Abstract
Background
Childhood obesity has become a major health problem in children under the age of 5 years. Providing reference standards would help paediatricians to detect and/or prevent health problems related to both low and high levels of body mass and to central adiposity later in life. Therefore, the aim of this study was to examine the prevalence of different weight status categories and to provide sex- and age-specific anthropometry reference standards for Spanish preschool children.
Methods
A total of 3178 preschool children (4.59±0.87 years old) participated in this study. Prevalence of different degrees of obesity (mild, severe, and morbid) and other weight status categories were determined.
Results
Reference standards were obtained. Prevalence of overweight and obese preschool children in the Spanish population ranged from 21.4 to 34.8%. Specifically, the obesity prevalence was 3.5, 1.2, and 1.3% of these subjects were categorized as mild, severe, and morbid obese. Sex- and age-specific reference standards for anthropometric parameters are provided for every 0.25 years (i.e. every trimester of life).
Conclusion
Our results show a high prevalence of overweight/obese preschoolers. The provided sex- and age-specific anthropometric reference standards could help paediatricians to track and monitor anthropometric changes at this early stage in order to prevent overweight/obesity.
Similar content being viewed by others
Introduction
Examining the entire body mass index (BMI) spectrum, from underweight to obesity, has a relevant role in the clinical setting.1 This would enable monitoring the somatic development of children and would help early diagnosis, given the established relations between weight status and health parameters. Different criteria have been used to classify underweight, normal weight, overweight, and obesity. The most internationally well known and most frequently used criteria are the World Obesity Federation (WOF)2 and World Health Organization (WHO).3 However, differences in study methodologies to establish the criteria (i.e. sample size or characteristics of the study sample) could lead to considerable variation in prevalence estimates.1,4 Thus, there is a need to examine the prevalence of the whole BMI spectrum using different criteria.
Obesity, which can be found at the top of the BMI spectrum, has become a major health problem in young people in the past years.5 Recent evidence has shown that the rates of overweight/obesity have reached epidemic proportions in children under the age of 5 years.5 In line with this assumption, the WHO reported that more than 41 million children of this age group were classified as overweight or obese in 2014. Likewise, it is estimated that by 2020 the number of overweight/obese children between the ages of 3 and 5 years will rise to 60 million.6 In Europe, the prevalence of overweight/obese children (between 2 and 9.9 years old) based on the WOF2 criteria ranged from 21 to 42% in the south of Europe and remained under 11% in the north, being higher in girls than in boys (21.1 vs. 18.6%).4 Similarly, data showed a higher prevalence of overweight/obesity in preschoolers in the south compared with the north of Europe (WOF 17 vs. 9%, WHO 31 vs. 21%).7 However, these studies examined small samples of children from one single region per country.4,7 Further studies in preschool children with larger sample sizes which are geographically distributed across multiple countries may provide a more real description of the global problem. Furthermore, previous studies in older children and adolescents observed that the increase of overweight/obesity prevalence has slowed down8,9 or even decreased.8,9 Nevertheless, the prevalence of severe and morbid obesity rates in childhood seems to have increased in several countries.10 To our knowledge, there is no previous information about the prevalence of severe/morbid obesity in preschool children. Therefore, it would be highly relevant from a clinical and public health perspective to assess the prevalence of different degrees of obesity (mild, severe, and morbid). Furthermore, it would be of great interest to examine the new cut-points for defining morbid obesity in children in relation to adults’ BMI cut-point of ≥40 kg/m2.
In the past decades, underweight has received much less attention, even though the health consequences of its different degrees could affect growth and development. This is also of public health concern.11 A trend analysis conducted by de Onis et al.12 showed that the worldwide prevalence of childhood underweight was projected to decline from 26.5% in 1990 to 17.6% in 2015. In developed countries, the prevalence was estimated to decrease from 1.6 to 0.9%. However, the percentage of underweight children has been seen to have risen from 1 to 23% depending on the characteristics of the study sample, the year of study, the country, and the definition of underweight.13,14 Therefore, the classification of different degrees of underweight and obesity and different weight status according to different cut-off criteria such as WOF and WHO are needed.
For an accurate assessment and interpretation of the anthropometric parameters, sex- and age-specific reference standards are needed. Previous studies have shown anthropometric reference standards in children and adolescents for specific populations.15,16,17,18 However, international cut-points for markers of abdominal adiposity in children are still lacking. For instance, for the definition of metabolic syndrome in youth, central obesity is defined as a waist circumference above the sex- and age-specific 95th percentile.19 Therefore, from a public health point of view, these reference standards would help health care professionals to detect and/or prevent health problems related to low and high levels of total and central fatness later in life. Nevertheless, most of the examined studies provided reference values for children at the age of ≥6 years.17,18 To the best of our knowledge, there is no study providing reference values in Spanish preschool children.
The aims of our study are (1) to determine the prevalence of underweight, normal weight, overweight, and different grades of obesity (mild, severe, and morbid) based on WOF and WHO criteria and (2) to examine sex- and age-specific anthropometric parameters obtained in a relatively large and geographically distributed sample of Spanish preschool children aged 3.0–6.25 years.
Methods
Study design and participants
This study is under the framework of the PREFIT (Assessing levels of FITness in PREeschoolers) project. The purpose of this project was to assess anthropometry and physical fitness in preschool children from 10 different cities in Spain (i.e. South: Almería, Cádiz, Granada, Canary Island; Centre: Castellón de la Plana, Cuenca, Madrid, Palma de Mallorca; and North: Vitoria-Gasteiz and Zaragoza). The selection of cities was based on: (1) having a geographical distribution of the data across Spain and (2) convenience, that is, having a research group that could participate in the study. The data collection took place from January 2014 to November 2015. This study was conducted according to the guidelines of the Declaration of Helsinki and all procedures involving human subjects were approved by the Review Committee for Research Involving Human Subjects (reference number: 845). A written informed consent was obtained from the parents or legal guardians of all subjects.
A total of 4338 preschoolers were invited to participate in the project. The information about the aims and protocol of the study were provided to the families by the teachers/staff of the schools involved. Of these, 20 children were excluded due to suffering from any disease that limited the correct performance of the test or because they cried during the tests. Thus, all the children who were healthy and did not present any impediment during the execution of the test were included in the analyses. Finally, a total of 3178 children (mean age 4.59 (±0.87) years old, 1677 boys; participation rate of 73.7%) were recruited from different schools and participated in the study. The flow chart is shown in Figure S1.
Measures
Weight (kg) and height (cm) were assessed barefoot and in light clothing with a balance scale (SECA 213, Hamburg, Germany) and stadiometer (SECA 213, Hamburg, Germany), respectively. Thereafter, we calculated BMI (kg/m2). The cut-off points used to determine the entire growth spectrum (i.e. from underweight to obesity) and its prevalence were those established by the WOF2,20 and by the WHO.21 The WOF is based on survey data from six different countries in Asia, Europe, and America. The cut-offs were developed for youth aged from 2 to 18 years old and provided weight status categories for each month of age from underweight to severe obesity.2 Additionally, morbid obesity was just recently defined, which provides new opportunities to study the most pathological obesity from very young ages.20 The WHO data are based on a sample of healthy breastfed infants and young children from different places around the world (i.e. Brazil, Ghana, India, Norway, Oman, and the United States). The WHO child growth standards provided cut-offs based on sex- and age-specific z-scores for underweight, normal weight, overweight, and obesity (not categorizing into mild, severe, or morbid obesity).3
We assessed waist circumference (cm) with a non-elastic tape (SECA 200, Hamburg, Germany) at the level of the umbilicus zone. The measurements were taken at the end of normal expiration without the non-elastic tape compressing the skin. Thereafter, we calculated the waist-to-height ratio and provided its reference standards.
All the anthropometric measurements were taken twice, and we calculated the mean of both measurements, which were then used for the analyses. Likewise, a strict protocol was performed to ensure standardization across all the involved centres.
Statistical analyses
Characteristics of the study sample and prevalence of weight status categories
Descriptive anthropometric characteristics were calculated for the entire sample, and separated by sex and age groups. To explore possible differences between sex and age groups, we performed a two-way analysis of variance with sex and age groups (i.e. 3, 4, and 5 years old) as fixed factors and anthropometric characteristics as dependent variables. The significance level was fixed at p < 0.05. To estimate the prevalence of weight status categories, frequencies were calculated. The 95% confidence intervals were simultaneously calculated using the approach of Glaz and Sison22 (R package DescTools23).
Sex- and age-specific anthropometric reference standards
To determine reference standards for the study sample, the Generalized Additive Model for Location, Scale and Shape (GAMLSS) was used.24 GAMLSS is an extension of the LMS (latent moderated structural equations) method and is able to model up to four parameters of different distributions: µ accounts for the location, σ for the scale, υ for the skewness, and τ for the kurtosis. The Box–Cox Cole and Green, Box–Cox t, and Box–Cox power exponential distribution were fitted to the observed data. Furthermore, the influence of age on the distribution parameters was modelled constantly, linearly, or as a cubic spline function. Goodness of fit was assessed by the Bayesian information criterion and worm plots.25 More information about the procedure has been described elsewhere.26 The anthropometric percentile curves (1st, 3rd, 5th, 10th, 15th, 20th, 30th, 40th, 50th, 60th, 70th, 80th, 85th, 90th, 95th, 97th, and 99th percentiles) were calculated based on the model that showed the best goodness of fit (Table S1). Reference standards were provided for boys and girls with a precision of 0.25 years of age (each trimester, i.e. every 3 months of the year) as a main outcome of the manuscript and also every 0.025 years of age as supplementary material (which would be equivalent to approximately 9 days/1.5 week of age increments).
The descriptive statistical analyses were performed with the SPSS software (version 20, IBM Corporation, New York, NY, USA). Reference standard analyses were performed using the GAMLSS package (version 4.4-0) for the statistical software R (version 3.3.1, R Foundation for Statistical Computing, Vienna, Austria).27
Results
Characteristics of the study sample
Table S2 shows the anthropometric characteristics of the study sample. In short, boys were slightly heavier and taller compared to girls (all p < 0.001). In contrast, girls showed higher waist circumference and waist-to-height ratio compared to boys (all p ≤ 0.010). No significant differences between sexes were observed regarding age and BMI (p > 0.807). As expected, in regards to the age group, older children were heavier, taller, and presented higher waist circumference compared to younger children (all p < 0.001). Waist-to-height ratio decreased as the age increased (p < 0.001). BMI did not differ between age groups (p = 0.093).
Prevalence of weight status categories
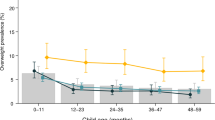
Prevalence of weight status categories using both the WOF and the WHO definitions in preschool children is shown in Fig. 1. Overall, following the WOF cut-off points, the prevalence of the different degrees of underweight were 0.2 (95% confidence interval (CI), 0.0–1.7), 0.6 (95% CI, 0.0–2.2), and 4.1% (95% CI, 2.6–5.6) for underweight types III, II, and I, respectively. Normal weight prevalence was 73.7% (95% CI, 72.2–75.2). Overweight prevalence in preschool children was 15.4% (95% CI, 13.9–17.0), while the prevalence of mild (obesity type I), severe (obesity type II), and morbid obesity (obesity type III) were 3.5% (95% CI, 2.0–5.0), 1.2% (95% CI, 0.0–2.7), and 1.3% (95% CI, 0.0–2.8), respectively, which sum up to a total prevalence of obesity of 6.0% (95% CI, 4.5–7.5). On the other hand, using the WHO references, underweight prevalence was 0.1 (95% CI, 0.0–1.8), 0.3 (95% CI, 0.0–2.0), and 2.8% (95% CI, 1.1–4.6) for underweight types III, II, and I respectively. A percentage of 62.1% (95% CI, 60.4–63.8) of the sample was classified as normal weight. The prevalence of overweight and obesity were 29.0% (95% CI, 27.3–30.8) and 5.8% (95% CI, 4.1–7.5), respectively. We observed main differences between WOF and WHO prevalence for normal weight (73.7% with WOF vs. 62.1% with WHO) and overweight (15.4% with WOF vs. 29.0% with WHO). Underweight and obesity prevalence, however, were much closer (underweight: 4.8% with WOF vs. 3.1% with WHO; obesity: 6% with both WOF and WHO).
In regards to sex comparison, different patterns were observed for WOF and WHO in underweight. These showed that girls have lower percentages than boys following the WOF criteria but not the WHO criteria (WOF: 5.1 (95% CI, 3.1–7.1) vs. 4.6 (95% CI, 2.4–6.9); WHO: 1.9 (95% CI, 0.0–4.2) vs. 4.5 (95% CI, 2.0–7.2) for boys and girls, respectively). In normal weight, boys presented higher percentage points than girls (WOF: 75.6 (95% CI, 73.7–77.6) vs. 71.6% (95% CI, 69.4–73.9); WHO: 66.1 (95% CI, 63.9–68.5) vs. 57.6% (95% CI, 55.0–60.2) for boys and girls, respectively). It was observed that overweight percentage was higher in girls than in boys using either the WOF or the WHO (WOF: 13.1 (95% CI, 11.1–15.1) vs. 18.1% (95% CI, 15.9–20.4); WHO: 27.2 (95% CI, 24.9–29.5) vs. 31.0% (95% CI, 28.5–33.7) for boys and girls, respectively). In obesity, depending on the criteria selected, the results differed between sexes (WOF: 6.2 (95% CI, 4.2–8.2) vs. 5.8% (95% CI, 3.6–8.1); WHO: 4.8 (95% CI, 2.6–7.2) vs. 6.9% (95% CI, 4.3–9.5) for boys and girls, respectively).
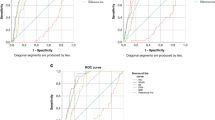
Sex- and age-specific anthropometric reference standards
Reference standards (i.e. 10th, 20th, 30th, 40th, 50th, 60th, 70th, 80th, 90th, and 99th percentiles) for weight, height, BMI, waist circumference, and waist-to-height ratio for every 0.25 years of age (trimester of year) from 3 to 6.25 years old are shown in Tables 1 and 2. More detailed reference standards for the 1st, 3rd, 5th, 10th, 15th, 20th, 30th, 40th, 50th, 60th, 70th, 80th, 85th, 90th, 95th, 97th, and 99th percentiles and for each 0.025 years of age are provided in the supplementary material (Tables in xlsx format). The 1st, 5th, 15th, 25th, 50th, 75th, 85th, 95th, and 99th percentiles curves for each anthropometric parameter are shown in Figs. 2 and 3. Differences between the 95th and 99th percentile curves were larger in weight, BMI, waist circumference, and waist-to-height ratio than between other shown percentiles in boys and girls and in all age groups. These differences, however, were greater in older children. The 50th percentile curve of BMI showed a plateau in boys from 4 to 5.5 years old and in girls across the whole age range. The 95th and 99th percentile curves in boys’ but not girls’ BMI had a J-curve, being more pronounced in the 99th percentile curve.
Discussion
The main findings of the present study are the following: (1) The prevalence of underweight in children was found to be 3–5%, whilst the normal weight prevalence ranged from 62.1 to 73.7%. (2) The prevalence of overweight/obesity in Spanish preschool children was 21.4 and 34.8% according to the WOF and WHO criteria, respectively. Among the whole study population, 6% of children had obesity according to the previously mentioned criteria. Likewise, regardless of the criteria used, the prevalence of overweight/obesity was higher in girls than in boys. (3) More specifically, severe or morbid obesity was found in 2.5% of the children. and (4) Sex- and age-specific reference standards for weight, height, BMI, waist circumference, and waist-to-height ratio from a relatively large sample of preschool children geographically distributed across Spain are provided. This will allow a better interpretation of anthropometric assessments at this early stage of life in future studies. To the best of our knowledge, this is the first study ever to report the prevalence of the different degrees of obesity and underweight in preschool children in Spain or any other large-scale study conducted in any other country.
Prevalence of weight status categories
In regards to underweight status, only a few studies examined the prevalence in preschool children.12,14 In Spain, a trend analysis (1983–2011) showed that underweight prevalence increased from 13.7 to 22.6% in preschoolers aged 2–5 years old.14 Our results showed much lower rates of underweight (3–5%), in line with previous studies in preschoolers from other developed countries (1%)12 and also in Spanish and Portuguese children aged 6–8 years old (1–6%).13,28 Such differences could be explained by the different characteristics of the study samples and the criteria selected for grouping weight status, as well as by the dates of the measurements. Nevertheless, regardless of the variation observed among studies, it is interesting to highlight that our study shows that underweight prevalence was slightly lower than those obtained in obesity (mild, severe, and morbid). In addition, most of the children classified as underweight belonged to the milder category of underweight (i.e. type I, BMI 17–18.4 kg/m2 at 18 years of age).
Little is known about the increased risk for diseases related to underweight compared to obesity in children, and more studies are needed in this direction. In this context, one study observed greater morbidity in underweight compared to obesity in preschoolers.11 Therefore, at these early ages, low body weight is also an important factor that should be considered from a public health point of view.
Approximately 15.4 and 29% (according to the WOF and WHO criteria, respectively) of the examined preschool children were overweight. Our results are in line with those found in European children (2.0–9.9 years old), where the total overweight prevalence was 12.8% based on WOF.4 Particularly, WOF data showed that Spain (including only one city, i.e. Zaragoza) presented the same overweight rate that we found in the entire sample of Spanish preschool children (i.e. overweight: 15%).4
For obesity rates, we observed that the same prevalence of this weight status was obtained using WHO and WOF (6%). Ahrens et al.4 also showed a similar percentage (i.e. 7%) in European children from 2 to 9 years old when using the WOF criteria. Likewise, they specifically provided the Spanish prevalence (including only one city) showing the same percentage (i.e. 6%) as we observed in our project where the data are provided by large geographically distributed sample. However, there is no information about prevalence of different degrees of obesity (from mild to morbid), which hampers any comparison.
Considering overweight and obesity prevalence together, our study showed that already at preschool ages, 21 and 35% of the sample examined were classified into these two weight status categories. Based on data of 144 countries, de Onis et al.6 calculated a global prevalence of overweight/obesity in preschool children of 12.9% according to the WHO criteria. Such differences between prevalence could be explained by1 the different z-score criteria used for overweight/obesity classification, which did not include those at risk of overweight, that is, z-score >1 and ≤2 in overweight category;2 the timeframe of 15–25 years of difference between the measurements (de Onis et al. study: 1990–2000 and PREFIT study: 2014–2015); and3 the sample characteristics measured (de Onis et al. study: developing and developed countries vs. PREFIT study: developed country).
A further exploratory analysis using the same categorization as de Onis et al.6 was conducted. This analysis showed a difference between PREFIT and the global situation in developed countries, that is, higher overweight/obesity prevalence in PREFIT (18.2 vs. 12.9%). The higher proportion of overweight/obesity in Spanish preschoolers than those of the global average is not surprising given the fact that obesity is unequally distributed in Europe, being preschoolers and adolescents from the south heavier compared to their peers from the north.7,29 Health-related factors such as higher levels of sedentary behaviour and lower levels of physical activity might explain these differences.29,30
It is important to note that, based on the WOF and WHO categories, our data showed differences (i.e. 2–15% points) between criteria. These differences have also been observed in previous studies.7,19 Differences between the most known international criteria (WOF and WHO) might be due to the creation (characteristics of the study sample measured, countries evaluated, and sample sizes) and definition of the weight status categories. In this sense, although we cannot express our preference for one of the criteria, we see some advantages on using the BMI cut-offs provided by the WOF: (1) these cut-points are linked to the well-accepted BMI cut-points in adults for defining underweight, normal weight, overweight, and obesity (i.e. 18.5, 25, and 30 kg/m2) and (2) it provides the opportunity to study different degrees of obesity (mild, severe, and the recently published morbid obesity cut-offs).20 In contrast, WHO cut-off defines obesity as one group, without degrees of severity. We consider that analysing different degrees of obesity is a novel result in our study, where we observed that about 1.3% of the study sample presented morbid obesity at preschool ages, and 2.5% of the children were either severe or morbid obese. Indeed, considering the whole population in Spain from 3 to 5 years old, 1.3% with morbid obesity would represent more than 14,000 preschool children. Thus, considering severe and morbid obesity together, this figure would increase up to ~30,000.31 This result is crucial, since it is well known that severe and morbid obesity are among the most pathogenic conditions.
In addition, obesity at this age tracks into adulthood, and obesity-related non-communicable diseases such as cardiovascular diseases, diabetes, physical, and mental problems might appear in adulthood.32 For example, longitudinal studies showed that overweight/obesity status in adolescents was strongly associated with increased mortality in adulthood due to cardiovascular diseases or other obesity-related risk factors.33 In addition, it has been reported that the risk of cardiovascular disease mortality increased by 7% for every 2 additional years lived with obesity.34 For this reason, early prevention of excess of weight, particularly obesity in preschool ages, is a major public health aim worldwide.
Sex- and age-specific reference standards
Available information providing sex- and age-specific anthropometric reference standards in preschool children are limited to few studies.16,18 Moreover, due to the differences in the applied methodologies (different inclusion or exclusion criteria of the study sample or the anthropometric tests used), our results are not fully comparable with other studies.
Overall weight and height values were slightly higher in boys compared to girls, whereas no differences were observed in BMI. The trend of the weight and height growth curves was practically similar for boys and girls. In comparison with the data provided in previous studies in 5-year-old children, preschoolers from Spain were approximately 1 kg heavier (50th percentile: 19.8 and 19.6 for boys and girls, respectively) compared to those peers measured by the WHO,3 and about 0.5 kg in comparison with Colombian counterparts.15 However, taking together the WHO and Colombian reference data in 5 year olds, we observed that Spanish preschool children were slightly taller than those who belonged to the WHO data (differences ranged from 0.5 to 1 cm)3 and Colombian preschoolers (differences ranged from 1.5 to 1.9 cm).15
Our study provides an estimate of the rate of growths. For the 50th percentile curve of 3 to 6 year olds, the 1-year increase is between 2 and 3 kg for weight and approximately 7 cm for height. In this period of life, preschool children experience many physiological and developmental changes, and thus the reference standards were provided every 0.025 year steps (every 9 days/1.5 week of age approximately). BMI showed a slightly different pattern for boys and girls. In girls, the 50th percentile curve showed a plateau effect across all age groups. In boys, although changes were not remarkably different, BMI started declining at the age of 3 years and rose up to the starting point at the age of 6 years. Boys also showed a plateau effect between the ages of 4 and 5.5 years old. It is also important to note the J-curve trend depicted in the highest percentiles (95th and 99th percentiles) of the boys’ BMI. Particularly, the peak of adiposity rebound was found at the age of 4 years in the 99th percentile for boys. Similar ages for adiposity rebound were observed in the WHO (4 years old)3 and Colombian reference standard (5 years old).15 In girls, neither the curves nor the reference data depicted a clear pattern in the highest percentiles to detect the age for adiposity rebound. It is of interest to highlight the relevance of the identification of critical periods for the development of childhood obesity for targeting prevention measures, given the negative consequences of an early adiposity rebound for obesity (e.g. impaired glucose tolerance and diabetes) in adults.35,36
Waist circumference is a well-known estimate of abdominal fat in adults, but little has been studied in children in this regard.18 In this sense, Brambilla et al.37 assessed the association between waist circumference and visceral and subcutaneous abdominal adipose tissue measured by magnetic resonance imaging in children from 7 to 16 years old. The researchers concluded that waist circumference can be a good predictor of abdominal adiposity in children and adolescents. Our results showed a similar curve trend between sexes with slightly higher values in girls than in boys. Likewise, waist circumference increased with age. Based on the 50th percentile curve, we can observe that differences between years were about 0.3 and 0.6 cm per year for boys and girls, respectively. Nagy et al.18 established percentile reference curves for European children from 2.0 to 10.9 years old based on the IDEFICS study, which provided approximately the same trend between years (differences around 0.7 cm). It also showed higher waist circumference in girls than in boys. However, these results cannot be compared with our results since overweight and obese children were excluded,18 hence not representing the whole population.
The same patterns in boys and girls were observed for both waist-to-height ratio and waist circumference. In contradiction to the waist circumference percentile curves, the waist-to-height ratio decreased as age increased. Although we cannot directly compare our percentile curves with the curves from the IDEFICS study since the eligibility criteria were different, it is interesting to mention that the results depicted the same trend. Moreover, our study could contribute to the creation of international standards, for instance, for waist circumference and waist-to-height ratio in order to define abdominal obesity by connecting the percentile curves to adults’ cut-points as it was done for BMI by Cole and Lobstein.2
This study provides several contributions to the existing literature the following information: (1) we provide the prevalence of Spanish preschool children across weight status categories based on well-known and most-frequently used criteria (WOF and WHO). More specifically, we provide, for the first time (not only in Spain, but also worldwide), severe and morbid obesity rates in preschool children from a large geographically distributed sample of preschoolers; and (2) we provide age- and sex-specific anthropometric reference standards by increments of trimesters of life, which are needed for children from 3 to 5 years old in whom growth is extremely fast with dramatic changes (we provide also a calculator to automatically compare these reference data). Likewise, the present anthropometric reference standards enable other researchers or professionals to classify preschool children into sex- and age-specific percentiles. In line with this assumption, an excel-based calculator will be available at our group’s website. With this tool, researchers or practitioners can simply copy and paste sex, age, and the result of the anthropometric tests, and the calculator will indicate which percentile belongs to the entered anthropometric value compared with the reference data presented in this article. The calculator will work for entering either the data of one child or copying and pasting columns from a data set, for instance, of 2500 subjects (temporally available for submission purposes at Dropbox: https://www.dropbox.com/sh/les8w15j03md1fj/AADID9TTKRql9EoND_tUQzdra?dl=0). Once the paper is accepted for publication, it will be permanently and publically available at PROFITH webpage: http://profith.ugr.es/recursos/prefit.
Limitations and strengths
A limitation of this study is the lack of other adiposity markers (e.g. fat mass, fat free mass) accurately measured with gold standard methods. The main strengths of our study are the relatively large sample size in preschool children geographically distributed in Spain, the prevalence reported in all obesity categories, the sex- and age-specific anthropometric standards, the derivation of the percentile curves using GAMLSS, and the standardization of measurements across all the centres involved.
In conclusion, our results show a high prevalence of overweight/obesity in preschool Spanish children (WOF: 21% and WHO: 35%) being 6% of them obese. It is of concern that at these very early ages 2.5% of children were severe/morbid obese (1.2% severe + 1.3% morbid). Likewise, the prevalence of underweight was slightly lower than obesity in preschoolers (i.e. 3–5 vs. 6%, respectively). Moreover, we provide sex- and age-specific anthropometric reference standards in preschoolers between the ages of 3 and 5 years old, which will allow a better interpretation of anthropometric assessment in Spanish preschool children. These reference values could help paediatricians to evaluate weight status and track monitor growth at early ages, and thus prevent overweight and obesity over time in Spanish preschool children.
References
Mayer, M. et al. Weight and body mass index (BMI): current data for Austrian boys and girls aged 4 to under 19 years. Ann. Hum. Biol. 42, 45–55 (2015).
Cole, T. J. & Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 7, 284–294 (2012).
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 450, 76–85 (2006).
Ahrens, W. et al. Prevalence of overweight and obesity in European children below the age of 10. Int. J. Obes. (2005) 38(Suppl. 2), S99–S107 (2014).
World Health Organization. Global Strategy on Diet, Physical Activity and Health (2016). http://www.who.int/dietphysicalactivity/childhood/en/. Accessed 31 Aug 2017.
de Onis, M., Blossner, M. & Borghi, E. Global prevalence and trends of overweight and obesity among preschool children. Am. J. Clin. Nutr. 92, 1257–1264 (2010).
Cadenas-Sanchez, C. et al. Prevalence of overweight/obesity and fitness level in preschool children from the north compared with the south of Europe: an exploration with two countries. Pediatr. Obes. 11, 403–410 (2015).
Bluher, S. et al. Age-specific stabilization in obesity prevalence in German children: a cross-sectional study from 1999 to 2008. Int. J. Pediatr. Obes. 6, e199–e206 (2011).
Olds, T. et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int. J. Pediatr. Obes. 6, 342–360 (2011).
Ortega, F. B., Ruiz, J. R. & Labayen I. Trends in the prevalence of morbid obesity in Australian children and adolescents from 1985 to 2008: what do we know about? Int. J. Obes. 35, 1332–1333 (2005).
Wake, M. et al. Morbidity patterns among the underweight, overweight and obese between 2 and 18 years: population-based cross-sectional analyses. Int. J. Obes. 37, 86–93 (2005).
de Onis, M., Blossner, M., Borghi, E., Frongillo, E. A. & Morris, R. Estimates of global prevalence of childhood underweight in 1990 and 2015. JAMA 291, 2600–2606 (2004).
Rito, A. et al. Prevalence of obesity among Portuguese children (6-8 years old) using three definition criteria: COSI Portugal, 2008. Pediatr. Obes. 7, 413–422 (2012).
de Ruiter, I., Olmedo-Requena, R., Sanchez-Cruz, J. J. & Jimenez-Moleon, J. J. Trends in child obesity and underweight in Spain by birth year and age, 1983 to 2011. Rev. Esp. Cardiol. 70, 646–655 (2017).
Duran, P. et al. Colombian reference growth curves for height, weight, body mass index and head circumference. Acta Paediatr. 105, e116–e125 (2016).
Wells, J. C. et al. Body-composition reference data for simple and reference techniques and a 4-component model: a new UK reference child. Am. J. Clin. Nutr. 96, 1316–1326 (2012).
Moreno, L. A. et al. Body fat distribution reference standards in Spanish adolescents: the AVENA Study. Int. J. Obes. 31, 1798–1805 (2007).
Nagy, P. et al. Percentile reference values for anthropometric body composition indices in European children from the IDEFICS study. Int. J. Obes. 38(Suppl. 2), S15–S25 (2014).
Ahrens, W. et al. Metabolic syndrome in young children: definitions and results of the IDEFICS study. Int. J. Obes. (2005) 38(Suppl. 2), S4–S14 (2014).
Bervoets, L. & Massa, G. Defining morbid obesity in children based on BMI 40 at age 18 using the extended international (IOTF) cut-offs. Pediatr. Obes. 9, e94–e98 (2014).
World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development (World Health Organization, Geneva, 2006).
Glaz, J. & Sison, C. P. Simultaneous confidence intervals for multinomial proportions. J. Stat. Plan Inference 82, 251–262 (1997).
Signorell, A et al. DescTools: Tools for descriptive statistics. R package version 0.99.26 (2018).
Rigby, R. A. & Stasinopoulos, D. M. Generalized additive models for location, scale and shape. J. R. Stat. Soc. Ser. C 54, 507–554 (2005).
van Buuren, S. & Fredriks, M. Worm plot: a simple diagnostic device for modelling growth reference curves. Stat. Med. 20, 1259–1277 (2001).
Intemann, T. P. H., Herrmann, D., Ahrens, W., Pigeot, I. in: Analysis of Large and Complex Data. Studies in Classification, Data Analysis, and Knowledge Organization (eds Wilhelm, A. F. & Kestler, H. A.) 385–394 (Springer International Publishing, Heidelberg, 2016).
Team R. C. [Internet]. R.: A Language and Environment for Statistical Computing. https://www.R-project.org/.
Gulias-Gonzalez, R. et al. Excess of weight, but not underweight, is associated with poor physical fitness in children and adolescents from Castilla-La Mancha, Spain. Eur. J. Pediatr. 173, 727–735 (2014).
Ortega, F. B. et al. Health inequalities in urban adolescents: role of physical activity, diet, and genetics. Pediatrics 133, e884–e895 (2014).
Ruiz, J. R. et al. Objectively measured physical activity and sedentary time in European adolescents: the HELENA study. Am. J. Epidemiol. 174, 173–184 (2011).
Statistic NIo. Population Statistics by Age and Sex (2016). https://stats.oecd.org/index.aspx?DataSetCode=RPOP. Accessed 16 Sep 2016.
Lakshman, R., Elks, C. E. & Ong, K. K. Childhood obesity. Circulation 126, 1770–1779 (2012).
Twig, G. et al. Diabetes risk among overweight and obese metabolically healthy young adults. Diabetes Care 37, 2989–2995 (2014).
Abdullah, A. et al. The number of years lived with obesity and the risk of all-cause and cause-specific mortality. Int J. Epidemiol. 40, 985–996 (2011).
Rolland-Cachera, M. F., Deheeger, M., Maillot, M. & Bellisle, F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int J. Obes. 30(Suppl. 4), S11–S17 (2006).
Bornhorst, C. et al. Associations between early body mass index trajectories and later metabolic risk factors in European children: the IDEFICS study. Eur. J. Epidemiol. 31, 513–525 (2016).
Brambilla, P., et al. Crossvalidation of anthropometry against magnetic resonance imaging for the assessment of visceral and subcutaneous adipose tissue in children. Int. J. Obes. 30, 23–30 (2006).
Acknowledgements
We thank the participation of the preschoolers, parents, and teachers in this study. We are grateful to Ms. Carmen Sainz-Quinn for assistance with the English language. This work is part of a Ph.D. Thesis conducted in the Biomedicine Doctoral Studies of the University of Granada, Spain. The PREFIT project takes place owing to the funding of the Ramón y Cajal grant held by FBO (RYC-2011-09011). C.C.-S. is supported by a grant from the Spanish Ministry of Economy and Competitiveness (BES-2014-068829). E.G.A. and F.B.O. are supported by a grant from the Spanish Ministry of Science and Innovation (RYC-2014-16390 and RYC-2011-09011, respectively). C.A.-B., A.P.-B., and G.S.-D. are supported by the Spanish Ministry of Education (FPU13/03137, FPU15/05337, and FPU13/04365, respectively). Additional funding was obtained from the University of Granada, Plan Propio de Investigación 2016, Excellence actions: Units of Excellence; Unit of Excellence on Exercise and Health (UCEES) and by the Junta de Andalucia, Consejería de Conocimiento, Investigación y Universidades. In addition, funding was provided by the SAMID III network, RETICS, the PN I+D+I 2017-2021 (Spain), ISCIII-Sub-Directorate General for Research Assessment and Promotion, the European Regional Development Fund (ERDF) (RD16/0022, SOMM17/6107/UGR), the EXERNET Research Network on Exercise and Health in Special Populations (DEP2005-00046/ACTI), the University of the Basque Country (GIU14/21), and the University of Zaragoza (JIUZ-2014-BIO-08).
Author information
Authors and Affiliations
Consortia
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: C.C.-S., T.I., I.L., C.A.-B., J.S.-M., P.J.B., M.R.B.-V., A.P.-B., G.S.-D., P.P., G.V.-R., and F.B.O. Drafting the article or revising it critically for important intellectual content: C.C.-S., T.I., I.L., C.A.-B., J.S.-M., P.J.B., M.R.B.-V., A.P.-B., G.S.-D., P.P., G.V.-R., L.A.M., and F.B.O. Final approval of the version to be published: C.C.-S., T.I., I.L., C.A.-B., J.S.-M., P.J.B., M.R.B.-V., A.P.-B., G.S.-D., P.P., G.V.-R., L.A.M., and F.B.O.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
See Supplementary information for a complete list of the PREFIT project members.
Rights and permissions
About this article
Cite this article
Cadenas-Sanchez, C., Intemann, T., Labayen, I. et al. Prevalence of severe/morbid obesity and other weight status and anthropometric reference standards in Spanish preschool children: The PREFIT project. Pediatr Res 87, 501–510 (2020). https://doi.org/10.1038/s41390-019-0325-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0325-8