Abstract
Background
Approximately 10–20% of children with idiopathic nephrotic syndrome (NS) fail to respond to steroid therapy. NS is divided into steroid-sensitive NS (SSNS) and steroid-resistant NS (SRNS). Over 45 recessive and dominant genes have been found to be associated with SRNS and/or focal segmental glomerulosclerosis (FSGS).
Methods
Targeted sequencing of 339 candidate genes, expressed in glomerular filtration barrier or located in the signaling pathway of podocyte function, were sequenced by NGS in a cohort of total 89 Chinese Han children (29 sporadic SRNS, 33 sporadic SSNS, and 27 healthy).
Results
Two variants (WT1 p.R441X and NPHS2 p.G149V) were screened out as pathogenic mutations and 14 variants were likely pathogenic. Mutations of KIRREL2 (SRNS vs SSNS: 24.1% vs 3.0%, adjusted OR = 10.11, 95% CI: 1.56–198.66, P = 0.039) were significantly associated with the risk of pediatric sporadic SRNS. Besides, three pathogenic or likely pathogenic variants were identified in HP gene.
Conclusion
Two pathogenic mutations and 14 likely pathogenic mutations were discovered through targeted sequencing of 339 candidate genes. Two genes, HP and KIRREL2, as candidate genes, were first proposed to be associated with the risk of pediatric sporadic SRNS.
Similar content being viewed by others
Introduction
Idiopathic nephrotic syndrome (NS) is a common glomerular disease in children, occurring in 16 per 100,000 children1, and is characterized by massive proteinuria, hypoalbuminemia, hyperlipidemia, and edema at different levels. The first-line therapy for children with idiopathic NS is steroid treatment. Most children with idiopathic NS show a favorable long-term outcome when treated with glucocorticosteroid, although a number of them may experience steroid-dependent relapses2. Approximately 10–20% of children with idiopathic NS fail to respond to steroid therapy. Moreover, 30–40% of these patients will progress to end-stage renal disease (ESRD) within 10 years upon disease onset, and dialysis or renal transplantation will be the only treatments they can benefit from3. According to the patients’ responses to steroid therapy, NS is divided into steroid-sensitive NS (SSNS) and steroid-resistant NS (SRNS). Focal segmental glomerulosclerosis (FSGS) is the major disease subtype observed in patients with SRNS. Molecular genetic studies have revealed that a considerable proportion of patients with SRNS carried some gene mutations, leading to profound podocyte dysfunction, and these patients were usually also resistant to immunosuppressive agents4.
Currently, over 45 genes have been reported to be associated with SRNS and/or FSGS with autosomal dominant (AD), autosomal recessive (AR), X-linked dominant (XD), X-linked recessive (XR), or maternal modes of inheritance5,6, such as WT1 (AD), NPHS1 (AR), NPHS2 (AR), WDR73 (AR), XPO5 (AR), NXF5 (XR), COL4A5 (XD), and so on7,8,9,10. Almost all the patients with SRNS harboring pathogenic mutations would eventually suffer from renal failure. The incidence of genetic mutations in children with sporadic SRNS is estimated to be 20% in Caucasian, and the frequently mutated genes were NPHS2 and WT111. However, the prevalence of NPHS2 mutation is quite low in Asians12,13. Thus it suggests that the mutational spectrum varies significantly among different races and ethnicities. There are only few reports about mutation profiles of children with SRNS in China.
In this study, 339 genes expressed in glomerular filtration barrier or located in the signaling pathway of podocyte function were chosen to be interrogated by next-generation sequencing (NGS) in Chinese Han children with sporadic SRNS or SSNS. The aim of this study is to discover novel pathogenic mutations in Chinese Han children with sporadic SRNS.
Methods
Patients
Twenty-nine sporadic SRNS Chinese Han children, as well as 33 sporadic SSNS Chinese Han children worked as the disease control group, were recruited from Capital Institute of Pediatrics between 2011 and 2015. The inclusion criteria are: (1) non-consanguineous marriages with primary NS and (2) no family history of renal diseases. Twenty-seven healthy Chinese Han children without family history of renal diseases or abnormal urinalyses checked by imaging examination were also included in this study.
The procedures were approved by the Ethics Committee of Capital Institute of Pediatrics. After receiving informed consent from, blood samples and comprehensive clinical data were collected and analyzed. NS was defined by the level of urinary protein excretion (≥50 mg/kg per 24 h) and the presence of hypoalbuminemia. Steroid resistance was defined by persistent proteinuria after 4 weeks of daily 1.5–2 mg/kg prednisone treatment (maximum dose 60 mg/day).
Targeted NGS and mutational analysis
Genomic DNA was extracted from patients’ peripheral blood leukocytes using the QIAamp DNA Blood Mini Kit (Qiagen, Shanghai, China) according to the manufacturer’s protocol. A set of probes were developed to capture the whole exons of 339 target genes (Table S1) (Roche). A portion of these genes have been demonstrated to express at glomerular filtration barrier including the fenestrated endothelial cell layer, the glomerular basement membrane (GBM), and the epithelial podocyte layer. The other portion of these genes may be involved in the signaling pathways of podocyte predicted by GeneCards, STRING, KEGG and other databases. Targeted sequencing was performed on the HiSeq 2500 platform (Illumina).
Low-quality reads, duplicate reads, and potential adaptor contaminations were removed from the primary data and reads were quality-trimmed. The unique reads were mapped to the human genome (hg19/GRCh37) using the BWA software (Burrows Wheeler Aligner http://sourceforge.net/projects/biobwa/). GATK software (https://software.broadinstitute.org/gatk/) was used to detect single-nucleotide mutations, small insertions, and deletions. The mutation effects on protein function were evaluated using SIFT (http://sift.jcvi.org/), PolyPhen-2 HDIV (http://genetics.bwh.harvard.edu/pph2/), and PolyPhen-2 HVAR (http://genetics.bwh.harvard.edu/pph2/).
Mutations will be filtered out from further analysis if meeting any of the following criteria:
-
1.
minor allele frequency >0.5% as shown in the public database, such as 1000 Genomes Project (1000 G) (http://www.1000genomes.org/), Exome sequencing project (ESP6500) (http://evs.gs.washington.edu/EVS/), and Exome Aggregation Consortium (ExAC) (http://exac.broadinstitute.org/).
-
2.
mutations in introns except the splicing site (±10 bp).
-
3.
synonymous mutations (not caused changes of amino acid sequence).
-
4.
at least two scores within the listed range: SIFT (score > 0.05), PolyPhen-2 HDIV (score ≤ 0.452), or PolyPhen-2 HVAR (score ≤ 0.446).
-
5.
mutations also detected in the healthy Chinese Han children.
All rare mutations were validated by Sanger sequencing. Direct sequencing of the purified PCR products was performed using ABI 310 Genetic Analyzer (Applied Biosystems). Sequence analysis was carried out using the Sequence Pilot software14.
Statistical analysis
Median, standard deviations, and range values were calculated for continuous variables. Chi-square (χ2) test, Fisher test, and t test of univariate analysis were performed to examine the relationship between diseases (SRNS, SSNS) and patients’ clinical pathological features. Associations between SRNS and patients’ gene mutations were further evaluated by multivariate logistic regression analysis. Adjusted odds ratio (OR) and 95% confidence interval (95% CI) were given. P values <0.05 (two-sided) were considered as statistically significant. All statistical analyses were performed with R 3.2.3 (http://www.r-project.org/).
Results
Clinical characteristics
The clinical characteristics of 29 sporadic SRNS children and 33 sporadic SSNS children are summarized in Tables S2 and S3. For 29 SRNS patients, the mean age of disease onset was 50.9 (SE: ±45.5) months. Renal biopsy revealed FSGS in 8 patients, mesangial proliferative glomerulonephritis (MsPGN) in 6 patients, and minimal-change nephrotic syndrome (MCNS) in 2 patients. There were 5 patients with chronic renal failure (CRF) and 3 patients with acute renal failure (ARF). The mean level of urine protein and serum albumin were 162.2 (SE: ±64.6) (mg/kg/d) and 14.7 (SE: ±4.8) (g/L), respectively. For 33 SSNS children who worked as the disease control group, patients’ age of disease onset ranged from 13 to 100 months, with a mean at the age of 46.4 (SE: ±25.6) months, and the mean time of remission was 9.2 (SE: ±4.7) days (Table 1). All patients with SRNS were treated with glucocorticoids combined with immunosuppressor, and high level of urine protein was reduced in 13 patients but not to the normal level (Table S2).
Identification and classification of variants in NS
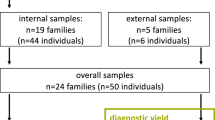
After a multistep filtration as illustrated in Fig. 1, 143 variants from the SRNS group and 135 variants from the SSNS group were selected as the candidate variants for subsequent analysis. After cross-checking against 143 variants from SSNS group, 128 SRNS-specific mutations were identified in 87 out of the 339 target genes. These mutations include 124 missense, 1 nonsense, 1 splice sites, 1 small deletion, and 1 small insertion. And 83 out of the 128 mutations (64.8%) are novel mutations, which have not been reported in the literatures. A detailed description of all these 128 mutations is listed in Table S4. These 128 exclusive mutations were further classified into three groups based on available evidence (Table 2).
Schematic visualization of the analytical workflow for this study. First, candidate mutations in the steroid-resistant nephrotic syndrome (SRNS) group and the steroid-sensitive nephrotic syndrome group were selected by a multistep filtration. Second, two kinds of analysis were performed to reveal genetic characteristics of Chinese children with SRNS
Two variants that met pathogenic criteria were regarded as pathogenic mutations for SRNS (Table 3). Notably, the truncating mutation in WT1 (p.R441X), previously reported as a pathogenic mutation causing Denys–Drash syndrome and Wilms’ tumor15,16,17, was found in patient I-3 with CRF. Furthermore, in patient I-26 with FSGS, we found a novel homozygous variant (p.G149V) in NPHS2, which is the most frequently mutated gene in SRNS.
Fourteen variants classified as likely pathogenic mutations were identified in 11 genes from 10 patients (Table 3). Among these likely pathogenic mutations, 11 were nonsynonymous variants that occurred in well-known SRNS-associated genes. Two variants p.R802W (novel) and p.R1464H, located in MYH9 gene that was known to cause Macrothrombocytopenia with sensorineural deafness, Epstein syndrome, Sebastian syndrome, and Fechtner syndrome, were found in a female patient with FSGS and ARF and a male patient with MCNS, respectively. A variant (p.E1109K) in LAMB2 causing AR Pierson syndrome was identified in two female patients with CRF and MsPGN, respectively. Furthermore, two novel homozygous variants in HP and RHOXF2B were detected in two patients. A female patient diagnosed as FSGS harbored a splicing site variant (c.1516+1G>A) in CD44 gene.
Analysis of the candidate genes related with the risk of SRNS
To evaluate the risk of genes mutated in SRNS patients in disease development, we collapsed information on all rare variants within a gene into a single dichotomous variable for each subject by indicating whether or not the subject has any rare variants within this gene. Fisher test was applied to compare the mutation frequency between the SRNS and the SSNS groups. The results demonstrated that children with SRNS had a higher chance to obtain mutations in KIRREL2 than in children with SSNS (SRNS vs SSNS: 24.1% vs 3.0%, OR = 10.18, 95% CI: 1.13–456.32, P = 0.021), and the mutations of ITGA2 were more likely to occur in SRNS children than in SSNS children (SRNS vs SSNS: 13.3% vs 0%, P = 0.043) (Fig. 2). However, the logistic multivariate analysis results indicated that only KIRREL2 mutations were more frequently observed to be significant in NS patients who were steroid-resistant (SRNS vs SSNS: 24.1% vs 3.0%, adjusted OR = 10.11, 95% CI: 1.56–198.66, P = 0.039) (Table 4).
As carrying pathogenic or likely pathogenic mutations, three genes (HP, RHOXF2B, CD44) were highly speculated to be associated with SRNS. We calculated the RVIS scores for each candidate gene in order to assess how well these genes tolerate functional variations (http://chgv.org/GenicIntolerance/). RVIS is a score that measures the ratio of any functional variation defined as missense, nonsense, and splice acceptor/donor variants and synonymous (neutral) variation residing in a single gene. The score is designed to rank genes in terms of whether they have any common functional genetic variation relative to the genome wide expectation, given the amount of apparently neutral variations a certain gene has. HP and ITGA2 may be intolerant, but KIRREL2 is probably more tolerant to functional variants in the general population (Table 5).
Discussion
In the present study, targeted sequencing of 339 candidate genes were sequenced by NGS in a cohort of total 89 Chinese Han children (29 sporadic SRNS, 33 sporadic SSNS, and 27 healthy), which is the most number of genes interrogated in a single study to date. The mean age of disease onset was 50.9 (SE: ±45.5) months in the cohort of 29 SRNS patients (15 males, 14 females) and 46.4 (SE: ±25.6) months in the cohort of 33 SSNS children (26 males, 7 females) as the disease control group.
We identified 128 exclusive mutations from 87 genes in all of the 29 sporadic SRNS children, including 124 missense, 1 nonsense, 1 splice sites, 1 small deletion, and 1 small insertion. And 84 out of the 128 variants (64.8%) were novel mutations. Among these 128 mutations, 15 mutations identified from 12 children with SRNS were located in well-known SRNS-related genes. The mutation rate is 40%, which was higher compared to the mutation rates described in previously studies with cohorts of Chinese SRNS children (28.3%18 and 31.7%19). Based on our selective criteria, 3 pathogenic mutations and 14 likely pathogenic mutations were achieved.
The HP gene encodes an acute phase-reactant tetrameric haptoglobin20. The major function of haptoglobin is to bind free plasma hemoglobin (Hb) in order to form a stable Hp–Hb complex. It prevents the Hb-induced oxidative tissue damage and the loss of iron in the kidneys21. Mutations in HP may cause ahaptoglobinemia or hypohaptoglobinemia22. Furthermore, an evidence yielded by a latest research revealed that the level of haptoglobin in the serum was markedly elevated in SRNS patients compared to SSNS patients23. But the relationship between the mutations in HP and the occurrence of SRNS remains inconclusive. The novel homozygous mutation in HP p.K320N was found in patient I-14 with MsPGN but showing a normal renal function. And the HP p.R227P mutation was detected in patient I-27 with FSGS and acute renal failure. Even though no mutations in gene HP were identified from the SSNS group, the statistical analysis implicated that there was no significant link between HP gene and sporadic SRNS (P = 0.222). The reason is probably that the sample size in this study cohort is relative small.
The KIRREL2 gene also named as Neph3 or filtrin encodes a protein with five Ig domains. KIRREL2 belongs to a member of the NEPH family that interacts with podocin, a glomerular slit diaphragm protein24. Interestingly, a recent study showed the evidence of Neph3 in preventing the glomerular protein leakage, as the decreased expression of Neph3 in renal biopsies are found to be associated with podocytopathy and protein-losing nephropathy25. In addition, nonsynonymous variants in KIRREL2 gene were also proven to cause the nephrotic syndrome in dogs26. Moreover, a recent investigation indicated an association of the V353M variant in KIRREL2 with the disease severity of primary hematuric glomerulopathies. Functional studies showed that Neph3 homodimerization and Neph3–Nephrin heterodimerization were severely compromised by this mutation. Thus the variant V353M acts as a negative modifier of primary glomerular hematuria27. In this study, the statistical analysis revealed that children with sporadic SRNS had a higher chance to obtain mutations in KIRREL2 than in children with sporadic SSNS (SRNS vs SSNS: 24.1% vs 3.0%, adjusted OR = 10.11, 95% CI: 1.56–198.66, P = 0.039). Further investigations will be necessary in order to inspect whether the mutations in gene KIRREL2 are related to pediatric SRNS. The gene ITGA2 encodes the alpha subunit of a transmembrane receptor for collagens and related proteins, named alpha-2 integrin, which forms a heterodimer with a beta subunit and mediates the adhesion of platelets and other cell types to the extracellular matrix28. Alpha-2 integrin was shown to involve in cell adhesion and also participated in cell-surface-mediated signaling29. Loss of alpha-2 integrin was associated with bleeding disorder platelet type 9 and antibodies against this protein were found in several immune disorders, including neonatal alloimmune thrombocytopenia30,31. ITGA2-deficient mice had moderate level of proteinuria and showed enhanced glomerular and tubulointerstitial matrix deposition and fibrosis. The cell–matrix interaction via collagen receptors (DDR1, ITGA2, COL4A3) regulated GBM maturation and matrix accumulation, which were crucial for the maintenance of normal GBM architecture and function32,33. Besides, the pediatric NS is caused by the abnormal structure and dysfunction of the glomerular filtration barriers, including the fenestrated endothelial cell layer, the GBM, the epithelial podocyte layer, and the mesangial cells. However, the mutations in ITGA2 were found to be not significantly associated with the risk of SRNS by the logistic multivariate analysis in the present study. Future studies should concentrate on examining the role of ITGA2 in renal disease, especially in pediatric SRNS.
The MYH9 gene encodes the nonmuscle myosin heavy chain IIA (myosin II), a cytoskeletal contractile protein that is abundantly expressed in the kidney, mainly in the glomerulus and peritubular vessels34. Mutations in MYH9 gene are related to a number of rare autosomal-dominant disorders, such as May–Hegglin disease, Sebastian syndrome, Fechtner syndrome, and Epstein syndrome. Patients with these diseases often showed symptoms of congenital macrothrombocytopenia, polymorphonuclear inclusion bodies, proteinuria, chronic kidney disease progressing toward ESRD, sensorineural deafness, and presenile cataracts35. It has been reported that the p.E1841K mutation, one of common missense mutations in MYH9, resulted in the alteration of podocyte cytoskeletal structure and caused podocytes to be more susceptible to the injury of a damaging stimulus36. In this study, two heterozygous single-nucleotide polymorphisms (SNPs), MYH9 p.R1464H and MYH9 p.R802W (novel), were detected in patient I-23 with MCNS and patient I-27 with FSGS and acute renal failure, respectively. Furthermore, the blood routine examination of patients I-23 and I-27 did not show platelet abnormalities. It suggests that these two SNPs may contribute to the induction of sporadic SRNS and are likely pathogenic. Unfortunately, the parental DNA was not available in this study and thus de novo mutations were not identified in these pediatric patients with SRNS.
In summary, this study presents a clear mutation panoramagram of 339 genes based on the cohort of total 89 Chinese Han children (29 sporadic SRNS, 33 sporadic SSNS, and 27 healthy) and reveals the mutational spectrum and novel candidate genes in Chinese Han children with SRNS. Based on our selective criteria, 2 pathogenic mutations and 14 likely pathogenic mutations were discovered. And two candidate genes, HP and KIRREL2, were first proposed to be associated with the induction of pediatric sporadic SRNS. Our results demonstrated that screening for pathogenic mutations in children with idiopathic NS might be helpful for early disease diagnosis, and the unnecessary use of renal biopsy and steroid treatment for pediatric patients could be prevented.
References
Gipson, D. S. et al. Management of childhood onset nephrotic syndrome. Pediatrics 124, 747–757 (2009).
Hahn, D., Hodson, E. M., Willis, N. S. & Craig, J. C. Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst. Rev. 3, CD001533 (2015).
Mekahli, D. et al. Long-term outcome of idiopathic steroid resistant nephrotic syndrome: a multicenter study. Pediatr. Nephrol. 24, 1525–1532 (2009).
Giglio, S. et al. Heterogeneous genetic alterations in sporadic nephrotic syndrome associate with resistance to immunosuppression. J. Am. Soc. Nephrol. 26, 230–236 (2015).
Joshi, S., Andersen, R., Jespersen, B. & Rittig, S. Genetics of steroid-resistant nephrotic syndrome: a review of mutation spectrum and suggested approach for genetic testing. Acta Paediatr. 102, 844–856 (2013).
Brown, E. J., Pollak, M. R. & Barua, M. Genetic testing for nephrotic syndrome and FSGS in the era of next-generation sequencing. Kidney Int. 85, 1030–1038 (2014).
Lovric, S., Ashraf, S., Tan, W. & Hildebrandt, F. Genetic testing in steroid-resistant nephrotic syndrome: when and how? Nephrol. Dial. Transplant. 31, 1802–1813 (2016).
Tasic, V., Gucev, Z. & Polenakovic, M. Steroid resistant nephrotic syndrome-genetic consideration. Pril. (Makedon. Akad. Nauk. Umet. Odd. Med. Nauk.) 36, 5–12 (2015).
Becherucci, F. et al. Lessons from genetics: is it time to revise the therapeutic approach to children with steroid-resistant nephrotic syndrome? J. Nephrol. 29, 543–550 (2016).
Ha, T.-S. Genetics of hereditary nephrotic syndrome: a clinical review. Korean J. Pediatr. 60, 55–63 (2017).
Sadowski, C. E. et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J. Am. Soc. Nephrol. 26, 1279–1289 (2015).
Maruyama, K. et al. NPHS2 mutations in sporadic steroid-resistant nephrotic syndrome in Japanese children. Pediatr. Nephrol. 18, 412–416 (2003).
Li, J. et al. WT1 gene mutations in Chinese children with early onset nephrotic syndrome. Pediatr. Res. 68, 155–158 (2010).
Petrovski, S., Wang, Q., Heinzen, E. L., Allen, A. S. & Goldstein, D. B. Genic intolerance to functional variation and the interpretation of personal genomes. PLoS Genet. 9, e1003709 (2013).
Little, M. H. et al. Zinc finger point mutations within the WT1 gene in Wilms tumor patients. Proc. Natl. Acad. Sci. USA 89, 4791–4795 (1992).
Little, M. H. et al. Evidence that WT1 mutations in Denys-Drash syndrome patients may act in a dominant-negative fashion. Hum. Mol. Genet. 2, 259–264 (1993).
Schumacher, V. et al. Correlation of germ-line mutations and two-hit inactivation of the WT1 gene with Wilms tumors of stromal-predominant histology. Proc. Natl. Acad. Sci. USA 94, 3972–3977 (1997).
Wang, F. et al. Spectrum of mutations in Chinese children with steroid-resistant nephrotic syndrome. Pediatr. Nephrol. 32, 1181–1192 (2017).
Wang, Y. et al. Mutation spectrum of genes associated with steroid-resistant nephrotic syndrome in Chinese children. Gene 625, 15–20 (2017).
Haugen, T. H., Hanley, J. M. & Heath, E. C. Haptoglobin: a novel mode of biosynthesis of a liver secretory glycoprotein. J. Biol. Chem. 256, 1055–1057 (1981).
Asleh, R. et al. Genetically determined heterogeneity in hemoglobin scavenging and susceptibility to diabetic cardiovascular disease. Circ. Res. 92, 1193–1200 (2003).
Teye, K. et al. A-61C and C-101G Hp gene promoter polymorphisms are, respectively, associated with ahaptoglobinaemia and hypohaptoglobinaemia in Ghana. Clin. Genet. 64, 439–443 (2003).
Wen, Q. et al. Proteomic profiling identifies haptoglobin as a potential serum biomarker for steroid-resistant nephrotic syndrome. Am. J. Nephrol. 36, 105–113 (2012).
Sellin, L. et al. NEPH1 defines a novel family of podocin interacting proteins. FASEB J. 17, 115–117 (2003).
Ihalmo, P. et al. Expression of filtrin in human glomerular diseases. Nephrol. Dial. Transplant. 22, 1903–1909 (2007).
Littman, M. P., Wiley, C. A., Raducha, M. G. & Henthorn, P. S. Glomerulopathy and mutations in NPHS1 and KIRREL2 in soft-coated Wheaten Terrier dogs. Mamm. Genome 24, 119–126 (2013).
Voskarides, K. et al. A functional variant in NEPH3 gene confers high risk of renal failure in primary hematuric glomerulopathies. Evidence for predisposition to microalbuminuria in the general population. PLoS ONE 12, e0174274 (2017).
Inoue, O., Suzuki-Inoue, K., Dean, W. L., Frampton, J. & Watson, S. P. Integrin alpha2beta1 mediates outside-in regulation of platelet spreading on collagen through activation of Src kinases and PLCgamma2. J. Cell Biol. 160, 769–780 (2003).
Kim, S.-H., Turnbull, J. & Guimond, S. Extracellular matrix and cell signalling: the dynamic cooperation of integrin, proteoglycan and growth factor receptor. J. Endocrinol. 209, 139–151 (2011).
Lane-Serff, H., Sun, Y., Metcalfe, P. & Wright, G. J. Expression of recombinant ITGA2 and CD109 for the detection of human platelet antigen (HPA)-5 and -15 alloantibodies. Br. J. Haematol. 161, 453–455 (2013).
Peterson, J. A. et al. New low-frequency platelet glycoprotein polymorphisms associated with neonatal alloimmune thrombocytopenia. Transfusion 50, 324–333 (2010).
Girgert, R. et al. Integrin α2-deficient mice provide insights into specific functions of collagen receptors in the kidney. Fibrogenesis Tissue Repair 3, 19 (2010).
Rubel, D. et al. Collagen receptors integrin alpha2beta1 and discoidin domain receptor 1 regulate maturation of the glomerular basement membrane and loss of integrin alpha2beta1 delays kidney fibrosis in COL4A3 knockout mice. Matrix Biol. 34, 13–21 (2014).
Arrondel, C. et al. Expression of the nonmuscle myosin heavy chain IIA in the human kidney and screening for MYH9 mutations in Epstein and Fechtner syndromes. J. Am. Soc. Nephrol. 13, 65–74 (2002).
Galeano, D., Zanoli, L., L’Imperio, V., Fatuzzo, P. & Granata, A. Renal diseases related to MYH9 disorders. G. Ital. Nefrol. 34, 40–57 (2017).
Cechova, S. et al. MYH9 E1841K mutation augments proteinuria and podocyte injury and migration. J. Am. Soc. Nephrol. 29, 155–167 (2018).
Acknowledgements
We are indebted to the patients and families for participating in this study and to the clinical teams involved in recruitment and sample collection. This work was supported by the National Natural Science Foundation of China (81100504, 81570649).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Li, J., Wang, L., Wan, L. et al. Mutational spectrum and novel candidate genes in Chinese children with sporadic steroid-resistant nephrotic syndrome. Pediatr Res 85, 816–821 (2019). https://doi.org/10.1038/s41390-019-0321-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0321-z