Abstract
Background
It is known that the heart is not the only organ affected in congenital heart disease (CHD); there is growth restriction of both the brain and the whole body. The protective mechanism of “the brain-sparing phenomenon” re-directs blood flow toward the growing brain in fetuses with CHD. We hypothesized that these changes would result in impaired fetal kidney growth.
Methods
The preoperative ultrasound measurements of kidney length were obtained retrospectively from 452 neonates requiring surgery for CHD. Percentiles were generated based on regression analysis of normative kidney length from three datasets according to both corrected gestational age and to birthweight.
Results
As a cohort, neonates with CHD have significantly enlarged kidneys, with a mean percentile ranging from 54.1–72.7 (p < 0.001), depending on the three normal population datasets used for comparison. The kidneys of neonates with left heart obstruction were consistently demonstrated to be greater than normal, unlike those with cyanotic heart disease which were shown to have either normal or enlarged kidneys, depending on the reference population used.
Conclusions
The kidneys of newborns with CHD are not reduced in size, and on average are larger than normal. The nature of this size discrepancy and its subsequent clinical significance is unknown.
Similar content being viewed by others
Introduction
Congenital heart disease (CHD) is the most common congenital condition, affecting ~9.1 neonates per 1000 live births worldwide.1 Even in non-syndromic children, it is not just the heart that is affected. Rosenthal reported that there are different patterns of prenatal brain and body growth restriction in CHD patients, depending on the type of CHD.2 This growth restriction is thought to be due in part to the changes in the circulation and oxygen saturation levels that occur in some forms of complex CHD.3,4,5
The altered brain development in children with CHD occurs despite the presence of the “brain-sparing phenomenon” in which blood flow to the brain is preferentially preserved at the expense of perfusion of other organs.6 Although renal perfusion in CHD has not yet been studied, it is known to be reduced in pregnancies complicated by placental insufficiency and intrauterine growth restriction,7,8,9 and these offspring have smaller kidneys.10 We hypothesized that the in utero growth of kidneys might be compromised in CHD patients, due to alterations in the fetal circulation.
Whilst fetal renal development in patients with CHD has not been investigated before, there is a known relationship between CHD and renal problems. Indeed, up to 50% of adults with CHD have significantly impaired kidney function.11 The currently known contributors of CHD to kidney disease include cardiac failure, chronic hypoxemia, and acute ischemic injury during cardiac surgery.11 These insults result in histological changes, including glomerulomegaly, interstitial fibrosis, and increased mesangial matrix and cellularity.12,13
Due to these well-recognized alterations in fetal blood flow and observed changes in brain development, we questioned whether CHD also affects kidney development in utero, resulting in reduced kidney size at birth. Such a finding would be highly significant, as the formation of nephrons ceases after week 36 of gestation.14 Beginning ex utero life with a reduced number of nephrons predisposes patients to chronic kidney disease and hypertension, due to reduced functional reserve.14,15
Given the high incidence of co-existing renal tract abnormalities in patients with CHD,16 renal ultrasonography is performed routinely in newborns undergoing neonatal cardiac surgery. We aimed to use these scans to determine kidney length in these patients in the early post-natal period prior to surgical intervention.
Materials and methods
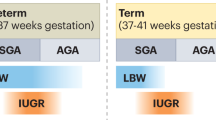
Ethics approval was granted for access to the electronic cardiac database of the Royal Children’s Hospital. To form our retrospective cohort, all patients requiring surgery for CHD within the first 4 weeks of life from January 2011 to August 2017 were identified. Exclusion criteria included: multiple pregnancy; known genetic condition; multiple malformations; abnormal kidney, including horseshoe, multicystic, pelviectasis, duplex system, or presence of edema; absent kidney; and surgery in which only ligation of the patent ductus arteriosus was performed. Patients in whom the ultrasound measurement of the interpolar length of the kidneys was not available were excluded.
The hospital electronic medical records were reviewed to obtain birth and pregnancy information, and reports of interpolar kidney length from the preoperative renal ultrasound. The presence of oligohydramnios or polyhydramnios at any of the available prenatal ultrasounds was recorded. In the electronic medical records, 11 patients were described only as “term”, and two patients did not have their gestation recorded. These were assumed to be born at 40 weeks gestation. With the exception of patients with atrioventricular or ventricular septal defects, diagnoses were broadly sub-categorized as being left-sided obstruction or cyanotic (Table 1).
As a measure of possible ischemic injury to the kidneys, the highest lactate and lowest pH results (from arterial or capillary blood tests) prior to undergoing renal ultrasound were recorded for all patients and compared to normal values (lactate 1.4–4.1 mmol/L; pH 7.31–7.47).17 The highest serum creatinine level prior to renal ultrasound was recorded, and in term patients this was compared to the normal value (mean ± two standard deviations) for that age.18
Statistical analysis
Analyses were carried out using R software (version 3.2.3, R Foundation, Vienna, Austria, http://www.r-project.org/). Patient demographics were summarized using descriptive statistics. One-sample t-tests were used to compare patient birth demographic means to those of a normal population.19
The means of the left and the right kidney did not differ for the population (left mean = 4.52; right = 4.53; p = 0.7), and thus the average kidney length for each patient was used for further analysis. Percentiles were generated based on regression analysis on normative kidney length according to corrected gestational age at the time of ultrasound20 and according to birthweight based on a 1990 published normative data-set of UK newborns with birthweight of at least 2.4 kg.21 As no universally accepted normative data are available on neonatal kidney lengths, post hoc, kidney length in relation to birthweight was compared to a second, more recent Danish population, which reported on newborns over 3 kg birthweight.22 Thirty-eight patients were older than the age range in the reference data. There were 22 patients below and 18 above the birthweight reference range. Data from these patients were included by extrapolation when using the two original populations, but not for the post hoc analysis with a more recent Danish population (in which patients with a birthweight <3 kg were excluded as per the comparison population; n = 304). These percentiles were compared to normal using one-sample t-tests. Pearson correlation coefficients were calculated when assessing the association between kidney length with birthweight and gestational age.
Two-tailed two-sample t-tests were used to compare weight-based means between groups based on whether the patient was appropriate vs. small for gestational age and also for diagnostic group. A two-tailed two-sample t-test was used to compare the rates of oligohydramnios and polyhydramnios in this population to those of a population of normal, uncomplicated pregnancies.23
Results
Population demographics
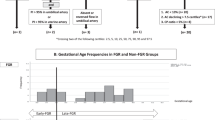
After applying the exclusion criteria, a total of 452 neonates remained for analysis. The characteristics of this population are shown in Table 1. Transposition of the great arteries (28%) and coarctation of the aorta (26%) were the most frequent primary diagnoses. When diagnoses were grouped into broader categories, cyanotic heart disease was present in 52% of the population.
Birth-related information is provided in Table 2. The average gestational age at birth was 38 weeks and 5 days (range from 30 + 4 to 42 + 2). Only one patient was post-term, and 43 were preterm. There was no difference in the birthweight of patients compared to normals, but length and head circumference were significantly smaller in our patients. Thirty-three patients were classed as small for gestational age (SGA; weight < 10th centile for age), and six patients had microcephaly (head circumference < 3rd centile for gestational age).
Kidneys
The mean kidney length in the cohort was 4.5 cm (Table 3). There was a stronger correlation between kidney length and birthweight than with age (r = 0.37 and r = 0.31, respectively).
Regardless of whether it was compared to corrected gestational age or with birthweight (based on the UK reference population), the percentile for kidney length in neonates with CHD was significantly larger than normal (p < 0.001), with a mean percentile of 72.7 or 62.0, respectively (Table 3). This was also true for SGA patients (65.0%, p = 0.002, n = 33). When comparing different diagnostic groups (Table 4), the kidneys of those with left-sided obstruction CHD had larger kidneys than those with cyanotic CHD (p < 0.0001). There was no difference in the weight-based percentiles of those with TGA compared to those with other forms of cyanotic CHD (p = 0.1). Within the subgroup of left-sided obstruction CHD, patients with HLHS had smaller weight-based renal length percentiles than those with coarctation of the aorta (61.0 vs. 69.3, p = 0.04).
In the post hoc analysis using weight-based percentiles from a Danish reference population,22 the cohort of CHD patients with birthweight >3 kg were again demonstrated to have enlarged kidneys (54.1%, p < 0.001) (Table 3). When separated according to the type of CHD, the kidney length of patients with left-sided obstruction CHD remained larger than normal (60.4%, p < 0.001), unlike those with cyanotic CHD (p = 0.3). The weight-based percentiles for our population compared to the two normal populations is plotted in Fig. 1.
Blood tests
When blood results were examined for evidence of ischemia at any time in the postnatal period prior to renal ultrasound assessment, 61% of patients had low pH (<7.31) and 32% had high lactate (>4.1 mmol/L). Preoperative serum creatinine levels were available in 353 term infants, with 107 (30%) of these patients having elevated levels for their age. The mean age of peak creatinine level was 4.4 days. There was no difference in the frequency of acidosis between cyanotic and left-sided obstruction CHD (p = 0.27). However more neonates with cyanotic CHD had elevated lactate compared to those with left-sided obstruction CHD (52.6% vs. 33.1%, p = 0.0002).
Amniotic fluid levels
In total, 22 (18.0%) of the 122 patients with reported amniotic fluid indices had abnormal values, which is significantly higher than the rate in a normal population (8%; p < 0.001). There was no difference in the frequency of abnormal amniotic fluid indices between those with cyanotic and those with left-sided obstruction CHD (p = 0.29). Fourteen (11.5%) of these 122 pregnancies had documentation of oligohydramnios, one of which was due to premature rupture of membranes (this patient was excluded from subsequent analysis). The average birthweight percentile of those with oligohydramnios (28.9%) was significantly reduced compared to those reported to have normal amniotic fluid indices (47.0%, p = 0.018), however there was no difference in mean percentiles (p = 0.3) for renal length.
Eight of the 122 patients with recorded amniotic fluid indices had polyhydramnios. After excluding the five cases with underlying maternal gestational diabetes mellitus (GDM), the rate of polyhydramnios still differed significantly from that of a normal population (p < 0.0001). There was no difference in the mean birthweight percentile (p = 0.3) or in renal percentile (p = 0.14) of those with non-GDM polyhydramnios compared to those with normal amniotic fluid indices.
Discussion
Counter to our hypothesis, we found that newborns with CHD seem to have larger kidneys compared to the normal population. Even patients born SGA with oligohydramnios had enlarged kidneys, which is in contrast to the observation that fetal growth restriction due to placental insufficiency or preeclampsia results in decreased kidney size.10,24 Whilst newborns with cyanotic CHD had smaller kidneys than those with CHD due to left heart obstruction, it seems that they may still be larger than the normal population: age-based kidney percentiles, and weight-based kidney percentiles derived from a UK population21 both indicate enlarged kidneys. However our post hoc analysis against the Danish population,22 which is a larger reference population, but only included term neonates born >3 kg, showed that newborns with left heart obstruction had enlarged kidneys but that those with cyanotic CHD have normal-sized kidneys. Possible explanations for these different results include differences in data quantitation, inclusion of SGA newborns in the former study, or perhaps true differences between the two normal populations. The weight exclusion criteria applied in the latter study meant that a significant proportion of our population (148/452) also needed to be excluded; the smaller patient population size used in the post hoc analysis may have partly contributed to the lack of a statistically significant result. Nonetheless the lack of any reduction in relative kidney size in the newborns with cyanotic heart disease, and significant enlargement in newborns with left-sided obstruction, was surprising and counter to our hypothesis.
The underlying mechanism for these observations is unclear. The in utero changes in fetal blood flow are difficult to assess in CHD and whilst semi-quantitative assessment is possible using ultrasound methods, accurate measurements have only recently become possible with fetal MRI scans. A recent study25 has described the use of MRI T2 mapping and phase-contrast imaging to measure blood oxygen saturation and blood flow, respectively. Of the 30 fetuses in the study with CHD, there were eight fetuses with single ventricle physiology, seven with transposition of the great arteries and seven with tetralogy of Fallot. The study confirmed the common understanding that total combined biventricular output is reduced in hearts with single ventricle physiology. The main focus of the study was to determine the changes in cerebral blood flow patterns in CHD however, so there are no reported data on flow or the oxygen saturation of blood in the descending aorta.
The theoretical changes in regional blood flow and oxygenation in various forms of CHD are described in the seminal text of Rudolph.26 In transposition of the great arteries, which contributed more than half of our cases of cyanotic heart disease, there is a postulated increase in the oxygen saturation to the lower body in comparison to the normal fetus. An increase in oxygen saturation in descending aortic blood is also likely to occur in pulmonary atresia and tricuspid atresia. We hypothesize that this increase in oxygenation with a relatively normal amount of blood flow to the lower body may contribute to increased growth of the kidneys.
The changes in lower body perfusion in fetuses with left heart obstruction due to coarctation and HLHS are different to those of transposition and pulmonary atresia. If alterations in the amount of blood flow and oxygen saturation to the kidneys in fetal life were important, we might expect to see a difference in children with coarctation as compared to HLHS. The magnitude of this change will be related to the degree of arch hypoplasia and is likely to be relatively more minor in isolated coarctation. In addition to the increased volume of flow to the lower body in cases of coarctation, there may also be a slight increase in oxygenation saturation of blood in the lower body. Accordingly, we would expect those with HLHS to have smaller kidneys than those with isolated coarctation of the aorta, which is consistent with our findings.
Whilst the discussion so far assumes that the increased kidney size is reflective of better growth and an increase in nephron number, an alternative hypothesis is that this may be partly due to ischemia and subsequent edema or glomerulomegaly in unaffected nephrons prior to the ultrasound scan. We have however excluded the two patients with overtly edematous kidneys on ultrasound from this study. This pathological remodeling may also incorporate early cyanotic nephropathy, which has previously been detected in patients with CHD from infancy to adulthood.12,27,28 These studies had only a few neonatal patients however, and thus more likely reflect the results of longer duration of cyanosis. Whether patients with CHD as young as 1 week show the same changes of glomerulomegaly is unknown. Nevertheless, immaturity itself is sufficient to cause glomerulomegaly and reduced nephron number.29 Given that underdevelopment of the brain3,4 and body as a whole2 is characteristic of newborns with CHD, perhaps there is also a degree of renal immaturity contributing to pathological remodeling of these kidneys.
We also report the incidental finding of abnormal amniotic fluid levels in CHD. However, the relationship between CHD, urine production and amniotic fluid levels is not straight forward. Since renal anomalies are the most common cause of oligohydramnios,30 the trend we identified for oligohydramnios may indicate impaired fetal kidney function in CHD. A small study31 found that only CHD fetuses that also had heart failure had reduced urine production, and this was associated with either normal (5/11 fetuses) or increased (6/11 fetuses) amniotic fluid levels. Nevertheless, we found no difference in kidney percentiles when comparing those with and without changes in amniotic fluid volume. There were however a limited number (122/452) of patients with reports of amniotic fluid volume available. Furthermore, these patients had a varying number of antenatal ultrasounds performed, which were conducted at variable timepoints.
There are some potential limitations in this retrospective study. Kidney length is only a crude indicator of renal mass. It is possible that the transverse and anterior–posterior dimensions of these kidneys are reduced, meaning that overall renal volume is not altered. Indeed, altered kidney morphology (changes in specific kidney dimensions only) has been shown in SGA newborns,32 and also in adults with chronic kidney disease.33 Unfortunately not all patients had serum creatinine levels available at the time of ultrasound, and urine protein excretion was not available. There is a need for future studies to calculate the kidney volume by using multiple planes of imaging, which was unfortunately not possible in our study due to its retrospective nature and also renal length by ultrasound is the current standard of care for assessment of renal size. The postulated changes in in utero blood flow have not been proven but it may be possible in future studies using MRI to accurately measure these changes. Additional information on kidney function (serial serum creatinine and urine protein excretion) and renal growth would be important to ascertain longer-term functional effects of these renal ultrasound findings
Conclusions
This study provides the first indication that renal alterations exist at the time of birth, with the observation that the kidneys of newborns with CHD are not reduced in size and at least for left-sided obstructive pathologies, leads to renal enlargement. The nature of this increased tissue and its subsequent clinical significance is unknown, and requires further investigation.
References
van der Linde, D. et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J. Am. Coll. Cardiol. 58, 2241–2247 (2011).
Rosenthal, G. L. Patterns of prenatal growth among infants with cardiovascular malformations: possible fetal hemodynamic effects. Am. J. Epidemiol. 143, 505–513 (1996).
Lim, J. M. et al. Cerebral oxygen delivery is reduced in newborns with congenital heart disease. J. Thorac. Cardiovasc. Surg. 152, 1095–1103 (2016).
Licht, D. J. et al. Preoperative cerebral blood flow is diminished in neonates with severe congenital heart defects. J. Thorac. Cardiovasc. Surg. 128, 841–849 (2004).
Matthiesen, N. B. et al. Congenital heart defects and indices of fetal cerebral growth in a nationwide cohort of 924 422 liveborn infants. Circulation 133, 566–575 (2016).
Donofrio, T. M. et al. Autoregulation of cerebral blood flow in fetuses with congenital heart disease: the brain sparing effect. Pediatr. Cardiol. 24, 436–443 (2003).
Stigter, R. H., Mulder, E. J. H., Bruinse, H. W. & Visser, G. H. A. Doppler studies on the fetal renal artery in the severely growth-restricted fetus. Ultrasound Obstet. Gynecol. 18, 141–145 (2001).
Troyano, J. M., Clavijo, M. T., Reyes, I., Martínez-Wallin, I. & Marco, O. Y. Fetal hemodynamic profile in uncommon vessels. Ultrasound Rev. Obstet. Gynecol. 3, 170–177 (2003).
Arduini, D. & Rizzo, G. Fetal renal artery velocity waveforms and amniotic fluid volume in growth-retarded and post-term fetuses. Obstet. Gynecol. 77, 370–373 (1991).
Wang, Y.-P. et al. Effects of a restricted fetal growth environment on human kidney morphology, cell apoptosis and gene expression. J. Renin Angiotensin Aldosterone Syst. 16, 1028–1035 (2014).
Morgan, C., Al-Aklabi, M. & Garcia Guerra, G. Chronic kidney disease in congenital heart disease patients: a narrative review of evidence. Can. J. Kidney Health Dis. 2, 27 (2015).
Gupte, P. A., Vaideeswar, P. & Kandalkar, B. M. Cyanotic nephropathy—a morphometric analysis. Congenit. Heart Dis. 9, 280–285 (2014).
Perloff, J. K., Latta, H. & Barsotti, P. Pathogenesis of the glomerular abnormality in cyanotic congenital heart disease. Am. J. Cardiol. 86, 1198–1204 (2000).
Ingelfinger, J. R. Disparities in renal endowment: causes and consequences. Adv. Chronic Kidney Dis. 15, 107–114 (2008).
Brenner, B. M., Garcia, D. L. & Anderson, S. Glomeruli and blood pressureless of one, more the other? Am. J. Hypertens. 1, 335–347 (1988).
Murugasu, B. et al. Sonographic screening for renal tract anomalies associated with congenital heart disease. J. Clin. Ultrasound 18, 79–83 (1990).
Cousineau, J., Anctil, S., Carceller, A., Gonthier, M. & Delvin, E. E. Neonate capillary blood gas reference values. Clin. Biochem. 38, 905–907 (2005).
Boer, D. P., de Rijke, Y. B., Hop, W. C., Cransberg, K. & Dorresteijn, E. M. Reference values for serum creatinine in children younger than 1 year of age. Pediatr. Nephrol. 25, 2107–2113 (2010).
Olsen, I. E., Groveman, S. A., Lawson, M. L., Clark, R. H. & Zemel, B. S. New intrauterine growth curves based on United States Data. Pediatrics 125,e214–e224 (2010).
Chitty, L. S. & Altman, D. G. Charts of fetal size: kidney and renal pelvis measurements. Prenat. Diagn. 23, 891–897 (2003).
Scott, J. E., Hunter, E. W., Lee, R. E. & Matthews, J. N. Ultrasound measurement of renal size in newborn infants. Arch. Dis. Child. 65, 361–364 (1990).
Schmidt, I. M. et al. Kidney growth in 717 healthy children aged 0-18 months: a longitudinal cohort study. Pediatr. Nephrol. 19, 992–1003 (2004).
Magann, E. F., Sanderson, M., Martin, J. N. & Chauhan, S. The amniotic fluid index, single deepest pocket, and two-diameter pocket in normal human pregnancy. Am. J. Obstet. Gynecol. 182, 1581–1588 (2000).
Latini, G. et al. Foetal growth of kidneys, liver and spleen in intrauterine growth restriction: “programming” causing “metabolic syndrome” in adult age. Acta Pædiatrica 93, 1635–1639 (2004).
Sun, L. et al. Reduced fetal cerebral oxygen consumption is associated with smaller brain size in fetuses with congenital heart disease. Circulation 131, 1313–1323 (2015).
Rudolph, A. M. in Congenital Diseases of the Heart: Clinical-Physiological Considerations (Wiley-Blackwell, 2009).
Variend, S. & Howat, A. J. Renal glomerular size in infants with congenital heart disease and in cases of sudden infant death syndrome. Eur. J. Pediatr. 145, 90–93 (1986).
Zheng, J., Yao, Y., Han, L. & Xiao, Y. Renal function and injury in infants and young children with congenital heart disease. Pediatr. Nephrol. 28, 99–104 (2013).
Brennan, S. & Kandasamy, Y. Ultrasound Imaging of the renal parenchyma of premature neonates for the assessment of renal growth and glomerulomegaly. Ultrasound Med. Biol. 43, 2546–2549 (2017).
Nash, P. Amniotic fluid index. Neonatal Netw. 32, 46–49 (2013).
Xie, J.-X., Lv, G.-R., Chen, Q.-Y. & Hou, M. The effect of fetal congenital heart disease on in utero urine production rate. Prenat. Diagn. 32, 536–541 (2012).
Konje, J. C., Okaro, C. I., Bell, S. C., de Chazal, R. & Taylor, D. J. A cross-sectional study of changes in fetal renal size with gestation in appropriate- and small-for-gestational-age fetuses. Ultrasound Obstet. Gynecol. 10, 22–26 (1997).
Nakazato, T., Ikehira, H. & Imasawa, T. Determinants of renal shape in chronic kidney disease patients. Clin. Exp. Nephrol. 20, 748–756 (2016).
Acknowledgements
The Murdoch Children’s Research Institute is supported by the Victorian Government’s Operational Infrastructure Support Program. The Heart Research Group is supported by Big W and RCH 1000 of the Royal Children’s Hospital Foundation.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: G.B.S., D.Z., J.Y.K., and M.M.H.C. Drafting the article or revising it critically for important intellectual content: G.B.S., D.Z., J.Y.K., and M.M.H.C. Final approval of the version to be published: G.B.S., D.Z., J.Y.K., and M.M.H.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scholes, G.B., Zannino, D., Kausman, J.Y. et al. Altered in utero kidney development in newborns with congenital heart disease. Pediatr Res 85, 644–649 (2019). https://doi.org/10.1038/s41390-018-0163-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0163-0