Abstract
Background
Both preterm birth and sleep disordered breathing (SDB) affect sleep in children. We compared the effects of SDB on sleep macro-architecture and micro-architecture in children born preterm (N = 50) and children born at term (N = 50). We hypothesized that sleep would be more disrupted in children born preterm.
Methods
Polysomnographic studies matched for age (3–12 years) and SDB severity were analyzed. Sleep macro-architecture was assessed using standard criteria and micro-architecture was evaluated using spectral analysis of the electroencephalogram and slow wave activity (SWA) calculated for each sleep stage across the night.
Results
Ex-preterm children (gestational age 29.3 ± 3.6 weeks, mean ± standard error of the mean) were not different from controls for demographic or respiratory parameters or sleep macro-architecture. Theta power in N2 tended to be higher for F4 (p < 0.05) and C4 (p < 0.07). In the second non-rapid eye movement period, SWA was significantly higher in the preterm group compared to the term group for both F4 and C4 (p < 0.05 for both).
Conclusions
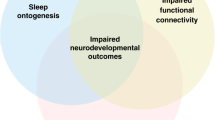
Sleep micro-architecture in children born preterm showed increased theta power and SWA. These differences provide evidence of increased sleep debt and reduced dissipation of sleep debt across the night. Further studies are required to identify if these findings are related to impaired neurocognition and behavior.
Similar content being viewed by others
Introduction
Preterm birth (<37 weeks of gestation) affects about 10% of births, and globally around 15 million babies are born preterm each year.1 Previously, we have shown that prematurity is associated with altered micro- and macro-sleep architecture changes indicative of reduced sleep quantity and quality in childhood.2 In that study, children aged 5–12 years were studied with overnight polysomnography (PSG) and the children born preterm had less total sleep time (TST) (by 64 min) and less non-rapid eye movement (NREM) sleep, more wake after sleep onset (WASO), and lower sleep efficiency, all indicating reduced and more fragmented sleep patterns compared to those children born at term. Consistent with these macro-architecture findings, sleep micro-architecture assessed by spectral analysis of the electroencephalogram (EEG) showed reduced delta and sigma EEG power, indicating less deep sleep (N3) and fewer sleep spindles.2 Reduced delta power and sleep spindles occur during recovery sleep following sleep deprivation and the authors suggested that this may reflect compensatory sleep recovery to repay sleep debt. Spectral analysis of the EEG also allows quantification of slow wave activity (SWA) reflecting the dissipation of delta power across the night. SWA is a physiological marker of the homeostatic regulation or drive for sleep and cortical maturation.3 It has been suggested that alterations in SWA may be indicative of disruptions to the normal developmental process and may result from early brain insults that occur during critical periods of development as frequently occuring in infants born preterm.4
Children born preterm are at increased risk of obstructive sleep disordered breathing (SDB). SDB describes a spectrum of respiratory disorders ranging from primary snoring (PS), which is not associated with significant desaturation or sleep fragmentation to obstructive sleep apnea (OSA), which is characterized by repetitive hypoxia, hypercarbia, and/or sleep disruption.5 SDB affects 4–11% of children;6 however, population cohort studies show that SDB is three to six times more likely in children born preterm.7,8,9 This predisposition persists into adulthood, with twice as many adults who were born preterm having OSA compared to those born at term.10 It has been suggested that infants born prematurely are predisposed to upper airway obstruction and oxygen desaturation during sleep due to reduced upper airway muscle tone, a highly compliant chest wall and high nasal resistance.11 SDB in children born at term has been associated with adverse effects on both the cardiovascular system12 and daytime behavior and learning.13 It is thought that these adverse outcomes are mediated by the repetitive hypoxia and sleep disruption, which are associated with SDB.14 Studies using both conventional PSG measurements of sleep macro-architecture and spectral analysis of the EEG to assess sleep micro-architecture in children born at term have not identified major changes in those children with SDB.15 Preterm-born children are at increased risk of daytime behavioral and learning problems, but how SDB impacts on sleep in this group has not been assessed. Thus, the aim of this study was to compare sleep macro-architecture and micro-architecture in children with SDB born preterm with those born at term. We hypothesized that sleep would be more disrupted in those children born preterm.
Methods
Ethical approval for this project was obtained from the Monash University and Monash Health Human Research Ethics Committees. Written informed consent to use sleep and demographic data for research purposes was obtained from parents and verbal assent from children when they attended the sleep study.
Between 2011 and 2016, 75 children (25 F/50 M) aged 3–12 years who had been born preterm (<37 weeks gestational age), and 1402 age-matched children (589 F/813 M) who were born at term (38–42 weeks gestational age) underwent overnight PSG for assessment of SDB at the Melbourne Children’s Sleep Center. All children were otherwise healthy with no comorbidities, such as craniofacial syndromes, developmental disability, and genetic syndromes as assessed by the referring clinician, and were not taking any medications known to affect breathing or sleep. From this cohort, 50 children born preterm were randomly selected, and matched for month and year of study, age, gender, and SDB severity with 50 children born at term.
Prior to commencement of the PSG study, children were weighed and measured and body mass index (BMI) z-score was calculated. Parents completed a demographics questionnaire including gestation at birth. Socioeconomic status (SES) was derived from the Australian Bureau of Statistics Index of Relative Socioeconomic Advantage/Disadvantage (SEIFA) 2011 national census data based on postal code.16 The SEIFA score has a mean of 1000 with a standard deviation (s.d.) of 100 and is presented as a raw score, with a higher score being indicative of higher income, education, employment, occupation, and housing.
All children underwent standard overnight pediatric PSG, recorded using either a Compumedics Series E or Grael Sleep System (Compumedics, Melbourne, VIC, Australia). Briefly, EEG (Cz, F3-A2, F4-A1, C3-A2, C4-A1, O1-A2, O2-A1), right and left electrooculogram, submental electromyogram (EMG), left and right anterior tibialis muscle EMG, and electrocardiogram recordings were obtained. Peripheral oxygen saturation was recorded using a 2-s averaging time (Masimo Radical Oximeter; Masimo Corporation, Irvine, CA, USA). Transcutaneous carbon dioxide was recorded using TINA TCM4 (Radiometer, Copenhagen, Denmark). Abdominal and thoracic respiratory parameters were measured using inductance plethysmography (Pro-Tech zRIPTM Effort Sensor, Pro-Tech Services Inc., Mukilteo, WA, USA). Oronasal airflow (Sandman® BreathSensorTM, Child Airflow Thermistor, Tyco Healthcare, UK) and nasal pressure (Salter Style®, Salter Labs, Arvin, CA, USA) measurements were also obtained. All signals were sampled at 512 Hz.
Sleep macro-architecture
Following the PSG study, sleep and respiratory events were scored by trained pediatric polysomnographic technicians in 30 s epochs according to standard criteria. Sleep was divided into NREM stages NI, N2, and N3 and rapid eye movement (REM) sleep.17,18 All respiratory events were >2 breaths in duration. An obstructive apnea was defined as the cessation of airflow in association with ongoing respiratory effort; an obstructive hypopnea was defined as ≥30% decrease in nasal pressure signal amplitude, associated with work of breathing and an arousal or ≥3% decrease in oxygen saturation; a central apnea was defined as cessation of airflow without inspiratory effort lasting either ≥20 s (s) or at least the duration of two breaths associated with an arousal or ≥3% oxygen desaturation, and a central hypopnea as ≥30% decrease in nasal pressure signal amplitude with absent inspiratory effort throughout the entire duration of the event. A mixed apnea was defined if an event was associated with absent respiratory effort during one portion of the event and the presence of inspiratory effort in another portion, regardless of which portion came first.17,18 An obstructive apnea hypopnea index (OAHI) was defined as the total number of obstructive apneas, mixed apneas, and obstructive hypopneas per hour of total sleep time (TST) and was used to define SDB severity groups. Snoring during the PSG study was documented by the sleep technicians. PS was defined as an OAHI ≤1 event/h; mild OSA as an OAHI >1–≤5 events/h; and moderate/severe (MS) OSA as an OAHI >5 events/h. A central apnea hypopnea index was defined as the total number of central apneas and central hypopneas per hour of TST.
Standard measures of sleep quality were calculated for each participant and included the following parameters. The duration of each sleep stage (N1, N2, N3, REM) was expressed as a % of TST. Wake after sleep onset (WASO) was calculated as the percentage of time awake during the sleep period time (SPT), defined as the amount of time in minutes from sleep onset until lights on at the end of the study, including all periods of wake in between. TST was defined as SPT excluding all periods of wake. Other variables calculated included time in bed (TIB), sleep latency, REM latency, and sleep efficiency. TIB was defined as the time between lights off and lights on. Sleep latency was defined as the period from lights off to the first 3 consecutive epochs of N1 sleep or an epoch of any other stage. REM latency was defined as the period from sleep onset to the first epoch of REM sleep. Sleep efficiency was defined as the ratio of TST to TIB.
Sleep micro-architecture: spectral analysis
Micro-architecture was assessed using spectral analysis of the EEG signal19 performed in Labchart 7.2 (ADInstruments, Sydney, Australia). Raw EEG signals were recorded using a band-pass filter ranging from 0.3 to 100 Hz and a sampling frequency of 512 Hz. Spectral analysis was performed on both EEG channels (C4-M1 and F4-M1). To remove any low- or high-frequency artifact from the signal, the EEG signal was digitally filtered using a band-pass filter ranging from 0.5 to 30 Hz. Epochs containing significant artifact, defined as a 30 s epoch containing >10 s of movement artifact that interrupted the EEG signal, were excluded from analysis. In all studies the first epoch of the recording was deleted, as well as the last epoch if it did not run for the full 30 s. The following frequency bands were set as delta power (0.5–3.9 Hz), theta power (4–7.9 Hz), alpha power (8–11.9 Hz), sigma power (12–13.9 Hz), and beta power (14–30 Hz).15 Spectral analysis was run using a fast Fourier transform (FFT) size of 1024 over the entire PSG recording with a Hanning window, which allowed edge effects to be avoided.20 The FFT output provided a total power for 2-s blocks with a frequency resolution of 0.5 Hz. These 0.5 Hz frequency bins were subsequently summed within five frequency bands, producing a single power value for each band. In addition, total power for each 2-s block was determined (0.5–30 Hz), and the spectral edge frequency (SEF), below which 95% of the EEG spectral power resides. A mean value for each frequency was calculated for each 30 s epoch and then averaged per sleep stage within each child.
SWA is expressed as delta power (0.5–3.9 Hz) and is greatest at the beginning of the sleep period, gradually dissipating over the night. SWA was averaged across each NREM period as determined from sleep stage scored data. A NREM period was defined as the succession of N2 or N3 of >15 min duration that was terminated by either one 30 s epoch of REM or a period of wakefulness of at least 5 min duration. The first four NREM periods across the night were analyzed.
Statistical analysis
Statistical analysis was performed using SigmaPlot (SigmaPlot Version 13.0, Systat Software, San Jose, CA, USA). Data were first tested for normality and equal variance. Demographic and PSG data were compared between preterm-born and term-born groups using paired two-sample Student’s T tests when normally distributed and Wilcoxon’s matched-pairs signed-rank tests when not. EEG spectral parameters in each sleep stage between SDB severity groups and SWA in each of the NREM periods across the night were compared with two-way analysis of variance with Student–Newman–Keuls post-hoc testing when normally distributed and Friedman two-way analysis of variance if non-parametric. Pearson’s correlation analysis was used to test the relationship between gestational age at birth and sleep and in the preterm-born group. All data are presented as mean ± standard error of the mean (s.e.m.) for ease of comparison, and a p value ≤0.05 was considered statistically significant.
Results
One child in each group was excluded from analysis due to artifact in the EEG. Demographic data for the study cohort (N = 98) are presented in presented in Table 1. Preterm-born children were born between 23 and 35 weeks of gestation. There were no differences between the groups for gender, age, height, weight, BMI, BMI z-score, or SES at the time of the study. By design the preterm-born cohort was born at significantly younger gestational age (p < 0.001).
Sleep macro-architecture
Sleep macro-architecture and respiratory data are presented in Table 2. There were no differences between the two groups for any of the parameters recorded. There were no effects of gestational age at birth on sleep macro-architecture or respiratory parameters in the preterm-born group.
Sleep micro-architecture
Comparison between EEG power values for total power (0.5–30 Hz), SEF, delta power 0.5–3.9 Hz), theta power (4–7.9 Hz), alpha power (8–11.9 Hz), sigma power (12–13.9 Hz), and beta power (14–30 Hz) between children born preterm and those born at term for C4 are presented in Fig. 1 and F4 in Fig. 2 for N1, N2, N3, and REM sleep. There were no differences between groups for total power, SEF, delta, alpha, sigma, or beta power in any of the sleep stages. F4 theta power was significantly higher in N2 in the children born preterm (p < 0.05) and this just failed to reach statistical significance for C4 (p < 0.07).
F4-derived electroencephalogram (EEG) power spectral analysis for total power, spectral edge frequency power, delta power, theta power, alpha power, sigma power, and beta power, during N1, N2, N3, and REM sleep in preterm-born children (black bars) and term-born children (gray bars). Data are presented as mean ± s.e.m.
C4-derived electroencephalogram (EEG) power spectral analysis for total power, spectral edge frequency power, delta power, theta power, alpha power, sigma power, and beta power, during N1, N2, N3, and REM sleep in preterm-born children (black bars) and term-born children (gray bars). Data are presented as mean ± s.e.m. * p < 0.05
In the children born preterm, when spectral power was plotted against gestational age at birth, significant correlations were found for C4 total power in N2 (r2 = 0.093, p = 0.04), N3 (r2 = 0.089, p = 0.04), and REM (r2 = 0.101, p = 0.03), C4 delta power in N1 (r2 = 0.101, p = 0.03), N2 (r2 = 0.141, p = 0.009), N3 (r2 = 0.084, p = 0.05), and REM (r2 = 0.110, p = 0.03), C4 beta power in N2 (r2 = 0.092, p = 0.04), and C4 alpha power in N2 (r2 = 0.137, p = 0.011) and REM (r2 = 0.128, p = 0.014). No correlations were found for any of the F4 spectral indices.
SWA across the night
The time course of SWA across the night in preterm and term children is presented in Fig. 3 for C4 and F4. As expected, SWA dissipated over the night, being highest in the first NREM period (NREMP1) and lowest in the fourth NREM period (NREMP4). In term children, SWA in NREMP1 was higher than in NREMP2, NREMP3 and NREMP4 and NREMP2 SWA was higher than in NREMP3 and NREMP4 for both F4 and C4. In preterm children, NREMP1 was higher than in NREMP2, NREMP3, and NREMP4, with no differences between NREMP2 and NREMP3 and NREMP4. In NREMP2 SWA was significantly higher in the preterm group compared to the term group for both F4 and C4 (p < 0.05 for both).
Effects of SDB severity on sleep micro-architecture
Children were divided into SDB severity groups (PS, mild OSA, MS OSA) and data for EEG spectral parameters for C4 are presented in Table 3, and compared between SDB severity groups within and between the term and preterm groups. N2 SEF and beta power were higher in the preterm group with MS OSA (p < 0.05 for both) compared to the term group, N2 alpha power was lower in the preterm group with mild OSA (p < 0.05), N3 SEF and alpha power, and REM sigma power were lower in the preterm group with mild OSA (p < 0.05 for all). F4 N2 and N3 alpha power and F4 N3 SEF were also lower in the preterm group with Mild OSA (p < 0.05 for all, data not shown). When comparing spectral parameters within the preterm and term groups, there were no differences in any EEG spectral parameter in awake or N1 sleep. In N2 C4 SEF and beta power were higher in the MS OSA group compared to both the PS and mild OSA groups in children born preterm. There were no severity group differences in N2 in the term-born children. In N3 F4 SEF and alpha were lower in the preterm group in those children with mild OSA and within the preterm group those with PS had higher SEF than those with mild OSA and those with MS OSA had higher alpha than those children with mild OSA.
Discussion
Preterm birth is associated with a number of adverse consequences, including an increased risk of SDB. To the best of our knowledge, this was the first study to assess the impact of SDB on sleep macro- and micro-architecture in children born preterm compared to a matched group of children born at term. We found that although conventional clinical measures of sleep quantity and quality were not different between the groups, there were differences in sleep micro-architecture, assessed using spectral analysis techniques. We found that in the groups as a whole Theta power was higher in N2 sleep in the children born preterm. SWA was also higher in the preterm group in the second NREM period of the night, indicating that the dissipation of SWA was reduced in these children at the start of the night. When the children were divided into groups based on SDB severity, the preterm children exhibited differences between severity groups, particularly in N2 and N3 sleep, that were not evident in the term children.
Previous studies by our group in children with SDB born at term, using conventional polysomnographic measurements of sleep macro-architecture have not identified major changes in those children with SDB compared to non-snoring control children.15 These findings have been supported by a number of other studies.21,22,23,24,25,26 In contrast, other studies have identified small decreases in the percentage of N3 sleep in children with OSA compared to non-snoring control children27 and increased percentage of N1 sleep.27,28
There are fewer studies examining the effects of preterm birth on sleep macro-architecture in children. In the current study of preterm-born children with SDB, we did not find differences in sleep macro-architecture. In a previous polysomnographic study by our group in a smaller number of preterm-born children (N = 15) without SDB, we reported reduced total sleep time by 45–64 min with reduced NREM sleep compared to term-born children (N = 20).2 In children, similar to our study, the overall total amount of N2 sleep was not different in children with SDB, but the duration of individual N2 epochs were significantly reduced.22 After adenotonsillectomy, sleep stage durations were no longer different between controls and children with SDB. The authors suggested that the mean duration of individual epochs of N2, the stage that occupies ~50% of the night in children, could provide a more sensitive measure of the effects of SDB on sleep architecture than conventional measures, which typically record only the proportion of each sleep stage in relation to total sleep time.22 In contrast to the findings of our study and that of Chervin et al.,22 a study of children born very preterm aged 6–10 years found more night time awakenings and more N2 sleep with less SWS, indicating more disrupted sleep macro-architecture.4 Our findings of no difference in sleep macro-architecture suggest that sleep macro-architecture is similarly affected by SDB in both preterm-born and term-born children. The lack of any significant differences between the term-born and preterm-born children when comparing the duration of N2 and N3 and REM sleep suggests that these essential stages of sleep are strongly protected in children with SDB.
Our spectral analysis, which assessed micro-architecture, found that Theta activity in N2 was significantly higher in preterm children in F4 with a similar trend in C4. In adults, increased spectral power density in delta and theta has been found after sleep deprivation.29 Our findings that Theta power in N2 was increased in the preterm-born children suggests that the preterm-born children may have an increased sleep debt compared to the children born at term. This idea is supported by our finding that SWA was increased in N2 in the second NREM period of the night in the children born preterm. This suggests reduced dissipation of sleep debt. Previous studies in pre-school children born at term with SDB showed both increased accumulation and dissipation of SWA,30 with higher SWA in the first NREM period (reflecting accumulation of sleep debt) and higher levels still present in the fourth NREM period (reflecting impaired dissipation of sleep debt). When children were followed up 3 years after the initial study and re-grouped into resolved SDB, unresolved SDB and control groups, both the SDB groups had higher mean SWA in the first NREM period at baseline and the resolved group (who had the highest OAHI at baseline) showed an increase in SWA in the fourth NREM period at baseline.31 The mean difference in SWA in the first NREM period between the SDB groups and the control group decreased at the follow-up and the increase in the fourth NREM period was not apparent. The study showed that irrespective of whether SDB completely resolves or not, children whose quantitative sleepiness improved over time, as measured by SWA at the beginning of the night, have improved sustained attention and a reduction in externalizing behaviors. Thus, increased sleepiness may underpin the increased disruptive behaviors that are common in children with SDB.32 Previous studies linking sleep macro-architecture have shown increased N2 sleep and reduced slow wave sleep were associated with increased total and behavioral difficulties, hyperactivity-inattention, and peer problems in very preterm-born children.4 In term-born children with SDB, SWA dissipation was predictive of deficits in problem solving and sustained attention, regardless of SDB severity.33 Whether children born preterm with SDB exhibit increased behavioral problems compared to their term-born counterparts is yet to be elucidated.
When children were divided into SDB severity groups, we identified differences between preterm and term children in N2, N3, and REM sleep for SEF, beta, alpha, and sigma power, but could identify no consistent trend in these. Importantly, we did not identify any differences between groups in delta or theta power, supporting the idea that these essential stages of sleep are protected. Our finding that the preterm children exhibited differences between severity groups, particularly in N2 and N3 sleep, which were not evident in the term children, suggests that SDB severity has a greater effect on sleep micro-architecture in these children.
We acknowledge the limitations of our study. The study was retrospective and we did not have access to data on birth weight or neonatal history or behavior and neurocognition. All of the children were referred for assessment of SDB and we did not have access to a non-snoring control group of preterm children recruited from the community. We acknowledge that we did not adjust our significance levels to control for multiple statistical testing and future studies with an even larger sample size should do this in order to confirm our findings.
In conclusion, children born preterm with SDB exhibit similar sleep macro-architecture but showed evidence of increased sleep debt and reduced dissipation of sleep debt across the night. These findings suggest the children born preterm should be screened for SDB and more research needs to be done to confirm our findings and identify if they are related to the increased behavioral and emotional problems that are common in children born preterm.
References
World Health Organisation 2018. Preterm birth fact sheet. https://www.who.int/news-room/fact-sheets/detail/preterm-birth.
Yiallourou, S. R. et al. Being born too small and too early may alter sleep in childhood. Sleep https://doi.org/10.1093/sleep/zsx193 (2017).
Buchmann, A. et al. EEG sleep slow-wave activity as a mirror of cortical maturation. Cereb. Cortex 21, 607–615 (2011).
Perkinson-Gloor, N. et al. The role of sleep and the hypothalamic-pituitary-adrenal axis for behavioral and emotional problems in very preterm children during middle childhood. J. Psychiatr. Res. 60, 141–147 (2015).
Marcus, C. L. et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 130, 576–584 (2012).
Lumeng, J. C. & Chervin, R. D. Epidemiology of pediatric obstructive sleep apnea. Proc. Am. Thorac. Soc. 5, 242–252 (2008).
Rosen, C. L. et al. Prevalence and risk factors for sleep-disordered breathing in 8- to 11-year-old children: association with race and prematurity. J. Pediatr. 142, 383–389 (2003).
Emancipator, J. L. et al. Variation of cognition and achievement with sleep-disordered breathing in full-term and preterm children. Arch. Pediatr. Adolesc. Med. 160, 203–210 (2006).
Raynes-Greenow, C. H. et al. Sleep apnea in early childhood associated with preterm birth but not small for gestational age: a population-based record linkage study. Sleep 35, 1475–1480 (2012).
Paavonen, E. J. et al. Very low birth weight increases risk for sleep-disordered breathing in young adulthood: the helsinki study of very low birth weight adults. Pediatrics 120, 778–784 (2007).
Arens, R. & Marcus, C. L. Pathophysiology of upper airway obstruction: a developmental perspective. Sleep 27, 997–1019 (2004).
Nisbet, L. C., Yiallourou, S. R., Walter, L. M. & Horne, R. S. Blood pressure regulation, autonomic control and sleep disordered breathing in children. Sleep Med. Rev. 18, 179–189 (2014).
Biggs, S. N., Nixon, G. M. & Horne, R. S. The conundrum of primary snoring in children: hat are we missing in regards to cognitive and behavioural morbidity? Sleep Med. Rev. 18, 463–475 (2014).
Beebe, D. W. & Gozal, D. Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. J. Sleep Res. 11, 1–16 (2002).
Yang, J. S. et al. Determining sleep quality in children with sleep disordered breathing: EEG spectral analysis compared with conventional polysomnography. Sleep 33, 1165–1172 (2010).
Australian Bureau of Statistics. Socio-economic indexes for areas (siefa). Technical paper http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/22CEDA8038AF7A0DCA257B3B00116E34/$File/2033.0.55.001%20seifa%202011%20technical%20paper.pdf (2011).
Berry, R. B. et al. Rules for scoring respiratory events in sleep: update of the 2007 aasm manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the american academy of sleep medicine. J. Clin. Sleep Med. 8, 597–619 (2012).
American Thoracic Society. Standards and indications for cardiopulmonary sleep studies in children. Am. J. Respir. Crit. Care Med. 153, 866–878 (1996).
Kellaway, P. An Orderly Approach to Visual analysis: Characteristics of the Normal EEG of Adults and Children (Raven Press, New York, 1990).
Jenni, O. G. & Carskadon, M. A. Spectral analysis of the sleep electroencephalogram during adolescence. Sleep 27, 774–783 (2004).
Kennedy, J. D. et al. Reduced neurocognition in children who snore. Pediatr. Pulmonol. 37, 330–337 (2004).
Chervin, R. D., Fetterolf, J. L., Ruzicka, D. L., Thelen, B. J. & Burns, J. W. Sleep stage dynamics differ between children with and without obstructive sleep apnea. Sleep 32, 1325–1332 (2009).
Kheirandish-Gozal, L. et al. Reduced NREM sleep instability in children with sleep disordered breathing. Sleep 30, 450–457 (2007).
Goh, D. Y., Galster, P. & Marcus, C. L. Sleep architecture and respiratory disturbances in children with obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 162, 682–686 (2000).
Yamadera, W. et al. Sleep architectures of obstructive sleep apnea syndrome in the young child. Psychiatry Clin. Neurosci. 54, 330–331 (2000).
Walter, L. M. et al. Differential effects of sleep disordered breathing on polysomnographic characteristics in preschool and school aged children. Sleep Med. 13, 810–815 (2012).
Durdik, P. et al. Sleep architecture in children with common phenotype of obstructive sleep apnea. J. Clin. Sleep Med. 14, 9–14 (2018).
Zhu, Y. et al. Sleep architecture in school-aged children with primary snoring. Sleep Med. 15, 303–308 (2014).
Dijk, D. J., Brunner, D. P., Beersma, D. G. & Borbely, A. A. Electroencephalogram power density and slow wave sleep as a function of prior waking and circadian phase. Sleep 13, 430–440 (1990).
Biggs, S. N. et al. Time course of EEG slow-wave activity in pre-school children with sleep disordered breathing: a possible mechanism for daytime deficits? Sleep Med. 13, 999–1005 (2012).
Weichard, A. J. et al. Association between slow-wave activity, cognition and behaviour in children with sleep-disordered breathing. Sleep Med. 25, 49–55 (2016).
Bourke, R. S. et al. Neurobehavioral function is impaired in children with all severities of sleep disordered breathing. Sleep Med. 12, 222–229 (2011).
Christiansz, J. A. et al. Slow wave activity and executive dysfunction in children with sleep disordered breathing. Sleep Breath. 22, 517–525 (2018).
Acknowledgements
We wish to thank all the children and their parents who participated in this study and the staff of the Melbourne Children’s Sleep Center. Support for this project was provided by the Victorian Government’s Operational Infrastructure Support Program.
Author information
Authors and Affiliations
Contributions
R.S.C.H. conceived and designed the study, was involved in interpretation of the data, drafting the article and revising it for final approval by all authors of the version to be published. M.C. and T.C.H.W. were involved in acquisition and analysis of the data, revising the manuscript and final approval of the version to be published. A.W. and L.M.W. were involved in analysis and interpretation of the data and final approval of the version to be published. G.M.N. provided critically important intellectual content, revising the manuscript and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chan, M., Wong, T.C.H., Weichard, A. et al. Sleep macro-architecture and micro-architecture in children born preterm with sleep disordered breathing. Pediatr Res 87, 703–710 (2020). https://doi.org/10.1038/s41390-019-0453-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0453-1
This article is cited by
-
The Relationship Between Sleep, Epilepsy, and Development: a Review
Current Neurology and Neuroscience Reports (2023)