Abstract
Background
Despite high initiation rates for mother’s own milk (MOM) provision, MOM feeding at discharge from the neonatal intensive care unit (NICU) drops precipitously and reveals a racial/ethnic disparity. This study sought to identify factors that (1) predict MOM feeding at NICU discharge, and (2) mediate racial/ethnic disparity in MOM feeding at discharge.
Methods
Secondary analysis of prospective cohort study of 415 mothers and their very low birth weight infants. Variables were grouped into five categories (demographics, neighborhood structural, social, maternal health, and MOM pumping). Significant predictors from each category were entered into a multivariable logistic regression model.
Results
Although 97.6% of infants received MOM feedings, black infants were significantly less likely to receive MOM feeding at discharge. Positive predictors were daily pumping frequency, reaching pumped MOM volume ≥500 mL/day by 14 days, and maternal age. Negative predictors were low socioeconomic status (SES) and perceived breastfeeding support from the infant’s maternal grandmother. Low SES, maternal age, and daily pumping frequency mediated the racial/ethnic differences.
Conclusions
Multiple potentially modifiable factors predict MOM feeding at NICU discharge. Importantly, low SES, pumping frequency, and maternal age were identified as the mediators of racial and ethnic disparity. Strategies to mitigate the effects of modifiable factors should be developed and evaluated in future research.
Similar content being viewed by others
Introduction
In the United States, black women give birth to very low birth weight (birth weight <1500 g, VLBW) infants 2.6 times more often than non-Hispanic white (white) women,1 yet significantly fewer black premature infants receive mother’s own milk (MOM, not including donor milk) compared to non-black premature infants.2 This disparity increases the risk of short- and long-term complications of prematurity for black VLBW infants,3,4 because MOM feedings reduce the risk of these serious and costly complications in a dose–response manner. Mothers also receive a dose-related benefit of MOM feeding, with longer periods of lactation associated with reduced risks of health conditions including breast and ovarian cancer, diabetes, hyperlipidemia, hypertension, myocardial infarction, and premature death,5 all of which disproportionately affect black women.6
These findings have informed the American Academy of Pediatrics (AAP) recommendation that all infants, including VLBW infants, receive exclusive MOM feedings for the first 6 months of life. As a result, the initiation rates of MOM provision have increased in many institutions,7 and the racial and ethnic disparities in initiation rates have been significantly reduced or even abolished in some neonatal intensive care units (NICUs), although disparities in sustaining MOM provision remain.8 While many mothers of VLBW infants do not maintain MOM provision through to NICU discharge, significantly fewer black VLBW infants receive MOM feedings at NICU discharge (MOM at DC) compared to non-black infants. This disparity occurs despite high initiation rates and a goal to continue MOM provision after NICU discharge.9,10 While the pattern of high initiation but low maintenance rates for MOM provision may appear similar to black mothers of healthy term infants, it is likely that the underlying causes for mothers of VLBW infants differ because these mothers are breast pump-dependent, experience incomplete mammary gland development, and frequently have health problems that predispose them to preterm delivery and delayed lactogenesis.11,12 Although numerous studies have attempted to predict MOM feeding at discharge,2,9,13,14,15 limited research has targeted the racial disparity in this outcome.13 Our objectives were to identify specific factors that predict MOM feeding at NICU discharge for VLBW infants, and to identify specific factors that mediate racial and ethnic disparity in MOM feeding at NICU discharge.
Methods
This study is a secondary analysis of a prospective cohort study of 430 VLBW infants and their mothers who were enrolled between February 2008 and December 2012 at Rush University Medical Center (RUMC) that demonstrated high-dose MOM feedings reduced the risk and associated costs of potentially preventable morbidities in VLBW infants.3 All VLBW infants were eligible unless they met the exclusion criteria (birth gestational age (GA) >35 weeks, NICU admission at >24 h of age, initiation of feedings >14 days of life, major congenital anomalies or chromosomal disorders, and maternal conditions that precluded MOM provision). For multiple gestations, one infant was randomly selected for inclusion. Of eligible infants, 93% were enrolled in this cohort study. Prospectively collected data for 415 mother–infant dyads were used for this secondary analysis, after removing 15 mother–infant dyads as detailed in the cohort diagram (Fig. 1). All mothers received standardized lactation care by employed NICU-specific breastfeeding peer counselors, all of whom are former NICU parents and represent the racial/ethnic composition of the NICU families. Mothers initiated MOM removal with a hospital-grade breast pump, were able to rent a subsidized hospital-grade pump for in-home use, and had access to a complimentary taxi service to weekly NICU lactation meetings. The RUMC Institutional Review Board approved this secondary analysis and the original cohort study, and signed informed consent was obtained from mothers for themselves and their infants for the original cohort study.
Data were prospectively collected using questionnaires and maternal and infant medical records. Maternal characteristics included: age, marital status, self-stated race/ethnicity (non-Hispanic black (black), non-Hispanic white (white), Hispanic, and Asian), low SES (yes/no for maternal eligibility for Special Supplemental Nutrition Program for Women, Infants, and Children (WIC)), highest education level, number of children in household, and home address. Six Asian mothers, who constituted a small proportion of subjects, were grouped with white mothers because of similar sociodemographic characteristics and lack of significant differences in pumping frequency, cumulative MOM volume through 2 weeks, and rate of MOM at DC between Asian and white mothers (data not shown). Infant characteristics included sex, birth weight (BW), GA, small for GA status, and daily intake (mL) of MOM and formula from birth to NICU discharge. During the study years, donor human milk was not available for routine use and the hospital did not have Baby Friendly Hospital designation. MOM feeding at the time of infant discharge was classified based on feedings received on the last full day of hospitalization before NICU discharge: any MOM (exclusive MOM or some MOM and some formula) and no MOM (only formula). Addition of bovine fortifier did not influence categorization as exclusive MOM because standard nutritional practice in the study NICU was to discontinue fortification several days prior to discharge, thus infants received unfortified MOM at NICU discharge.
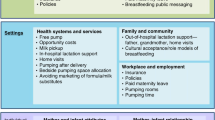
Data were categorized according to the study conceptual model (Fig. 2), in which the significant factors from each category are noted in bold. These five categories of factors included both NICU and non-NICU factors that have been previously associated with lactation outcomes or are plausible for a breast pump-dependent mother with a VLBW infant and a prolonged NICU hospitalization. Social factors16 included maternal education,17 maternal smoking,17,18 maternal perception of support and non-support for breastfeeding and pumping (both as a dichotomous variable of presence of support and as identification of specific supportive/non-supportive person),19 baseline occupational status (unemployed, employed, student) and plan to return to work or school,8 first maternal MOM feeding goal after infant’s NICU admission (any MOM or none),10,14 and previous MOM feeding or formula feeding experience.19
Neighborhood structural factors20 were assessed by linking home addresses to communities and census tracts using ArcGIS version 10.2.2 (Esri, Redlands, CA, USA). Factors included distances to NICU,15 public transportation, nearest WIC office, and nearest breastfeeding support as a marker of the neighborhood breastfeeding culture,21 access to a car,15 concentrated disadvantage,21,22 and violent crime for the 2010 calendar year.22 Maternal health factors23 included pre-pregnancy body mass index,11 diabetes mellitus,24 hypertension and/or pre-eclampsia,17 mode of delivery,12 and multiple gestation. MOM pumping factors included type of breast pump (hospital grade vs. portable electric vs. hand expression).7 The remaining factors were collected using prospective pumping records maintained by a subset of mothers (n = 205; 49%): time to pumping initiation after delivery,14 daily pumping frequency,14,25 minutes spent pumping daily, and daily pumped MOM volume.14 Coming to volume (CTV) was defined as producing a total pumped MOM volume ≥500 mL/day for at least one 24 h period during the first 14 days postpartum.23 Maternal demographics included maternal age, number of children in household, low SES defined as maternal eligibility for WIC, and marital status.8,9,17
Handling of missing data: Nearly half of participants (n = 202; 49%) had complete data for all variables in the present analyses. Of the 213 participants with missing data, the majority (n = 185; 87%) were missing only MOM pumping records because maintenance of the pumping record was encouraged but not mandatory for study participation (Supplemental Table S1). Characteristics of mothers with and without missing data were compared by χ2 and independent t tests (Supplemental Table S2). Missing data were imputed using chained equations26 to create 50 imputed datasets. Fifty imputations were selected because the fraction of missing information for the number of days pumped was 0.41.27 All variables in Supplemental Table S1 were included in the imputation model to satisfy the assumption of missing at random. Estimates from the imputed datasets were then pooled to account for within- and between-dataset variation. Analyses were performed using the SAS software (SAS Institute, Inc., Cary, NC, USA).
Statistical analysis
Descriptive statistics included frequencies, percentages, and mean ± SD. Bivariate analyses were conducted using χ2 and one-way analysis of variance. Post hoc pairwise analyses were conducted for variables that differed by race/ethnicity using Bonferroni adjustment to account for three pairwise tests. For each category of factors, multivariable binary logistic regression analyses adjusting for important infant variables (GA and 5 min APGAR score as an acuity marker) were previously conducted16,20,23 to narrow the candidate factors from the five categories into the following significant predictors of MOM feeding at discharge: maternal education, breastfeeding support from mother’s mother, MOM feeding goal, maternal smoking, access to a car, hypertension and/or pre-eclampsia, multiple gestation, mean daily pumping frequency, CTV, maternal age, number of children in household, SES, and marital status. These significant predictors from each category and infant covariates were entered into a multivariable logistic regression model (Fig. 2) using a two-step process intended to reduce the number of variables in the final model. In Step 1, separate logistic regression models were estimated for each of the individual factors (social, neighborhood structural, maternal health and infant, and MOM pumping) controlling for demographics. In Step 2, demographic factors and only those individual factors that were significant at p < 0.15 were included. Type 1 error was set at p < 0.05.
Mediation analyses were then conducted to identify specific factors that mediate and may partially explain the racial/ethnic disparity in MOM feeding at discharge. We identified candidate mediators that met two criteria: (a) significantly related to race/ethnicity (see Table 1), and (b) significantly predicted MOM feeding at discharge in the final multivariate model (see Table 2). All candidate mediators were then included in a multiple mediator model estimated using MPlus.28 Two binary dummy codes were utilized for race/ethnicity (white vs. black and Hispanic vs. black). A robust weighted least squares estimator allowed for estimation of indirect effects for binary and continuous mediators.28 Bootstrap confidence intervals using 5000 samples were calculated for all parameter estimates to account for the asymmetric standard errors of the indirect effects. Separate models were estimated for each of the 50 imputed datasets and mean parameter estimates and upper/lower bounds of the confidence intervals are presented.
Results
Of 430 enrolled mother–infant dyads, 415 were included in this analysis (Fig. 1). The 15 excluded mothers were more likely to be black (86.7% excluded vs. 51.1% included, p = 0.025) and to have chorioamnionitis (40.0% excluded vs. 10.6% included; p = 0.001), cesarean delivery (93.3% excluded vs. 62.4% included; p = 0.015), and Type II diabetes (13.3% excluded vs. 1.9% included; p = 0.004). Excluded mothers were similar to included mothers for all other characteristics.
Table 1 summarizes maternal and infant characteristics for the 415 mother–infant dyads and by race/ethnicity subgroups; all Hispanic mothers in the cohort were of white race. Compared to other mothers, black mothers were significantly younger, had fewer mean daily pumping sessions, and were less likely to be married. Among multiparous mothers, black mothers were significantly less likely to have breastfed or provided MOM. Black mothers were less likely to have access to a car than Hispanic mothers. Black mothers had lower education levels than white mothers, while Hispanic mothers had lower education levels than both other groups. White mothers were less likely to have low SES, more likely to smoke, and more likely to have a multiple gestation. Black infants were significantly less likely to receive MOM feeding at NICU discharge (23.1%) compared to white (42.2%) and Hispanic (43.4%) infants (p < 0.001 for differences among the three groups).
Multivariate logistic regression models
Positive predictors of MOM feeding at discharge included older maternal age (odds ratio (OR) 1.10 [1.03–1.16], p = 0.002), mean number of daily pumping sessions during the first 14 postpartum days (OR 1.71 [1.24–2.35], p = 0.001), and CTV by postpartum day 14 (OR 8.29 [3.37–20.42]], p < 0.001). Significant negative predictors of MOM feeding at NICU discharge were low SES (OR 0.34 [0.14–0.83], p = 0.019) and perceived breastfeeding support from the mother’s mother (infant’s maternal grandmother) (OR .47 [0.25–0.87], p = 0.016) (Table 2). Figure 3 depicts the effect of low SES defined as WIC eligibility on rate of MOM at DC by racial/ethnic subgroups, with lower rates of MOM at DC noted for white and black infants compared to Hispanic infants. Sensitivity analyses were conducted removing Asian mothers form the white group. No significant differences were detected between model results with and without Asian mothers.
Mediation analyses
Three candidate mediator variables (maternal age, low SES, and mean number of daily pumping sessions) were included in the multiple mediator model (Table 3). Indirect effects for white vs. black mothers on MOM at discharge were significant for maternal age, low SES, and daily pumping frequency. White mothers were older, less likely to be of low SES and had greater daily pumping frequency. Each of these variables was more likely to be associated with infants’ receiving MOM at DC. Indirect effects for Hispanic vs. black mothers on MOM at discharge were significant for maternal age and daily pumping sessions. Hispanic mothers were older and had greater daily pumping frequency, and each of these conditions was associated with infants’ receiving MOM at DC. The indirect effect of Hispanic vs black mothers on MOM at discharge through low SES was non-significant.
Discussion
In our study, 98% of mothers of VLBW infants initiated MOM provision, with no racial/ethnic disparities in initiation rates. However, racial/ethnic differences were evident at NICU discharge with significantly fewer black VLBW infants still receiving MOM feeding, despite black mothers indicating they wanted to continue MOM feeding after NICU discharge.10 Our analysis included several factors that are not modifiable during the NICU stay and that have been previously associated with MOM feeding: maternal age,2 low SES,18 GA,2 number of children at home,9 marital status,9 maternal health,29 maternal education,17 and maternal smoking.17,18 Of these, only maternal age and low SES emerged as significant non-modifiable predictors of MOM feeding at NICU discharge in this cohort. We also identified key predictors that are potentially modifiable during the NICU stay: pumping factors and family support. We then identified factors that mediate the racial/ethnic disparity in MOM feeding at discharge. Maternal age, low SES, and pumping factors mediated the black–white disparity, whereas maternal age and pumping factors mediated the black–Hispanic disparity.
A significant modifiable factor consistent with previous studies14,25 was daily pumping frequency during the first 14 days postpartum, which had a dose-dependent effect on MOM feeding at discharge. The mammary gland is especially sensitive to stimulation by the infant or breast pump during the transition from secretory differentiation to secretory activation and this stimulation is thought to have a programming effect on mammary secretory cells.30 Notably, 40% of mothers who kept logs pumped ≥5 times per day, which has been shown to be associated with longer lactation duration in mothers of preterm infants. Furman et al.14 found that mothers of VLBW infants who continued lactation after 40 weeks post-menstrual age were more likely to pump ≥5 times per day at 3 weeks post partum than women who had discontinued lactation by this time. Hill et al.25 demonstrated a significant effect of pumping frequency in mothers of preterm infants, with pumping ≥6 times per day associated with increased odds of producing ≥500 mL/day MOM by weeks 2–5 post partum. However, only two (1%) of the mothers pumped our recommended frequency of 8–12 times per day, which may be partly attributed to the mother’s own health concerns and/or the stress associated with preterm delivery and the NICU environment. Based on the paucity of studies, it is undetermined if the currently recommended frequency of 8–12 times per day is more efficacious then 5–6 times per day, but our data indicate that it may be difficult to attain even with dedicated NICU-specific lactation care. CTV was also a significant predictor of MOM feeding at discharge in our study. Previous researchers have also reported that high volumes of MOM during the second week of life significantly predicted MOM adequacy at 6 weeks post partum.25,29 These findings indicate that evidence-based lactation care should be concentrated in the first 2 weeks postpartum for mothers of VLBW infants with a primary focus on frequency of pumping and the MOM volume target of ≥500 mL/day. Given the complexity of pumping in mothers of VLBW infants, specific strategies and close monitoring of MOM volume are required.31 Intensive communication in the first 2 weeks may be our best intervention. Daily maternal follow-up by breastfeeding peer counselors, lactation consultants, or nursing in-person or via phone to monitor changes in pumped MOM volume, actual (not theoretical) pumping frequency, and practical challenges such as nipple discomfort that affect pumping can provide real-time advice and targeted support.31
A surprising finding was that mothers’ perception of support for MOM feeding from their own mothers was negatively associated with MOM feeding at NICU discharge. While this was true for the entire cohort, we have previously shown that subgroup analysis demonstrated this was a significant predictor in the black subgroup, but not in the white or Hispanic subgroups.16 Despite this previous subgroup finding, it did not mediate racial/ethnic disparity in our cohort. It is well known that grandmothers have significant impact on infant feeding decisions.32,33 However, our results contradict previous literature which reports a direct relation between support of family and friends and pumping behavior15 in mothers of infants in the NICU. A potential explanation is that grandmothers may want to facilitate their own daughter’s well-being by supporting her paid work or education rather than prioritizing the daughter developing her maternal role.32 Additionally, grandmothers may regard breastfeeding as a barrier to their own ability to bond with their grandchild or may have inaccurate breastfeeding knowledge.32 A study conducted by Rossman et al.34 found that teen mothers in the NICU reported that their mothers (infants’ maternal grandmothers) supported the decision to provide MOM; however, when prompted to provide examples of support, the mothers shared grandmothers’ specific comments and behaviors that were negative and undermined MOM provision efforts. Teen mothers relied on their mothers’ advice despite grandmothers lacking breastfeeding experience or knowledge.34 Pilot studies of breastfeeding education for grandmothers in non-NICU settings demonstrate equivocal results, with grandmothers receiving the intervention demonstrating improvement in breastfeeding knowledge without accompanying changes in attitude.35 However, NICU breastfeeding education targeting grandmothers may be a strategy to address this modifiable factor and merits further investigation.
While previous researchers have focused on factors associated with MOM feeding at discharge, we extended this area of investigation to determining whether these factors differ between black and non-black mothers. We identified low SES/WIC eligibility as a significant mediator of the black–white disparity in our cohort, meaning that poverty explained the difference in MOM receipt between black and non-black infants at NICU discharge. These results are similar to Lee et al.,36 who reported no black–white disparity in breastfeeding duration for mothers in Philadelphia after adjusting for multiple factors, including receipt of WIC benefits. However, our analyses did not address whether this finding is due to WIC serving as a marker for poverty18 or due to practices at WIC agencies. We theorize both are plausible, although the impact of WIC practices seems a less likely explanation because of the standardized NICU-specific lactation support available in the study NICU, including dedicated lactation care by breastfeeding peer counselors and the accessibility of subsidized rental of a hospital-grade pump in the NICU. However, mothers receiving WIC benefits may have been influenced by policies that were common during 2008–2012, since changes in WIC policies and food packages have been shown to impact breastfeeding decisions by mothers of primarily healthy infants.37 Due to missing data for household income (over 50% of subjects declined to answer the question or did not know), we were unable to separately control for WIC and poverty.
An important aspect specific to mothers of VLBW infants is that they are breast pump-dependent and incur additional costs,31 which are especially burdensome to low SES mothers. Obtaining a breast pump promptly is critical to establishing MOM supply over the first 2 weeks postpartum,30 which we have demonstrated is a strong predictor of continued MOM feeding at NICU discharge. However, pump purchase or monthly rental charges, even when subsidized, can be cost prohibitive for WIC-eligible mothers. Providing free breast pumps to disadvantaged mothers may mitigate racial and ethnic disparity, and has previously been associated with increased MOM provision in NICU mothers.7 Additional costs incurred by NICU mothers include potential loss of paid opportunities or having to pay others for caregiving or other household responsibilities during the approximately 2 h spent pumping and cleaning pump equipment daily. A recent randomized pilot study of such an incentive resulted in significantly greater breastfeeding rates among WIC-enrolled Puerto Rican mothers during the first 6 months postpartum.38 Similarly, a large cluster randomized controlled trial of financial incentives to breastfeed demonstrated significantly higher 6–8 week breastfeeding prevalence in areas of the United Kingdom with low baseline breastfeeding prevalence.39 However, there remain concerns regarding the ethical implications of such an incentive, despite the fact that many of these mothers receive a similar incentive to not breastfeed in the form of free formula.38,39
The black–Hispanic disparity in our cohort differed from the black–white disparity, as previously reported.36 While maternal age and pumping factors mediated the effect, there may be other unmeasured factors that could contribute to racial/ethnic differences. Other researchers have highlighted the importance of nativity and acculturation in breastfeeding outcomes.33 While we did not collect these factors, a sizeable minority of Hispanics in Chicago are foreign born, and we speculate that this may have had an impact as the Hispanic WIC-eligible mothers had higher rates of MOM at discharge compared to black and white WIC-eligible mothers (Fig. 3).
Limitations
Generalizability of results may be influenced by the fact that our sample is from a single urban NICU that serves predominantly minority, socioeconomically disadvantaged mothers. While we collected self-stated race, we did not code multiple races and selectively chose black if it was one of the multiple races that were reported. A strength of our study is the large number of black and Hispanic mothers who almost universally initiated lactation. However, roughly half of the cohort did not maintain pumping records, and rates of maintaining pumping records differed significantly by race/ethnicity such that black mothers maintained records at approximately half the rate of white or Hispanic mothers (Supplemental Table S1). Women who did not maintain pumping records also differed in other sociodemographic characteristics from the subset of mothers who maintained pumping records (Supplemental Table S2). Although missing data were imputed, having complete data for pumping records would strengthen these findings. Furthermore, there remains the potential that mothers who did not maintain pumping records may have pumped very infrequently and may have had low rates of CTV by postpartum day 14, since MOM at discharge was uncommon in the imputed group (Supplemental Table S2). Thus, mean number of daily pumping sessions and CTV over the first 2 weeks postpartum may have an even stronger effect than we detected. The use of WIC to define SES is another limitation of our study, since SES may be defined by multiple characteristics such as income, education (which was included as a separate demographic factor in our analysis), occupation or a combination of these. We selected WIC due to the high proportion of subjects for which this variable was available (99%) and its correlation with income due to eligibility criteria of annual income ≤185% of the US federal poverty income limit. Our mediation analyses included a binary mediator (low SES), and even though we used an approach shown to be appropriate for binary mediators,28 this remains an area of ongoing debate. Thus, these results should be interpreted with due caution. Another limitation is that we used infant’s receipt of MOM in the last full 24 h prior to discharge as our primary outcome, which may over-report continued pumping if the mother had sufficient amounts of previously frozen MOM for feedings at the time of discharge. Another limitation was that mothers rarely identified persons who did not support their breastfeeding choice, but only those who did support their choice. This may reflect discomfort with reporting unsupportive friends and family. Finally, no data were collected on skin-to-skin care or direct breastfeeding which have been associated with increased MOM feedings in premature infants,40 although both are encouraged and standard practices in our NICU.
Conclusions
This study of a large recent cohort of mothers of VLBW infants identified the important modifiable factors of family support and pumping factors that were associated with MOM feeding at NICU discharge, and identified WIC eligibility, pumping factors, and maternal age as mediators of racial/ethnic disparities. These findings are important to the design of evidence-based interventions focused on improving rates of MOM feedings at NICU discharge. Although the importance of pumping frequency and early MOM volume have been previously documented, these data highlight the importance of close monitoring and developing and testing strategies to positively influence these modifiable factors. With the unexpected finding that perceived support from the infant’s maternal grandmother was associated with decreased odds of MOM feedings, further study of grandmothers and the support they provide to their daughters is warranted. Given the paucity of literature regarding the potential influence of WIC on breastfeeding in mothers of VLBW infants, interventions to mitigate the impact of poverty in this vulnerable population that is at risk for so many potentially modifiable adverse health outcomes are urgently needed.
Change history
18 September 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
March of Dimes. Very low birthweight by race/ethnicity: United States, 2012–2014 Average. http://www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=99&top=4&stop=54&lev=1&slev=1&obj=1 (2017).
Lee, H. C. & Gould, J. B. Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. J. Pediatr. 155, 657–62.e1-2 (2009).
Patel, A. L. et al. Impact of early human milk on sepsis and health care costs in very low birthweight infants. J. Perinatol. 33, 514–519 (2013).
Patra, K. et al. NICU human milk dose and 20-month neurodevelopmental outcome in very low birth weight infants. Neonatology 112, 330–336 (2017).
Stuebe, A. M. & Schwarz, E. B. The risks and benefits of infant feeding practices for women and their children. J. Perinatol. 30, 155–162 (2010).
Stewart, S. L. et al. Disparities in ovarian cancer survival in the United States (2001–2009): findings from the CONCORD-2 study. Cancer 123(Suppl. 24), 5138–5159 (2017).
Philipp, B. L., Brown, E. & Merewood, A. Pumps for peanuts: leveling the field in the neonatal intensive care unit. J. Perinatol. 20, 249–250 (2000).
Sisk, P. M., Lovelady, C. A., Dillard, R. G. & Gruber, K. J. Lactation counseling for mothers of very low birth weight infants: effect on maternal anxiety and infant intake of human milk. Pediatrics 117, e67–e75 (2006).
Pineda, R. G. Predictors of breastfeeding and breastmilk feeding among very low birth weight infants. Breastfeed. Med. 6, 15–19 (2011).
Hoban, R. et al. Goals for human milk feeding in mothers of very low birth weight infants: how do goals change and are they achieved during the NICU hospitalization? Breastfeed. Med. 10, 305–311 (2015).
Nommsen-Rivers, L. A., Chantry, C. J., Peerson, J. M., Cohen, R. J. & Dewey, K. G. Delayed onset of lactogenesis among first-time mothers is related to maternal obesity and factors associated with ineffective breastfeeding. Am. J. Clin. Nutr. 92, 574–584 (2010).
Dewey, K. G., Nommsen-Rivers, L. A., Heinig, M. J. & Cohen, R. J. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics 112(Part 1), 607–619 (2003).
Lau, C., Hurst, N. M., Smith, E. O. & Schanler, R. J. Ethnic/racial diversity, maternal stress, lactation and very low birthweight infants. J. Perinatol. 27, 399–408 (2007).
Furman, L., Minich, N. & Hack, M. Correlates of lactation in mothers of very low birth weight infants. Pediatrics 109, e57 (2002).
Sisk, P. M., Quandt, S., Parson, N. & Tucker, J. Breast milk expression and maintenance in mothers of very low birth weight infants: supports and barriers. J. Hum. Lact. 26, 368–375 (2010).
Fleurant, E. et al. Barriers to human milk feeding at discharge of very-low-birth-weight infants: maternal goal setting as a key social factor. Breastfeed. Med. 12, 20–27 (2017).
Sisk, P. M., Lovelady, C. A., Dillard, R. G., Gruber, K. J. & O’Shea, T. M. Maternal and infant characteristics associated with human milk feeding in very low birth weight infants. J. Hum. Lact. 25, 412–419 (2009).
Li, R. & Grummer-Strawn, L. Racial and ethnic disparities in breastfeeding among United States infants: Third National Health and Nutrition Examination Survey, 1988-1994. Birth 29, 251–257 (2002).
Tenfelde, S. M., Finnegan, L., Miller, A. M. & Hill, P. D. Risk of breastfeeding cessation among low-income women, infants, and children: a discrete time survival analysis. Nurs. Res. 61, 86–95 (2012).
Riley, B. S. et al. Barriers to human milk feeding at discharge of VLBW infants: evaluation of neighborhood structural factors. Breastfeed. Med. 11, 335–342 (2016).
Burdette, A. M. Neighborhood context and breastfeeding behaviors among urban mothers. J. Hum. Lact. 29, 597–604 (2013).
Anthopolos, R., Kaufman, J. S., Messer, L. C. & Miranda, M. L. Racial residential segregation and preterm birth: built environment as a mediator. Epidemiology 25, 397–405 (2014).
Hoban, R. et al. Milk volume at 2 weeks predicts mother’s own milk feeding at neonatal intensive care unit discharge for very low birthweight infants. Breastfeed. Med. 13, 135–141 (2018).
Hartmann, P. & Cregan, M. Lactogenesis and the effects of insulin-dependent diabetes mellitus and prematurity. J. Nutr. 131, 3016S–3020S (2001).
Hill, P. D., Aldag, J. C. & Chatterton, R. T. Effects of pumping style on milk production in mothers of non-nursing preterm infants. J. Hum. Lact. 15, 209–216 (1999).
van Buuren, S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat. Methods Med. Res. 16, 219–242 (2007).
Graham, J. W., Olchowski, A. E. & Gilreath, T. D. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev. Sci. 8, 206–213 (2007).
Muthen, B. Applications of Causally Defined Direct and Indirect Effects in Mediation Analysis Using SEM in Mplus (Muthén & Muthén, Los Angeles, 2011).
Omarsdottir, S. et al. Predictors of sustained maternal milk feeds in extremely preterm infants. J. Perinatol. 35, 367–372 (2015).
Meier, P. P., Patel, A. L., Hoban, R. & Engstrom, J. L. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 36, 493–499 (2016).
Meier, P. P., Johnson, T. J., Patel, A. L. & Rossman, B. Evidence-based methods that promote human milk feeding of preterm infants: an expert review. Clin. Perinatol. 44, 1–22 (2017).
Grassley, J. & Eschiti, V. Grandmother breastfeeding support: what do mothers need and want? Birth 35, 329–335 (2008).
McKinney, C. O., et al. Racial and ethnic differences in breastfeeding. Pediatrics 138, e20152388 (2016).
Rossman, B., Meier, P. P., Janes, J. E., Lawrence, C. & Patel, A. L. Human Milk provision experiences, goals, and outcomes for teen mothers with low-birth-weight infants in the neonatal intensive care unit. Breastfeed. Med. 12, 351–358 (2017).
Grassley, J. S., Spencer, B. S. & Law, B. A grandmothers’ tea: evaluation of a breastfeeding support intervention. J. Perinat. Educ. 21, 80–89 (2012).
Lee, H. J., Ilo, I. T., McCollum, K. F. & Culhane, J. F. Racial/ethnic differences in breastfeeding initiation and duration among low-income, inner-city mothers. Soc. Sci. Q. 90, 1251–1271 (2009).
Rasmussen, K. M. et al. New opportunities for breastfeeding promotion and support in WIC: review of WIC food packages, improving balance and choice. J. Nutr. Educ. Behav. 49(Suppl. 2), S197–S201.e1 (2017).
Washio, Y. et al. Incentive-based intervention to maintain breastfeeding among low-income Puerto Rican mothers. Pediatrics 139, e20163119 (2017).
Relton, C. et al. Effect of financial incentives on breastfeeding: a cluster randomized clinical trial. JAMA Pediatr. 172, e174523 (2018).
Parker, M. G. & Patel, A. L. Using quality improvement to increase human milk use for preterm infants. Semin. Perinatol. 41, 175–186 (2017).
Acknowledgements
Thank you to the patients and families who participated in this research. The research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number R03HD081412. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
A.L.P. conceptualized and designed the study, coordinated and supervised data collection, drafted the initial manuscript, and reviewed and revised the manuscript. M.E.S., R.H., and H.B. supervised data collection, carried out the initial analyses, and reviewed and revised the manuscript. T.J.J. and J.L.E. supervised data collection and reviewed and revised the manuscript. E.F. and B.R. made substantial contributions to data collection. P.P.M. conceptualized and designed the study, coordinated and supervised data collection, and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Patel, A.L., Schoeny, M., Hoban, R. et al. Mediators of racial and ethnic disparity in mother’s own milk feeding in very low birth weight infants. Pediatr Res 85, 662–670 (2019). https://doi.org/10.1038/s41390-019-0290-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0290-2
This article is cited by
-
Leveraging mHealth and a milk expression frequency biomarker during postpartum to prolong lactation among parents of critically ill infants: a pilot study
Journal of Perinatology (2023)
-
Early pumping frequency and coming to volume for mother’s own milk feeding in hospitalized infants
Journal of Perinatology (2023)
-
Transmission of negative biases through social commentary included in neonatal intensive care unit progress notes
Journal of Perinatology (2023)
-
Study protocol for reducing disparity in receipt of mother’s own milk in very low birth weight infants (ReDiMOM): a randomized trial to improve adherence to sustained maternal breast pump use
BMC Pediatrics (2022)
-
Human milk feeding and wheeze in Black infants born preterm
Journal of Perinatology (2022)