlation between improved weight gain and increased mass growth of the ipsilateral lung normalized by birth weight (r = 0.497, p = 0.100; Fig. 4a). This trend continued when weight gain was compared to the difference in mass growth rate of the ipsilateral lung versus the contralateral lung (r = 0.428, p = 0.165; Fig. 4b), demonstrating an improved rate of mass growth in the ipsilateral lung compared to the contralateral lung in infants with improved weight gain.
a Correlation of infant weight gain (g/week) and rate of growth of right (orange circles) (Pearson’s r = 0.091, p = 0.778) and left (gray squares) (Pearson’s r = 0.497, p = 0.100) lung mass in infants with mild (empty markers) and moderate (filled markers) congenital diaphragmatic hernia (CDH). b Correlation of infant weight gain (g/week) and difference in mass growth rate of ipsilateral (left) and contralateral (right) lung (Pearson’s r = 0.428, p = 0.165) in infants with mild (empty marker) and moderate (filled marker) CDH
Discussion
Pulmonary hypoplasia is the primary cause of morbidity and mortality in several fetal and neonatal diagnoses, including CDH, omphalocele, congenital pulmonary airway malformations, congenital dysplastic renal disease, renal agenesis, lower urinary tract obstruction, and prolonged rupture of membranes causing oligohydramnios.28,29,30 While previous work suggested that the potential for catch-up growth in pulmonary hypoplasia via increases in lung volumes was possible, conclusions were limited since volume growth could not be definitively attributed to true lung parenchymal growth.18 Importantly, the current study answers this question for the first time by demonstrating a significant increase in lung mass between prenatal and post-repair time points, suggesting that this lung mass growth represents a true potential for catch-up growth in the hypoplastic lung.
We evaluated prenatal and post-repair lung mass in infants with CDH and found that total lung mass grew significantly between the prenatal and post-repair imaging time points. The average total lung mass at the prenatal MRI was 29.0 g, compared to 61.7 g at the time of post-repair MRI (p < 0.001). We also saw significant increase in the ipsilateral and contralateral lung mass during this period. Importantly, the ratio of the ipsilateral lung to the contralateral lung increased significantly, showing a faster increase in both the absolute and relative mass of the ipsilateral lung compared to the contralateral lung. The average ipsilateral-to-contralateral ratio at the prenatal scan was 0.30, compared to 0.73 at the post-repair MRI (p = 0.0017). This suggests that the lung ipsilateral to the diaphragmatic defect undergoes catch-up growth in the prenatal to post-repair period. This is a significant and previously unknown finding, as it demonstrates that the lungs grow in actual mass of parenchymal tissue, rather than simply suffering balloon-like volume expansion.
In order to evaluate the relationship between CDH severity and lung growth, the correlation between O:E LHR and rate of lung mass growth was evaluated. We demonstrated a positive trend between O:E LHR and the total lung mass rate of growth. This suggests that babies with higher O:E LHR and therefore less severe hypoplasia had better overall growth in lung mass. Individually, the ipsilateral lung mass and contralateral lung mass rate of growth show positive, non-significant trends, supporting the finding that less severity correlates with faster lung growth. Because increased severity coincides with worsening clinical status of the infant, the clinical status of the infant may confound the impact of CDH severity on lung growth. Therefore, to compensate for this factor, the contralateral lung was used as an internal control by comparing the relationship between the difference in the ipsilateral and contralateral lung mass growth versus the O:E LHR. Using this approach, we found a negative trend, suggesting that lower O:E LHR (i.e., more severe hypoplasia) correlated with a faster rate of ipsilateral lung growth compared to contralateral lung growth. Although this trend is certainly not significant, it is consistent with previous statistically significant findings by Schopper et al. that infants with more severe hypoplasia may have better catch-up growth of the ipsilateral lung.18
We have demonstrated overall and catch-up growth in the prenatal to post-repair time period, but the factors that influence this rate of growth and the potential areas of intervention are unknown. Possible influential factors include severity of hypoplasia, degree of prematurity, time of hernia repair, type of hernia repair, weight gain and nutrition, and postnatal interventions (extracorporeal membrane oxygenation, supplemental oxygen, etc.). To evaluate the impact of weight gain on lung growth, we compared the relationship between the rate of weight gain (g/week) and the rate of lung mass growth in the prenatal to post-repair period. Similar to previous results with lung volume growth, we found a positive trend of ipsilateral lung mass growth and improved weight gain (r = 0.497, p = 0.100). In contrast, the rate of contralateral lung mass growth showed no correlation with weight gain. This supports the hypothesis that the ipsilateral lung has improved rate of mass growth in infants with better weight gain. When weight gain was correlated with the difference in the rate of ipsilateral and contralateral lung mass growth, we again found a positive trend, such that infants with improved weight gain showed more catch-up mass growth of the ipsilateral lung (r = 0.428, p = 0.165). Since this comparison used the contralateral lung as an internal control, this positive trend suggests that the increased mass growth of the ipsilateral lung is more specific than simply a general growth in organ size associated with an increased rate of total body growth. This trend needs further investigation in a larger study, but confirmation of this trend has clinical impact, showing a possible modifiable factor that may improve lung growth of hypoplastic lungs.
The relatively small sample size is an important limitation on the statistical power of this study. We do form some preliminary conclusions in the current study using data that does not reach statistical significance; however, these conclusions are supported both by data from the current data set on lung mass growth and our previous evaluation of lung volume growth.18 Unfortunately, large study groups in this population are limited by the number of infants with CDH, the number of infants who survive to clinical stability, and the number of infants who are well enough to undergo MRI without sedation. The study also includes only left-sided CDH, so it is uncertain whether the same conclusions apply to right-sided CDH, which is far less common. The current study included no infants with severe hypoplasia. This limitation is likely due to the clinical instability and higher early mortality of these severe infants and the corresponding limited opportunities to obtain post-repair MRI. Further, we obtained only prenatal and post-repair MRI, which limits our ability to evaluate the impact of specific events (i.e. delivery, hernia repair, etc.) on the rate and linearity of growth. Our evaluation of lung mass growth related to weight gain is limited by the inability to differentiate accumulation of body fluid from true weight gain. It is possible that some of the weight gain we observed was due to the accumulation of fluid. However, it is more intuitive that the weight gain associated with improved lung growth is true nutritional growth as opposed to fluid accumulation. Clearly, further research is needed to investigate the relationship between weight gain and nutrition on lung growth in this population.
Finally, since the current study does not include analysis of lung histology or pulmonary function, we cannot claim that we are measuring normal lung development, but the evaluation of lung volume and lung mass is likely a strong representation of true lung growth. Since our cohort population was largely still in infancy at the time of analysis, we were not able to investigate correlations with follow-up pulmonary function tests. Future studies will aim to follow patients longitudinally to assess the impact on pulmonary function.
In the current study, we advance the use of postnatal MRI to evaluate lung growth in infants with pulmonary hypoplasia and demonstrate true growth in lung mass in CDH infants between prenatal and postnatal time points. Our data support the potential for catch-up lung growth in patients with pulmonary hypoplasia. In addition, our data suggest the potential importance of weight gain and good nutrition for growth of hypoplastic lungs and raises the opportunity for investigation of other factors that might improve lung growth and clinical outcomes in these patients.
References
Bebbington, M. et al. Comparison of ultrasound and magnetic resonance imaging parameters in predicting survival in isolated left-sided congenital diaphragmatic hernia. Ultrasound Obstet. Gynecol. 43, 670–674 (2014).
Busing, K. A. et al. MR relative fetal lung volume in congenital diaphragmatic hernia: survival and need for extracorporeal membrane oxygenation. Radiology 248, 240–246 (2008).
Coleman, A. et al. Fetal lung growth represented by longitudinal changes in MRI-derived fetal lung volume parameters predicts survival in isolated left-sided congenital diaphragmatic hernia. Prenat. Diagn. 35, 160–166 (2015).
Done, E. et al. Prenatal diagnosis, prediction of outcome and in utero therapy of isolated congenital diaphragmatic hernia. Prenat. Diagn. 28, 581–591 (2008).
Kehl, S. et al. Prediction of mortality and the need for neonatal extracorporeal membrane oxygenation therapy by 3-dimensional sonography and magnetic resonance imaging in fetuses with congenital diaphragmatic hernias. J. Ultrasound Med. 32, 981–988 (2013).
Kinane, T. B. Lung development and implications for hypoplasia found in congenital diaphragmatic hernia. Am. J. Med. Genet. C Semin. Med. Genet. 145C, 117–124 (2007).
Lee, T. C. et al. Late gestation fetal magnetic resonance imaging-derived total lung volume predicts postnatal survival and need for extracorporeal membrane oxygenation support in isolated congenital diaphragmatic hernia. J. Pediatr. Surg. 46, 1165–1171 (2011).
Lipshutz, G. S. et al. Prospective analysis of lung-to-head ratio predicts survival for patients with prenatally diagnosed congenital diaphragmatic hernia. J. Pediatr. Surg. 32, 1634–1636 (1997).
Metkus, A. P., Filly, R. A., Stringer, M. D., Harrison, M. R. & Adzick, N. S. Sonographic predictors of survival in fetal diaphragmatic hernia. J. Pediatr. Surg. 31, 148–151 (1996). Discussion 151–152.
Russo, F. M. et al. Lung size and liver herniation predict the need for extra corporeal membrane oxygenation but not pulmonary hypertension in isolated congenital diaphragmatic hernia: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 49, 704–713 (2016).
van den Hout, L. et al. Risk factors for chronic lung disease and mortality in newborns with congenital diaphragmatic hernia. Neonatology 98, 370–380 (2010).
Duncan, K. R., Gowland, P. A., Moore, R. J., Baker, P. N. & Johnson, I. R. Assessment of fetal lung growth in utero with echo-planar MR imaging. Radiology 210, 197–200 (1999).
Jani, J. et al. Value of prenatal magnetic resonance imaging in the prediction of postnatal outcome in fetuses with diaphragmatic hernia. Ultrasound Obstet. Gynecol. 32, 793–799 (2008).
Mahieu-Caputo, D. et al. Fetal lung volume measurement by magnetic resonance imaging in congenital diaphragmatic hernia. BJOG 108, 863–868 (2001).
Rypens, F. et al. Fetal lung volume: estimation at MR imaging-initial results. Radiology 219, 236–241 (2001).
Williams, G. et al. Fetal relative lung volume: quantification by using prenatal MR imaging lung volumetry. Radiology 233, 457–462 (2004).
Alfaraj, M. A. et al. Congenital diaphragmatic hernia: lung-to-head ratio and lung volume for prediction of outcome. Am. J. Obstet. Gynecol. 205, 43 e41–43 e48 (2011).
Schopper, M. A. et al. Evaluation of neonatal lung volume growth by pulmonary magnetic resonance imaging in patients with congenital diaphragmatic hernia. J. Pediatr. 188, 96–102 e101 (2017).
Breeze, A. C. et al. Postmortem fetal organ volumetry using magnetic resonance imaging and comparison to organ weights at conventional autopsy. Ultrasound Obstet. Gynecol. 31, 187–193 (2008).
Prodhomme, O. et al. Organ volume measurements: comparison between MRI and autopsy findings in infants following sudden unexpected death. Arch. Dis. Child. Fetal Neonatal Ed. 97, F434–F438 (2012).
Higano, N. S. et al. Quantification of neonatal lung parenchymal density via ultrashort echo time MRI with comparison to CT. J. Magn. Reson. Imaging 46, 992–1000 (2017).
Hahn, A. D. et al. Pulmonary MRI of neonates in the intensive care unit using 3D ultrashort echo time and a small footprint MRI system. J. Magn. Reson. Imaging 45, 463–471 (2017).
Higano, N. S. et al. Retrospective respiratory self‐gating and removal of bulk motion in pulmonary UTE MRI of neonates and adults. Magn. Reson. Med. 77, 1284–1295 (2017).
Phithakwatchara, N. et al. Differential patterns of prenatal ipsilateral and contralateral lung growth in cases of isolated left-sided congenital diaphragmatic hernia. Prenat. Diagn. 35, 769–776 (2015).
Tkach, J. A. et al. An MRI system for imaging neonates in the NICU: initial feasibility study. Pediatr. Radiol. 42, 1347–1356 (2012).
Walkup, L. L. et al. Quantitative magnetic resonance imaging of bronchopulmonary dysplasia in the neonatal intensive care unit environment. Am. J. Respir. Crit. Care Med. 192, 1215–1222 (2015).
Walkup, L. L. & Woods, J. C. Newer imaging techniques for bronchopulmonary dysplasia. Clin. Perinatol. 42, 871–887 (2015).
Wu, C. S., Chen, C. M. & Chou, H. C. Pulmonary hypoplasia induced by oligohydramnios: findings from animal models and a population-based study. Pediatr. Neonatol. 58, 3–7 (2016).
Page, D. V. & Stocker, J. T. Anomalies associated with pulmonary hypoplasia. Am. Rev. Respir. Dis. 125, 216–221 (1982).
Triebwasser, J. E. & Treadwell, M. C. Prenatal prediction of pulmonary hypoplasia. Semin. Fetal Neonatal Med. 22, 245–249 (2017).
Acknowledgements
This work was supported by an NIH grant 1T35HL113229-02 and The Perinatal Institute at Cincinnati Children’s Hospital.
Author information
Authors and Affiliations
Contributions
S.A.A., N.S.H., J.A.T., J.C.W., and P.S.K. were responsible for contributions to concept and design, acquisition analysis, and interpretation of data. All authors were responsible for drafting the article or revising it critically for important intellectual content and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adaikalam, S.A., Higano, N.S., Tkach, J.A. et al. Neonatal lung growth in congenital diaphragmatic hernia: evaluation of lung density and mass by pulmonary MRI. Pediatr Res 86, 635–640 (2019). https://doi.org/10.1038/s41390-019-0480-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0480-y