Abstract
Background
We aimed to compare the accuracy of the ponderal index (PI) vs. BMI-for-age z-scores transformed (BMIz) in estimating body fat levels and classifying obesity in children and adolescents from a Brazilian urban population.
Methods
This is a cross-sectional study with 1149 participants (53.2% male), aged 6 to 18 years. Body fat percent (BFP) was obtained by multi-frequency bioelectrical impedance. Non-linear regression analysis provided the accuracy of both BMIz and PI in estimating BFP. False positive rate was obtained from the proportion of individuals placed at or above the 95th percentile for BMIz or PI, whereas their BFP was discordantly below the 95th percentile.
Results
PI and BMIz appeared with similar stability from childhood to adolescence for both boys and girls. The portion of the variability in BFP explained by BMIz (R2 = 0.74 and R2 = 0.75) was close to the variability in BFP explained by PI (R2 = 0.73 and R2 = 0.75) for boys and girls, respectively. False positive rate was higher for BMIz compared with PI among boys (21.8% vs. 3.9%) and girls (28.5% vs. 17.5%).
Conclusions
PI is a promising index for replacing BMIz in children and adolescents due to its potential to reduce false diagnosis of obesity.
Similar content being viewed by others
Introduction
Obesity has become a global problem because of its elevated prevalence not only in adults but also in children and adolescents1,2,3,4,5,6,7,8. In 2016, 41 million of young children up to 5 years of age were afflicted with overweight or obesity worldwide, the vast majority living in developing countries9. The global age-standardized prevalence of obesity increased from 0.7% (0.4–1.2%) in 1975 to 5.6% (4.8–6.5%) in 2016 in girls, and from 0.9% (0.5–1.3%) in 1975 to 7.8% (6.7–9.1%) in 2016 in boys7. Obesity in childhood has been associated with an increased risk of early onset of chronic diseases (type 2 diabetes, hypertension) and mortality in adult life10,11,12,13. Estimates indicate that the current prevalence of adolescents with overweight could lead to a 5%–16% increase in the incidence of coronary heart disease by 203514.
To implement strategies for prevention and treatment of children and adolescents with excessive body weight, it is necessary to have effective and low-cost tools capable of correctly diagnosing obesity in this specific population. The body mass index (BMI), calculated as the ratio between weight and squared height (kg/m2) has been extensively used to indicate the presence of overweight and obesity in adults by using the cut-off points determined by the World Health Organization (WHO)8. These cut-offs are only valid for adults because in adulthood height is constant. Therefore, an increase in BMI generally indicates an increase in body fat. In children and adolescents, however, height progressively increases until the beginning of adulthood. To address this issue, the WHO developed child growth standards by which age- and sex-specific BMI percentiles for individuals from 2 to 19 years were obtained15. Indeed, BMI-for-age z-scores transformed (BMIz) has become the standard method to indicate the presence of overweight or obesity in this age group, because z-scores indicate the number of standard deviations above or below the mean for a reference group. Nevertheless, though the z-score correction is reasonable, as it provides sex and age adjustments, BMI may not be very accurate, as it has been shown that weight scales to height in a varied way, from an exponent close to 2.0 up to 3.5 depending on the stage of physical growth from birth to puberty16. Besides, using BMIz has been called into question for children with more severe obesity (>97th percentile)17.
The ponderal index (PI) has been used in pediatric clinical settings at least since the 1960s. For example, Miller and Hassanein18 addressed the abnormal patterns of fetal growth by establishing distribution curves of PI in newborn infants according to their fetal ages. Recently, Peterson et al.19 studying 2285 non-Hispanic white individuals aged 8 to 29 years, have shown that overweight and obesity can be diagnosed without using complicated percentile tables by using the PI, calculated as weight divided by height cubed. In addition, the same investigators have shown that PI diagnoses overweight in adolescents more accurately than BMIz. To our knowledge, Peterson’s study was the first and only comparing the accuracy of PI with BMIz in estimating body fat levels in adolescents and young adults. Taking into account the lack of studies and the relevance of the theme, it is important to carry out additional studies to validate this new index for different populations.
Based on the possible applicability of PI as a useful tool to provide screening for childhood obesity in a clinical setting, the aim of this study was to compare the accuracy of PI vs. BMIz in estimating body fat levels and classifying obesity in children and adolescents from a Brazilian urban population.
Methods
Study design and sample selection
This is a cross-sectional study with data taken from databases containing two samples of children and adolescents (data from 2014 to 2016) totaling 1149 individuals (53.3% boys), 291 (25.3%) black, 201 (17.5%) white, and 657 (57.2%) “pardo”.
The first sample consisted of 856 individuals aged 6 to 18 years that were enrolled in a social project called “Estação Conhecimento”, that is a partnership between a mining company (Fundação VALE) and the community. The project is directed toward schoolchildren living in the neighborhood of the project, settled in the municipality of Serra, in the State of Espírito Santo, Brazil. In general, this region is occupied by low income families. All participants were regularly enrolled in municipal public schools and participated in the project part-time on weekdays to receive additional classes (beyond those regular classes at school) and to have the opportunity to participate in sports and cultural activities.
The second sample consisted of 293 children and adolescents aged 8 to 15 years enrolled in public schools in the municipality of Vitória, State of Espírito Santo, Brazil. Most of the schoolchildren enrolled in public schools in this municipality also belong to the lowest socioeconomic class. These municipalities are neighbors and both belong to the metropolitan region of Vitória.
All schoolchildren attended the Cardiovascular Investigation Clinic located at the University Hospital of the Federal University of Espírito Santo. Data were obtained by questionnaires and exams carried out in the morning period after 10–12 h of fasting. All data were collected during a single visit by trained investigators previously certified by a senior investigator. Children with missing data on any of the variables of interest were excluded from the final analysis. Both projects were approved by the Center for Health Sciences Ethics Committee (opinion numbers: 30385014.8.0000.5060 and 1.565.490, respectively) and written and informed consent was obtained from the parents or legal guardians before enrollment.
Anthropometry
Anthropometric parameters were measured according to a standard protocol20. Weight was measured using an electronic scale (Toledo 2099, Brazil) with 0.05 kg precision in barefoot individuals using only undergarments after bladder emptying. Height was obtained in a wall-mounted stadiometer (Seca Stadiometer—Seca GmBH & Co, Hamburg, Germany) with 0.1 cm precision. Body fat percentage (BFP) was measured by multi-frequency bioelectrical impedance analysis (MF-BIA8, InBody 230, Bioespace, South Korea). BFP obtained by multi-frequency bioelectrical impedance was highly correlated (r > 0.9) with that obtained by Dual-energy X-ray Absorptiometry (DEXA) in children and adolescents aged 7 to 18 years21. BMI was calculated as the ratio between weight and height squared (kg/m2). BMIz-scores (BMIz) was obtained with the aid of free software WHO Anthroplus in accordance with Word Health Organization Growth Child Standards15. PI was calculated by dividing weight by height cubed (kg/m3). BMIz and PI were simultaneously inserted into the database.
Statistical analysis
The general characteristics of the sample are expressed as mean ± standard deviation for continuous variables, or percentage and 95% confidence interval (95% CI) for proportions. Normality of all data was tested with the Kolmogorov–Smirnov test. Comparisons between sexes for the variables following a normal distribution were performed with the unpaired Student’s t-test. As neither PI nor BMIz presented a normal distribution, the comparison between sexes for these variables was provided by Mann–Whitney U test.
For both sexes, age was categorized into eleven groups and two procedures were performed. First, the coefficients of variation of each age category for both PI and BMIz were calculated, and second, a one-way ANOVA was used to compare the mean values between the age categories for both PI and BMIz. This last procedure was performed to test the stability of both PI and BMIz with age.
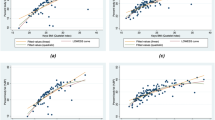
Linear and non-linear regression analyses were performed to define the function of best fit for the data points on the scatter plots showing the association between BMIz and BFP, as well as PI and BFP. For the non-linear regression, a second-order polynomial function was fitted to data points and then expressed by a quadratic equation. The highest R2 value was taken into account to choose the most appropriate model (linear or non-linear) in the regression of BFP on both PI and BMIz.
To determine the false positive rates, each individual’s BFP, PI, and BMIz were translated into a percentile ranking and then dichotomized into lean versus obese using the 95th percentile. Although using the 95th percentile as a cut-off value for obesity is somewhat arbitrary, it has been previously shown that this cut-off provided a close approximation to the obesity boundary of the International Obesity Task Force, which encompasses children and adolescents from six countries including Brazil and the United States of America22,23. False positive rate was obtained from the proportion of individuals placed at ≥P95th according to PI or BMIz while their BFP was at <P95th. Fisher’s exact test was used to compare the proportions of false positive rates and false negative rates between PI and BMIz.
All statistical procedures were carried out with the SPSS 21.0 statistical package (SPSS Inc., Chicago, Illinois) and GraphPad Prism 6.01 (GraphPad Software, Inc., CA). Two-sided statistical significance was set at P < 0.05.
Results
The main physical characteristics of the sample are described in Table 1. The age and body weight were similar between boys and girls. However, as expected, boys were taller than girls (P = 0.012). Even using a nonparametric statistic, BMIz was not different between boys and girls (P = 0.352), whereas PI was greater in girls than in boys (P < 0.001), thus justifying the need for splitting further analyses by sex.
Eleven age groups were established and the mean values obtained for PI and BMIz were compared among all age groups in order to provide a measurement of stability. In Table 2 the age categories are specified along with the number of individuals by category. The coefficient of variation associated with the mean values of PI and BMIz are also presented.
In a visual inspection, PI seems more stable from childhood to adolescence than BMIz, in both boys and girls (Fig. 1a, b). The values of PI were not significantly different across the age categories in both girls (P = 0.390) and boys (P = 0.124). Similarly, the values of BMIz were not different across the age categories in both girls (P = 0.126) and boys (P = 0.096)
Non-linear regressions of BFP on BMIz and PI are exhibited in the scatter plots of Fig. 2. A curvilinear relationship between BFP and BMIz can be clearly observed for boys (Fig. 2a). As seen by the R2 value obtained from the non-linear regression, BMIz explained 74% of the total variability of BFP (P < 0.001). Similarly, for girls, BMIz explained 75% (P < 0.001) of the total variability of BFP (Fig. 2b). The R2 values obtained from the regression of BFP on PI were very similar to those observed in the regression of BFP on BMIz, for both boys (0.73, P < 0.001) and girls (0.75, P < 0.001), respectively (Fig. 2c, d).
An individual was considered to be a false positive if she or he had a BMIz or PI at or above the 95th percentile but a BFP that was discordantly below the 95th percentile. Figure 3a shows that the false positive rate obtained in boys was higher for BMIz (21.8%; 95% CI, 18.9%–23.4%, P < 0.001) compared with PI (3.9%; 95% CI, 2.5%–6.2%), (P < 0.001). Similarly, the false positive rate obtained in girls (Fig. 3b) was also significantly higher for BMIz (28.5%; 95% CI, 27.5%–30.2%) compared with PI (17.5%; 95% CI, 14.9%–23.8%), (P = 0.032).
Comparison of false positive rates of obesity between BMIz and PI in boys (a) and girls (b). Comparison of false negative rates of obesity between BMIz and PI in boys (c) and girls (d). Misclassification rates between BMIz and PI in boys (e) and girls (f). *Statistically significant difference (P < 0.05)
An individual was considered to be a false negative if she or he had a BMIz or PI below the 95th percentile but a BFP that was discordantly at or above the 95th percentile. Figure 3c shows that the false negative rate obtained in boys was higher for PI (9.9%; 95% CI, 7.4%–12.3%) compared with BMIz (4.4%; 95% CI, 2.6%–6.1%), (P < 0.001). In line with these results, Fig. 3d shows that the false negative rate observed in girls was also higher for PI (10.8%; 95% CI, 8.1%–13.5%) than for BMIz (5.2%; 95% CI, 3.2%–7.2%), (P < 0.001). The total rate of classification was not different between BMIz and PI for both boys (6.4%; 95% CI, 4.4%–8.4% vs. 9.4%; 95% CI, 7.1%–11.7%, P = 0.257) and girls (8.3%; 95% CI, 6.0%–10.6% vs. 11.1%; 95% CI, 8.4%–13.7%, P = 0.097).
Discussion
The main findings of this study showed that PI, like BMIz, was quite stable along the age range covering the final period of childhood and throughout adolescence. In addition, PI was as accurate as BMIz as a proxy of BFP. Nevertheless, PI was superior to BMIz in avoiding misdiagnoses of obesity and equally good as classifying weight status in Brazilian children and adolescents with obesity, so classified in accordance with BFP.
Peterson et al.19 conducted a study using data from NHANES 1999–2006 comparing BMI and PI regarding their stability at different ages, accuracy in estimating body fat, and accuracy in classifying overweight and obesity status in children and adolescents. Based on their data, the authors claimed that PI could be a substitute for BMIz due to its greater accuracy for the screening of overweight and obesity.
As well established, for children and adolescents (aged 2 to 19 years) instead of raw BMI, BMIz-scores according to sex- and age-specific BMI percentiles are necessary to take into account interindividual differences in pubertal development. When testing stability with age, Peterson et al.19 included in the study individuals from 8 to 29 years and compared the stability of PI and raw BMI within this age range. As previously reported, scaling of weight to height among children and adolescents is under significant influence from fatness, since boys and girls with obesity tend to be taller than their lean counterparts24,25, whereas this effect of fatness on size attainment is not necessarily observed among adults26. Moreover, a child’s BMI tends to be lower than that of an adult even if his body fat is much higher. Considering an actual example from our databases, an 8-year-old child with BMI of 21.6 kg/m2 was ranked at the 97th percentile of his corresponding BMI-for-age, and consequently directed to the group of individuals with obesity. The body fat measured in this child was nearly 35% of his total body weight. In contrast, a 29-year-old man with a similar BMI (21.5 kg/m2) was classified as normal weight and only 16% of his body weight was composed of fat. Thus, when we replaced raw BMI by BMIz, which is the standard for children and adolescents, we observed that BMIz and PI have a similar pattern of stability in children and adolescents from 6 to 18 years.
We also demonstrated that both BMIz and PI provided similar R2 values in the non-linear regression analysis both for boys and girls. In general, BFP explained more than 70% of the variability of both BMIz and PI. Indeed, our results are in line with that reported by Katzmarzyk et al.27 who presented the association between BMIz and BFP in children aged 9 to 11 years from 12 countries spread over the five continents, including from Brazil. Overall, the correlation between BMIz (standards by the CDC) and BFP ranged from 0.71–0.88 for boys and from 0.71–0.93 for girls, which transforming to R2 would provide a range from 0.50–0.77 for boys and 0.50–0.86 for girls. In Brazilian children, the R2 resultant from the regression of BFP on BMIz among boys (0.61) and girls (0.76) were both close to our results.
In line with our findings, when Peterson et al.19 restricted the sample to individuals aged 8 to 17 years, they reported that PI was better than BMIz for accurately classifying overweight and obesity status in children and adolescents. In this regard Burton et al.28, addressed the issue of why, in the calculation of BMI, weight scales to height with a power of 2.0 (expressing area), instead of scaling with a power of 3.0 (expressing volume), given that for objects with different size (i.e., length in humans) but identical shape (a single cylinder as in humans), the volume has to be proportional to the cube of length, and the ratio of mass/(length3) tends to be constant. Moreover, even if shape varies, the ratio mass/(length3) remains as a full index of shape and is independent of size. In this sense, it seems that BMI has been traditionally used because it is just a convenient approximation to the Benn index, which is calculated as mass/heightp, where p is selected to minimize the correlation with height29. As a matter of fact, it has been shown that p is nearly 2 in adults, while in children the height is highly correlated with fat mass (p = 5.8)30, suggesting that a different approach to the fat content should be provided for children.
Recently, some studies have tested the effectiveness of PI as a predictor of cardiometabolic risk31,32,33. However, it is worth mentioning that the present study was the second to show that PI is better for the screening of obesity. Thus, although both indexes seem to present similar validity as a proxy of BFP, PI clearly shows some advantages because it can be calculated with no concerns about adjustments for age, besides being more accurate than BMIz-scores in avoiding false positive diagnoses of obesity. These characteristics make PI easier to use in a clinical setting than the BMI z-scores.
The inconsistent finding on the false positive obesity in boys and girls may be due to an imbalance between body composition and the indices of adiposity according to sex, that is, in the extreme percentiles, neither PI nor BMIz translated into a proportionally higher percent body fat.
This study has some limitations. First, given the cross-sectional nature of the study, cause and effect relationship cannot be determined. Indeed, a prospective analysis would be beneficial in ensuring that variations over time were not resultant from interindividual variations. Second, a random sample of the population of children and adolescents was not tested. Therefore, there is a limitation in extrapolating the results for the general population of children and adolescents. Third, we did not perform an internal validation of multi-frequency bioelectrical impedance to establish its accuracy in assessing BFP in the studied population. However, validation of multi-frequency bioelectrical impedance with eight-point tactile electrodes versus DEXA has been provided for children and adolescents34. Besides, a possible measurement bias does not differently affect the capacity of PI and BMIz as estimators of body fat. Fourth, BMIz was obtained from the standards by the Centers for Disease Control and Prevention, while we cannot guarantee that Brazilian children and adolescents share physical similarities with American children and adolescents. Fifth, sample size was small for creating categories of sex and age groups without interfering with statistical power. Despite these limitations, our study supports the use of PI as a proxy of body fat in children and adolescents as being a useful tool for providing screening for obesity in the pediatric population.
In conclusion, PI is a promising index for replacing BMIz in providing screening for obesity in Brazilian children and adolescents, both in epidemiological studies and in the clinical routine, due to its potential to reduce false diagnosis of obesity.
References
Lobstein, T., Baur, L. & Uauy, R. IASO International Obesity Task Force. Obesity in children and young people: a crisis in public health. Obes. Rev. 5, 4–104 (2004).
Olshansky, S. J. et al. A potential decline in life expectancy in the United States in the 21st century. N. Engl. J. Med. 352, 1138–1145 (2005).
Wang, Y., Beydoun, M. A., Liang, L., Caballero, B. & Kumanyika, S. K. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. (Silver Spring) 16, 2323–2330 (2008).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781 (2014).
Lobstein, T. et al. Child and adolescent obesity: part of a bigger picture. Lancet 385, 2510–2520 (2015).
World Health Organization. Consideration of the evidence on childhood obesity for the Commission on Ending Childhood Obesity: report of the ad hoc working group on science and evidence for ending childhood obesity. (WHO, Geneva, 2016). (http://apps.who.int/iris/bitstream/10665/206549/1/9789241565332_eng.pdf?ua=1).
NCD Risk Factor Collaboration. Worldwide trends in body mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
World Health Organization. Obesity and overweight. (WHO, Geneva, Switzerland, 2018). (http://www.who.int/mediacentre/factsheets/fs311/en/).
World Health Organization. Report of the Commission on Ending Childhood Obesity: implementation plan: executive summary. (WHO, Geneva, 2017). http://www.who.int/iris/handle/10665/259349.
Wang, Y. C., McPherson, K., Marsh, T., Gortmaker, S. L. & Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 378, 815–825 (2011).
Reilly, J. J. & Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J. Obes. 35, 891–898 (2011).
Litwin, S. E. Childhood obesity and adulthood cardiovascular disease: quantifying the lifetime cumulative burden of cardiovascular risk factors. J. Am. Coll. Cardiol. 64, 1588–1590 (2014).
Twig, G. et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 374, 2430–2440 (2016).
Bibbins-Domingo, K., Coxson, P., Pletcher, M. J., Lightwood, J. & Goldman, L. Adolescent overweight and future adult coronary heart disease. N. Engl. J. Med. 357, 2371–2379 (2007).
World Health Organization. Multicentre Growth Reference Study Group. Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. (WHO, Geneva, 2006).
Medeiros da Silva Mazzeti, C., Cumpian Silva, J., Rinaldi, A. E. M. & Conde, W. L. The allometric scaling of body mass and height in children and adolescents in five countries. Am. J. Hum. Biol. 30, e23101 (2018).
Freedman, D. S. et al. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999-2000 to 2013-14. Obesity (Silver Spring) 25, 739–746 (2017).
Miller, H. C. & Hassanein, K. Diagnosis of impaired fetal growth in newborn infants. Pediatrics 48, 511–522 (1971).
Peterson, C. M. et al. Tri-ponderal mass index vs body mass index in estimating body fat during adolescence. JAMA Pediatr. 171, 629–636 (2017).
Lohman T., Roche A., Martorell E. Anthropometric standardization reference manual. (Human Kinetics, Champaign, 1988).
Lee, K., Lee, S., Kim, S. Y., Kim, S. J. & Kim, Y. J. Percent body fat cutoff values for classifying overweight and obesity recommended by the International Obesity Task Force (IOTF) in Korean children. Asia Pac. J. Clin. Nutr. 16, 649–655 (2007).
McCarthy, H. D., Cole, T. J., Fry, T., Jebb, S. A. & Prentice, A. M. Body fat reference curves for children. Int. J. Obes. 30, 598–602 (2006).
Cole, T. J., Bellizzi, M. C., Flegal, K. M. & Dietz, W. H. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320, 1240–1243 (2000).
Garn, S. M. & Haskell, J. A. Fat thickness and developmental status in childhood and adolescence. AMA J. Dis. Child 99, 746–751 (1960).
Garn, S. M., Clark, D. C. & Guire, K. E. Levels of fatness and size attainment. Am. J. Phys. Anthr. 40, 447–449 (1974).
Garn, S. M. Obesity in black and white mothers and daughters. Am. J. Public Health 84, 1727–1728 (1994).
Katzmarzyk, P. T. et al. Association between body mass index and body fat in 9-11-year-old children from countries spanning a range of human development. Int J. Obes. Suppl. 5, S43–S46 (2015).
Burton, R. F. Why is the body mass index calculated as mass/height2, not as mass/height3? Ann. Hum. Biol. 34, 656–663 (2007).
Benn, R. T. Some mathematical properties of weight-for-height indices used as measures of adiposity. Brit J. Prev. Soc. Med 25, 42–50 (1971).
Wells, J. C. K. & Cole, T. J. and ALSPAC study team. Adjustment of fat-free mass and fat mass for height in children aged 8 y. Int. J. Obes. 26, 947–952 (2002).
Jiang, Y. et al. Waist-to-height ratio remains an accurate and practical way of identifying cardiometabolic risks in children and adolescents. Acta Paediatr. 107, 1629–1634 (2018).
Ramírez-Vélez, R. et al. Tri-ponderal mass index vs. fat mass/height3 as a screening tool for metabolic syndrome prediction in Colombian children and young people. Nutrients 10, 412 (2018).
Margolis-Gil, M., Yackobovitz-Gavan, M., Phillip, M. & Shalitin, S. Which predictors differentiate between obese children and adolescents with cardiometabolic complications and those with metabolically healthy obesity? Pedia. Diabetes 19, 1147–1155 (2018).
Lim, J. S. et al. Cross-calibration of multi-frequency bioelectrical impedance analysis with eight-point tactile electrodes and dual-energy X-ray absorptiometry for assessment of body composition in healthy children aged 6–18 years. Pedia. Int. 51, 263–268 (2009).
Acknowledgements
The authors wish to thank the unwavering support of “Estação Conhecimento” and VALE Foundation, Vitória, ES, Brazil, during the period of data collection. This work was supported by the Pro-Rectory of Research and Post-Graduate Studies of the Federal University of Espírito Santo (Institutional Program Fund for Research Support, 2015); Foundation for Supporting Research and Innovation of Espírito Santo (FAPES)—Research Program for SUS (PPSUS) (grant 65854420/2014); Fundação VALE; and Laboratory Thommasi of Vitória, ES, Brazil, that funded the accomplishment of part of the biochemical exams. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication
Author information
Authors and Affiliations
Contributions
D.Z., P.R.O., and F.S.N. analyzed the data, interpreted the results, and drafted the manuscript. R.d.O.A. participated in the design of the work and contributed to the analysis of data and interpretation of results. V.O.P., C.R.M., and M.A.S.P. contributed to acquisition of data. M.C.R.B. and E.R.d.F. participated in the design of the work and supervised the acquisition of data. J.G.M. conceptualized and designed the study, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zaniqueli, D., Oliosa, P.R., Neves, F.S. et al. Ponderal index classifies obesity in children and adolescents more accurately than body mass index z-scores. Pediatr Res 86, 128–133 (2019). https://doi.org/10.1038/s41390-019-0395-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0395-7
This article is cited by
-
Predictors of central and general obesity in Iranian preschool children: which anthropometric indices can be used as screening tools?
BMC Pediatrics (2022)
-
Health indices for the evaluation and monitoring of health in children and adolescents in prevention and health promotion: a scoping review
BMC Public Health (2021)
-
Uric acid reference values: report on 1750 healthy Brazilian children and adolescents
Pediatric Research (2021)