Abstract
Background
Langerhans cell histiocytosis (LCH) is a histiocytic disorder driven by a constitutive activation of the MAPK signaling pathway in myeloid cells. In 50–60% of cases, it is caused by the BRAFV600E mutation. There is evidence that levels of BRAFV600E in the peripheral blood of patients with LCH correlate with disease burden and could be used as marker for disease extent and response to therapy. However, there is currently no consensus on how testing for minimal disseminated disease should be performed.
Methods
Different approaches to determine the mutation load in patients with LCH were assessed and longitudinal evaluation of patient DNA during treatment with chemotherapy and/or the RAF inhibitor vemurafenib was performed. DNA was isolated from whole blood, different leukocyte subsets, and circulating cell-free DNA (ccf-DNA).
Results
We show that determining BRAF levels from whole blood is superior to using ccfDNA. Furthermore, it is important to identify the clinically relevant BRAF-mutated cellular subpopulations such as CD14+ monocytes or CD1c+ DCs, since other blood cells can also harbor the mutation and therefore confound whole blood or ccfDNA measurements.
Conclusion
Our data support the view that single-agent treatment with an RAF inhibitor reduces disease activity but does not cure LCH.
Similar content being viewed by others
Introduction
Langerhans cell histiocytosis (LCH) is a myeloid neoplasm characterized by the accumulation of CD1a+CD207+ (langerin+) positive cells resembling histiocytes and a prominent inflammatory infiltrate.1,2 Any age group may be affected, but its most severe clinical course predominantly affects young children. The clinical course of LCH presents in a wide range, including both spontaneous regression of single lesions as well as rapid dissemination and life-threatening multisystem disease that needs to be treated with systemic chemotherapy and in some cases hematopoietic stem cell transplantation. Targeted therapies with RAF or MEK inhibitors are emerging as important part of the treatment, although it is still unclear how they should be incorporated in current treatment regimens. One major problem in the management of LCH is the very high number of patients who are refractory to initial treatment or reactivate within a few years.3 The current international treatment protocol for LCH in children (“LCH-IV”, EudraCT Nr.: 2011-001699-20) comprises empiric multimodal chemotherapy with treatment decisions that solely rely on clinical presentation. Biological markers that could assess disease burden and measure treatment response would significantly improve decision-making and treatment of these patients by enabling more personalized treatment of children with LCH.
Genomic analyses revealed constitutive activation of MAPK signaling in a significant number of LCH patients.4,5 In 50–60% of cases, the MAPK activation is caused by the BRAFV600E mutation. The BRAFV600E mutation has been described in several cancer types, predominantly in melanoma, papillary thyroid tumors, and colorectal cancer. During the last years, the detection of mutated BRAF was introduced as a marker for prognosis and treatment outcome, therefore several detection methods were established.6,7,8,9,10 Recent studies have presented several approaches using BRAFV600E levels in children with LCH to monitor disease burden and to predict treatment outcome.6,11,12,13,14 In addition, an association of BRAFV600E status with a more severe clinical outcome and increased resistance to first-line chemotherapy was presented by Héritier et al.11 The same group evaluated cell-free BRAFV600E as a biomarker for monitoring the response to therapy and obtained promising results.12 In our previous reports we used a method called Intplex, a refined allele-specific quantitative PCR using SYBRgreen based on the protocol published by the group of Thierry.6,7
There is no consensus on how BRAF should be determined in the peripheral blood of patients with LCH: it is unclear whether ccf DNA, whole-blood DNA, or cellular DNA should be determined. Furthermore, there are different methods to determine BRAF in the peripheral blood, among them were allele-specific SYBRGreen PCR, Taqman Mutation Detection Assay and digital droplet PCR (ddPCR). In view of the large impact BRAF measurements could have on future treatment protocols for children with LCH and the necessity to align protocols between different laboratories, we have assessed different methods and approaches and propose an approach that could be used by different laboratories to assess BRAF in patients with histiocytoses.
Materials and methods
Patients
This study was conducted in accordance with the Declaration of Helsinki after approval by the local IRB, and written and informed consent of the parents.
Molecular analysis
Peripheral blood mononuclear cells (PBMCs) from patients were isolated by density-gradient centrifugation using Ficoll-Paque (GE Healthcare, UK). DNA was isolated either from whole blood or flow cytometric sorted cell subsets using the QIAamp DNA blood mini kit (Quiagen, Germany). ccfDNA was isolated using the ChargeSwitch gDNA 1 ml Serum Kit (CS11040, ThermoFisher Scientific, MA).
Detection of BRAF V600E
BRAFV600E allele-specific PCR using SYBRgreen was performed as described previously.6 Briefly, qRT-PCR was performed using Maxima SYBR Green/ROX qPCR Master Mix (Thermo Scientific). Assays were performed in triplicate using primers specific for BRAFwt and BRAFV600E. ABI 7500 Fast Detection System (Applied Biosystems, Foster City, CA) was used. Percentage of mutated allele was calculated as m% = (Conc MUT/Conc REF). For the Taqman® mutation detection assays: Mutation Allele Assay: BRAF_476_mu -4465804 Hs00000111_mu and wild-type allele reference Assay - BRAF_476_wt -4465804 Hs00000110_wt (ThermoFisher Scientific) were used according to the manufacturer’s description. Assays were performed in triplicate using the Applied Biosystems 7500 Fast Detection System (Applied Biosystems, Foster City, CA). ddPCR was performed using the Mutation Assay BRAF p.V600E c.1799T-A, Human (dHsaMDV2010027 Biorad, Germany) and the QX200 Droplet Digital PCR System (Biorad). For samples containing 1% or less BRAFV600E-mutated cells, three wells were pooled, for amounts above 1% single wells were analyzed according to the manufacturer’s description
Cell sorting, flow cytometric techniques and chimerism analysis
All chimerism analyses were performed on flow-sorted CD45+ leukocyte subtypes defined by their unique antigen co-expression. Myeloid cells were CD14+ monocytes and HLA-DR+CD1c+CD11c+ DCs; T-cells were defined by their positivity for CD3+CD4+ and CD3+CD8+. Cell sorting was performed on a FACSAria instrument (BD Biosciences, San Jose, CA). The FACSDiVa software (BD Biosciences) was used for data evaluation. The number of cells isolated for subsequent FISH analysis ranged from 1000 to 10,000. Chimerism analyses from gender-mismatched donor were analyzed using Dual-color FISH performed according to the standard procedures15 with commercially available probes specific for the centromeric and heterochromatic regions of the X and Y chromosomes, respectively. Depending on the number of cells available, up to 500 cells were analyzed within each sorted cell fraction.
Results
In a first set of experiments, we compared three widely used methods to determine levels of mutated BRAF: an allele-specific PCR method,7 a commercially available Taqman Mutation Detection Assay which was already used in several studies,10,16 and a commercially available digital droplet PCR Kit.17 To evaluate the three methods, we diluted genomic DNA from the A673 cell line, which contains a heterozygous BRAFV600E mutation with wild-type DNA extracted from blood of healthy donors ranging from 100% mutated cells to 0.01% mutated cells and performed the PCR reactions in parallel. As depicted in Fig. 1a, the SYBRGreen-based allele-specific PCR and ddPCR correlate well to the cell amounts used in the reaction. In contrast, an overestimation of the mutational load was observed with the Taqman Mutation Detection Assay, especially in the lower range (Fig. 1b). Lower levels of the mutated allele (≤0.05% of cells) are below the detection limit of the Taqman method (Fig. 1b, c). In contrast, ddPCR and the allele-specific SYBRGreen PCR precisely reflect the amount of cells used down to a level of around 0.01% mutated BRAF allele. Therefore, both these methods are equally suited to determine BRAFV600E in the peripheral blood.
Comparison of three allele-specific PCR methods. The percentage of measured BRAFV600E mutated cells (Y-axis) is depicted versus the percentage of BRAFV600E mutated cells used in the PCR reactions (X-axis) for a 100 to 0.01%, b 2 to 0.01% and c 0.1 to 0.01% BRAFV600E-positive cells used. Black: calculated amount of cells used; Green: PCR reaction using SYBRGreen; Purple: PCR reaction using Taqman Mutation Detection Assay; Red: ddPCR reaction
We then performed sequential sample analysis during therapy and follow-up of five BRAFV600E biopsy-positive patients using the allele-specific PCR (Fig. 2). Clinical characteristics of the studied patients are summarized in Table 1.
Longitudinal assessment of BRAFV600E-positive cells in patients with LCH. Patients a 134 b 107 and c 73 with MS-LCH. Patients d 202 and e 216 were diagnosed with multifocal bone lesions. All patients were BRAFV600E positive in their biopsy samples. Y-axis represents the percentage of circulating BRAFV600E mutated cells during therapy. X-axis represents days after therapy start. SCT Stem cell transplantation, IC1 Initial Course 1, IC2 Initial Course 2, CR Clinical Remission, R Relapse
Patient 134 was diagnosed with multisystem LCH (MS-LCH) with involvement of skin and liver and low levels of mutated BRAF in his PB (0.19%) were detected (Fig. 2a). Chemotherapy with vinblastine and prednisolone for 12 weeks (IC 1 and 2) resulted in improvement of skin and remission of liver disease. After additional 24 weeks of treatment with vincristine, prednisolone, and cytarabine (Stratum II), his skin improved even further. When continuation therapy was started, the patient was clinically in remission but his BRAFV600E levels had increased to 3.5%. About 40 days later, the patient relapsed and deteriorated clinically with involvement of skin, liver, spleen, and the hematopoietic system. At the molecular level, BRAFV600E peaked at 15.1% (Fig. 2a). Because of his critical condition, treatment with vemurafenib was started, which lead to a rapid clinical response and a moderate decrease of BRAFV600E levels. With vemurafenib as single-agent, stable very good partial remission of skin, liver, spleen, and the hematopoietic system over a period of 20 months is observed, but BRAFV600E is still detectable (7.2%). Up to now, the patient is still treated with the inhibitor.
Patient 107 was reported previously until the timepoint he received a hematopoietic stem cell transplantation (HSCT).6 This patient had MS-LCH, which was refractory to chemotherapy, subsequently received vemurafenib, and was then transplanted from a matched sibling donor using a reduced intensity-conditioning (RIC) regime. One month after HSCT, the patient was clinically well, showed no signs of disease and the amount of BRAFV600E-positive cells was low (between 0.01 and 0.7%), but still detectable. Vemurafenib was discontinued 1 month after transplantation. While the patient stayed clinically stable for 9 months, BRAFV600E levels started to increase steadily 1 month after cessation of treatment with vemurafenib. Nine months after vemurafenib discontinuation (day 755 after initial start with vemurafenib) the patient relapsed, presenting osteolytic lesions in the skull. Therapy with vinblastine/prednisolone according to the LCH-IV protocol was re-administered, but the clinical condition worsened involving febrile neutropenia, clostridia enteritis, EBV reactivation and the mutational load increased up to 10%. At that time (day 822 after initial vemurafenib start) vemurafenib was prescribed again and the patient stabilized soon accompanied by a drop in his BRAFV600E levels. He is now clinically well and is treated with vemurafenib every other day (Fig. 2b). The patient still has measurable levels of BRAFV600E in the peripheral blood.
Patient 73 was diagnosed with MS-LCH with involvement of lungs, skin, bone, and gingiva. Before treatment, 0.3% of his peripheral blood cells were BRAFV600E positive. During IC1 and 2, bone involvement was stable, but the skin disease got worse. According to the LCH-IV protocol, the patient was therefore switched to Second-line Initial Therapy (Stratum II in LCH-IV). With this therapy his skin and bone LCH improved, accompanied by a drop of BRAFV600E detectable in his PB (0.02%). At the end of therapy he was in clinical remission and BRAFV600E levels in the peripheral blood had decreased below the detection limit (0.01%) (Fig. 2c).
Patient 202 presented with multifocal bone lesions and 0.034% BRAFV600E-positive cells. After IC 1 and 2 the patient clinically improved and accordingly continuation therapy was initiated. He was in clinical remission after completion of the therapy. At the same time BRAFV600E was below the detection limit (0.009%) (Fig. 2d).
Patient 216 was diagnosed with LCH with multifocal bone lesions. Administration of IC1 and 2 resulted in an improved clinical condition. After continuation treatment the patient was disease free. Although the BRAFV600E mutation was identified in the biopsy, the mutation was never detected in the patients peripheral blood (Fig. 2e).
Taken together, patients 73, 202, and 216, who all were BRAFV600E negative at the end of their therapy, have not relapsed until now (9 months, 10 months and 4 months after the end of therapy). In contrast, patients relapsed if BRAFV600E was still detectable at the end of therapy, even though BRAFV600E levels dropped drastically and no clinically apparent signs of disease were observed. These observations suggest that BRAFV600E mutation load could serve as a predictive marker of LCH relapse and should therefore be carefully monitored. Furthermore, vemurafenib reduced BRAFV600E levels, but did not eliminate BRAFV600E in two patients even after long-term therapy.
Next, we longitudinally assessed BRAFV600E levels in circulating cell-free DNA of three patients with BRAFV600E-positive MS-LCH (Fig. 3). Overall, the pattern of cf BRAFV600E levels reflects the pattern observed with DNA isolated from whole peripheral blood. In patient 134, while ccf mutational load was as low as in PB at time of diagnosis, BRAFV600E levels increased up to 31% after administration of vemurafenib. While ccfBRAFV600E varied between 4 and 31%, BRAFV600E remained at comparable values in DNA isolated from whole blood (between 6 and 10%) during treatment, reflecting the stable clinical presentation of this patient (Fig. 3a). For patients 107 (Fig. 3b) and 26218 (Fig. 3c), amounts of ccfBRAFV600E again varied to a much higher degree compared to PB levels. The most prominent variation occurred around day 100 after the start of vemurafenib treatment of patient 262. In contrast to the whole blood BRAFV600E level, which was 5.4%, ccf mutation load was 31.2%. Blood sampling was performed using standard EDTA tubes and not cell-free DNA collection tubes, which preserve ccfDNA and inhibit the lysis of nucleated cells, which would contaminate ccfDNA with cellular DNA.19 Therefore these data have to be interpreted with caution and underline the necessity of a strictly regulated protocol, preferably using ccf-DNA collection tubes and short and temperature-stable transportation.
Comparison of BRAFV600E levels in whole blood and plasma. DNA was isolated either from whole blood, or circulating cell-free DNA from plasma of three patients a 134, b 107, and c 262 with MS-LCH. Y-axis represents the percentage of circulating BRAFV600E-mutated cells during therapy. X-axis represents days after therapy start. SCT Stem cell transplantation, IC1 Initial Course 1, IC2 Initial Course 2, whole blood in black, plasma in red, CR Clinical Remission, R Relapse
In patients with LCH, mutated BRAF can be detected in different cell types such as monocytes, dendritic cells, or lymphocytes.10,20 It is unclear, which and if one of these populations contribute to LCH-pathogenesis and might contain precursors of the lesional LCH cells. We therefore tested whether specific cell populations reflected the clinical situation of a given patient better than others. To this end, we sorted defined cell populations using flow cytometry and analyzed the mutational load in these populations in three patients whenever possible. Limitations in this case were either low volume of blood drawn, coagulated blood, or cytopenia at time of blood sampling. As described earlier, the amount of mutated BRAFV600E in the peripheral blood of patient 134 was initially very low (0.19%). However, when we analyzed CD14+ monocytes and CD1c+ DCs—two cell populations that might contain the progenitors of the CD1a+CD207+ LCH cells10,21,22 - 3.9% of CD14+ monocytes and 1.3% of CD1c+ DCs (mDCs) were BRAFV600E positive. The highest observed level of BRAFV600E in these populations was detected at about 40 days on vemurafenib (CD14+ 26.2%, CD1c+ DC 12.0%). A drop of mutated BRAF levels in whole PB was accompanied by a small reduction of BRAF in monocytes and CD1c+ DC at day 130 after start with vemurafenib, but mutated BRAF nevertheless stayed relatively high (day 356 CD14+ 17.3%, CD1c+ 14.1%) (Fig. 4a).
Determination of BRAFV600E levels in CD14+ monocytes and CD1c+ DCs. BRAFV600E mutational load for patient 134 was determined from whole blood and flow cytometry sorted CD14+ monocytes (CD14) and CD1c+ DCs (mDC). Y-axis represents the percentage of circulating BRAFV600E-mutated cells during therapy. X-axis represents days after therapy start. IC1 Initial Course 1, IC2 Initial Course 2, CD14+ monocytes in green, CD1c DC+ in red, CR Clinical Remission, R Relapse
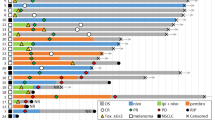
However, the possibly most interesting results were obtained when analyzing different peripheral blood cell populations of patient 107. In contrast to patient 134, the mutational load in monocytes and CD1c+ DC was lower compared to whole blood after initial treatment with vemurafenib (Fig. 5a). If CD14+ monocytes and CD1c+ DC account only for a minor proportion of BRAFV600E-positive cells, which other cell populations might be mutated? To address this question, we analyzed CD16+ monocytes, granulocytes, and T-cell subpopulations in this patient. While CD16+ monocytes and granulocytes showed only minimal positivity (data not shown), a high percentage of T-cells carried the BRAF mutation. After the first cessation of vemurafenib when total BRAF in whole blood was rising to around 10%, 12.4% of CD8+ and 46.8% of CD4+ T-cells were BRAFV600E positive (Fig. 5b). These levels increased further and reached their peak at the time when the percentage of total BRAFV600E-mutated cells was at a maximum, about 850 days after initial start of vemurafenib (13.2% in PB, 79.2% in CD4+, 23.0% in CD8+). When the mutational load in the peripheral blood decreased after re-administration of vemurafenib to 3.3%, also the amount of BRAFV600E in CD4+ (28.6%) and CD8+ (5.8%) declined. Therefore, the levels of BRAFV600E in the peripheral blood of this patient are caused primarily by BRAFV600E-positive T-cells. This finding is important when considering that LCH is currently categorized as myeloid neoplasm that might originate from CD14+ monocytes or CD1c+ DCs.10,20,22,23
Determination of BRAFV600E levels in cell subpopulations and chimerism analysis after SCT. a BRAFV600E mutational load for patient 107 was determined from whole blood and flow cytometry sorted CD14+ monocytes (CD14), CD1c+ DCs (mDC) and together with b CD3+, CD4+, and CD8+ T-cells. Y-axis represents the percentage of circulating BRAFV600E-mutated cells during therapy. X-axis represents days after therapy start. c Chimerism analysis for flow cytometry sorted CD14+ monocytes (CD14), CD1c+ DCs (mDC), CD3+, CD4+ and CD8+ T-cells. Y-axis represents the percentage of % cells from the recipient. X-axis represents days after therapy start. d BRAFV600E mutational load for patients 107 (black), 134 (gray) and 289 (white) were determined from whole blood (107, 134) and bone marrow aspirate (289) and flow cytometry sorted CD14+ monocytes (CD14), CD1c+ DCs (mDC), CD4+, and CD8+ T-cells. SCT stem cell transplantation, IC1 initial course 1, CR clinical remission, R relapse
We therefore took a closer look at the CD14+ monocytes in this patient. Low levels of BRAFV600E were detected in monocytes after transplantation during the time the patient was in a clinical stable condition, but were elevated (0.9%) at time of relapse. In contrast, during an increase of BRAFV600E in T-cells (and consequently also in whole blood) around day 822, the BRAFV600E levels were low in CD14+ monocytes, perhaps reflecting the clinical remission of the patient (Fig. 5a). Taken together, these data show that while the dynamics of total BRAFV600E and its levels in the T-cell subpopulations are similar, they do not necessarily correlate with the clinical picture, which might be reflected more accurately by the BRAFV600E content in myeloid cells. Chimerism in peripheral blood populations showed that CD14+ monocytes and CD1c+ DCs were mainly from the donor, whereas, T-cells were predominantly from the recipient (Fig. 5c). Furthermore, 3.4% of CD34+ stem cells were from the recipient, indicating that a pool of potentially BRAFV600E-positive cells remained after transplant, which could potentially induce an LCH relapse.
To assess whether BRAFV600E can also be detected in other patients, we analyzed CD4+ and CD8+ T-cells, CD14+ monocytes, and CD1c+ DCs in two children with MS-LCH at timepoints when they were clinically stable but had high levels of BRAFV600E in whole blood analysis. (134: 8.2% ~1 year after clinical remission, 289: 12.5% about 180 days after clinical remission). Patient 289, presented with MS-LCH with involvement of skin, liver, spleen, bone marrow and lymph nodes and initial BRAFV600E levels of 30% in BM. Two weeks after start with vemurafenib, the patient went into clinical remission except for hepatosplenomegaly, which resolved after two more weeks of treatment. The amount of total BRAFV600E levels in the bone marrow decreased to 14% after two weeks, and varied between 8 and 12% during the next 178 days. However, no signs of disease were apparent during this time and the patient is still clinically well.
When we analyzed BRAFV600E levels in those two patients, we also observed high levels in CD4+ and CD8+ T-cells (134: 10.9% in CD4+ and 6.2% in CD8+ cells; 289: 34.5% in CD4+ and 39.0% in CD8+ cells Fig. 5d). Together, these data show that non-myeloid cells that carry the mutation can contribute to high levels of BRAFV600E in the peripheral blood.
Discussion
LCH is a highly heterogeneous disease with a broad range of clinical manifestations unified by the accumulation of CD1a+CD207+ histiocytes and constitutive activation of the MAPK signaling pathway.23 In 50–60% of cases, the MAPK activation is caused by the BRAFV600E mutation.4 Promising studies demonstrate the use of BRAFV600E measurements in patients to assess therapy response and predict treatment outcome.12 Therefore, a prospective international trial that incorporates the analysis of BRAFV600E in the peripheral blood of LCH patients during therapy is urgently needed. In order to do this, the question which detection method should be used for the assessment of circulating BRAFV600E needs to be solved. Here we tested three different qPCR-based methods. While the commercially available Taqman Mutation Allele Assay leads to an up to 7-fold overestimation of the mutational load at percentages above 1%, BRAFV600E mutations are not detected at all below 0.05%, which is in line with the detection limit of 0.1%, stated by the company. The method based on the previously published method Intplex7 using a phosphate-modified blocking oligonucleotide targeting the wild-type allele and ddPCR both demonstrated high accuracy also at low levels of mutated allele.
In addition to whole blood and cellular DNA, we have also evaluated the use of ccfDNA, an established biomarker in a wide range of different solid tumors.9,24 Although the overall pattern of BRAFV600E levels correlated with the pattern determined using whole-blood DNA, we observed several outliers showing elevated BRAFV600E amounts at times of clinical stable conditions. These discrepancies might be explained by pre-analytical inaccuracies such as longer time spans between drawing of the blood and isolation of ccfDNA and or changes in temperature during transportation to the laboratory. The influence of time on DNA concentration was previously reported with almost a 3-fold increase of ccfDNA amount 24 h post blood drawing and an increase to over 60-fold by 96 h in one study.25 For the present study, blood sampling was performed using standard EDTA tubes (similarly to the study of Heritier12) and not ccfDNA collection tubes. The use of these collection tubes would be highly recommended for further studies that aim to include patients from a large number of treatment centers. Alternatively, EDTA tubes could be used if blood samples are immediately processed and frozen plasma (−80 °C) is shipped to the analyzing institution. This requires a standardized centrifugation protocol, which has to be implemented at each hospital sending blood or plasma for analysis. Children in this study were on average 592 days old (ranging from 115 days to 1089 days) and the amount of blood received was on average 2 ml. Swinkels and colleagues reported that in addition to pre-analytical factors including centrifugal force and pipetting efficacy, also the amount of blood collected influences efficiency of removal of contaminating cellular DNA from plasma.26 One problem is the low concentration of ccfDNA isolated from plasma. Although the plasma of cancer patients in general contains higher amounts of ccfDNA in comparison to healthy controls, the amount varies considerably depending on the type and stage of cancer. For instance, in adults with LCH a mean quantity of 316.5 pg/ml (median, 290.4 pg/ml) was detected.14 In our opinion however, the major disadvantage of BRAFV600E analysis from both plasma and whole blood is the loss of the information which of the cell populations contain mutated BRAF in a given patient. BRAFV600E can be detected in several cell subsets, and the implication of the presence of a mutated allele for LCH pathogenesis in the specific cell subsets is not known yet. For example, in patient 107 the highest BRAF levels were detected in T-cells (up to 70% of CD4+ T-cells), which also seemed to be the largest contributing cell subset to the amount of mutated BRAF measured in peripheral blood and plasma. Therefore this patient had high levels of mutated BRAF when just analyzing total DNA or ccf-DNA from the PB, even though he was clinically stable. Since the relevance of the mutation in T-cells in LCH is unclear (it is unlikely that BRAF mutated T cells contribute to the development of CD1a+CD207+ LCH cells), it is likely that measurement of ccf-DNA or whole blood is inaccurate in some patients to measure disease activity. Therefore, precise monitoring of LCH-relevant populations such as CD14+ monocytes or CD1c+ DCs might be necessary in some patients to obtain accurate results. We propose that in future collaborative trials that study BRAF levels in the peripheral blood of patients with LCH should take this into account and investigate subset-specific levels in addition to bulk BRAF.
Nevertheless, there is a correlation of BRAFV600E levels and clinical outcome and response. In accordance with the results of Héritier et al.11 and our own recent study,6 we observed that some patients who were treated by conventional chemotherapy or BRAF inhibitors and showed clinical remission accompanied by a decrease of BRAFV600E but still remained positive for BRAFV600E, relapsed after the cessation of their therapy. This suggests that treatment reduces disease activity but does not lead to an eradication of the disease at the molecular level, which could lead to a relapse. In line, patients with no detectable BRAFV600E in the peripheral blood at the end of therapy (below 0.01%) remained in remission so far (maximum time of observation 10 months).
In our patient who was transplanted, 3.4% of CD34+ stem cells were from the recipient, which might be the cause of the relapse after SCT. We therefore question whether reduced intensity conditioning is the best treatment approach for patients with high-risk LCH that receive allogeneic HSCT. The view of LCH as hematologic malignancy by many27 (but not all28), could support this view. Perhaps some patients with high-risk LCH should be treated with myeloablative conditioning.
Taken together, we suggest EDTA blood should be collected from patients with LCH. This enables both determining mutational content from whole blood and from different, sorted cell subsets. In our hands there is no difference in the sensitivity between ddPCR and the Intplex PCR, therefore both methods can be used to trace minute amounts of mutated BRAF in the peripheral blood. As next step, protocols need to be aligned between different laboratories and a collaborative study that tests whether BRAF can be used as marker for minimal disseminated disease in patients with LCH has to be initiated. Such efforts will ultimately improve clinical decision-making and help patients to receive the appropriate therapy.
References
Haroche, J. et al. Histiocytoses: emerging neoplasia behind inflammation. Lancet Oncol. 18, e113–e125 (2017).
Emile, J. F. et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood 127, 2672–2681 (2016).
Gadner, H. et al. Therapy prolongation improves outcome in multisystem Langerhans cell histiocytosis. Blood 121, 5006–5014 (2013).
Badalian-Very, G. et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood 116, 1919–1923 (2010).
Durham, B. H., Diamond, E. L. & Abdel-Wahab, O. Histiocytic neoplasms in the era of personalized genomic medicine. Curr. Opin. Hematol. 23, 416–425 (2016).
Kolenová. A., et al. Targeted inhibition of the MAPK pathway: emerging salvage option for progressive life-threatening multisystem LCH. Blood Adv. 1, 352–356 (2017)
Thierry, A. R. et al. Clinical validation of the detection of KRAS and BRAF mutations from circulating tumor DNA. Nat. Med. 20, 430–435 (2014).
Lopez-Rios, F. et al. Comparison of molecular testing methods for the detection of EGFR mutations in formalin-fixed paraffin-embedded tissue specimens of non-small cell lung cancer. J. Clin. Pathol. 66, 381–385 (2013).
Siravegna G., et al. Integrating liquid biopsies into the management of cancer. Nat. Rev. Clin. Oncol. 14, 531–548 (2017).
Milne P., et al. Hematopoietic origin of Langerhans cell histiocytosis and Erdheim Chester disease in adults. Blood 130, 167–175 (2017).
Heritier, S. et al. BRAF mutation correlates with high-risk langerhans cell histiocytosis and increased resistance to first-line therapy. J. Clin. Oncol. 34, 3023–3030 (2016).
Heritier, S. et al. Circulating cell-free BRAF(V600E) as a biomarker in children with Langerhans cell histiocytosis. Br. J. Haematol. 178, 457–467 (2017).
Janku, F. et al. BRAF V600E mutations in urine and plasma cell-free DNA from patients with Erdheim-Chester disease. Oncotarget 5, 3607–3610 (2014).
Kobayashi, M. & Tojo, A. The BRAF-V600E mutation in circulating cell-free DNA is a promising biomarker of high-risk adult Langerhans cell histiocytosis. Blood 124, 2610–2611 (2014).
Pichler, H. et al. Peripheral blood late mixed chimerism in leucocyte subpopulations following allogeneic stem cell transplantation for childhood malignancies: does it matter? Br. J. Haematol. 173, 905–917 (2016).
Yang, Y. et al. Detection of EGFR and BRAF mutations by competitive allele-specific TaqMan polymerase chain reaction in lung adenocarcinoma. Oncol. Lett. 15, 3295–3304 (2018).
Taylor, S. C., Laperriere, G. & Germain, H. Droplet digital PCR versus qPCR for gene expression analysis with low abundant targets: from variable nonsense to publication quality data. Sci. Rep. 7, 2409 (2017).
Heisig, A. et al. Vemurafenib in Langerhans cell histiocytosis: report of a pediatric patient and review of the literature. Oncotarget 9, 22236–22240 (2018).
Medina Diaz, I. et al. Performance of streck cfDNA blood collection tubes for liquid biopsy testing. PLoS One 11, e0166354 (2016).
Berres, M. L. et al. BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J. Exp. Med 212, 281 (2015).
Milne P., et al. CD1c+ blood dendritic cells have Langerhans cell potential. Blood 125, 470–473 (2015).
Schwentner R., et al. JAG2 signaling induces differentiation of CD14(+) monocytes into Langerhans cell histiocytosis-like cells. J. Leukoc. Biol. 1–11 (2018).
Allen, C. E., Merad, M. & McClain, K. L. Langerhans-cell histiocytosis. N. Engl. J. Med. 379, 856–868 (2018).
Schwarzenbach, H., Hoon, D. S. & Pantel, K. Cell-free nucleic acids as biomarkers in cancer patients. Nat. Rev. Cancer 11, 426–437 (2011).
Rothwell, D. G. et al. Genetic profiling of tumours using both circulating free DNA and circulating tumour cells isolated from the same preserved whole blood sample. Mol. Oncol. 10, 566–574 (2016).
Swinkels, D. W. et al. Effects of blood-processing protocols on cell-free DNA quantification in plasma. Clin. Chem. 49, 525–526 (2003).
Egeler, R. M. et al. Langerhans cell histiocytosis is a neoplasm and consequently its recurrence is a relapse: In memory of Bob Arceci. Pediatr. Blood Cancer 63, 1704–1712 (2016).
Braier, J. Is Langerhans cell histiocytosis a neoplasia? Pediatr. Blood Cancer 64, e26267 (2017).
Acknowledgments
The authors thank Dieter Printz, Julia Stemberger, Angela Schumich, and Elke Zipperer for flow cytometry analysis and cell sorting, and Oskar Haas, Karin Nebral, and Margit König for FISH analysis. This work was supported by a Clinical Investigator-driven grant from the St Anna Kinderkrebsforschung and the Histiozytosehilfe e.V.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schwentner, R., Kolenová, A., Jug, G. et al. Longitudinal assessment of peripheral blood BRAFV600E levels in patients with Langerhans cell histiocytosis. Pediatr Res 85, 856–864 (2019). https://doi.org/10.1038/s41390-018-0238-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0238-y
This article is cited by
-
Optimal timing of liver transplantation for liver cirrhosis caused by sclerosing cholangitis in a patient with Langerhans cell histiocytosis: a case report
International Journal of Hematology (2023)
-
Detection of BRAF V600E mutation in radiological Langerhans cell histiocytosis-associated neurodegenerative disease using droplet digital PCR analysis
International Journal of Hematology (2023)
-
The coming of age of Langerhans cell histiocytosis
Nature Immunology (2020)