Abstract
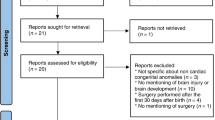
The aim is to review the evidence about the utility of term-equivalent age (TEA) magnetic resonance imaging (MRI) in predicting neurodevelopmental outcomes for preterm neonates. Preterm birth accounts for ~12% of all deliveries in the United States and is the leading cause of neurologic disabilities in children. From the neonatologist perspective, it is critically important to identify preterm infants at risk of subsequent neurodevelopmental disability who may benefit from early intervention services. However “the choose wisely campaign” also emphasizes the need to have ongoing cost/benefit discussions regarding care of preterm newborns to avoid waste that comes from subjecting infants to procedures that do not help. We performed a MEDLINE EMBASE database review from 2000 to 2018 to account for the technical evolution in the cranial ultrasound machines and introduction of MRI imaging in the NICU. Studies were graded based on the strength of their design using the GRADE guidelines and summarized with respect to brain MRI vs. cranial US (1) detection of white matter injury; (2) cerebellar hemorrhage; (3) long-term neurodevelopmental outcomes and impact on parental anxiety. We conclude with a hospital-specific guideline algorithm for performing TEA MRI based on risk evaluations ≤32 weeks.
Similar content being viewed by others
Introduction
Preterm birth is a major public health concern with the dramatic increase of survival rates. Despite improved survival and mortality, long-term neurodevelopmental outcomes remain a concern. In very preterm infants (<30 weeks of gestation), ~10–15% will develop cerebral palsy, 40% will develop mild motor deficits while 30–60% will experience cognitive deficits.1 Tremendous brain growth occurs in the first year after birth, but the period between 24 and 40 weeks’ gestation is a critical period in brain development. Primary neurulation occurs in the first 1–2 months of gestation, prosencephalic development occurs during the 2nd and 3rd month of gestation, and neuronal proliferation occurs in the subsequent 3–4 months. This is followed by neuronal migration in the 3rd to 5th month of gestation and then myelination. Cerebral lesions associated with prematurity and neurodevelopmental impairments are caused by both the nature/extent of direct cerebral injury, as well the arrested growth during the critical windows of brain development. Recently advanced magnetic resonance imaging (MRI) studies has demonstrated critical periods of tissue-specific ex-utero growth trajectory postnally.2 These critical periods of ex-utero brain growth simultaneously highlight intense vulnerability to postnatal interventions as well as valuable opportunities for plasticity, regeneration and repair. White matter brain injury is the most common form of injury in preterm infants and may present clinically as periventricular leukomalacia (PVL), punctate white matter injury, intraparenchymal hemorrhage, ischemia, and/or moderate-to-severe ventriculomegaly with white matter loss.3 The aim of this review is to describe the evidence supporting the utility of TEA MRI and cranial US in predicting neurodevelopmental outcomes in preterm neonates.
Cranial ultrasound in preterm neonates
In the neonatal intensive care unit, serial cranial ultrasound (CUS) is the standard of care, because it is widely available, inexpensive, and non-invasive. CUS was introduced to the neonatal intensive care units in the late 1970s.4 In 2002, a practice parameter by the American Academy of Neurology and the Practice Committee of the Child Neurology Society recommended routine screening CUS in all infants with gestational age of <30 weeks at 7 and 14 days of age, serially to be optimally repeated between 36 and 40 weeks’ postmenstrual age.5
Serial CUS performed in the first 2 weeks of life can detect more than 80% of germinal matrix/intraventricular hemorrhage (GM/IVH). Paneth et al.6 in a large study determining the level of agreement between ultrasound diagnosis of GM/IVH and histological postmortem examination of the brain, reported that 50% of the initial GM/IVH were missed by the sonographic readers. The study reported that when three scans were serially viewed, and the lesion was at least 1 cm in diameter, all GM/IVH were detected. White matter lesions less well detected on ultrasound are hyperechoic lesions or echodenisties (ED); hypoechoic lesions or echolucenicies (EL); or ventricular enlargement (VE).7
The posterior limb of the internal capsule and the corona radiata are two important areas in the brain because the corticospinal tract (CST) is located in the posterior portion of the internal capsule. The CST is the major neuronal pathway that mediates voluntary skilled movements in the human brain.8 Injury to these areas can be difficult to be visualized by US but is associated with poor motor developmental outcomes in neonates.9 Another area of injury that is associated with high prevalence of long-term cognitive, learning and behavioral disability that is not easily visualized without extended windows is the cerebellum. Cerebellar hemorrhage has been reported with increasing prevalence in premature neonates, particularly extremely low birth weight infants (ELBW); although it remains significantly underdiagnosed.10,11
CUS performed after the first month of life was more prognostic compared with scans performed in the first 1–2 weeks of life. De Vries et al. performed weekly CUS on 2139 neonates with 1636 neonates born ≤32 weeks of gestation, and 503 infants born between 33 and 36 weeks of gestation. CUS was performed once a week until discharge, and at 40 weeks postmenstrual age. Forty-six percent of the neonates with white matter EL were identified after 28 days of life, and 14% of these abnormalities were not identified until 40 weeks postmenstrual age.7 This study highlighted the importance of sequential and late CUS in detecting abnormalities predictive of cerebral palsy (79% of the CP cases had major US abnormalities). This was further emphasized in a later study by the same author.12 It concluded that sequential CUS until discharge followed by a repeat CUS at TEA should identify infants with cystic PVL and hemorrhagic parenchymal infarction. Sarkar et al.13 further demonstrated in a large cohort of NICHD Neonatal Research Network (12,739 infants), that about 15% of the cystic PVL lesions seen on early imaging, were no longer visible on follow-up imaging close to 36 weeks postmenstrual age.
Advantages of CUS are ease of performance with minimal disruption to the baby, and it can be performed on all ventilated infants without any sedation. However, its disadvantages are: (1) operator, machine, and probe dependant; (2) poor visualization of the periphery of the brain and posterior fossa (cerebellum); (3) poor sensitivity to diffuse white matter injury and large interobserver variability. One of the obstacles for CUS in detecting cerebellar hemorrhages is its poor visualization and delineation of the frequency, extent, and sequelae of preterm cerebellar hemorrhage. Microhemorrhages <3 mm in size are not detected on CUS.14,15,16 Despite the fact that addition of routine mastoid views to CUS has helped improve detection rate, microhemorrhages are still better detected with MRI.17
Brain MRI in preterm neonates
MRI provides high-resolution images of the brain of premature neonates without using ionizing radiations. It allows better definition of the lesions in terms of site, extent, and type of pathology compared to CUS and provides more detailed characterization of WM in infants. Parenchymal lesions, punctate hyperintensities, diffuse excessive high signal intensity (DEHSI) are typically identifiable on conventional imaging sequences including T1- and T2-weighted images. Barnett et al. and colleagues, using diffusion-weighted MRI, studied 491 infants born <34 weeks of gestation without focal destructive brain lesions; they identified independent association of diffuse white matter injury at term-equivalent age with perinatal risk factors including lower GA at birth, fetal growth restriction, increased number of days requiring ventilation, parenteral nutrition, necrotizing enterolcolitis, and male sex.18
Various scoring systems were developed to stratify the MRI findings of white and gray-matter injury. Miller et al.19 validated an MRI scoring system for white matter injury associated with adverse neurodevelopmental outcomes.The severity of white matter abnormalities on MRI was classified as normal (no white matter lesions), minimal (3 or fewer areas of T1 signal abnormality measuring <2 mm), moderate (>3 areas of T1 signal abnormality or these areas measuring <2 mm, but >5% of the hemisphere involved), or severe (>5% of the hemisphere involved). Newborns were diagnosed with mild ventriculomegaly if the largest atrial ventricular diameter measured was 8–10 mm, and with moderate/severe ventriculomegaly if it measured >10 mm.20
Woodward et al.21 in their study used a modified standardized MRI scoring system consisting of eight 3-point scales. White matter abnormality was graded according to 5 scales, including the nature and the extent of white matter signal abnormality, the loss in the volume of periventricular white matter, the extent of any cystic abnormalities, ventricular dilatation, or the thinning of the corpus callosum. Gray-matter abnormality was graded according to three scales including the extent of gray-matter signal abnormality, the quality of gyral maturation, and the size of the subarachnoid space.
Kidokoro et al.22 used a new scoring system that included PVL and cerebellar hemorrhage, besides using Papile et al.23 classification for IVH. The new scoring system compared to Woodward scoring system included cerebellar injury besides the white and gray-matter injury.
In addition to conventional MRI, diffusion tensor imaging (DTI) and novel surface-based morphometry methods are being developed to provide more insight into the period of exponential brain growth that occurs during the third trimester of pregnancy. These have been well addressed in other reviews24,25,26,27,28 and are not included as a search item in the table reviews listed below.
Several papers have established a correlation between neonatal conventional MRI at term equivalent and prediction of cerebral palsy (CP), with high sensitivity and specificity.3,29,30,31,32,33 The search strategy was conducted from 2000 to 2018 to account for the evolution in the CUS transducers, views and the introduction of MRI imaging in the NICU. Search was performed in MEDLINE and EMBASE database review and studies were graded by two examiners (J.I. and I.M.) based on the strength of their design using the GRADE guidelines.34 In case of dissent, the senior author LC was used to adjucate grading. The articles summarized in the tables highlight brain MRI, vs. CUS comparisons with respect to (1) detection of the types of brain injury, (2) long-term neurodevelopmental outcomes, (3) detection of cerebellar hemorrhage; and (4) impact on parental anxiety and cost evaluations.
Comparison of type of injury between CUS and MRI brain in preterm neonates
Highlighted studies’ methodologies are summarized in Table 1. Of note very few studies have directly compared CUS and MRI in preterm infants. Notably the existing litterature summarized has several limitations (lack of serial CUS in most studies, studies performed at different time points, lack of correlation to developmental outcomes).
Maalouf et al.35 compared the hard copy findings on CUS with findings on MRI to determine if normality and abnormality co-occur between them from birth and at TEA in preterm infants born at ≤30 weeks gestation. The median gestational age was 27 weeks, with median birth weight of 908 g. Enrolled infants were divided into three groups (first 4 days, postnatal age 7–95 days, between GA 38 and 44 weeks). A total of 62 paired MRI and CUS (performed on the same day) were included for 32 neonates. The study had no neurodevelopmental outcomes listed. CUS findings of mild or no white matter (WM) echogenicity had lower sensitivity (0.55) and lower predictive probability (PP) of 0.54 (0.41–0.66) for the presence of normal WM signal intensity on MRI. Moderate or severe white matter echogenicity on CUS had a PP of 0.54 (0.42–0.66) for the presence of small petechial WM hemorrhage and/or diffuse excessive high signal intensity (DEHSI) in the WM on T2-weighted MRI images. For CUS findings of mild/moderate or severe WM echogenicity performed at ≥7 days after birth, the PP was higher 0.72 (0.58–0.87) for the presence of WM hemorrhage and/or DEHSI on MRI. The study concluded that CUS can reliably predict the presence of IVH, hemorrhagic parenchymal infarction, germinal matrix hemorrhage on MRI. However it has poor predictability for DEHSI and small petechial hemorrhages detected on T2-weighted images. This predictability improves if CUS was performed ≥7 days postnatally. However the study only enrolled neonates who had CUS and MRI on the same day and infants were imaged as either part of a research cohort in infants born <30 weeks or for clinical indications.
Inder et al.,36 in a prospective study of a large unselected cohort of 96 VLBW babies, assessed the sensitivity and specificty of serial CUS performed in the first 6 weeks of age with MRI findings at term in characterizing the presence of WM injury. Mean GA was 27.9 weeks and mean birth weight was 1036 grams. WM signal intensity abnormality on MRI required T1 hyperintensity with no T2 hypointensity. They classified the white matter signal intensity as normal, focal signal intensity, an extensive signal intensity abnormality or cystic change. Seventy-four patients had normal or only transient echodenisty (<7 days) on the serial CUS. 10 (14%) of these patients had evidence of notable WM injury on MRI in the form of extensive signal intensity abnormality or cystic changes. Of the 22 patients with overt WM abnormality on CUS (prolonged echodensity >7 days, echolucency in the periventricular white matter), 14 (64%) patients had normal or focal signal intensity changes in the WM on the MRI. Prolonged echolucencies (>7 days) in the WM on the CUS had a sensitivity of 26% and positive predictive value of 36% for the presence of overt WM injury on MRI at term. In contrast, for cystic changes on MRI at term, CUS was associated with sensitivity of 75% and specificity of 100%. The study concluded that CUS in VLBW neonates demonstrated high reliability in the detection of cystic WM injury, but was significantly inferior in detecting non-cystic WM injury.
Whitby et al.,37 in a prospective double-blinded trial that included 134 premature and term infants, compared the clinical usefulness of MRI with CUS. MRI and CUS were done within 24 h of each other, both at term equivalent. In 56% of cases, the MRI detected additional clinical findings particularly in the posterior fossa, that were not identified on CUS. Limitations of this study were that the CUS was only performed once and the ultrasound views were limited to the anterior and lateral fontanels.
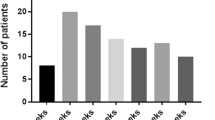
Neubauer et al.,38 performed a retrospective analysis of prospectively collected data on premature neonates <32 weeks, who underwent routine CUS as well as TEA brain MRI. Cerebral MRI at TEA was part of the routine follow-up program at their medical center in Austria. A validated scoring system, previously published by Kidokoro et al.22 was used. Cerebral MRI at TEA, as compared to CUS, detected brain injury in 25% of preterm infants. IVH was detected in 48 patients (16%), white matter disease in 30 (10%), and cerebellar hemorrhage in 24 (8%) of the 300 patients included in the study. IVH diagnosis was made by CUS in 46 (95.8%) of the 48 patients detected by MRI. In contrast, white matter disease and cerebellar hemorrhage was detected by CUS in only 10% (3 of 30 infants) and 8% (2 of 24 infants), respectively. All three cases of white matter disease diagnosed by CUS was the cystic form. The study did not mention the time points at which the CUS was done, while the MRI was performed as part of their routine follow-up for all preterm infants <32 weeks.
Comparison between CUS and MRI for prediction of neurodevelopmental outcomes
Studies summarized in Table 2 highlight the importance of WMI injury detected by term-equivalent MRI in relation to neurodevelopmental outcomes.
Valkama et al.31 studied 51 infants with gestational age <34 weeks or birth weight <1500 g were included. The study reported that parenchymal lesions seen on TEA MRI had 100% sensitivity in predicting CP, while CUS had only 67% sensitivity. However, CUS was only performed once at term, without previous sequential imaging which reduces its predictive value.
Mirmiran et al.3 studied 61 infants with gestational age <30 weeks and birth weight <1250 g. The study compared the value of serial CUS, performed in the first 2 weeks of life and then thereafter as clinically indicated, with a single MRI performed prior to discharge to predict cerebral palsy. There was increased sensitivity and positive predictive value of the MRI compared with CUS in predicting CP at 20 and 31 months.
Miller et al.19 studied a total of 89 infants with mean gestational age of 28 weeks, that had MRI performed at mean gestational ages of 32 weeks and 37 weeks. Moderate-to-severe abnormalities were seen in 37% of the cases on the first MRI and 32% of the cases on the second MRI. The severity of abnormal outcomes was significantly associated with an increased severity of white matter injury, ventriculomegaly, and IVH.
In a large study by Woodward et al.,21 the presence of moderate-to-severe white matter abnormalities on MRI were more sensitive than CUS findings of PVL or IVH in identifying children who subsequently had neurodevelopmental impairments. In another study by the same author39 of very preterm infants (≤32 weeks) with varying degrees of white matter abnormality on TEA MRI (none, mild, moderate to severe), compared to full term neonates, there was a linear association between the severity of white matter lesions and the cognitive scores at 4 and 6 years follow-up.
Nanba et al.9 made the association between T1 hyperintensity and cysts in the periventricular white matter, particularly the corona radiata on TEA MRI and gross motor function at 3–5 years. All 37 infants with CP had periventricular lesions or cysts in the corona radiata above the posterior limb of internal capsule (PLIC). On the other hand, all 17 infants with white matter lesions sparing the corona radiata had normal motor developmental outcome.
de Bruïne et al.40 found that the presence of six or more punctate white matter lesions on MRIs performed around or within 4 months of TEA, was significantly associated with lower motor development index (MDI) and psychomotor development index (PDI), more developmental delay and CP. These infants also had behavioral problems.
Iwata et al.41 in a prospective study, evaluated the association between MRI at TEA using composite scores of white matter and gray matter, and cognitive outcomes at 9 years of age using the Wechsler Intelligence Scale for Children, Third edition. Neonates with abnormal white matter had lower verbal (p value < 0.005), performance (p value < 0.001), and full scale (p value < 0.001), with higher incidence of cerebral palsy.
Kidokoro et al.,22 in a large prospective study that further assessed neurodevelopmental outcomes at 2 years, included 325 neonates from three different cohorts. Infants ≤32 weeks of gestation were recruited between 1998 and 2000 at Christchurch, New Zealand (n = 110); infants <30 weeks or <1250 g born between 2001 and 2003 at Royal Women Hospital in Melbourne, Australia (n = 227); and infants <30 weeks born between 2007 and 2010 at St Louis Children’s Hospital, Missouri, were included. MRI performed at TEA (≥37 to ≤42 weeks’ postmenstrual age) data was reviewed. PVL was diagnosed in 40 infants (12%), IVH in 62 infants (19%), and cerebellar hemorrhage in 31 infants (10%). Infants with high-grade PVL or IVH had lower MDI and PDI scores with higher incidence of CP. The study reported that cerebellar hemorrhage was not related to any neurodevelopmental outcome, a conclusion which will be discussed further in the following section. Of note, Bayley Scales of Infant Development Second Edition (BSID II) was used in the Christchurch and Melbourne cohorts and BSID III was used in the St Louis cohort.
In the large prospective NEURO study,15 increasing severity of WM injury on near-term MRI was associated with significantly lower mean BSID III cognitive scores, higher rates of cognitive scores <70 and <85, and moderate-to=severe CP. Both late CUS adverse findings and MRI findings of cerebellar lesions were independently associated with NDI or death, in comparison to early CUS, emphasizing the importance of serial and near-term imaging.
In a comprehensive study, Anderson et al.42 evaluated the predictive value of TEA MRI and neurodevelopmental outcomes at 7 years of age in very preterm infants, using a systematic structural scoring system. Higher global brain, cerebral white matter, and deep gray-matter abnormality scores by TEA MRI were associated with poorer performance in IQ (p value < 0.01), math computation (p value < 0.01), spelling (p value < 0.05), and motor function (p value < 0.001).
Finally, a systematic review and meta-analysis by Van’t Hooft et al.43 showed that the pooled sensitivity and specificity values for prediction of CP were 77% and 79%, respectively. For prediction of motor function, the values were 72% and 62%, respectively. The meta-analysis concluded that the presence of moderate-to-severe WM abnormality on TEA MRI can predict CP and motor function in preterm or very low birth weight infants.
Therefore, the studies reviewed of term equivalent WM brain abnormalities detected on MRI showed a lasting effect on cognitive, motor and academic performance of preterm neonates.
Comparison of CUS and MRI in detecting cerebellar injuries in preterm neonates
The volume of the cerebellum increases 5-fold from 24 weeks to 40 weeks gestation,44 while its surface area increases by 30-fold (Table 3). Disruptive cerebellar injuries occur in about 9% of infants weighing <750 g.45 It is assumed that cerebellar injury occurring during the critical period of development in the third trimester results in interruption of the cerebello-cerebral pathways and subsequent deafferentation to specific regions of the contralateral cerebral cortex. This results in abnormal cortical development46 and neurodevelopmental impairment.
Cerebellar injury in preterm infants is usually identified on the posterior fossa/mastoid views of CUS, which is dependent on the angle of performance and expertise of the technician. However, MRI brain can detect these injuries with higher sensitivity as shown in studies summarized in Table 3.
Zayek et al.47 performed a retrospective study to determine the impact of cerebellar hemorrhagic injury (CHI) detected on CUS on adverse neurodevelopmental outcomes in extremely preterm infants. The study found that the incidence of cerebellar hemorrhage was 10% among a cohort of 1120 neonates. Infants with cerebellar bleeds involving the medial and lateral aspect were at higher risk for mental and motor disabilities, but infants with involvement of the cerebellar hemispheres had higher rates of mental but not motor delays. However, the neurodevelopmental outcomes were assessed in this study by either BSID II or III, which can affect the actual rate of impairment given that BSID III can underestimate the rate of impairments.48
Limperopoulos et al.,45 in a retrospective case–control study, compared the neurodevelopmental outcomes in a cohort of 86 preterm infants (<32 weeks) divided in three groups: isolated cerebellar hemorrhagic infarction (CHI); age-matched controls; and CHI plus supratentorial parenchymal injury. In all these cases, MRI was clinically performed only after CHI was detected by the mastoid view of CUS. Infants with isolated CHI involving the vermis, had lower mean scores on all tested measures, including severe motor disabilities (48% vs 0%), expressive language (42% vs 0%), delayed receptive language (37% vs 0%), and cognitive deficits (40% vs 0%). Socialization difficulties and autism were exclusively associated with injury to the vermis.
Two studies further studied the percentage of cerebellar hemorrhages detected only on MRI and not on CUS. The NEURO study found that among 72 cases of cerebellar lesions detected on MRI, 31 cases (50%) had mastoid views on late CUS, and only one case was identified. In a cohort of 131 infants, Tam et al.49 reported that cerebellar hemorrhages were seen on both CUS and MRI in three cases. However smaller hemorrhages (1–3 mm) were only seen on MRI in 10 cases.
Anderson et al.42 recently reported higher cerebellar abnormality scores to be associated with poorer IQ, math computation and motor outcomes. Moderate–severe global abnormality on TEA MRI was associated with IQ reduction (6.9 points), motor scores (1.9 points), and math computation (7.1 points).
Comparison between CUS and MRI regarding parental anxiety and cost/benefit ratio
MRI is a diagnostic tool used to better define pathology, provide insight into the underlying cerebral injury and structure and assign relative risk (Table 4). The stratification of high-risk preterm infants at discharge can allow parents and providers to embrace the concept of rehabilitation as well as appropriate early interventions. The choosing wisely initiative lead by Dr Levinson has focused on increasing both the physicians’ and parents’ awareness to encourage discussions including cost/benefit ratio to avoid waste from unnecessary testing and cautioned against undiscerning routine screening of all term-equivalent preterm infants.33
The subject of parental involvement in decision making is particularly understudied. An important paper by Pearce et al. reflect on the parental anxiety felt following the complicated birth of their preterm infant, where a pre-discharge MRI revealed a moderate cerebellar hemorrhage.50 Table 4 summarizes studies of whether MRI counseling is helpful to families. The team in London, led by David Edwards51 recently performed a large randomized controlled trial. They enrolled over 500 babies who were born before 33 weeks of gestation in several London hospitals. All the babies had a head MRI and an ultrasound at around term equivalent (38–44 weeks) with the aims of comparing the effects of prognostic information derived from either MRI or CUS on parental anxiety, coping, and health costs. Primary outcome measure was maternal anxiety measured by the State-Trait Anxiety Inventory (STAI). They reported that maternal anxiety decreased but health-related costs increased in the MRI group. Mean costs of delivering a single MRI scan and routine clinical ultrasound were £773 and £458, respectively.
Melbourne et al.52 evaluated the clinical impact of applying routine TEA MRI for ELBW infants in a regional NICU and did a cost analysis comparing the TEA MRI with serial CUS. The median number of CUS for neonates with grade 3 or 4 IVH was 8, with a total cost of 1546$, which was comparable with MRI standardized cost of 1600$. Dr Barrington recent editorial53 points to individual patient considerations rather than risk calculations, where beyond CP, there is little evidence of studies addressing the effect of early interventions in the long term.54,55 The numbers of evidence-based studies addressing parental anxiety and parental involvement or cost analysis studies beyond the two listed in this review is limited. The different perceptions in studies where skilled counseling was performed as opposed to the case report where parents were not prepared, emphasizes the need of skilled physicians to update families of the neuroimaging study results and to initiate the appropriate referrals after discharge.
Conclusion
The summarized studies underscore the importance of term-equivalent imaging as a prognostic tool especially in high-risk ELBW <1000 g. The need to document term-equivalent (38–44 weeks) MRI findings in the high-risk preterm infants ≤29 weeks is emphasized. A report of abnormalities should include documentation of the number, size and location of any cystic lesions, degree of ventriculomegaly, degree of WM loss, reduction in volumes of the basal ganglia and thalamus, cerebellar lesions, and abnormal myelination of the posterior limb of the internal capsule.
There is significant evidence supporting serial and near-term CUS and/or MRI imaging. Brain MRI is more sensitive in detecting white matter abnormalities (WMA) and smaller cerebellar hemorrhages linked to adverse neurodevelopmental outcomes in preterm neonates. Identification of moderate to severe WMA as well as PLIC and cerebellar injury on TEA MRI has a high predictive value for CP and motor function impairment independent of early CUS and other factors. However, the ability to predict neurocognitive or behavioral impairments is limited on both early CUS and MRI.
The evidence remains un-conclusive and research publications addressing parental anxiety and cost analysis topics are needed to fill knowledge gaps.
Recommendations
We conclude that when feasible to obtain the brain MRI without needing transfers to a referral hospital, or delaying hospital discharge, the information obtained in preterm neonates ≤29 weeks at TEA, can be a useful adjunct tool in addition to pre- and postnatal risk factors, to comprehensively predict neurodevelopmental outcomes. This is important to help identify neonates who will benefit from early intervention services and to provide management plans with occupational and physical therapies after discharge. We include our hospital-based algorithm that addresses the 29–32 weeks gestational age separately from the high risk preterm ≤29 weeks where TEA MRI has a higher predictive yield (Fig. 1). This algorithm was developed after the critical review of the literature, and in context of having an MRI scanner within our NICU, and a dedicated neuro-NICU team involved in parental counseling and prognostication. Taking the limited evidence especially regarding the cost/benefit aspect into consideration, these algorithms should be individually considered in the context of the hospital setup and facilities. Meanwhile we recommend keeping parental involvement regarding timing and optimal imaging at TEA discussions. Other recommendations include following specifically outlined NICU algorithm protocols, having skilled physicians to update families of the neuroimaging study results and to initiate the appropriate referrals after discharge. These steps can help ensure adequate prognostication and ensure appropriate follow-up while alleviating undue anxiety.
References
Mathur, A. & Inder, T. Magnetic resonance imaging--insights into brain injury and outcomes in premature infants. J. Commun. Disord. 42, 248–255 (2009).
Matthews, L. G., Walsh, B. H., Knutsen, C., Neil, J. J., Smyser, C. D. & Rogers, C. E. et al. Brain growth in the NICU: critical periods of tissue-specific expansion. Pediatr. Res. 83, 976–981 (2018).
Mirmiran, M., Barnes, P. D., Keller, K., Constantinou, J. C., Fleisher, B. E. & Hintz, S. R. et al. Neonatal brain magnetic resonance imaging before discharge is better than serial cranial ultrasound in predicting cerebral palsy in very low birth weight preterm infants. Pediatrics 114, 992–998 (2004).
Pape, K. E., Blackwell, R. J., Cusick, G., Sherwood, A., Houang, M. T. & Thorburn, R. J. et al. Ultrasound detection of brain damage in preterm infants. Lancet 1, 1261–1264 (1979).
Ment, L. R., Bada, H. S., Barnes, P., Grant, P. E., Hirtz, D. & Papile, L. A. et al. Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 58, 1726–1738 (2002).
Paneth, N., Kazam, E., Monte, W. & Rudelli, R. Brain Damage in the Preterm Infant (MacKeith Press; distributed by Cambridge University Press, Cambridge, 1994).
De Vries, L. S., Van Haastert, I. L., Rademaker, K. J., Koopman, C. & Groenendaal, F. Ultrasound abnormalities preceding cerebral palsy in high-risk preterm infants. J. Pediatr. 144, 815–820 (2004).
Jang, S. H. A review of corticospinal tract location at corona radiata and posterior limb of the internal capsule in human brain. NeuroRehabilitation 24, 279–283 (2009).
Nanba, Y., Matsui, K., Aida, N., Sato, Y., Toyoshima, K. & Kawataki, M. et al. Magnetic resonance imaging regional T1 abnormalities at term accurately predict motor outcome in preterm infants. Pediatrics 120, e10–19 (2007).
Hirtz, D. & Ment, L. R. Cerebellar hemorrhage in the premature infant-time for a balanced approach. J. Pediatr. 178, 9–10 (2016).
Martin, R., Roessmann, U. & Fanaroff, A. Massive intracerebellar hemorrhage in low-birth-weight infants. J. Pediatr. 89, 290–293 (1976).
de Vries, L. S., van Haastert, I. C., Benders, M. J. & Groenendaal, F. Myth: cerebral palsy cannot be predicted by neonatal brain imaging. Semin Fetal Neonatal Med 16, 279–287 (2011).
Sarkar, S., Shankaran, S., Laptook, A. R., Sood, B. G., Do, B. & Stoll, B. J. et al. Screening cranial imaging at multiple time points improves cystic periventricular leukomalacia detection. Am. J. Perinatol. 32, 973–979 (2015).
Intrapiromkul, J., Northington, F., Huisman, T. A., Izbudak, I., Meoded, A. & Tekes, A. Accuracy of head ultrasound for the detection of intracranial hemorrhage in preterm neonates: comparison with brain MRI and susceptibility-weighted imaging. J. Neuroradiol. 40, 81–88 (2013).
Hintz, S. R., Barnes, P. D., Bulas, D., Slovis, T. L., Finer, N. N. & Wrage, L. A. et al. Neuroimaging and neurodevelopmental outcome in extremely preterm infants. Pediatrics 135, e32–42 (2015).
Horsch, S., Skiold, B., Hallberg, B., Nordell, B., Nordell, A. & Mosskin, M. et al. Cranial ultrasound and MRI at term age in extremely preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 95, F310–314 (2010).
Steggerda, S. J., de Bruine, F. T., Smits-Wintjens, V. E., Verbon, P., Walther, F. J. & van Wezel-Meijler, G. Posterior fossa abnormalities in high-risk term infants: comparison of ultrasound and MRI. Eur. Radiol. 25, 2575–2583 (2015).
Barnett, M. L., Tusor, N., Ball, G., Chew, A., Falconer, S. & Aljabar, P. et al. Exploring the multiple-hit hypothesis of preterm white matter damage using diffusion MRI. Neuroimage Clin. 17, 596–606 (2018).
Miller, S. P., Ferriero, D. M., Leonard, C., Piecuch, R., Glidden, D. V. & Partridge, J. C. et al. Early brain injury in premature newborns detected with magnetic resonance imaging is associated with adverse early neurodevelopmental outcome. J. Pediatr. 147, 609–616 (2005).
Graeb, D. A., Robertson, W. D., Lapointe, J. S., Nugent, R. A. & Harrison, P. B. Computed tomographic diagnosis of intraventricular hemorrhage. Etiol. Progn. Radiol. 143, 91–96 (1982).
Woodward, L. J., Anderson, P. J., Austin, N. C., Howard, K. & Inder, T. E. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N. Engl. J. Med. 355, 685–694 (2006).
Kidokoro, H., Anderson, P. J., Doyle, L. W., Woodward, L. J., Neil, J. J. & Inder, T. E. Brain injury and altered brain growth in preterm infants: predictors and prognosis. Pediatrics 134, e444–453 (2014).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Nosarti, C., Al-Asady, M. H., Frangou, S., Stewart, A. L., Rifkin, L. & Murray, R. M. Adolescents who were born very preterm have decreased brain volumes. Brain 125(Pt 7), 1616–1623 (2002).
Peterson, B. S., Vohr, B., Staib, L. H., Cannistraci, C. J., Dolberg, A. & Schneider, K. C. et al. Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. JAMA 284, 1939–1947 (2000).
Counsell, S. J., Allsop, J. M., Harrison, M. C., Larkman, D. J., Kennea, N. L. & Kapellou, O. et al. Diffusion-weighted imaging of the brain in preterm infants with focal and diffuse white matter abnormality. Pediatrics 112(1 Pt 1), 1–7 (2003).
Huppi, P. S. MR imaging and spectroscopy of brain development. Magn. Reson. Imaging Clin. N. Am. 9, 1–17, vii (2001).
Kroenke, C. D., Bretthorst, G. L., Inder, T. E. & Neil, J. J. Modeling water diffusion anisotropy within fixed newborn primate brain using Bayesian probability theory. Magn. Reson. Med. 55, 187–197 (2006).
van Wezel-Meijler, G., van der Knaap, M. S., Oosting, J., Sie, L. T., de Groot, L. & Huisman, J. et al. Predictive value of neonatal MRI as compared to ultrasound in premature infants with mild periventricular white matter changes. Neuropediatrics 30, 231–238 (1999).
Roelants-van Rijn, A. M., Groenendaal, F., Beek, F. J., Eken, P., van Haastert, I. C. & de Vries, L. S. Parenchymal brain injury in the preterm infant: comparison of cranial ultrasound, MRI and neurodevelopmental outcome. Neuropediatrics 32, 80–89 (2001).
Valkama, A. M., Paakko, E. L., Vainionpaa, L. K., Lanning, F. P., Ilkko, E. A. & Koivisto, M. E. Magnetic resonance imaging at term and neuromotor outcome in preterm infants. Acta Paediatr. 89, 348–355 (2000).
Aida, N., Nishimura, G., Hachiya, Y., Matsui, K., Takeuchi, M. & Itani, Y. MR imaging of perinatal brain damage: comparison of clinical outcome with initial and follow-up MR findings. Am. J. Neuroradiol. 19, 1909–1921 (1998).
Ho, T., Dukhovny, D., Zupancic, J. A., Goldmann, D. A., Horbar, J. D. & Pursley, D. M. Choosing wisely in newborn medicine: five opportunities to increase value. Pediatrics 136, e482–489 (2015).
Guyatt, G., Oxman, A. D., Akl, E. A., Kunz, R., Vist, G. & Brozek, J. et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 64, 383–394 (2011).
Maalouf, E. F., Duggan, P. J., Counsell, S. J., Rutherford, M. A., Cowan, F. & Azzopardi, D. et al. Comparison of findings on cranial ultrasound and magnetic resonance imaging in preterm infants. Pediatrics 107, 719–727 (2001).
Inder, T. E., Anderson, N. J., Spencer, C., Wells, S. & Volpe, J. J. White matter injury in the premature infant: a comparison between serial cranial sonographic and MR findings at term. Am. J. Neuroradiol. 24, 805–809 (2003).
Whitby, E. H., Paley, M. N., Smith, M. F., Sprigg, A., Woodhouse, N. & Griffiths, P. D. Low field strength magnetic resonance imaging of the neonatal brain. Arch. Dis. Child Fetal Neonatal Ed. 88, F203–208 (2003).
Neubauer, V., Djurdjevic, T., Griesmaier, E., Biermayr, M., Gizewski, E. R. & Kiechl-Kohlendorfer, U. Routine magnetic resonance imaging at term-equivalent age detects brain injury in 25% of a contemporary cohort of very preterm infants. PLoS ONE 12, e0169442 (2017).
Woodward, L. J., Clark, C. A., Bora, S. & Inder, T. E. Neonatal white matter abnormalities an important predictor of neurocognitive outcome for very preterm children. PLoS ONE 7, e51879 (2012).
de Bruïne, F. T., van den Berg-Huysmans, A. A., Leijser, L. M., Rijken, M., Steggerda, S. J. & van der Grond, J. et al. Clinical implications of MR imaging findings in the white matter in very preterm infants: a 2-year follow-up study. Radiology 261, 899–906 (2011).
Iwata, S., Nakamura, T., Hizume, E., Kihara, H., Takashima, S. & Matsuishi, T. et al. Qualitative brain MRI at term and cognitive outcomes at 9 years after very preterm birth. Pediatrics 129, e1138–1147 (2012).
Anderson, P. J., Treyvaud, K., Neil, J. J., Cheong, J. L. Y., Hunt, R. W. & Thompson, D. K. et al. Associations of newborn brain magnetic resonance imaging with long-term neurodevelopmental impairments in very preterm children. J. Pediatr. 187, 58–65.e1 (2017).
Van’t Hooft, J., van der Lee, J. H., Opmeer, B. C., Aarnoudse-Moens, C. S., Leenders, A. G. & Mol, B. W. et al. Predicting developmental outcomes in premature infants by term equivalent MRI: systematic review and meta-analysis. Syst. Rev. 4, 71 (2015).
Benders, M. J., Kersbergen, K. J. & de Vries, L. S. Neuroimaging of white matter injury, intraventricular and cerebellar hemorrhage. Clin. Perinatol. 41, 69–82 (2014).
Limperopoulos, C., Bassan, H., Gauvreau, K., Robertson, R. L. Jr & Sullivan, N. R. et al. Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors? Pediatrics 120, 584–593 (2007).
Limperopoulos, C., Chilingaryan, G., Guizard, N., Robertson, R. L. & Du Plessis, A. J. Cerebellar injury in the premature infant is associated with impaired growth of specific cerebral regions. Pediatr. Res. 68, 145–150 (2010).
Zayek, M. M., Benjamin, J. T., Maertens, P., Trimm, R. F., Lal, C. V. & Eyal, F. G. Cerebellar hemorrhage: a major morbidity in extremely preterm infants. J. Perinatol. 32, 699–704 (2012).
Anderson, P. J., De Luca, C. R., Hutchinson, E., Roberts, G. & Doyle, L. W. Victorian Infant Collaborative Group Underestimation of developmental delay by the new Bayley-III Scale. Arch. Pediatr. Adolesc. Med. 164, 352–356 (2010).
Tam, E. W., Rosenbluth, G., Rogers, E. E., Ferriero, D. M., Glidden, D. & Goldstein, R. B. et al. Cerebellar hemorrhage on magnetic resonance imaging in preterm newborns associated with abnormal neurologic outcome. J. Pediatr. 158, 245–250 (2011).
Pearce, R. & Baardsnes, J. Term MRI for small preterm babies: do parents really want to know and why has nobody asked them? Acta Paediatr. 101, 1013–1015 (2012).
Edwards, A. D., Redshaw, M. E., Kennea, N., Rivero-Arias, O., Gonzales-Cinca, N. & Nongena, P. et al. Effect of MRI on preterm infants and their families: a randomised trial with nested diagnostic and economic evaluation. Arch. Dis. Child Fetal Neonatal Ed. 103, F15–F21 (2018).
Melbourne, L., Chang, T., Murnick, J., Zaniletti, I., Glass, P. & Massaro, A. N. Clinical impact of term-equivalent magnetic resonance imaging in extremely low-birth-weight infants at a regional NICU. J. Perinatol. 36, 985–989 (2016).
Janvier, A. & Barrington, K. Trying to predict the future of ex-preterm infants: who benefits from a brain MRI at term? Acta Paediatr. 101, 1016–1017 (2012).
Novak, I., Morgan, C., Adde, L., Blackman, J., Boyd, R. N. & Brunstrom-Hernandez, J. et al. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907 (2017).
L Orton, J., McGinley, J. L., Fox, L. M. & Spittle, A. J. Challenges of neurodevelopmental follow-up for extremely preterm infants at two years. Early Hum. Dev. 91, 689–694 (2015).
Acknowledgements
L.C. is supported by NIH Grant K23HD069521 and 1R01NS102617-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ibrahim, J., Mir, I. & Chalak, L. Brain imaging in preterm infants <32 weeks gestation: a clinical review and algorithm for the use of cranial ultrasound and qualitative brain MRI. Pediatr Res 84, 799–806 (2018). https://doi.org/10.1038/s41390-018-0194-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0194-6
This article is cited by
-
Human Parechovirus (HPeV) infections: clinical presentations, patterns, and evolution of neonatal brain injury
Journal of Perinatology (2023)
-
Brain injury and long-term outcome after neonatal surgery for non-cardiac congenital anomalies
Pediatric Research (2023)
-
Prematurity and BPD: what general pediatricians should know
European Journal of Pediatrics (2023)
-
Amplitude-integrated EEG recorded at 32 weeks postconceptional age. Correlation with MRI at term
Journal of Perinatology (2022)
-
A neonatal neuroNICU collaborative approach to neuromonitoring of posthemorrhagic ventricular dilation in preterm infants
Pediatric Research (2022)