Abstract
Background
Reliable screening for iron deficiency (ID) has required a blood sample and cost-intensive laboratory measurements. A novel method to non-invasively measure erythrocyte zinc protoporphyrin (ZnPP), an established marker for ID, is evaluated in children.
Methods
ZnPP was determined non-invasively by fluorescence measurements on the wet vermillion of the lower lip in 99 hospitalized children aged 9 months to 5 years. For comparison, conventional ID parameters and ZnPP were determined from blood samples.
Results
The non-invasively measured ZnPP values had limits of agreement (LoA) of 14 µmol ZnPP/mol heme (95% confidence interval: 9–20) compared to fluorescence measurements directly in blood. Repeated high-performance liquid chromatography reference determinations had comparable LoA of 14 µmol ZnPP/mol heme (9–17). Non-invasive ZnPP measurements had sensitivity and specificity of 67% (39–88%) and 97% (91–99%), and negative and positive predictive value of 94% (90–97%) and 80% (55–93%), for detecting ID as defined by the soluble transferrin receptor (sTfR). In groups with more severe ID as defined by serum ferritin and sTfR, higher ZnPP values were found, with the highest ZnPP values for the group with ID anemia.
Conclusion
Non-invasive ZnPP measurements are reliably feasible in children. The simple and fast method has the potential to enable wide-spread screening for ID.
Similar content being viewed by others
Introduction
Iron deficiency (ID) is the most common nutrient deficiency worldwide.1 When severe, it can lead to ID anemia (IDA).2 Among children and adolescents, IDA is the leading cause of years lived with disability, affecting 619 million children and adolescents in 2013.1 In the United States, ID and IDA have a prevalence of ~7.1 and ~1.1% among children aged 1 to 5 years, respectively.3 Although ID and IDA can be effectively treated, the prevalence has not decreased over the past decade.3
Symptoms of ID include a reduced immune responsiveness4 and diminished physical performance.5 In the first years of life, iron is particularly important for the rapidly developing brain.6 Early ID appears to be associated with persistent central nervous system alterations, which cannot be completely reversed by iron supplementation in later years.6,7,8,9,10,11
Screening for IDA is frequently done by measuring hemoglobin, which can be determined non-invasively and might thus enhance applicability. For the United States, the American Academy of Pediatrics recommends universal screening by hemoglobin for children aged 12 months.12 Others have come to a similar conclusion,13,14 while the US Preventive Services Task Force has concluded that there is not enough evidence applicable to the United States to recommend universal IDA screening in children aged 6 to 24 months.15 In the United States, only about one-third of children with anemia are iron deficient, while two-third have anemia of other causes, for example, anemia of chronic disease.3,12,15,16 Consequently, screening for IDA by hemoglobin alone has a positive predictive value (PPV) of only ~35%.15,16 Other, more reliable parameters to assess the iron status require a blood sample and cost-intensive laboratory measurements.
Erythrocyte zinc protoporphyrin (ZnPP) is a reliable marker for ID, which was shown to be more sensitive and more specific for ID than hemoglobin in children.17,18 An increased amount of ZnPP is found in erythrocytes when an insufficient amount of iron is present in the last step of the heme synthesis pathway.19 More pronounced ID leads to higher ZnPP values, with highest values found for severe IDA.20 ZnPP can be measured with a portable hematofluorometer,21 but requires a drop of blood. Recently, we presented a method to measure ZnPP non-invasively from the lower lip and established proof of concept in 56 women after childbirth.22 This method enables non-invasive, fast and specific ID and IDA testing at the point of care, without the need for a blood withdrawal.
The objective of this investigation is1 to explore if non-invasive ZnPP measurements are feasible in children aged 9 months to 5 years, and2 to assess if ZnPP is a reliable marker for detecting iron-deficient erythropoiesis (IDE) and IDA in the investigated patient group of hospitalized children.
Methods
Clinical evaluation
Hospitalized children (n = 100) aged between 9 months and 5 years undergoing clinically indicated blood withdrawal were recruited between April and September 2016 at the Dr. von Hauner Children’s Hospital, LMU Munich, Germany. Children who received a transfusion of blood products in the 4 months preceding the measurements were excluded. A diverse cohort was chosen to demonstrate the general feasibility and accuracy of the non-invasive method, independent of possible comorbidities. A more detailed description of the cohort can be found in Supplementary Materials. For each subject, the age was recorded and the skin color assessed according to the Fitzpatrick Skin Phototype Classification Score.23 Ethical approval for the study was given by the Institutional Ethical Board of the Medical Faculty, Ludwig-Maximilians-University of Munich, Germany (study identifier: LFL_S2/2015, ClinicalTrials.gov identifier: NCT02701309). Written informed consent was obtained from each subject’s parent or legal guardian prior to study enrollment.
Blood sample collection and laboratory analysis
Residual blood samples (ethylenediaminetetraacetic acid (EDTA) and serum tubes) after completed diagnostic analyses were obtained on the day of the non-invasive measurement. The soluble transferrin receptor (sTfR), serum ferritin, c-reactive protein (CRP), and a complete blood count were determined as routine measurements. For fluorescence spectroscopic measurements, a 100 µL aliquot of EDTA blood was stored at +4 °C; measurements were carried out within 24 h after the blood withdrawal. For the determination of ZnPP by high-performance liquid chromatography (HPLC), two aliquots of EDTA blood (250 µL each) were stored at −80 °C. For six subjects, only an incomplete set of parameters could be determined due to an insufficient amount of left-over blood. Threshold values were supplied by the Institute of Laboratory Medicine for ferritin (low: <12 µg/L for children <12 months, otherwise <24 µg/L), CRP (elevated: >0.5 mg/dL), hemoglobin (low: <10.7 g/dL), and ZnPP (elevated: >50 µmol ZnPP/mol heme). For the sTfR, only a threshold value for adults was available (elevated: >1.76 mg/L). This threshold does not apply to children, for whom generally higher sTfR values are found.24 A study in 2153 children aged 1 to 5 years found an 11% higher threshold for sTfR compared to adults.24 Therefore, in this study, values of sTfR >1.95 mg/L (=1.11 × 1.76 mg/L) were considered as elevated.
Clinical definitions
The stage of ID (iron depletion, IDE, or IDA) was determined for each child from ferritin, sTfR, and hemoglobin values as suggested in the literature:25 “No ID”: normal ferritin, sTfR, and hemoglobin; “Iron depletion”: low ferritin, but normal sTfR and hemoglobin; “IDE”: low ferritin levels or elevated CRP, elevated sTfR, but normal hemoglobin; “IDA”: low ferritin levels or elevated CRP, elevated sTfR, and low hemoglobin.
Normal ferritin values were disregarded if an elevated CRP suggested a falsely elevated ferritin value due to its reaction as acute-phase protein.
Non-invasive measurement of the ZnPP/heme ratio
All non-invasive fluorescence measurements were conducted by the same physician (FM) during the clinically indicated inpatient stay. The ZnPP/heme ratio was measured non-invasively with a device adapted from the one used in a previous study.22
In brief, a 1000 µm optical fiber is placed gently on the red vermillion of the lower lip of the subject. The fiber is embedded into a 12-mm steel handpiece which narrows to 6 mm at the tip. For 13 children an optical fiber probe with a 5-mm handpiece embedded in a sterilized single-use pacifier was used instead to examine the influence on the behavior of the child. To avoid contamination or transmission of pathogens, the optical fiber probes were disinfected before and after usage.
The optical fiber probe is slowly moved over the lip, until the device indicates that a tissue site is found where the blood content is sufficient to ensure a reliable measurement. The identification is done in real time by analyzing the spectral features of the blood absorption in the tissue background fluorescence. Then, the measurement sequence is started with alternating excitation wavelengths (central wavelengths: 407 and 425 nm). The measurement procedure was repeated until 100 pairs of fluorescence spectra were recorded at tissue sites with sufficient blood content or until the measurement had to be stopped due to the behavior of the child. For the analysis, the fluorescence spectra excited at 407 nm were subtracted from the fluorescence spectra excited at 425 nm, reducing the fluorescence background.22,26 A spectral fitting procedure determined the amplitude of the ZnPP fluorescence for each spectrum. Averaging over all determined ZnPP amplitudes for each patient yielded the ZnPP value, which is proportional to the ZnPP/heme ratio.
Fluorescence spectroscopic measurements of the ZnPP/heme ratio in blood
The ZnPP/heme ratio was additionally determined by fluorescence spectroscopic measurements on EDTA blood as a reference determination. A bare 1000 µm optical fiber was connected to the fluorescence measurement device. The distal end was put into an aliquot of 100 µL EDTA blood. To minimize photobleaching, that is, photo-chemical destruction of the ZnPP molecules, the sample tube was rotated axially at 112 rpm during the measurement, yielding a stable fluorescence signal. Fluorescence spectra were acquired for 425-nm excitation. The amplitude of the ZnPP fluorescence was determined for each spectrum by a fit procedure similar to the non-invasive measurements. The resulting amplitudes were averaged, yielding the ZnPP value. The average standard deviation for five repeated measurements in 21 blood samples was 2.2%.
HPLC determination
HPLC was performed as additional reference determination of the ZnPP/heme ratio at the specialized laboratory MVZ Labor PD Dr. Volkmann und Kollegen GbR, Karlsruhe, Germany, as previously described.22 For evaluation of the repeatability of the method, a second determination was done for a subgroup of n = 58 children where a sufficient amount of EDTA blood was available. The comparison of these two determinations is shown in Supplementary Figure 1A, B. A bias of −10 µmol ZnPP/mol heme was found, and six outliers can be identified. The robust limit of agreement (LoA) equals 14 µmol ZnPP/mol heme for this comparison. Due to the unexpected bias and high number of outliers, we decided to use the fluorescence spectroscopic measurements in blood as reference measurements in the following. For transparency, all data with HPLC as reference are shown in Supplementary Information (Supplementary Figures S3 and S4 and Supplementary Tables S1 and S4).
Statistical data analysis
For direct comparison of the ZnPP values measured either non-invasively or directly in blood with the HPLC reference, the values were scaled. The scaling factor was derived by fitting a straight line with zero offset to the comparison of the measured ZnPP values to the reference HPLC determination (software: MATLAB R2014b, The MathWorks Inc., Natick, MA, USA, function: robustfit). For the quantitative comparison of two methods, the LoA and the bias were calculated using the robust τ-estimate (software: R version 3.2.2; function: scaleTau2; package: robustbase version 0.92.5) of the differences between the two methods, where the robust standard deviation was multiplied by 1.96. The 95% confidence intervals (CI) were calculated by bootstrapping (software: R; functions: boot and boot.ci; package: boot version 1.3.17). Sensitivity, specificity, negative predictive value (NPV), and PPV were calculated from contingency tables (software: R; function: BDtest; package: bdpv version 1.1).
Results
Practical feasibility
The practical feasibility of the non-invasive determination of the ZnPP/heme ratio was investigated in 99 of 100 children, as one child left the hospital prior to the non-invasive measurement. For 16 of 99 children, the non-invasive measurement could not be conducted due to their reluctant behavior and abrupt movements of the head, as well as crying. Most of these children had their pacifier in the mouth prior to the measurement. For the measurement on the lower lip, the pacifier had to be removed, which was often not tolerated by the child. Using the applicator embedded in the single-use pacifier did not result in an appreciable improvement. The percentage of reluctant children was similar among the 66 children aged up to 48 months (see also Supplementary Figure S2). All 33 children aged 4 years and older tolerated the measurement without difficulty. For all children who tolerated the measurement, the average time for the whole measurement procedure was about 3 min (median 169 s, mean 217 s), with a recording time on the lip of about 1 min (median 72 s, mean 85 s).
Non-invasive detection of ZnPP
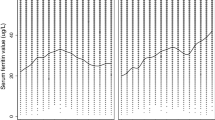
The non-invasive measurement results are compared to the fluorescence measurements directly in blood for 83 of 99 children, for which the measurement could be conducted. This comparison is shown in Fig. 1a, c, with corresponding Bland–Altman plots shown in Fig. 1b, d. The LoA of 14 µmol ZnPP/mol heme and the bias of 1 µmol ZnPP/mol heme are indicated as well.
In addition, both the ZnPP values measured non-invasively and directly in blood were compared with the HPLC reference, with LoAs of 19 and 15 µmol ZnPP/mol heme, respectively (see Supplementary Figure S3 for the correlation). For all comparisons, the LoA, including 95% CI and the bias, are listed in Supplementary Table S1. The non-invasive method approaches the precision of the reference HPLC method, for which, however, a large bias (−10 µmol ZnPP/mol heme) was found for the two repeated determinations (see Supplementary Figure 1).
In Fig. 1d, measurement results for the nine children with Fitzpatrick skin types IV, V, or VI are highlighted by circles. No increased variations or systematic deviations dependent on the skin pigmentation are observed for the non-invasive detection of the ZnPP/heme ratio.
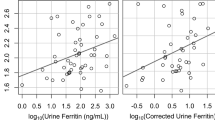
ZnPP measurement for the detection of ID
A secondary aim of this study was the comparison of ZnPP measurements with other ID parameters. In Fig. 2a, b, the ZnPP values are compared with the sTfR. For this comparison, the ZnPP determination by fluorescence measurements in blood is available for 93 children, the non-invasive measurements for 82 children. For the comparison with the ZnPP determination by fluorescence measurements in blood, sensitivity and specificity equaled 92% (95% CI: 66–100%) and 90% (95% CI: 83–95%), respectively. NPV and PPV equaled 99% (95% CI: 94–100%) and 58% (95% CI: 44–71%), respectively. For the comparison with the non-invasive ZnPP measurements, sensitivity and specificity equaled 67% (95% CI: 39–88%) and 97% (95% CI: 91–99%), respectively. NPV and PPV equaled 94% (95% CI: 90–97%) and 80% (95% CI: 55–93%), respectively.
In addition to the comparison of ZnPP with the sTfR, ZnPP values were also compared to the stage of ID as defined in the Methods section. For children whose iron status could not be classified according to this scheme, results are detailed below.
Figure 3 shows the distribution of ZnPP values measured directly in blood and non-invasively for the different groups. The corresponding descriptive statistics are given in Supplementary Table S2 and S3. For the measurements directly in blood, the average ZnPP value for the groups increases from 30 µmol ZnPP/mol heme (no ID), over 40 µmol ZnPP/mol heme (ID), over 68 µmol ZnPP/mol heme (IDE) to 143 µmol ZnPP/mol heme (IDA). For the non-invasive measurements, the average ZnPP value for the groups increases from 29 µmol ZnPP/mol heme (no ID), over 38 µmol ZnPP/mol heme (ID), over 98 µmol ZnPP/mol heme (IDE) to 102 µmol ZnPP/mol heme (IDA). Only a low number of subjects are found in the groups IDE and IDA (3 and 7, respectively).
For the children that could not be classified according to the given scheme, one child had borderline normal CRP = 0.49 mg/dL, ferritin = 34 µg/L, elevated sTfR = 1.98 mg/L, and ZnPP = 54 µmol/mol heme (measured directly in blood) and 52 µmol/mol heme (measured non-invasively), indicating IDE. Another four children had elevated CRP or very high ferritin (1531 µg/L) and low hemoglobin, but normal sTfR, indicating anemia of chronic disease. The mean ZnPP was 49 µmol/mol heme (range: 36–61, measured directly in blood) and 41 µmol/mol heme (range 32–50, measured non-invasively) for this group. The remaining children had low hemoglobin, but all other parameters were normal. The mean ZnPP was 28 µmol/mol heme (range: 23–31, measured directly in blood) and 28 µmol/mol heme (range: 15–39, measured non-invasively) for this group.
Discussion
The present investigation proves the feasibility of non-invasive measurement of ZnPP in children aged 9 months to 5 years. The precision of the measurement, quantified as LoA between the non-invasive measurements and the reference HPLC determination, was 19 µmol ZnPP/mol heme. This equals the LoA of 19 µmol ZnPP/mol heme found in a study on 56 women after childbirth.22 When comparing the non-invasive measurements with measurements directly in blood using the same device, a smaller LoA of 14 µmol ZnPP/mol heme was found. This equals the LoA of two repeated HPLC determinations, which had a bias of 10 µmol ZnPP/mol heme and showed six pronounced outliers. We therefore speculate that our fluorescence measurement directly in blood is the most reliable method, outperforming the current standard HPLC. In the non-invasive measurement an additional error is introduced due to variations of the composition of the lip. Though not systematically investigated, we found no obvious influence of skin pigmentation on the measurement results.
To assess the relevance of the determined LoAs for screening purposes, it can be helpful to compare with the hematofluorometer (Model 206D, AVIV Biomedical Inc., Lakewood, NJ, USA), which is most often used for ZnPP measurements.27,28,29 In point-of-care settings, whole blood is often measured with this instrument, because no sample preparation is required, accepting higher readings and lower precision compared to washed erythrocytes due to interfering background fluorescence from the blood plasma.25,30,31,32 Under these conditions, measurements of ZnPP by a hematofluorometer had LoA of 22 µmol ZnPP/mol heme when compared to HPLC in our study on 56 women after childbirth.22 The LoA of the non-invasive measurements are at least comparable and are thus considered sufficiently small for screening purposes.
In 16 of 99 children the non-invasive measurement could not be conducted due to their reluctant behavior. This may be partly due to the investigated inpatients, who may be more stressed and afraid of a medical examination than other children. Also, the measurements were proactively stopped if children were not comfortable with them to avoid study-induced stress to children and their parents. We therefore speculate that the compliance is even better under routine screening conditions. The applicability of the measurement may be further improved by reducing its duration to about 20 s compared to the current median measurement time of 72 s. This can be done by reducing the amount of recorded valid spectra from 100 to 30. In general, a higher number of recorded spectra will lead to a more precise measurement, which is why we a priori chose to aim for the high number of 100 valid spectra. In the present study, the calculated LoA include measurements on 35 children with 30 valid spectra or less, indicating that 30 valid spectra are sufficient for a reliable result. Results from an earlier study confirm this finding.22
In addition to the comparison of the non-invasive measurement with other means to assess the ZnPP value, we compared the measured ZnPP values with other ID parameters. For the investigated patient group, ZnPP measured directly in blood had a sensitivity and specificity of 92 and 90%, respectively, and NPV and PPV of 99 and 58%, respectively, for detecting ID as defined by the sTfR. A similar performance was found for the non-invasive ZnPP determination with a sensitivity and specificity of 67 and 97%, respectively, and NPV and PPV of 94 and 80%, respectively. Since only a small number of subjects (n = 10) were in the IDE and IDA groups, these parameters are determined only with large CIs. Still, the values show that ZnPP correlates well with the sTfR. This is expected since both parameters are elevated in the same stage of ID, where ID starts to have an impact on the erythropoiesis (IDE).33,34 For ID, mildly elevated ZnPP values were found only for few subjects, while most subjects had normal ZnPP values. For IDE, all ZnPP values were elevated. For IDA, a wide range of ZnPP values were found, with most ZnPP values elevated and ZnPP values above 300 µmol/mol heme. The group of anemic children without evidence for ID (normal ferritin and sTfR) had also normal ZnPP.
While these findings are in alignment with the literature,20 and support the usefulness of ZnPP and the non-invasive measurement method to screen for ID, larger studies are desirable for corroboration and to establish appropriate reference ranges for children, especially in risk groups for ID. Furthermore, the hospitalized patients with different diagnoses are not representative of a normal childhood population. For a comprehensive assessment of the iron status, a more complete set of ID parameters including transferrin saturation and hepcidin would be desirable. To estimate the full effect of inflammation, the measurement of both CRP and α-1-acid glycoprotein are recommended, especially for children.35 This was not possible in the present study due to an insufficient amount of left-over blood.
All biomarkers for ID are affected by the inflammatory response to infection, and may be influenced by conditions other than ID.36,37 Consequently, to diagnose ID in the best possible way, an extended set of different biomarkers is necessary. This is not feasible for screening, where time, costs, and ease of application play a major role, typically allowing only the determination of a single parameter. The best single parameter for ID screening may depend on the setting. For use in urban pediatric centers in the United States, ZnPP was suggested as suitable screening parameter for ID.38 In regions endemic for malaria and other infections, the World Health Organization also recommends measurement of ZnPP as the preferred indicator to screen children for ID.39 To date, the only other indicator for ID that can be measured non-invasively and at low cost is hemoglobin. However, hemoglobin has only a PPV of ~35% for ID,15,16 which is significantly lower than the 80% for non-invasive ZnPP measurements in our study. The combination of ZnPP with hemoglobin measurements can further improve the accuracy for ID screening in some settings, as was recently shown for Kenyan pre-school children.34
The present prototype device for the measurement is easily portable, robust, and has only a low power consumption below 7W (without tablet computer) with a supply voltage of 5V, making battery operation straightforward. Additionally, it does not need any chemicals or other disposables, except for potentially a single-use plastic cover in front of the measurement fiber to ensure hygenic measurements also without careful desinfection procedures. We therefore see no hurdles for the use of the device in resource-limited settings.
Conclusions
The present investigation demonstrates that non-invasive detection of ZnPP at the lower lip is reliably possible for children aged 9 months to 5 years, irrespective of their skin color. This novel method has the potential to improve the screening situation for ID in children by enabling simple and fast non-invasive measurements at the point of care.
References
Global Burden of Disease Pediatrics Collaboration, Kyu, H. H. et al. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: findings from the global burden of disease 2013 study. JAMA Pediatr. 170, 267–287 (2016).
Kassebaum, N. J. et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 123, 615–624 (2014).
Gupta, P. M., Perrine, C. G., Mei, Z. & Scanlon, K. S. Iron, anemia, and iron deficiency anemia among young children in the United States. Nutrients 8, 330 (2016).
Drakesmith, H. & Prentice, A. M. Hepcidin and the iron-infection axis. Science 338, 768–772 (2012).
Pasricha, S. R., Low, M., Thompson, J., Farrell, A. & De-Regil, L. M. Iron supplementation benefits physical performance in women of reproductive age: a systematic review and meta-analysis. J. Nutr. 144, 906–914 (2014).
Lozoff, B. et al. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr. Rev. 64, S34–S91 (2006).
Osendarp, S. J., Murray-Kolb, L. E. & Black, M. M. Case study on iron in mental development—in memory of John Beard (1947–2009). Nutr. Rev. 68(Suppl. 1), S48–S52 (2010).
Madan, N., Rusia, U., Sikka, M., Sharma, S. & Shankar, N. Developmental and neurophysiologic deficits in iron deficiency in children. Indian J. Pediatr. 78, 58–64 (2011).
Beard, J. L. Why iron deficiency is important in infant development. J. Nutr. 138, 2534–2536 (2008).
Lukowski, A. F. et al. Iron deficiency in infancy and neurocognitive functioning at 19 years: evidence of long-term deficits in executive function and recognition memory. Nutr. Neurosci. 13, 54–70 (2010).
Starnberg, J., Norman, M., Westrup, B., Domellöf, M. & Berglund, S. K. Lower cognitive test scores at age 7 in children born with marginally low birth weight. Pediatr Res. 83, 1129–1135 (2018).
Baker, R. D. & Greer, F. R. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics 126, 1040–1050 (2010).
Recommendations to prevent and control iron deficiency in the United States. Centers for disease control and prevention. MMWR Recomm. Rep. 47, 1–29 (1998).
Institute of Medicine (US) Committee on the Prevention, Detection, and Management of Iron Deficiency Anemia Among U.S. Children and Women of Childbearing Age 1993 Recommended Guidelines for Preventing and Treating Iron Deficiency Anemia in Infants and Children. in Iron Deficiency Anemia—Recommended Guidelines for the Prevention, Detection, and Management Among U.S. Children and Women of Childbearing Age (eds Earl, R. & Woteki, C.) (National Academies Press, Washington, DC, 1993).
Siu, A. L. Screening for iron deficiency anemia in young children: USPSTF recommendation statement. Pediatrics 136, 746–752 (2015).
White, K. C. Anemia is a poor predictor of iron deficiency among toddlers in the United States: for heme the bell tolls. Pediatrics 115, 315–320 (2005).
Mei, Z., Flores-Ayala, R. C., Grummer-Strawn, L. M. & Brittenham, G. M. Is erythrocyte protoporphyrin a better single screening test for iron deficiency compared to hemoglobin or mean cell volume in children and women? Nutrients 9, 557 (2017).
Mei, Z., Parvanta, I., Cogswell, M. E., Gunter, E. W. & Grummer-Strawn, L. M. Erythrocyte protoporphyrin or hemoglobin: which is a better screening test for iron deficiency in children and women? Am. J. Clin. Nutr. 77, 1229–1233 (2003).
Labbe, R. F., Vreman, H. J. & Stevenson, D. K. Zinc protoporphyrin: a metabolite with a mission. Clin. Chem. 45, 2060–2072 (1999).
Hastka, J., Lasserre, J. J., Schwarzbeck, A., Reiter, A. & Hehlmann, R. Laboratory tests of iron status: correlation or common sense? Clin. Chem. 42, 718–724 (1996).
Blumberg, W. E., Eisinger, J., Lamola, A. A. & Zuckerman, D. M. The hematofluorometer. Clin. Chem. 23, 270–274 (1977).
Hennig, G. et al. Non-invasive detection of iron deficiency by fluorescence measurement of erythrocyte zinc protoporphyrin in the lip. Nat. Commun. 7, 10776 (2016).
Fitzpatrick, T. B. The validity and practicality of sun-reactive skin types i through vi. Arch. Dermatol. 124, 869–871 (1988).
Mei, Z. et al. Serum soluble transferrin receptor concentrations in US preschool children and non-pregnant women of childbearing age from the National Health and Nutrition Examination Survey 2003–2010. Clin. Chim. Acta 413, 1479–1484 (2012).
Suominen, P., Punnonen, K., Rajamaki, A. & Irjala, K. Serum transferrin receptor and transferrin receptor–ferritin index identify healthy subjects with subclinical iron deficits. Blood 92, 2934–2939 (1998).
Hennig, G. et al. Dual-wavelength excitation for fluorescence-based quantification of zinc protoporphyrin IX and protoporphyrin IX in whole blood. J. Biophotonics 7, 514–524 (2014).
Myers, B., Walker, A. & Davies, J. M. The utility of the zinc-protoporphyrin assay as an initial screen for iron-deficient erythropoiesis. Hematol. J. 3, 116–117 (2002).
Rettmer, R. L. et al. Zinc protoporphyrin/heme ratio for diagnosis of preanemic iron deficiency. Pediatrics 104, e37–e37 (1999).
Siegel, R. M. & LaGrone, D. H. The use of zinc protoporphyrin in screening young children for iron deficiency. Clin. Pediatr. 33, 473–479 (1994).
Buhrmann, E., Mentzer, W. C. & Lubin, B. H. The influence of plasma bilirubin on zinc protoporphyrin measurement by a hematofluorimeter. J. Lab. Clin. Med 91, 710–716 (1978).
Schifman, R. B. & Finley, P. R. Measurement of near-normal concentrations of erythrocyte protoporphyrin with the hematofluorometer: influence of plasma on “front-surface illumination” assay. Clin. Chem. 27, 153–156 (1981).
Hastka, J., Lasserre, J. J., Schwarzbeck, A., Strauch, M. & Hehlmann, R. Washing erythrocytes to remove interferents in measurements of zinc protoporphyrin by front-face hematofluorometry. Clin. Chem. 38, 2184–2189 (1992).
Labbe, R. F. & Dewanji, A. Iron assessment tests: transferrin receptor vis-a-vis zinc protoporphyrin. Clin. Biochem. 37, 165–174 (2004).
Teshome, E. M., Prentice, A. M., Demir, A. Y., Andang’o, P. E. A. & Verhoef, H. Diagnostic utility of zinc protoporphyrin to detect iron deficiency in Kenyan preschool children: a community-based survey. BMC Hematol. 17, 11 (2017).
Thurnham, D. I. et al. Adjusting plasma ferritin concentrations to remove the effects of subclinical inflammation in the assessment of iron deficiency: a meta-analysis. Am. J. Clin. Nutr. 92, 546–555 (2010).
WHO & CDC. Assessing the Iron Status of Populations (WHO Press, Geneva, Switzerland, 2007).
Brittenham, G. M. in Hematology: Basic Principles and Practice (eds Hoffman, R. et al.) 437–449 (Elsevier Health Sciences, Amsterdam, 2013).
Magge, H., Sprinz, P., Adams, W. G., Drainoni, M. L. & Meyers, A. Zinc protoporphyrin and iron deficiency screening: trends and therapeutic response in an urban pediatric center. JAMA Pediatr. 167, 361–367 (2013).
WHO. Conclusions and recommendations of the WHO Consultation on prevention and control of iron deficiency in infants and young children in malaria-endemic areas. Food Nutr. Bull. 28, S621–S627 (2007).
Acknowledgments
We thank H.D. for his support in the practical implementation of the study. This work was financially supported, in part, by a subaward from Columbia University in the City of New York, and EXIST Forschungstransfer by the German Federal Ministry for Economic Affairs and Energy (grant number: 03EFFBY109).
Author information
Authors and Affiliations
Contributions
CH and GH designed and constructed the instrument, helped conceptualizing and designing the study, performed the statistical analyses, drafted the initial manuscript, and reviewed and revised the manuscript. FM conducted the patient measurements, helped drafting the initial manuscript, and reviewed the manuscript. HS designed the instrument, conceptualized and designed the study, and reviewed and revised the manuscript. LMH and MV conceptualized and designed the study, supervised the blood sample measurements and data collection, and reviewed the manuscript. RS helped conceptualizing and designing the study, gave advice for statistical analyses, and reviewed the manuscript. BK conceptualized and designed the study, supervised the patient measurements and data collection, and reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors have indicated they have no financial relationships relevant to this article to disclose. CH and GH are co-founders of the company FerroSens GmbH. The other authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Homann, C., Hennig, G., Maier, F. et al. Non-invasive measurement of erythrocyte zinc protoporphyrin in children. Pediatr Res 85, 349–354 (2019). https://doi.org/10.1038/s41390-018-0247-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0247-x
This article is cited by
-
Smartphone-based point-of-care anemia screening in rural Bihar in India
Communications Medicine (2023)
-
Can TSH level and premenstrual spotting constitute a non-invasive marker for the diagnosis of endometriosis?
BMC Women's Health (2021)