Abstract
Background
Soluble forms of RAGE (sRAGE) have been found circulating in plasma and tissues. Evidence is accruing in human subjects linking levels of sRAGE to oxidative stress in many disorders. Because sickle cell disease (SCD) is a state of oxidative stress, we tested the hypothesis that circulating sRAGE levels may be involved in the vascular pathology of SCD.
Objectives
To determine the sRAGE levels in children and adolescents with SCD and investigate their association with markers of hemolysis, iron overload, and SCD-related organ complications.
Subjects and methods
The level of sRAGE was measured in 40 children and adolescent with SCD compared with 40 healthy controls using enzyme-linked immunosorbent assay (ELISA).
Results
sRAGE was significantly higher in patients compared with controls (p < 0.001) and was elevated in patients with history of stroke, acute lung syndrome, and frequency of sickling crisis or serum ferritin > 2500 (p < 0.05). Patients with high sRAGE levels are candidates for chelation. sRAGE was positively correlated with HbS% (r = 0.422, p = 0.007), LDH (r = 0.329, p = 0.038), and serum ferritin levels (r = 0.516, p = 0.001). Multivariable regression analysis proved that both HbS% and serum ferritin were significant independent factors affecting sRAGE level (p < 0.05).
Conclusion
Our findings suggest that sRAGE may be considered as a marker for vascular dysfunction in SCD patients.
Similar content being viewed by others
Introduction
Sickle cell disease (SCD) is a class of hemoglobinopathy, which results from a point mutation in a single gene, which results in a mutant B-globin protein (HbS), in which the sixth amino is changed from glutamic acid to valine. In the homozygous SCD (HbSS), and other compound heterozygous states such as sickle B-thalassemia, deoxygenated HbS molecules form polymers, which damage the red cell membrane and increase its rigidity.1
SCD induces chronic states of oxidative stress and inflammation. Several mechanisms contribute to the high oxidative burden in sickle cell patients, including1 the excessive levels of cell-free hemoglobin with its catalytic action on oxidative reactions,2 the characteristic recurrent ischemia-reperfusion injury,3 a chronic proinflammatory state, and4 higher autoxidation of HbS. All contributing to an increased generation of reactive oxygen species (ROS) potentially contributing to the characteristic widespread organ damage.2
Oxidative stress also results in increased production and accumulation of advanced glycation end products (AGEs), which are not only well-established markers of oxidative stress,3,4 but are themselves oxidatively active and have been demonstrated to play a role in the pathophysiology of hemolysis-related organ complications in SCD.5,6
These glycated end products primarily bind to their receptors (RAGE) that are transmembrane proteins that are a part of the immunoglobulin superfamily. RAGEs are upregulated in response to increased circulating levels of AGEs. Upon AGE-RAGE binding, RAGE activates multiple downstream cellular signaling cascade leading to the activation of nuclear factor-KB (NF-KB). Consequently, this causes increased expression of proinflammatory cytokines, chemokines, adhesion molecules, as well as enhanced oxidative stress that may culminate in local inflammation and tissue damage.7
Soluble forms of RAGE (sRAGE) exist in the circulation and correspond to the extracellular domain of RAGE lacking cytosolic and transmembrane domains. There are two mechanisms that have been identified to produce sRAGE. The first is the alternative splicing to remove the transmembrane region forming a splice variant of RAGE named endogenous secretory RAGE (es RAGE) and the other mechanism is proteolytical cleavage from the cell surface full-length RAGE mediated by disintegrins and matrix metalloproteinase(MMP)-9. This extracellular form is named cleaved RAGE (cRAGE).8
Because the balance between the synthesis of sRAGE and full-length RAGE significantly impacts intracellular signaling and may be important determinant of AGE-induced dysfunction,9 recent clinical researches has begun to investigate the potential significance of circulating sRAGE as a useful biomarker of RAGE mediated pathological conditions and as a novel approach to prevent or treat morbid complications of these disorders.10
To date, no study has been designed to test the hypothesis that sRAGE may be involved in the vascular pathology of SCD. Accordingly, we aimed in our work to determine the sRAGE levels in children and adolescents with SCD and investigate their association with markers of hemolysis, iron overload, and SCD-related organ complications.
Patients and methods
This case control cross sectional study included 40 patients with SCD recruited from the regular attendants of the Pediatric Hematology Clinic, Pediatric Hospital, Ain Shams University. Forty healthy subjects were enrolled as a control group.
Hemoglobin analysis was done using high performance liquid chromatography (HPLC) and confirmed by genotyping.11 An informed consent was obtained from the guardian of each patient or control before participation. The procedures were approved by the Ethical Committee of Human Experimentation of Ain Shams University, and are in accordance with the Helsinki Declaration of 1975.
Exclusion criteria were infection, chronic inflammatory condition other than SCD, complications unrelated to SCD, such as cardiovascular diseases, rheumatoid arthritis, or other autoimmune diseases, diabetes mellitus, or renal insufficiency.
At time of sample collection, all patients were in a steady state (defined as a period without pain or painful crisis for at least 4 weeks)2 and those who had sickling crisis (defined as musculo-skeletal pain which could not be explained except by SCD)12 were excluded. The frequency of sickling crisis in the previous year was divided into mild (defined as 2 or less episodes requiring medical visits) or severe (defined as 3 or more episodes requiring medical visits).13 Acute chest syndrome, which was defined as a new radiodensity on chest radiograph accompanied by fever and/or respiratory symptoms.14 Diagnosis was confirmed by presence of radiographic changes in chest X-Ray. Stroke was manifested by either seizures or signs of lateralization or disturbed conscious level. Diagnosis based on magnetic resonance imaging (MRI) brain and whether stroke was arterial or venous was determined by magnetic resonance angiography (MRA) and magnetic resonance venography (MRV) brain.
All of SCD patients were transfused and received hydroxyurea (Bristol-Meyers-Squibb, NY) as an oral daily dose ranging from 10 to 25 mg/kg/day.
The patients with serum ferritin above 1000 ug/L received the three main chelator agents as follows: deferoxamine (Novartis, Basel, Swizerland) as a subcutaneous injection over 8 h ranging from 20 to 50 mg/kg, deferasirox (Novartis, Basel, Swizerland) as a single oral dose ranging from 20 to 40 mg/kg and deferiprone (Apotex, Toronto, Canada) orally divided into 2 or 3 doses ranging from 50 to 100 mg/kg.
Sample preparation
Peripheral blood samples were collected on potassium-ethylene diamine tetra-acetic acid (K2-EDTA) (1.2 mg/mL) for complete blood count (CBC) and hemoglobin analysis. For chemical analysis and enzyme-linked immunosorbent assay (ELISA), clotted samples were obtained and serum was separated by centrifugation for 15 min at 1000× g then stored at −20 °C till subsequent use in ELISA.
Laboratory analysis
Laboratory investigations included CBC using Sysmex XT-1800i (Sysmex, Kobe, Japan), examination of Leishman-stained smears for differential white blood cell (WBC) count, hemoglobin analysis by HPLC using D-10 (BioRad, Marnes La Coquette, France), markers of hemolysis (lactate dehydrogenase [LDH] and indirect bilirubin), and serum ferritin on Cobas Integra 800 (Roche Diagnostics, Mannheim, Germany). Serum ferritin level was measured and a cut-off value of 2500 μg/L was used as indicator of poor prognosis with higher incidence of cardiac complications and shortened survival.15
Determination of serum level of sRAGE was done by ELISA using Quantikine Human RAGE Immunoassay (R&D system, Minneapolis)
Statistical analysis
Data were collected, revised, coded, and entered to the Statistical Package for Social Science (IBM SPSSTM) version 20. Qualitative data were presented as numbers and percentages while quantitative data were entered into Kolmogorov–Smirnov test of normality and parametric distribution data were presented as mean, standard deviations, and ranges while non-parametric distribution data were presented as median with interquartile range (IQR). In order to compare parametric quantitative variables between two groups, Student’s t-test was applied. For comparison of non-parametric quantitative variables between two groups, Mann–Whitney test was used. The comparison between two groups with qualitative data was done using Chi-square test. Person correlation coefficient were used to assess the association between two normally distributed variables. When a variable was not normally distributed, a Spearman correlation test was performed. Multivariable linear regression analysis was employed to determine the relation between sRAGE and clinical and laboratory variables. A p-value < 0.05 was considered significant in all analyses.
Results
Patients with SCD included 24 patients with sickle cell anemia (SCA) and 16 patients with sickle beta thalassemia. The clinical and laboratory characteristics of the studied patients are listed in Table 1.
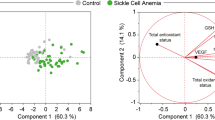
The level of sRAGE was significantly higher in SCD patients compared to the control group (p < 0.001) (Fig. 1). A sub-analysis of the patients group according to their genotypes revealed that patients with SCA (Homozygous SS) had a significantly elevated sRAGE level than those with the milder sickle beta thalassemia (p = 0.005) (Table 2).
Evaluation of the measured sRAGE level in relation to the clinical data of the patients, revealed that patients who had a previous history of stoke manifestations, acute chest syndrome or frequent sickling crisis (>3 attacks/year) were presented with significantly higher sRAGE than patients without (p < 0.05) (Table 2). Moreover, patients with serum ferritin > 2500 had significantly increased sRAGE compared with patients below these cutoffs (p = 0.02) (Table 2). Notably, sRAGE was significantly increased in patients with serum ferritin > 2500 μg/L suggesting a relation with iron overload and an indication for chelation therapy (p = 0.002) (Table 2). However, there was no significant difference in sRAGE level as regards age, sex, family history, disease duration, and splenectomy (P > 0.05).
The measured sRAGE showed significant positive correlations with percentage of HbS, LDH, and serum ferritin levels (Fig. 2, Table 3). Upon performing multivariable regression analysis, only HbS and ferritin were proved to be significant independent factors affecting sRAGE levels (Table 4).
Discussion
SCD induces chronic states of oxidative stress and inflammation.16 There is an increasing evidence points towards an oxidative stress response responsible for the pathophysiology of secondary dysfunction in sickle cell patients.17 Formation and accumulation of AGE and the consequences of AGE/RAGE interaction have been studied in SCD, previously.6
Despite the fact that sRAGE has been identified two decades ago, it still retains a lot of its mystery. To date, no previous published data investigated the role of sRAGE in the pathobiology of SCD.
We found elevated sRAGE levels in SCD patients compared with healthy controls. Three considerations may explain this finding. Firstly, the increase in the levels of serum AGEs induces the expression and production of MMP-9.18 Furthermore, AGE/RAGE interaction increases production of ROS19 which is known to increase the expression and activity of MMPs.20 This in turn triggers RAGE shedding and would increase sRAGE in the serum.21 Secondly, it is believed that oxidative stress, might selectively alter splicing mechanisms, thereby directly affecting esRAGE levels.22 Thirdly, formation and accumulation of AGEs upregulates endothelial RAGE expression. Since both cRAGE and esRAGE are derived from RAGE, an alteration in the RAGE will be reflected in the alteration in sRAGE.23
We measured sRAGE level in relation to patients genoytpes and we reported a significantly higher level in SCA (HbSS) patients than in those with compound heterozygous sickle beta thalassemia.
It has been known that patients with HbSS have higher rates of hemolysis due to higher autoxidation of HbS. During hemolytic episodes. The hydrophobic haem rapidly intercalates into the plasma membrane of endothelial cells where it releases its iron, which potentiates endothelial cell activation by catalyzing non-enzymatic generation of ROS and AGEs.24In this series our finding that HbS percentage had a positive impact on sRAGE, and independently affect its level could be explained.
Previous studies have proved that plasma levels of AGEs are increased and associated with hemolysis and hemolysis-related complications in SCD.6,25 Furthermore, a multivariate regression analysis done by Nur and his collegues6 revealed that AGEs were related to LDH (the classical biomarker of intravascular hemolysis). These observations are consistent with ours that confirmed a significant correlation between LDH and sRAGE levels.
The measured levels of sRAGE were elevated among our patients who had history of frequent sickling crisis (>3 attacks/year). The repeated bouts of sickling and reversible vasoocclusion induce the release of high mobility group box 1 (HMGB1). HMGB1 is a nuclear chromatin-binding protein that aids in regulating gene expression and maintaining nuclear DNA structure.16 HMGB1 may signal through RAGE, and via toll-like receptors, TLR2 and TLR4. Activation of these receptors results in the activation of NF-KB. Interestingly, the presence of NF-KB binding sites in RAGE promoter creates a positive feedback loop through increasing RAGE expression and subsequently, increases RAGE shedding.26
The sickled red blood cells can contribute to the pathogenesis of stroke via abnormal adherence to the vascular endothelium and by hemolysis which results in endothelial cell activation, a hypercoagulable state. The end result is vasculopathy and occlusion.27
RAGE is also critically implicated in the medio-intimal proliferative reaction after vascular damage. Moreover, the inflammatory and oxidant milieu sustained by RAGE activation enhances the generation of its ligands (AGE, S100/calgranulins and HMGB-1), thus sustaining detrimental vicious circle. These factors can lead to architectural remodeling of the vessel wall and vasculopathy.28 In parallel, RAGE activation enhances MMP expression through in vivo ROS generation promoting a subsequent release of sRAGE.21 These observations may lie behind the elevated sRAGE levels in our patients with previous history of stroke manifestations.
Acute chest syndrome (ACS) is a frequent cause of acute lung injury in children with SCD.29In the physiological state, pulmonary tissue displays a relatively high expression of RAGE, with alveolar type I(ATI) pneumocytes accounting for the vast majority of RAGE expression. Accordingly, alteration in RAGE levels and RAGE-ligand interaction have been involved in damage to ATI pneumocytes which is an important feature of acute lung injury.30
Consistent with these findings, Vazzana et al.31 reported that local circulating levels of sRAGE may be considered as a biomarker of pulmonary tissue damage. Also, Calfee and colleagues32 showed that higher baseline plasma RAGE levels are significantly correlated with increased severity of lung injury. These findings are further supported by ours reporting that patients with history of acute lung syndrome exhibit higher sRAGE levels.
In SCD, the major and unavoidable complication of transfusions is iron overload.33 Iron may contribute directly to endothelial damage, vasculopathy and an inflammatory response.34 In this study, patients with significantly higher sRAGE were candidates for chelation therapy. The indication for iron chelators in these patients referred to high iron overload as a complication of repeated blood transfusion. Moreover, when ferritin was inserted in a multivariate regression model, it was strongly related to sRAGE level. This finding may explain the significant association between high sRAGE in patients received chelation treatment.
In spite of increased levels of sRAGE that neutralize AGEs-mediated damage by acting as a decoy, complications occur in SCD. It is well known that AGEs are positive regulators of the cellular RAGE expression and an increased formation of AGEs enhanced the expression and secretion of sRAGE.35 In addition, the positive association between sRAGE and AGEs observed previously36 support the view that sRAGE could be a reflection of the activity of AGE-RAGE axis, which proved to be implicated in endothelial and vascular damage, as well as chronic organ complications in SCD.6,25 Furthermore, elevated levels of serum sRAGE might be not sufficient to handle large amount of AGEs effectively. A unified formula that takes into consideration of AGEs and sRAGE (AGEs/sRAGE) was suggested by Prasad23 to be better biomarker for all AGE-RAGE associated diseases. We also recommend using this formula to untangle the inter-relationship between serum levels of sRAGE and AGEs and to provide a deeper insight into the pathobiology of sRAGE. This prompts further investigations.
The levels of sRAGE are also elevated in diabetes, acute lung injury, and renal disease. In contrast, low levels of sRAGE have been suggested to be marker of disease states, such as coronary artery disease, atherosclerosis, essential hypertension,37 and rheumatoid arthritis.8
Indeed, many factors may contribute to regulation of sRAGE levels. Firstly, the main driver of the outcome on sRAGE levels is any factor that may directly affect ADAM10 or MMP activities at the cellular level or whether they might selectively alter splicing mechanisms. Secondly, the cell types most likely to be releasing sRAGE might differ in different pathological states. Finally, the degree of ligand burden.22 Piarulli and colleagues38 proposed that a superimposed acute events such as inflammation and oxidative stress stimulate an abrupt rise in sRAGE levels. A preliminary study by Uchida and co-workers39 referred the high levels of sRAGE to the compensatory anti-inflammation phenomenon in response to tissue damage. Furthermore, a pervious study by Yonekura et al.40 has lead to the hypothesis that sRAGE could be an immunomodulatory, bioactive molecule per se.
Alternatively, many previous studies have demonstrated a decreased sRAGE levels in patients groups indicating that lowered concentrations could be a reliable biomarker of deficient and/or altered inflammatory control in humans.3,37 In the light of the previous concepts future investigations are needed to shed more light on the biological mechanisms involved in the generation and clearance of sRAGE to solve its mystery.
In conclusion, sRAGE is significantly enhanced in SCD and may be considered as a marker of vascular dysfunction in those patients. In clinical setting, early identification of SCD patients with elevated levels of sRAGE might be of particular importance to identify at-risk patients and direct them to RAGE-targeted treatments such as anti-RAGE antibodies that inhibit the activation of RAGE signaling. These novel therapies directed towards the biological basis of vasculopathy and vasoocclusion should be investigated and could provide a breakthrough in complications prevention in sickle cell disorders.
References
Rees, D. C., Williams, T. N. & Gladwin, M. T. Sickle- cell diseas. Lancet 376, 2018–2031 (2010).
van Beers, E. J. et al. Circulating erythrocyte-derived microparticles are associated with coagulation activation in sickle cell disease. Haematologica 94, 1513–1519 (2009).
Koyama, Y. et al. High serum level of pentosidine, an advanced glycation end product (AGE), is a risk factor of patients with heart failure. J. Card. Faliure 13, 199–206 (2007).
Gerrits, E. G. et al. Skin autofluorescence: a tool to identify type 2 diabetic patients at risk for developing microvascular complications. Diabetes Care 32, 517–521 (2008).
Ahmed, N. Advanced glycation endproducts—role in pathology of diabetic complications. Diabetes Res. Clin. Pract. 67, 3–21 (2005).
Nur, E. et al. Plasma levels of advanced glycation end products are associated with haemolysis-related organ complications in sickle cell patients. Br. J. Haematol. 151, 62–69 (2010).
Kay A. M., Simpson L., Stewart J. A. The role of AGE/RAGE signaling in Diabetes-Mediated Vascular calcification. J. Diabetes Res. 2016, 6809703 (2016).
Maillard-Lefebvre, H. et al. Soluble receptor for advanced glycation end products: a new biomarker in diagnosis and prognosis of chronic inflammatory disease. Rheumatology 48, 1190–1196 (2009).
Ding, Q. & Keller, J. N. Evaluation of rage isoforms,ligands,and signaling in the brain.Biochimica et Biophysica Acta(BBA)-Molecular. Cell Res. 1746, 18–27 (2005).
Ahmad, S. et al. AGEs, RAGEs and sRAGE, friend or foe for cancer. Semin. Cancer Biol. 17, 30032–30039 (2017).
Wethers, D. L. Sickle cell disease in childhood: Part I. Laboratory diagnosis, pathophysiology and health maintenance. Am. Fam. Phys. 62, 1013–1020 (2000).
Platt, O. S. et al. Pain in sickle cell disease. Rates risk Factors, N. Engl. J. Med. 325, 11–16 (1991).
Darbari, D. S. et al. Markers of severe vaso-occlusive painful episode frequency in children and adolescents with sickle cell anemia. J. Pediatr. 160, 286–290 (2012).
Ballas, S. K. et al. Definitions of the phenotypic manifestations of sickle cell disease. Am. J. Hematol. 85, 6 (2010).
Musallam, K. M. et al. Elevated liver iron concentration is a marker of increased morbidity in patients with b thalassemia intermedia. Haematologica 96, 1605–1612 (2011).
Xu, H. et al. Sickle cell disease increases hig mobility group box 1: a novel mechanism of inflammation. Blood 124, 3978–3981 (2014).
Queiroz, R. F. & Lima, E. S. Oxidative stress in sickle cell disease. RevBras Hematol. Hemoter. 35, 16–17 (2013).
Zhang, F. et al. The novel function of advanced glycation end products in regulation of MMP-9 production. J. Surg. Res. 171, 871–876 (2011).
Parasad, K. Soluble receptor for advanced glycation end products (sRAGE)and cardiovascular disease. Int. J. Angiol. 15, 57–68 (2006).
Rajagopalan, S., Meng, X. P., Ramasamy, S., Harrison, D. G. & Galis, Z. S. Reactive oxygen Species produced by macrophage-derived foam cells regulate the activity of vascular matrix metalloproteinases in vitro. Implications for atherosclerosis plaque stability. J. Clin. Invest. 98, 2572–2579 (1996).
Siwik, D. A., Pagano, P. J. & Colucci, W. S. Oxidative stess regulates collagen synthesis and matrix metalloproteinase activity in cardiac fibroblasts. Am. J. Physiol. Cell. Physiol. 280, C53–C60 (2001).
Schmidt, A. M. Soluble RAGEs-Prospects for treating and tracking metabolic and inflammatory disease. Vasc. Pharmacol. 72, 1–8 (2015).
Prasad, K. Low levels of serum soluble receptors for advanced glycation end products, biomarkers for disease for disease state: Myth or reality. Int. J. Angiol. 23, 11–16 (2014).
Galaris, D. & Pantopoulos, K. Oxidative stress and iron homeostasis: mechanistic and health aspects. Crit. Rev. Clin. Lab. Sci. 45, 1–23 (2008).
Somjee, S. S. et al. Advanced glycation end products in sickle cell anemia. Br. J. Hematol. 128, 112–118 (2004).
Van Beijnum, J. R., Buurman, W. A. & Griffioen, A. W. Convergence and amplification of the toll-like receptor (TLR) and receptor for advanced glycation end products (RAGE) signaling pathways via high mobility group B1(HMGB1). Angiogenesis 11, 91–99 (2008).
Switzer, J. A., Hess, D. C., Nichols, F. T. & Adams, R. J. Pathophysiology and treatment of stroke in sickle-cell disease: present and future. Lancet Neurol. 5, 501–512 (2006).
Ramasamy, R., Yan, S. F., Herold, K., Clynes, R. & Schmidt, A. M. Receptor for advanced glycation end products: fundamental roles in the inflammatory response: winding the way to the pathogenesis of endothelial dysfunction and atherosclerosis. Ann. N. Y. Acad. Sci. 1126, 7 (2008).
Jain, S., Bakshi, N. & Krishnamurti, L. Acute chest syndrome in chidren with sickle cell disease. Pediatr. Allergy Immunol. Pulmonol. 30, 191–201 (2017).
Chuah, Y. K., Basir, R., Talib, H., Tie, T. H. & Nordin, N. Receptor for advanced glycation end products and its involvement in inflammatory diseases. Int. Inflamm. 403460, 15 (2013). ID.
Vazzana, N., Santilli, F., Cuccurullo, C. & Davi, G. Soluble forms of RAGE in internal medicine. Intern. Emerg. Med. 4, 389–401 (2009).
Calfee, C. S. et al. Plasma receptor for advanced glycation end products and clinical outcomes in aute lung injuy. Thorax 63, 1083–1089 (2008).
Raghupathy, R., Manwani, D. & Little, J. A. Iron overload in sickle cell disease. Adv. Hematol. 272940, 9 (2010).
Ballas, S. K. & Marcolina, M. J. Determinants of red cell survival and erythropoietic activity in patients with sickle cell anemia in the steady state. Hemoglobin 24, 277–286 (2000).
Miura, J. et al. Endogenous secretory receptor for advanced glycation endproducts levels are correlated with serum pentosidine and CML in patients with type 1 diabetes. Arterioscler. Thromb. Vasc. Biol. 27, 253–254 (2007).
Tan, K. C. et al. Association between serum levels of soluble receptor for advanced glycation end products and circulating advanced glycation end products in type 2 diabetes. Diabetologia 49, 2756–2762 (2006).
Geroldi, D. et al. Decreased plasma levels of soluble receptor for advanced glycation end products in patients with essential hypertension. J. Hypertens. 23, 1725–1729 (2005).
Piarulli, F., Sartore, G. & Lapolla, A. Glyco-oxidation and cardiovascular complications in type 2 diabetes: a clinical update. Acta Diabetol. 50, 101–110 (2013).
Uchida, T. et al. Receptor for advanced glycation end-products is a marker of type 1 cell injury in acute lung injury. Am. J. Resp. Crit. Care Med. 173, 1008–1015 (2006).
Yonekura, H. et al. Novel splice variants of the receptor for advanced glycation end-products expressed in human vascular endothelial cells and pericytes, and their putative roles in diabetes-induced vascular injury. Biochem. J. 370, 1097–1099 (2003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Safwat, N.A., Kenny, M.A. Soluble receptor for advanced glycation end products as a vasculopathy biomarker in sickle cell disease. Pediatr Res 84, 869–874 (2018). https://doi.org/10.1038/s41390-018-0221-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0221-7