Abstract
Background
Immunothrombosis is a physiological process based on the release of neutrophil extracellular traps (NETs) to immobilise, contain and kill bacteria. This is an innate immune response in which the local activation of blood coagulation exerts the critical protective function during microbial infection. In recent years, there has been much interest in the adult literature about the key role of immunothrombosis in pathologic states including thrombosis, cancer, sepsis and trauma. Currently, little research has been done into its role in paediatric conditions.
Methods
We conducted a literature search of the National Library of Medicine (MEDLINE/PubMed) from the years 2000 to May 2018 and qualitatively identified 24 relevant papers. References of articles included for full-text review were checked for relevant publications.
Results
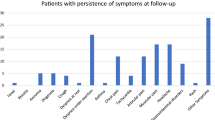
Our aim is to summarise the most relevant evidences regarding an excessive production or defective removal of NETs in paediatric conditions. In particular, we have divided the role of immunothrombosis into acute (sepsis, necrotising enterocolitis, otitis media, neonatal arterial ischaemic stroke, haemolytic anaemic diseases) and chronic (systemic lupus erythematous, type 1 diabetes mellitus, respiratory diseases, graft-versus-host disease) conditions to find important similarities in their pathophysiology.
Conclusion
The field of immunothrombosis in paediatric conditions is still in its infancy. We have presented multiple pathways of NET-induced disease together with possible areas of future research and treatments.
Similar content being viewed by others
Introduction
Immunothrombosis, a term first coined in 2013, describes the crosstalk between the activation of neutrophils and their interaction with platelets in the coagulation system. This mechanism is a response of the innate immune system to pathogens, used to fight acute illness but which, under certain circumstances, can lead to adverse acute effects (e.g. thrombosis) or chronic illness (e.g. autoimmune diseases).1,2,3
The presence of bacterial products in the blood stream activates the neutrophils to release neutrophil extracellular traps (NETs), which comprised DNA, histones, granule enzymes released from neutrophils and bactericidal molecules. Since their discovery, a lot of research has been done both in vitro and in vivo to understand the role of NETs in disease processes.4 The vast majority of this knowledge however is based on evidence in adults, where NETs are known to be implicated in sepsis, acute lung injury, autoimmune diseases, cancer and multiple sclerosis amongst others.5,6,7,8 It has been proposed that the phenomenon may operate via multiple pathways, after variable mechanistic concordance has been noted in past research.9,10 Based on limited evidence in children, we know that some conditions, such as sepsis and autoimmune diseases, can have similar pathophysiological pathways as in adults but this is often not well known among paediatric practitioners.
This expert review aims to discuss the current literature on NETosis in children with the focus on finding scope for future research and treatment.
Methods
We conducted a systematic literature search of the National Library of Medicine (MEDLINE/PubMed) from the years 2000 to May 2018 with variable combinations of the following terms: ‘immunothrombosis’, ‘NETosis’, ‘neutrophil extracellular traps’, ‘paediatric’, ‘children’, ‘neonates’, ‘paediatric conditions’, ‘sepsis’ and ‘thrombosis’. A total of 272 papers were identified. Duplicates and non-English papers were excluded and the remaining screened. Twenty-four papers were then qualitatively selected based on relevance to the topic by two authors (TF and SG). References of articles included for full-text review were checked for relevant publications.
Results
The pathogenesis of immunothrombosis has been attributed to the presence of NETs and their release via NETosis.11 The components of a NET consist primarily of a chromatin backbone with citrullinated histones, often loaded with a specific protein cargo dependent on the inflammatory environment (Table 1).7,10,12,13
NETosis occurs when neutrophils are activated by certain stimuli, such as lipopolysaccharide or autoantibodies, which sets off a sequence of events that lead to increased reactive oxygen species production, allowing for the release of the NETs (Fig. 1).14,15,16
NETosis and immunothrombosis. Multiple stimuli can induce NETosis including: pathogens, lipopolysaccharide (LPS), autoantibodies, immune complexes, tumour necrosis factors (TNF), interleukins (IL-8), interferons (type I and II INFs) and activated platelets. Binding of these stimuli to neutrophils can occur via toll-like receptors (TLR-4), Fc receptors (FcR), P-selectin glycoprotein ligand-1 receptors (PSGL-1) and complement receptors, amongst others. Once bound, there is induction of endoplasmic reticulum calcium (Ca2+) store release and membrane channel opening, causing an increase in cytoplasmic Ca2+ levels. This increase in Ca2+ initiates a sequence of events leading to the release of NETs. An increase in protein kinase C (PKC) activity causes phosphorylation of Gp91phox and NADPH oxidase assembly. This triggers an increase in the production of reactive oxygen species (ROS) and nitric oxide (NO), which breakdown the nuclear and granule membranes, allowing for mixing of the nuclear, granular and cytoplasmic substances. In this process, histones are citrullinated and cleaved prior to chromatin decondensation. Plasma membrane rupture allows for NETosis to complete, expelling NETs formed mainly of DNA, histones and NET-associated proteins (neutrophil elastase (NE), myeloperoxidase (MPO) and cathepsin G (CG)). NE assists thrombus formation by inhibiting anticoagulants, antithrombin (AT) and activated protein C (APC), and tissue factor pathway inhibitor (TFPI). Other elements of NETs induce the coagulation cascade; DNA is involved in the intrinsic pathway whilst tissue factor (TF) has a role in the extrinsic pathway and citrullinated histones are also known to promote thrombin generation. NETs also promote a hyper-coagulability status through platelet activation via histone H3 and H4. All of the above combine together to form a thrombus via immunothrombosis
This overview model of NETosis and immunothrombosis also provides a platform to view the relationship between neutrophils and infection, and applies to any conditions where pathogens are present. Neutrophils are activated by pathogens and accumulate near the endothelium, bound with platelets, where they release both NETs and tissue factor. The pathogens become trapped in the NETs and a coagulation cascade is initiated, leading to microcirculatory and potential organ damage.10,15
Below we present categorised information on paediatric NET-associated conditions, focusing on the method of action of NETs in their pathophysiology. We have tried to group acute and chronic conditions affected by immunothrombosis to see if the mechanisms of action were comparable or whether NET disfunction varied between the two groups.
Acute conditions
Sepsis
Sepsis remains one of the leading causes of death in children and is defined as a systemic inflammatory response syndrome resulting from a proven infection.17 NETosis is part of the innate immune response to microbe infections and it is highly activated in sepsis.18 NETs promote a hyper-coagulability status, through platelet activation via histone H3 and H4, causing a significant thrombotic reaction and inhibition of fibrinolytic activity. The cellular events during sepsis that trigger venous thromboembolism in response to systemic inflammation remain unknown. High levels of NETs has been correlated with organ injury via both the formation of thrombi in the endothelium and the direct attack though histone and myeloperoxidase-dependent mechanisms.19 In particular, cell-free DNA (cfDNA) has shown to modulate coagulation and fibrinolysis.20 cfDNA is considered a natural foreign surface and activates the coagulation system via the contact pathway (factors XII and XI). Disseminated intravascular coagulopathy (DIC) is a direct consequence of upregulated immunothrombosis due to higher level of NETs compared to septic patient without DIC.21 Neonates are more vulnerable to DIC as their haemostatic system is balanced and dynamic but not as stable as the adult one.
Other studies have also documented histones affecting toll-like receptors 2 and 4 (TLR-2 and 4) stimulating the production of pro-inflammatory cytokines via myeloid differentiation primary response 88 (MyD88) signalling, adding to the innate immune cell load in the area.18 Neutrophils that release NETs have also been described as potential sepsis biomarkers in neonates via two expressed factors; CD64 and soluble triggering receptor expressed on myeloid cells-1 (sTREM-1). CD64 is a high-affinity immunoglobulin Fcγ-1 receptor that mediates the phagocytosis of bacteria.22 Usually its levels are low, but can increase 10-fold in sepsis. sTREM-1 is an immunoglobulin expressed after exposure to LPS which attenuates inflammation.23 The link between inflammation, immunity and thrombosis in adult sepsis is an extremely active field of research where numerous lessons can be learnt and applied to paediatric sepsis. An interesting avenue of novel research in children with sepsis could be the development of drugs to modulate NET formation and activation of coagulation and fibrinolysis without increasing the risk of bleeding.
Necrotising enterocolitis
Necrotising enterocolitis (NEC) is a destructive gastrointestinal disease which affects premature neonates that can lead to intestinal necrosis, perforation and peritonitis. Alongside the key risk factor of prematurity, altered intestinal blood flow, bacterial colonisation, and enteral feeding are also all closely associated with NEC.24
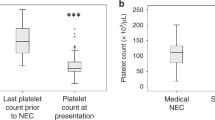
Despite decades of research, the pathophysiology of NEC remains unclear.24 It has been reported that levels of calprotectin, an anti-bacterial protein,25 are elevated in the stools of NEC affected neonates as compared to healthy controls (288.4 mg/L [SD 49.1]/98.0 mg/L [60.6], p < 0.001).26 Moreover, calprotectin accounts for ~60% of neutrophil cytosolic protein, and about 50–60% of this becomes incorporated into NETs during their formation.27 Immunohistochemical analysis of bowel samples taken from neonates surgically treated for NEC demonstrated activated neutrophils in NETs and NET-associated calprotectin as opposed to control patients who showed no NET formation or increase in calprotectin expression.28 It appears therefore that NETosis may participate in the pathophysiology of NEC, with calprotectin acting as a potential marker to distinguish NEC from feeding intolerance. Moreover, research into coagulation gene expression in infant NEC patients found that 12 genes were altered as compared to controls. Neutrophil elastase (NE), amongst others, was significantly upregulated (mean fold-change +2.74, p = 0.05) and there was an overall procoagulant effect elicited.29 NE is a serine protease responsible for local activation of immunothrombosis and of the coagulation cascade. Further, a recent paper showed that hyper-inflammation in a mouse model of NEC was dependent on NETosis and NEC severity was significantly reduced in mice incapable of forming NETs. Data on human histology also showed that immunothrombosis is present in NEC and this can lead to interesting research developments.30 Elevated circulating cfDNA levels in neonatal plasma have been associated at late-onset sepsis diagnosis and few days before NEC.31
It is therefore clear that insights into NEC would prove useful for several reasons: (i) it may help develop a treatment for a disease which is still linked to a very high mortality rate;32 (ii) it may represent a model to further investigate severe immunothrombosis in neonates as most of the interactions between inflammation, immunity and coagulation occur in the gut; (iii) since severe thrombosis of the mesentery is a common finding in NEC, further investigation may determine whether treatment against NETosis can selectively reduce thrombus formation and maintain blood supply to the gut.
Otitis media
Otitis media (OM) is an extremely common paediatric disease, affecting up to 80% of children worldwide before the age of 3 years.33 It is characterised by ear pain and effusions, and can lead to permanent hearing loss in some cases.34 The role of NETs in both recurrent acute OM and chronic OM is starting to be understood.35
It is known that the host inflammatory response is in part accountable for the middle ear bacterial outgrowth seen in Streptococcus pneumoniae OM, with NETs being the mediator responsible.36 Indeed, NET levels have been positively correlated with higher bacterial loads.37 Recently it has been shown that NET formation in the middle ear is IgA antibody-dependent and they provide an environment for bacterial replication, rather than destruction.34,38 Nontypeable Haemophilus influenzae (NTHi) has also been documented to cause OM, with NETs forming a biofilm, protecting the pathogen.39 Research describes how NTHi activates the epithelial cells, leading to IL-8 and leukotriene B4 production, recruiting neutrophils and subsequently triggering NETosis and the formation of a viscous biofilm, able to withstand immune clearance.36,38,39 There is however already some data that suggests transtympanic administration of the DNase Dornase Alfa leads to NETs ‘melting’, thus weakening the biofilm scaffolding and allowing for it to be cleared by the immune system.34,36 Further research into this mechanism of NET dismantling could lead to the widespread use of DNase to swiftly treat OM, and could potentially lead to mechanistically similar break down of NETs in other conditions where excessive NETosis forms part of the pathophysiology. It is important to note however, that there is some evidence indicating that the use of DNase to dismantle NETs may lead to worsening inflammatory tissue damage, as there is a prolonged reduction in NET-mediated antibacterial functioning.40 This could potentially aggravate the infection and lead to systemic inflammatory response syndrome. It has been suggested therefore that NET induction may prove a more fruitful therapeutic avenue than NET destruction.
Neonatal arterial ischaemic stroke
Neonatal arterial ischaemic stroke (NAIS), which often presents with seizures, is defined as occurring within the first 28 days of life,41 and is well documented as one of the most common forms of paediatric stroke.42 Typically the anterior circulation on the left side of the brain is affected, with an embolus most commonly lodging in the middle cerebral artery having passed through the patent foramen ovale.43 Despite causing severe motor, cognitive and/or behavioural abnormalities, the pathophysiology remains elusive. To date the only consistent independent risk factor for NAIS is perinatal inflammation secondary to infection/sepsis.2
The previously described interrelated process between inflammation and coagulation, namely immunothrombosis, is thought to play a role in the pathophysiology of NAIS. It has been shown that platelets play an important role in this, via the recruitment of neutrophils and monocytes (through CXCL-1, CXCL-2, CXCL-5, CCL-3, CCL-5, CCL-7), their adhesion (through P-selectin, CD-40) and activation (through TREM-1).1,2,44 It is possible that these immune cells lead to damaging inflammation within NAIS-susceptible arteries, triggering further thrombosis and occlusion. Further, in the context of sepsis, platelets bind to lipopolysaccharide via TLR-4, precipitating the binding of platelets to neutrophils, leading to swift NET formation and bacterial capture.19,45,46 This adds to the attraction of immune cells to the site, and the subsequent immunothrombotic cascade. In the complex cycles that precipitate arterial occlusion in a NAIS-susceptible artery, chemokine expression, leading to immunothrombosis, causes focal arteritis, ultimately increasing systemic inflammation (via CRP, IL-6, IL-1β, TNF-α) and ending in focal thrombosis and occlusion.2 Through further efforts into understanding the role of chemokine expression and induction of immunothrombosis in these cycles, we may be able to determine which individuals are at higher risk of NAIS, and subsequently develop prophylactic NET inhibitors to help reduce the incidence of NAIS.
Haemolytic anaemic diseases
Glucose-6-phosphate dehydrogenase (G6PD) deficiency, Shiga toxin-associated haemolytic uraemic syndrome (Stx-HUS) and Plasmodium falciparum (PF) malaria infection are three conditions affecting children that can all cause haemolytic anaemia.47,48,49 NETosis has been implicated in the pathophysiology of all three, either through its failure to produce NETs, or via their excessive release.
The most common enzymatic disorder of red blood cells is G6PD deficiency, which causes impaired NADPH production and increased susceptibility to bacterial infection.50 Symptoms usually only appear after certain triggers, and do so acutely. Research of severe cases has shown heavily reduced NADPH oxidase function in granulocytes, leading to impaired NET formation and accounting for the decreased microbial killing seen in the disease.49 NETs also play a role in Stx-HUS, which is caused primarily by Stx-producing Escherichia coli, by stimulating secretion of IL-6 and IL-8 from glomerular endothelial cells, thereby increasing the inflammatory response to the toxin.48,51 In addition to this increase in pro-inflammatory cytokines, NETs also activate platelets, contributing to immunothrombosis in the microvasculature of the kidney, which can lead to renal failure.45,48,52 In the case of malaria, there is evidence that increased NET production, secondary to the innate immune response, leads to the capture of PF parasites and subsequently stimulates the production of antinuclear IgG antibodies (ANA).47 The presence of both NETs and ANA supports the hypothesis that PF-induced autoimmune activity, via NETs, contributes to malaria pathogenesis in children, as observed in adults.53 Understanding exactly where NETs fit into the mechanisms of these diseases will allow for specific interventions to be developed. In G6PD deficiency, novel ways to restore NADPH oxidase function would allow for normal NET function. In Stx-HUS, blockage of the IL-6/8 pathways may result in lower levels of NETs. Further, in malaria, knowledge as to why there is increased NET production will allow for research into inhibiting this, thus reducing the production of ANA and therefore eliminating symptoms.
Chronic conditions
Systemic lupus erythematous
Autoimmune rheumatic diseases have been by far the most researched of the known NET-associated conditions. It has been suggested that chronic disparity between NET formation and degradation may be associated with the damage seen in the conditions.54 In adults, NETs have been found in various conditions including ANCA-associated vasculitis, systemic lupus erythematosus (SLE), rheumatoid arthritis, psoriatic arthritis, antiphospholipid syndrome, juvenile idiopathic arthritis, dermatomyositis, polymyositis and gout.55 In paediatrics, the role of NETs in SLE, a disease characterised by inflammation causing a spectrum of clinical manifestations that can affect any organ, is the most investigated.56,57
Briefly, SLE is an unregulated immune response caused by activation of the innate immune system, initiating release of inflammatory cytokines that go on to activate the adaptive immune system. This culminates in excessive autoantibody production and ultimately manifests itself through symptoms such as rash, clotting disorders and joint pain.56 This link between innate and adaptive immune systems is mediated by type 1 interferon (T1-IFN),58 being produced by the innate immune system, and acting on the adaptive immune system. In children, the B-cell-derived autoantibodies produced stimulate plasmacytoid dendritic cells (pDCs) to produce T1-IFN, forming a spiralling cascade between the innate and adaptive systems.56 SLE patients have been documented as having neutrophils producing abnormally high levels of NETs,55 which contributes to the T1-IFN predominance, or signature, seen in SLE affected children by further stimulating pDCs to produce T1-IFN.59,60,61 pDC TLR-9 activation is responsible for this, via binding with DNA and anti-DNA antibodies complexed with NET-derived antimicrobial peptides (LL37).59,62 A self-amplifying, positive feedback loop is then established, as T1-IFN in turn induced NETosis in these patients.62,63 It can therefore be seen that NETs are a major driving force in T1-IFN hyperproduction in SLE patients (Fig. 2).64,65
NETs in SLE. After exposure to anti-ribonucleoprotein (RNP) autoantibodies via Fc gamma receptor IIA (FcγRIIa), neutrophils produce NETosis. This occurs through toll like receptor (TLR-7) engagement leading to the increase in reactive oxygen species (ROS) production needed for NET formation. LL37 is incorporated into the NET structure, which acts to protect NET DNA from degradation. The NETs released from activated neutrophils bind to plasmacytoid dendritic cells (pDC) via FcγRIIa coupled with either anti-LL37 or anti-DNA antibodies. This stimulates TLR-9 activity and leads to T1-IFN production. This pDC-secreted T1-IFN heightens expression of TLR-7 in neutrophils, via interferon-α/β receptor (IFNAR), creating a positive feedback loop between the two cells, causing excess levels of T1-IFN, as seen in SLE patients
The effects of this elevated T1-IFN status in SLE patients are numerous, and contribute to the observed clinical picture (Supplemental Appendix 1).66 There are multiple points in the chain that links NETs to SLE that should be looked into and exploited. T1-IFN is the major driving force in SLE characterisation, and inhibiting its binding to interferon-α/β receptors (IFNAR) or inhibiting its production, by reducing NET levels, may allow for marked decreases in symptom expression in these patients. TLR-7 and 9 could potentially be targets for reducing NET levels in the SLE mechanism and warrant further research.
Type 1 diabetes mellitus
Type 1 diabetes mellitus (T1DM) is caused by autoimmune destruction of β-cells in the pancreatic Islets of Langerhans.67 Whilst the triggering factors of T1DM are not fully understood, it is widely accepted to be a multifactorial disease with peak incidence around puberty, which leaves patients dependent on life-long insulin treatment.68
It has already been documented that there is a reduction in circulating neutrophils in patients with T1DM, that is not due to peripheral cell death, impaired differentiation or anti-neutrophil antibodies.69 The pathological roles of the neutrophil however are still unclear. There is evidence showing a pronounced elevation in circulating protein levels and enzymatic activity of neutrophil elastase (NE) and proteinase 3 (PR3) in T1DM patients; both neutrophil serine proteases stored in neutrophil primary granules.67 Further, these increases were significantly correlated with increased NET formation (quantified using NET formation marker MPO-DNA complexes),70 pointing towards the conclusion that augmented NETosis caused the increase in NE and PR3 protein levels (r = 0.554, p < 0.001/r = 0.575, p < 0.001).67 Little is known around why there are fewer circulating neutrophils in T1DM patients or what effect this has on the disease expression. Further, whilst is seems that there is augmented NETosis in T1DM, it is not clear why. More efforts into determining the mechanisms behind the role of NETs in T1DM will pave the way towards minimising their potentially detrimental effects.
Respiratory diseases
Whilst NETs have been documented to have anti-bacterial,71 anti-fungal72 and anti-viral73 roles in respiratory host defence, they have also been implicated in the pathogenesis of conditions including cystic fibrosis (CF) and respiratory syncytial virus induced severe lower respiratory tract disease (RSV-LRTD).74,75,76 Over 85% of people with CF die prematurely from respiratory complications, and understanding the role of NETs could potentially help to prevent this.74 Long-term effects of RSV-LRTD are also well documented, including persistently low oxyhemoglobin levels, recurrent wheeze and extended LRTD.77
Recent reports highlight that the majority of extracellular DNA found in the CF lung originates from NETs.78 The CF lung is an environment favoured by chronic infections, namely Pseudomonas aeruginosa (P. aeruginosa), which potentially accounts for the high levels of NETs seen. Neutrophil elastase (NE), an azurophilic granule serine protease, is capable of degrading many of the structural proteins that make up the lung parenchyma,79 impairs the mucociliary escalator, and is known to be present in high concentrations in the airways of children with CF.74 Further studies have shown that NE is released in NETs, leading to the lung damage seen in CF.4 Other proteases, cathepsin G and proteinase 3, are also released in NETs, adding to this.80 It is not yet known however, whether the excess of NETs seen in CF is due to overproduction by CFTR-deficient neutrophils or simply due to lack of mucociliary clearance.74 It has also been noted that one of the immunothrombotic complications in CF is a degree of acquired P. aeruginosa resistance towards NET-mediated killing.81 Although it is well described that P. aeruginosa is hypermutable, it is not clear exactly why NET resistance occurs.
In the case of children with RVS-LRTD, there is occlusion of small airways by mucus plugs, causing airways obstruction. Although NETs trap the viral particles and have anti-viral properties, RSV has been shown to induce NETosis through a mechanism which appears to be TLR-4 dependent.82 It is thought that this excess in NETosis during RVS-LRTD contributes to the airway obstruction, through the formation of DNA-rich mucus plugs.75,76 It can therefore be seen that NETs inflict their damage either via direct lung injury or through airway obstruction (Fig. 3).76,83 The exact role of NETs in lung diseases is yet to be defined, but understanding this could lead to specific inhibition of NETs, or the blockage of NE activity, thus preventing the damage seen in CF. Further, unravelling the mechanism of how DNase can ‘melt’ NETs, might allow for its use in breaking down DNA-rich mucus plugs and helping to free air space in diseased lungs.
NETs in respiratory diseases. NETs are capable of causing lung damage through two pathways: airway obstruction (1) or direct lung injury (2). In the case of obstruction, the mixing of NETs with mucus forms highly viscoelastic mucous plugs which are protein and DNA rich. The excessive formation of NETs contributes to this damage, with extracellular NET level correlating inversely with lung function. The NET components myeloperoxidase (MPO) and citrullinated histones contribute via direct lung injury to both the alveolar epithelial cells and capillary endothelial cells, as NETs have effect on both sides of the alveolar-capillary interface
Graft-versus-host disease
Graft-versus-host disease (GvHD) is a common long-term complication following the receipt of transplanted tissue from a genetically different person, such as via a haematopoietic stem cell transplant (HSCT), bone marrow transplant (BMT) or any solid organ transplant.84,85 It is caused by the immune reaction precipitated by donor T lymphocytes and host antigens leading to the recruitment of macrophages, natural killer cells and cytotoxic T lymphocytes to target organs. It is also thought that NETosis is one of the links between the immune system and the damage caused to the recipient, via an undetermined mechanism. GvHD often manifests itself in the form of transplant-associated thrombotic microangiopathy (TA-TMA),85 which results in platelet aggregation and microthrombus formation leading to chronic multi-organ injury.86 The link between endothelial injury and complement activation in this disease process is poorly understood.
NETs are capable of activating compliment through both alternative and non-alternative pathways.85,87 In the alternative pathway, the membrane attack complex (MAC) C5b-9 is formed by NETs displaying complement factor P; this MAC is elevated in TA-TMA.87 Research into children post-HSCT, using plasma dsDNA concentration as a surrogate for NET level, found that elevated dsDNA levels were associated with increased risk of TA-TMA in future as well as overall mortality.85 It also suggested that IL-8 may have a role in NETosis, binding to neutrophils to stimulate NET production, after being released post-endothelial injury.85 Data from a study of patients undergoing BMT offered further understanding. It is known that this population is at increased risk for overwhelming infection,88 but the potential involvement of deficient NETosis is unclear. NET formation was quantified using NET-associated histone H3 release as a marker, and measured pre-BMT, pre-engraftment and post engraftment. Results showed decreased NET formation in all three groups as compared to control (p < 0.01),84 suggesting deficient NETosis may be an aspect of primary conditions resulting in the need for BMT. It also demonstrated prolonged defective NETosis even 200 days post BMT, identifying that NET deficiency may be involved in the pathophysiology that leaves patients with prolonged raised infection risk.84,89 Others have also suggested that impaired NET formation may be a novel innate immune deficiency of neonates that predisposes them to infection.90 The above examples indicate that NETs have a place in the development and extended effects of GvHD, but more needs to be understood about how the immune system uses NETs as an effector to inflict damage, so that we can stop them from doing so. Potential targets to focus on could be IL-8 and MAC C5b-9.
Discussion
We have described the mechanisms of action of a range of NET-associated paediatric conditions, all of which inflict major financial and humanitarian burdens on healthcare systems around the world. It is evident that the role of immunothrombosis and NETosis in each of the outlined diseases varies significantly,9 and thus presents multiple potential treatment targets to explore, whilst also posing the challenge of fully characterising each process.
Despite there being a relatively large knowledge base surrounding NETs, there has not yet been much impact on clinical practice in terms of effective treatments. Ramirez et al.6 suggested three possible reasons for this: (i) the low threshold of activation of neutrophils, which limits the development of reliable, easy, cheap diagnostic assays; (ii) the high costs of clinical trials; (iii) the lack of identification of appropriate targets to safely inhibit or decrease the NETs’ activity without impairing the defence.6
Neonates are more prone to infection than adults, perhaps due to the lower levels of NETosis exhibited by them,91 thus having a complete understand of the role of NETs in human disease would assist us in targeting treatment to either group. Currently, this age-dependent difference in NETosis makes it challenging to work on future pharmacological treatments.76,90 It is clear that NETs can exhibit both positive and negative influence on humans, depending on their levels and the stimuli acting upon them, which introduces the possible difficulty in developing specific treatments for sick patients. Thus the question arises as whether to stimulate or inhibit NETosis in the quest to reduce immunopathology.76
There is already some evidence that NETosis can be influenced by pharmacological intervention via one of the above-proposed routes. Through high-content screening, Chicca et al.92 have already identified a number of exogenous compounds able to modify NET function at various points of inhibition (Table 2).92 Moreover, Neonatal NET-Inhibitory Factor and other endogenously expressed NET-Inhibitory Peptides have been shown to inhibit NET formation in the blood of human umbilical cords by blocking the activity of peptidyl arginine deiminase 4 (PAD4).93 This demonstrates the potential for both exogenous and endogenous substances to be useful as therapeutic targets.
Further studies have shown that statins, through inhibition of the oxidative burst, increased NET formation,94 whilst treatment with cyclooxygenase in patients with bacterial pneumonia post BMT restored the ability of form NETs.95 The inhibition of NETosis has also been described, examples include the suppression of complement factor C5 and blocking of chemokine activation in neutrophils.96,97 Finally, some groups have also targeted the NET itself, using exogenous DNase to attack the extracellular DNA backbone of NETs, or histone blocking antibodies to dismantle them.6,98
As previously mentioned, the pathophysiology of SLE is currently the most understood of the NET-associated pathologies. As such, a number of already established drugs have been found to provide interesting results when used in the context of inhibiting NETosis (Table 3).7,99
More research is needed to evaluate the clinical efficacy of such drugs, but it is discoveries like this that lead to the development of tomorrow’s first-line treatments.
Conclusion
We have presented a review of the current research on immunothrombosis/NETosis in paediatric conditions ranging from SLE to NAIS to OM. Much of the pathophysiology remains unclear and there are many avenues that need exploring. More work should be done on understanding the role of NETs in the pathophysiology of paediatric diseases. This will ultimately leads to the development of innovative treatments of specific paediatric disorders that manifest through altered NET function.
References
Engelmann, B. & Massberg, S. Thrombosis as an intravascular effector of innate immunity. Nat. Rev. Immunol. 13, 34–45 (2013).
Giraud, A. et al. Role of perinatal inflammation in neonatal arterial ischemic stroke. Front. Neurol. 16, 612 (2017).
Vazquez-Garza, E. et al. Venous thromboembolism: thrombosis, inflammation, and immunothrombosis for clinicians. J. Thromb. Thrombolysis 44, 377–385 (2017).
Brinkmann, V. et al. Neutrophil extracellular traps kill bacteria. Science 303, 1532–1535 (2004).
Naegele, M. 1 et al. Neutrophils in multiple sclerosis are characterized by a primed phenotype. J. Neuroimmunol. 242, 60–71 (2012).
Ramirez, G. A. et al. Bet on NETs! Or on how to translate basic science into clinical practice. Front. Immunol. 7, 417 (2016).
Mitsios, A. et al. NETopathies? Unraveling the Dark Side of Old Diseases through Neutrophils. Front. Immunol. 7, 678 (2017).
Yang, S. et al. Neutrophil extracellular traps promote hypercoagulability in patients with sepsis. Shock 47, 132–139 (2017).
Kazzaz, N. M., Sule, G. & Knight, J. S. Intercellular interactions as regulators of NETosis. Front. Immunol. 14, 453 (2016).
Yang, H. et al. New insights into neutrophil extracellular traps: mechanisms of formation and role in inflammation. Front. Immunol. 7, 302 (2016).
Kimball, A. S. et al. The emerging role of NETs in venous thrombosis and immunothrombosis. Front. Immunol. 7, 236 (2016).
Vorobjeva, N. V. & Pinegin, B. V. Neutrophil extracellular traps: mechanisms of formation and role in health and disease. Biochemistry 79, 1580–1591 (2014).
Muñoz, L. E. et al. Editorial: NEtosis 2: the excitement continues. Front. Immunol. 20, 1318 (2017).
Kaplan, M. J. & Radic, M. Neutrophil extracellular traps (NETs): double-edged swords of innate immunity. J. Immunol. 189, 2689–2695 (2012).
Iba, T. et al. Is the neutrophil a ‘prima donna’ in the procoagulant process during sepsis? Crit. Care 18, 230 (2014).
Gaertner, F. & Massberg, S. Blood coagulation in immunothrombosis—At the frontline of intravascular immunity. Semin. Immunol. 28, 561–569 (2016).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). J. Am. Med. Assoc. 315, 801–810 (2016).
Shen, X. F. et al. Neutrophil dysregulation during sepsis: an overview and update. J. Cell. Mol. Med. 21, 1687–1697 (2017).
Clark, S. R. et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat. Med. 13, 463–469 (2007).
Gould, T. J., Lysov, Z. & Liaw, P. C. Extracellular DNA and histones: double-edged swords in immunothrombosi. J. Thromb. Haemost. 13, S82–S91 (2015).
Delabranche, X. et al. Evidence of netosis in septic shock-induced disseminated intravascular coagulation. Shock 47, 313–317 (2017).
Hoffmann, J. J. M. L. Neutrophil CD64: a diagnostic marker for infection and sepsis. Clin. Chem. Lab. Med. 47, 903–916 (2009).
Adly, A. A. et al. Circulating soluble triggering receptor expressed on myeloid cells‐1 (sTREM‐1) as diagnostic and prognostic marker in neonatal sepsis. Cytokine 65, 184–191 (2014).
Caplan, M. S. & Fanaroff, A. Necrotizing: a historical perspective. Semin. Perinatol. 41, 2–6 (2017).
Alibrahim, B., Aljasser, M. I. & Salh, B. Fecal calprotectin use in inflammatory bowel disease and beyond: a mini-review. Can. J. Gastroenterol. Hepatol. 29, 157–163 (2016).
Carroll, D. et al. Faecal calprotectin concentrations and diagnosis of necrotising enterocolitis. Lancet 361, 310–311 (2003).
Urban, C. F. et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 5, e1000639 (2009).
MacQueen, B. C. et al. Elevated fecal calprotectin levels during necrotizing enterocolitis are associated with activated neutrophils extruding neutrophil extracellular traps. J. Perinatol. 36, 862–869 (2016).
Giuliani, S. et al. Coagulation gene expression profiling in infants with necrotizing enterocolitis. J. Pediatr. Gastroenterol. Nutr. 63, e16975 (2016).
Vincent, D. et al. NEC is likely a NETs dependent process and markers of NETosis are predictive of NEC in mice and humans. Sci. Rep. 8, 12612 (2018).
Nguyen, D. N. et al. Elevated levels of circulating cell-free DNA and neutrophil proteins are associated with neonatal sepsis and necrotizing enterocolitis in immature mice, pigs and infants. Innate Immunol. 23, 524–536 (2017).
Allin, B. et al. A UK wide cohort study describing management and outcomes for infants with surgical necrotising enterocolitis. Sci. Rep. 7, 41149 (2017).
Cripps, A. W., Otczyk, D. C. & Kyd, J. M. Bacterial otitis media: a vaccine preventable disease? Vaccine 23, 2304–2310 (2005).
Short, K. R. et al. Antibodies mediate formation of neutrophil extracellular traps in the middle ear and facilitate secondary pneumococcal otitis media. Infect. Immun. 82, 364–370 (2014).
Val, S. et al. Proteomic characterization of middle ear fluid confirms neutrophil extracellular traps as a predominant innate immune response in chronic otitis media. PLoS. ONE 11, e0152865 (2016).
Thornton, R. B. et al. Neutrophil extracellular traps and bacterial biofilms in middle ear effusion of children with recurrent acute otitis media - a potential treatment target. PLoS. ONE 8, e53837 (2013).
Mittala, R. et al. Role of innate immunity in the pathogenesis of otitis media. Int. J. Infect. Dis. 29, 259–267 (2014).
Juneau, R. A. et al. Nontypeable haemophilus influenzae initiates formation of neutrophil extracellular traps. Infect. Immun. 79, 431–438 (2011).
Langereis, J. D. & Hermans, P. W. Novel concepts in nontypeable Haemophilus influenzae biofilm formation. FEMS Microbiol. Lett. 346, 81–89 (2013).
Meng, W. et al. Depletion of neutrophil extracellular traps in vivo results in hypersusceptibility to polymicrobial sepsis in mice. Crit. Care 16, R137 (2012).
Raju, T. N. K. et al. Ischemic perinatal stroke: summary of a workshop sponsored by the National Institute of Child Health and Human Development and the National Institute of Neurological Disorders and Stroke. Pediatrics 120, 609–616 (2007).
Kirton, A. & deVeber, G. Life after perinatal stroke. Stroke 44, 3265–3271 (2013).
Pulver, M. et al. Symptomatic neonatal arterial ischemic stroke with prenatal and postnatal neuroimaging. Child Neurol. Open 4, 329048X17730460 (2017).
de Stoppelaar, S. F., van’t Veer, C. & van der Poll, T. The role of platelets in sepsis. Thromb. Haemost. 112, 666–677 (2014).
Carestia, A., Kaufman, T. & Schattner, M. 1 Platelets: new bricks in the building of neutrophil extracellular traps. Front. Immunol. 6, 271 (2016).
Hoppenbrouwers, T., et al. Neutrophil extracellular traps in children with Meningococcal sepsis. Pediatr. Crit. Care Med. 19, e286–e291 (2018).
Baker, V. S. et al. Cytokine-associated neutrophil extracellular traps and antinuclear antibodies in Plasmodium falciparum infected children under six years of age. Malar. J. 7, 41 (2008).
Ramos, M. V. et al. Induction of neutrophil extracellular traps in Shiga toxin-associated hemolytic uremic syndrome. J. Innate Immunol. 8, 400–411 (2016).
Siler, U. et al. Severe glucose-6-phosphate dehydrogenase deficiency leads to susceptibility to infection and absent NETosis. J. Allergy Clin. Immunol. 139, 212–219 (2017).
Cappellini, M. D. & Fiorelli, G. Glucose-6-phosphate dehydrogenase deficiency. Lancet 371, 64–74 (2008).
Fernandez, G. C. et al. Relevance of neutrophils in the murine model of haemolytic uraemic syndrome: mechanisms involved in Shiga toxin type 2-induced neutrophilia. Clin. Exp. Immunol. 146, 76–84 (2006).
Fuchs, T. A. et al. Extracellular DNA traps promote thrombosis. Proc. Natl Acad. Sci. USA 107, 15880–15885 (2010).
Boeltz, S. et al. Neutrophil extracellular traps open the Pandora’s box in severe malaria. Front. Immunol. 8, 874 (2017).
Lood, C. et al. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat. Med. 22, 146–153 (2016).
Lee, K. H. et al. Neutrophil extracellular traps (NETs) in autoimmune diseases: a comprehensive review. Autoimmune Rev. 16, 1160–1173 (2017).
Midgley, A., Watson, L. & Beresford, M. W. New insights into the pathogenesis and management of lupus in children. Arch. Dis. Child. 99, 563–567 (2014).
Huttenlocher, A. & Smith, J. A. Neutrophils in pediatric autoimmune disease. Curr. Opin. Rheumatol. 27, 500–504 (2015).
Banchereau, J. & Pascual, V. Type I interferon in systemic lupus erythematosus and other autoimmune diseases. Immunity 25, 383–392 (2006).
Garcia-Romo, G. S. et al. Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci. Transl. Med. 3, 20 (2011).
Villanueva, E. et al. Netting neutrophils induce endothelial damage, infiltrate tissues, and expose immunostimulatory molecules in systemic lupus erythematosus. J. Immunol. 187, 538–552 (2011).
Xie, C. et al. Association between discoid lupus erythematosus and chronic granulomatous disease - report of two cases and review of the literature. Pediatr. Dermatol. 33, 114–120 (2016).
Tsokos, G. C. et al. New insights into the immunopathogenesis of systemic lupus erythematosus. Nat. Rev. Rheumatol. 22, 716–730 (2016).
Yu, Y. & Su, K. Neutrophil extracellular traps and systemic lupus erythematosus. J. Clin. Cell. Immunol. 4, 139 (2013).
Bosch, X. TRAPping the cellular mechanisms of lupus. EMBO Mol. Med. 3, 578–580 (2011).
Branzk, N. & Papayannopoulos, V. Molecular mechanisms regulating NETosis in infection and disease. Semin. Immunopathol. 35, 513–530 (2013).
Eloranta, M. L. & Rönnblom, L. Cause and consequences of the activated type I interferon system in SLE. J. Mol. Med. 94, 1103–1110 (2016).
Wang, Y. et al. Increased neutrophil elastase and proteinase 3 and augmented NETosis are closely associated with β-cell autoimmunity in patients with type 1 diabetes. Diabetes 63, 4239–4248 (2014).
Toumilehto, J. The emerging global epidemic of type 1 diabetes. Curr. Diab. Rep. 13, 795–804 (2013).
Valle, A. et al. Reduction of circulating neutrophils precedes and accompanies type 1 diabetes. Diabetes 63, 2072–2077 (2013).
Kessenbrock, K. et al. Netting neutrophils in autoimmune small-vessel vasculitis. Nat. Med. 15, 623–625 (2009).
Beiter, K. et al. An endonuclease allows Streptococcus pneumoniae to escape from neutrophil extracellular traps. Curr. Biol. 16, 401–407 (2006).
McCormick, A. et al. NETs formed by human neutrophils inhibit growth of the pathogenic mold Aspergillus fumigatus. Microbes Infect. 12, 928–936 (2010).
Saitoh, T. et al. Neutrophil extracellular traps mediate a host defense response to human immunodeficiency virus-1. Cell Host Microbe 12, 109–116 (2012).
Gray, R. D., McCullagh, B. N. & McCray, P. B. NETs and CF lung disease: current status and future prospects. Antibiotics 4, 62–75 (2015).
Cortjens, B. et al. Neutrophil extracellular traps cause airway obstruction during respiratory syncytial virus disease. J. Pathol. 238, 401–411 (2016).
Cortjens, B., van Woensel, J. B. & Bem, R. A. Neutrophil extracellular traps in respiratory disease: guided anti-microbial traps or toxic webs? Paediatr. Respir. Rev. 21, 54–61 (2017).
Simoes, E. A. Treatment and prevention of respiratory syncytial virus lower respiratory tract infection. long-term effects on respiratory outcomes. Am. J. Respir. Crit. Care. Med. 163, S14–S17 (2001).
Dwyer, M. et al. Cystic fibrosis sputum DNA has NETosis characteristics and neutrophil extracellular trap release is regulated by macrophage migration-inhibitory factor. J. Innate Immun. 6, 765–779 (2014).
Quinn, D. J., Weldon, S. & Taggart, C. C. Antiproteases as therapeutics to target inflammation in cystic fibrosis. Open Respir. Med. J. 4, 20–31 (2010).
Dubois, A. V. et al. Influence of DNA on the activities and inhibition of neutrophil serine proteases in cystic fibrosis sputum. Am. J. Respir. Cell Mol. Biol. 47, 80–86 (2012).
Young, R. L. et al. Neutrophil extracellular trap (NET)-mediated killing of Pseudomonas aeruginosa: evidence of acquired resistance within the CF airway, independent of CFTR. PLoS ONE 6, e23637 (2011).
Funchal, G. A. et al. Respiratory syncytial virus fusion protein promotes TLR-4–dependent neutrophil extracellular trap formation by human neutrophils. PLoS ONE 10, e0124082 (2015).
Wright, T. K. et al. Neutrophil extracellular traps are associated with inflammation in chronic airway disease. Respirology 21, 467–475 (2016).
Glenn, J. W. et al. Deficient neutrophil extracellular trap formation in patients undergoing bone marrow transplantation. Front. Immunol. 27, 250 (2016).
Gloude, N. J. et al. Circulating dsDNA, endothelial injury, and complement activation in thrombotic microangiopathy and GVHD. Blood 130, 1259–1266 (2017).
Jodele, S. et al. A new paradigm: diagnosis and management of HSCT- associated thrombotic microangiopathy as multi-system endothelial injury. Blood. Rev. 29, 191–204 (2015).
Eyuen, J. et al. NETosing neutrophils activate complement both on their own NETs and bacteria via alternative and non-alternative pathways. Front. Immunol. 7, 137 (2016).
Parody, R. et al. Severe infections after unrelated donor allogeneic hematopoietic stem cell transplantation in adults: comparison of cord blood transplantation with peripheral blood and bone marrow transplantation. Biol. Blood Marrow Transpl. 12, 734–748 (2006).
Ramaprasad, C., Pouch, S. & Pitrak, D. Neutrophil function after bone marrow and hematopoietic stem cell transplant. Leuk. Lymphoma 51, 756–767 (2010).
Yost, C. C. et al. Impaired neutrophil extracellular trap (NET) formation: a novel innate immune deficiency of human neonates. Blood 113, 6419–6427 (2009).
Lipp, P. et al. Less neutrophil extracellular trap formation in term newborns than in adults. Neonatology 111, 182–188 (2017).
Chicca, I. J. et al. Development and application of high-content biological screening for modulators of NET production. Front. Immunol. 9, 337 (2018).
Yost, C. C. et al. Neonatal NET-inhibitory factor and related peptides inhibit neutrophil extracellular trap formation. J. Clin. Investig. 126, 3783–3798 (2016).
Chow, O. A. et al. Statins enhance formation of phagocyte extracellular traps. Cell Host Microbe 8, 445–454 (2010).
Domingo-Gonzalez, R. et al. Inhibition of neutrophil extracellular trap formation after stem cell transplant by prostaglandin E2. Am. J. Respir. Crit. Care Med. 193, 186–197 (2016).
Garcia, C. C. et al. Complement C5 activation during influenza A infection in mice contributes to neutrophil recruitment and lung injury. PLoS ONE 8, e64443 (2013).
Rossaint, J. et al. Synchronized integrin engagement and chemokine activation is crucial in neutrophil extracellular trap–mediated sterile inflammation. Blood 123, 2573–2584 (2014).
Caudrillier, A. et al. Platelets induce neutrophil extracellular traps in transfusion-related acute lung injury. J. Clin. Investig. 122, 2661–2671 (2012).
Gupta, S. & Kaplan, M. J. The role of neutrophils and NETosis in autoimmune and renal diseases. Nat. Rev. Nephrol. 12, 402–413 (2016).
Author information
Authors and Affiliations
Contributions
T.F., S.G.: substantial contribution to conception and design, acquisition of data, analysis and interpretation of data. T.F., S.G., S.E., P.D.C.: drafting the article or revising it critically for important intellectual content. T.F., S.G., S.E., P.D.C.: final approval of the version to be published
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Franchi, T., Eaton, S., De Coppi, P. et al. The emerging role of immunothrombosis in paediatric conditions. Pediatr Res 86, 19–27 (2019). https://doi.org/10.1038/s41390-019-0343-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0343-6
This article is cited by
-
Pediatric immunothrombosis—Understudied… but what potential!
Pediatric Research (2019)