Abstract
Background
Pulmonary hypertension (PH) is multifactorial in origin and may develop early in children with sickle cell disease (C-SCD). Potential etiologies are hemolysis-induced endothelial dysfunction, left ventricular (LV) dysfunction, and chronic hypoxia. Nocturnal hypoxia (NH) in C-SCD is known to be a sequela of obstructive sleep apnea (OSA). The primary objective of this study is to correlate polysomnographic evidence NH with echocardiographic measures of PH in C-SCD.
Methods
We performed a retrospective chart review of 20 C-SCD (Hemoglobin SS), who had polysomnography and echocardiogram performed within a narrow time interval, and 31% of them had pre-existing cardiac conditions. Tricuspid regurgitant jet velocity (TRJV) ≥ 2.5 m/s was considered as an indicator of PH.
Results
Twenty-five percent of the subjects had NH. Forty percent of C-SCD, predominantly male, had evidence of PH based on an elevated TRJV. Children with NH compared to non-NH had significantly worse baseline hypoxemia (p < 0.001), higher TRJV (p = 0.005), and higher LV end-diastolic diameters (p = 0.009). The severity of NH was influenced by OSA. However, PH was not associated with OSA or duration of hydroxyurea therapy.
Conclusion
Our study indicates that NH is associated with PH in C-SCD, and that screening for NH may help to identify C-SCD with higher morbidity risk.
Similar content being viewed by others
Introduction
Pulmonary hypertension (PH) is a well-known and often fatal complication of sickle cell disease (SCD).1,2,3 About 11–46% of children with SCD have been found to have PH by echocardiogram (ECHO).4,5,6,7 However, cardiac catheterization confirms the PH diagnosis in only 6% of subjects in a large adult study.8 The pathophysiology of PH in SCD is multifactorial and is different from that of primary PH in many aspects. For example, in patients with primary PH, pulmonary vascular resistance is increased, while only one-third of SCD patients with PH demonstrate pulmonary vasculopathy.9 Instead, PH in SCD is more likely to be a sequela of increased pulmonary blood flow secondary to chronic anemia, chronic hemolysis, and chronic hypoxemia. Adults with SCD and PH have also been shown to have elevated LV filling pressures, a measure of left heart failure.10 Thus, PH associated with SCD is currently categorized as PH with an unclear multifactorial mechanism (PH Group 5).9,11 Hydroxyurea therapy reduces SCD-related complications by increasing fetal hemoglobin (HbF) percentage. However, the effect of hydroxyurea in preventing the development of PH in pediatric SCD is not well established, and more investigations are necessary.12
Chronic nocturnal hypoxia (NH) is common in children with SCD (C-SCD) and may also play a role in the development of PH. NH is diagnosed when oxygen saturation (SpO2) drops below 90% for ≥20% of the total sleep time (TST).13,14 Rogers et al. analyzed polysomnography from a cohort of 41 children with HbSS mutation.15 Average apnea–Hypopnea Index (AHI) in this group was 6.2, with 8% of TST spent with hypoxia. This group also demonstrated a higher prevalence of sleep apnea and NH in comparison to the control HbSC group.15 However, there is a lack of adequate evidence in C-SCD establishing a relationship between NH and PH.
C-SCD have increased hemolysis, resulting in the release of arginine and free hemoglobin.4 Free hemoglobin combines with NO (nitric oxide), a potent pulmonary vasodilator, which results in rapid clearance and decreased bioavailability of NO. This results in pulmonary vasoconstriction. Thus, increased hemolysis may lead to PH in SCD, and there could be a positive correlation between LDH, a marker of chronic hemolysis, and PH.16
Recognizing PH in the pediatric population can be uniquely challenging, given the limitations of symptom self-reporting, variations in parental perception of symptoms, and the inability to perform reliable diagnostic testing. Rosenzweig et al. cited an average time of 1–2 years from the start of symptoms to the diagnosis of PH, irrespective of etiology.17 PH causes a pressure overload on the right ventricle, which initially leads to ventricular hypertrophy and later, ventricular dilation. The gold standard for diagnosis of PH is a mean pulmonary artery pressure ≥25 mmHg measured by cardiac catheterization.18 However, cardiac catheterization is an invasive procedure. Thus, echocardiogram is recommended as the first-line diagnostic investigation when suspecting PH.19 Echocardiograms provide pressure estimates as well as structural assessments, which are essential in the identification and management of PH. Classically, tricuspid regurgitant jet velocity (TRJV) using echocardiogram has been used to assess pulmonary artery systolic pressures via the modified Bernoulli equation (PA systolic pressure = 4[TRmax]2). This assumes a right atrial pressure and requires a non-obstructed right ventricular outflow tract. A TRJV ≥ 2.5 m/s has been used as a surrogate marker of PH in many adult and pediatric studies on PH in SCD, and Kato et al. demonstrated that TRJV ≥ 2.5 m/s predicts a higher 3-year mortality rate in C-SCD,4,8,20,21 The American Heart Association/American Thoracic Society guidelines from 2015 state that pulmonary hypertension, as diagnosed by TRJV ≥ 2.5 m/s by echocardiogram can be considered as a threshold for more aggressive treatment for PH in C-SCD.19
It has been postulated that LV dysfunction may cause secondary pulmonary hypertension and thus a possible etiology for elevation in TRJV.22 Lower oxygen saturation during sleep is associated with increased LV diastolic dimensions and LV dysfunction which even precedes PH in C-SCD.23 Thus, we have also measured left ventricular end-diastolic diameter (LVEDD) Z score.
The objectives of this study are to correlate polysomnographic evidence of NH with an echocardiographic measure of PH (TRJV), to identify possible predictors of NH and PH, and to compare pulmonary function tests, ECHO parameters including TRJV and LVEDD in C-SCD with and without NH.
Material and methods
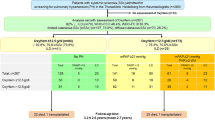
We completed a retrospective chart review of 56 C-SCD ages 4–18 years who had been followed by the comprehensive multidisciplinary sickle cell program at Penn State Hershey Children’s Hospital (Fig. 1) (http://childrens.pennstatehealth.org/hematology-oncology/patient-care-and-treatment/sickle-cell-anemia). Of this cohort, 20 HbSS children had both complete echocardiography and polysomnography performed. In three C-SCD, TRJV could not be estimated from the ECHO, and they were excluded from the study. We did not include children with HbSC and HbS/beta-thalassemia mutations since they have significantly better outcomes in comparison to HbSS. Children on oxygen or PH-targeted therapies were also excluded. At our SCD program, on the day of the comprehensive clinic visit, blood tests and pulmonary function tests (PFT) are routinely performed in addition to ECHOs, whenever necessary. Thus, the study participants are typically at their clinical baseline at these visits. Results of the abovementioned tests were obtained and analyzed. Of note, none of the lab, PFT, or ECHO data considered in this study was obtained during an inpatient stay. Patients’ demographics and other disease-related information were also collected including (i) number of ACS episodes and blood transfusions within the last 3 years before the ECHO (ii) the number of years of hydroxyurea therapy, and (iii) laboratory parameters related to SCD including total hemoglobin, HbF, LDH, and creatinine.
Polysomnography
We retrieved the polysomnographic reports and accessed the original polysomnography tracings whenever necessary. Presumed OSA due to a history of snoring (evaluation for obstructive sleep apnea) was the most common indication for polysomnography in our study subjects (17/20). The following parameters were defined and extracted: (i) apnea–hypopnea index (AHI): this represents the total numbers of central apneas, obstructive apneas, hypopneas, and/or mixed apneas per hour, (ii) NH was diagnosed when a subject spent more than 20% of TST with SpO2<90%; and percentage of TST spent with SpO2<90% was calculated, (iii) end tidal CO2 (ETCO2) >45 mmHg was recognized in hypercapnic range, and percentage distribution of ETCO2 >45 mmHg was calculated, and (iv) SpO2 at baseline while the subject was awake, and the lowest SpO2 during the polysomnogram.
Echocardiogram
All echocardiograms were re-read by a pediatric cardiologist blinded to the sleep study results. In our cohort, the indications for echocardiography were routine surveillance referral for pulmonary hypertension from SCD clinic (59%), follow-up of left ventricular dilation and other minor cardiac pathology from Pediatric Cardiology clinic (32%), and as a part of post-hospitalization work-up for SCD-related complications (9%). There was no other baseline cardiac pathology aside from LV dilation which is presumed to be due to chronic output states in SCD. Pulmonary hypertension was suspected when TRJV ≥ 2.5 m/s. LVEDD-Z were also measured. Each echocardiogram was thoroughly reviewed to ensure the absence of other hemodynamically significant lesions.
Statistical analysis
We divided the subjects into two groups for subgroup analysis; NH and non-NH. Continuous variables were compared using a two-sample t-test, while categorical variables were compared using Chi-square/Fisher’s exact test. Multiple linear regression analyses were conducted to identify the key predictors of NH and TRJV; and various factors including DLCO, hemoglobin, HbF, AHI, SpO2 at baseline, duration of hydroxyurea therapy were used as predictors. p < 0.05 was considered a cutoff value for significance (*), and p < 0.001 was considered highly significant (**). SPSS statistics (V24) and SAS 9.4 were used for the statistical analyses.24,25
We used the difference in TRJV between NH vs. non-NH groups to set the model equation for power estimation. We set the criteria of power (1 − β) at 0.80 and α = 0.05, two-tailed. The observed power of the study was 0.84, and an estimated 22 subjects were required to achieve the desired power of >0.80. G*power was used to estimate the power of the study. (http://www.gpower.hhu.de/en.html.) Penn State institutional review board approved the study.
Results
Twenty subjects (median age of 10 years, range 2–18 years, M: F = 9:11) with HbSS genotype were included in the study (supplemental table S1). Significant male predominance was recognized among the subjects with pulmonary hypertension using chi-square test (p = 0.005*) (Table 1). To demonstrate that both the ECHO and the sleep study were performed during the steady state, we compared the hemoglobin levels in all study participants around the time of their studies. The mean hemoglobin level near the time of the sleep study was 8.04 ± 1.17 mg/dL. This was not statistically different from the mean hemoglobin level near the time of ECHO (8.02 ± 1.08 mg/dL) (p = 0.9). Since ACS or blood transfusion can influence the outcome of ECHO, we reviewed the interval history between ECHO and polysomnography (study interval). Seven C-SCD received a blood transfusion during the study interval, and three of them received two or more transfusions. However, of those seven children, only two subjects had ECHO post blood transfusion with a long interval of 4 and 5 months, respectively. In addition, neither of the ECHOs was consistent with PH. Likewise, four C-SCD had one ACS each during the study interval, and only one of them had and ECHO performed after the ACS (8 months).
Polysomnography
Five out of 20 subjects (25%) had NH and children with NH had significantly higher TRJV (p = 0.004) in comparison to the non-NH group (Table 2). Only three subjects were hypercapnic during the sleep study. Two of them had not had a tonsillectomy and adenoidectomy (T&A), while the third subject had undergone T&A 7 years before the polysomnography. Three out of five children with NH, and four out of fifteen in the non-NH group had T&A even before the sleep study. AHI in children with NH mostly comprised obstructive hypopneas. NH had a significant association AHI (Pearson correlation = 0.57*, p = 0.008*), LVEDD-Z (Pearson correlation = 0.59*, p = 0.007*) and inverse relation with baseline awake SpO2 (Pearson correlation = −0.69*, p = 0.001*). Likewise, multiple linear regression analysis also indicated that AHI and baseline SpO2 were the significant predictors of NH. However, the model excluded LVEDD-Z (regression model I) (Table 3).
Echocardiogram
Eight study participants (40%) had a TRJV ≥ 2.5 m/s, and thus met the study’s diagnostic criteria for PH. Eleven out of 20 patients (55%) had LV dilation with mean LVEDD-Z of 2.10 ± 1.68. Multiple linear regression model II suggested that only NH was the possible predictor of high TRJV and also excluded other covariables including AHI, length of hydroxyurea therapy, hemoglobin/ HbF level, LVEDD, and DLCO as nonsignificant (Table 3). There was a significant correlation between NH and TRJV (Pearson correlation = 0.48, p = 0.032*) (Fig. 2).
Using the chi-square test (Fisher’s exact test), we found a significant correlation between PH and NH (p = 0.005) (Table 4).
Discussion
Previous studies have shown a widely variable prevalence of PH in C-SCD. Onyekwere et al. reported that 48% of subjects in a cohort of 52 C-SCD (ages 8–24 years) had a positive screening test with TRJV ≥ 2.5 m/s, and 11% of them had significantly higher TRJV (>3 m/s).6 Colombati et al. conducted a cohort study on 37 C-SCD (mean age of 6.2 years) and diagnosed 15 out of 37 children (41%) as PH positive (TRJV ≥ 2.5 m/s), at screening or during subsequent visits.26 These results indicate that PH may develop at an earlier age than expected. However, Sedrak et al. demonstrated that only 4 out of 38 (8.3%) C-SCD with HbSS mutation had increased TRJV ≥ 2.5 m/s which they speculated was due to the younger median age of their cohort (12 years).3 Our study demonstrated that 40% of C-SCD had elevated TRJV, which is consistent with the reports of Onyekwere et al. and Colombati et al.6,26 Since a significant percentage of the study subjects (32%) underwent an echocardiogram due to note of LV dilation on a previous echocardiogram/visit, our cohort may have had more cardiac pathology, and may not represent the general pediatric HbSS population.
All of our patients had polysomnography when they were at their clinical baseline. Some sleep studies were postponed due to illness, SCD-related crises, or hospitalization. There is a wide variation among the reported mean baseline SpO2 in C-SCD. Halphen et al., in a prospective study of 39 C-SCD, documented a mean baseline SpO2 of 97% with a range of (89–100%). We found that the C-SCD without NH had baseline SpO2 of 97 ± 2% and C-SCD with NH had baseline SpO2 of 92 ± 2% with an average of 96 ± 3% for the whole cohort.27
SCD-related complications tend to differ according to sex. Platt et al. reported that the disease outcome in SCD females was significantly better than that of males, whose life expectancy is 6 years less.28 Similarly, our study demonstrated that females had a lower prevalence of PH, which is a predictor of SCD-related mortality. However, identical studies in C-SCD are not available to compare our results.
We found a significant association between PH, as inferred by an elevated TRJV, and NH. This result was consistent with adult studies that cited a relationship between NH and higher pulmonary artery pressures in patients with obstructive sleep apnea (OSA) but without SCD.29,30 Few prospective studies have shown an association between lower baseline oxygen saturation with elevated TRJV in C-SCD.5,7 To the best of our knowledge, our study is the first to demonstrate that children with nocturnal hypoxia had higher TRJV. However, in our cohort, other independent variables including Hb/HbF levels, the degree of hemolysis (as indicated by LDH), number of ACS crisis, or blood transfusions failed to demonstrate an association with PH.
Previously, it was hypothesized that hydroxyurea therapy would be helpful to prevent progression of PH in SCD patients. However, prospective studies have not established hydroxyurea therapy as prevention from developing PH.12 Likewise, our study did not demonstrate a correlation between length of hydroxyurea therapy and PH severity.
C-SCD frequently have an increased incidence of OSA due to enlarged upper airway lymphoid tissues,31 and NH is often a result of OSA.31,32 Presumed OSA due to a history of snoring (17/20) was the most common indication for polysomnography in our study subjects. Despite a strong correlation between the degree of NH and AHI, NH is likely to be multifactorial in origin and is influenced by other factors such as baseline oxygen saturation as indicated by multiple regression model I. This observation is further supported by the fact that NH persists irrespective of history of T&A, which is the typical corrective treatment for OSA. Our study results indicate that NH, but not AHI is a predictor of TRJV. This finding was somewhat surprising since the degree of sleep apnea is usually considered a primary predictor of sleep-related breathing disorders, including PH. Needleman et al. demonstrated that in C-SCD, baseline hypoxia had a better predictive value for NH, than the degree of OSA.33 Thus, we conclude that in C-SCD the focus of sleep-disordered breathing should be NH, which may have a strong association with PH.
The limitations of this study include its moderate sample size, its retrospective nature, and the variable time lag between the sleep studies and echocardiograms. A multicenter prospective cohort study would be necessary to collect longitudinal data to monitor the pattern of NH and PH over a period of time. Since this was a correlational study, we tried to include the subjects who had both polysomnography and ECHO done within a narrow time range. PFTs were done mostly on the day of ECHO. Since the median interval between the sleep study and ECHO was 158 days, we also evaluated the interval history for ACS and blood transfusion which are two factors that can affect cardiovascular stability and ECHO findings. Because the hemoglobin obtained during the sleep study and ECHO were no different and there was the considerable time gap between ACS/blood transfusion and ECHO, we conclude that the ECHOs were performed at stable baseline condition. Since this was a retrospective study, we could only use TRJV ≥ 2.5 m/s as a surrogate marker of PH instead of measuring mean systolic pulmonary artery pressure invasively.
Our study underscored the importance of routine screening for NH in SCD children. Five of the study subjects were on nocturnal oxygen therapy post polysomnography. It was beyond the scope of our study to follow the PH indices over a period of time after initiation of oxygen therapy. At our institution, it can take months to schedule polysomnography, and sometimes it may also be associated with significant out-of-pocket costs for the family. Considering those facts, we would like there to be a more prominent role in routine overnight oximetry studies in the evaluation of C-SCD. Perhaps, annual screening nocturnal oximetry studies could be undertaken starting the age of 3 years. NH is likely to play a significant role in the development of PH. In adults with SCD, PH is a crucial predictor of mortality. Thus, finding and treating patients with NH may prevent or delay progression to PH in childhood or early adulthood. Ultimately, this may have a positive effect on overall life expectancy.
Thus, we conclude that in C-SCD, the focus of sleep-disordered breathing should be NH, which may have an association with pulmonary hypertension.
References
Castro, O. & Gladwin, M. T. Pulmonary hypertension in sickle cell disease: mechanisms, diagnosis, and management. Hematol. Oncol. Clin. North. Am. 19, 881–896 (2005).
Ataga, K. I. et al. Pulmonary hypertension in sickle cell disease. Am. J. Med. 117, 665–669 (2004).
Sedrak, A., Rao, S. P., Miller, S. T., Hekmat, V. & Rao, M. A prospective appraisal of pulmonary hypertension in children with sickle cell disease. J. Pediatr. Hematol. Oncol. 31, 97–100 (2009).
Kato, G. J., Onyekwere, O. C. & Gladwin, M. T. Pulmonary hypertension in sickle cell disease: relevance to children. Pediatr. Hematol. Oncol. 24, 159–170 (2007).
Minniti, C. P. et al. Elevated tricuspid regurgitant jet velocity in children and adolescents with sickle cell disease: association with hemolysis and hemoglobin oxygen desaturation. Haematologica 94, 340–347 (2009).
Onyekwere, O. et al. Pulmonary hypertension in children and adolescents with sickle cell disease. Pediatr. Cardiol. 29, 309–312 (2008).
Pashankar, F. D., Carbonella, J., Bazzy-Asaad, A. & Friedman, A. Prevalence and risk factors of elevated pulmonary artery pressures in children with sickle cell disease. Pediatrics 121, 777–782 (2008).
Hebson, C. et al. Elevated tricuspid regurgitant velocity as a marker for pulmonary hypertension in children with sickle cell disease: less prevalent and predictive than previously thought? J. Pediatr. Hematol. Oncol. 37, 134–139 (2015).
Simonneau, G. et al. Updated clinical classification of pulmonary hypertension. J. Am. Coll. Cardiol. 54, S43–S54 (2009).
Castro, O., Hoque, M. & Brown, B. D. Pulmonary hypertension in sickle cell disease: cardiac catheterization results and survival. Blood 101, 1257–1261 (2003).
Chaudry, R. A. et al. Paediatric sickle cell disease: pulmonary hypertension but normal vascular resistance. Arch. Dis. Child. 96, 131–136 (2011).
Gladwin, M. T. et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. New Engl. J. Med. 350, 886–895 (2004).
Schulz, R., Hummel, C., Heinemann, S., Seeger, W. & Grimminger, F. Serum levels of vascular endothelial growth factor are elevated in patients with obstructive sleep apnea and severe nighttime hypoxia. Am. J. Respir. Crit. Care. Med. 165, 67–70 (2002).
Hoth, K. F., Zimmerman, M. E., Meschede, K. A., Arnedt, J. T. & Aloia, M. S. Obstructive sleep apnea. Sleep. Breath. 17, 811–817 (2013).
Rogers, V. E., Lewin, D. S., Winnie, G. B. & Geiger-Brown, J. Polysomnographic characteristics of a referred sample of children with sickle cell disease. J. Clin. Sleep. Med. 6, 374 (2010).
Kato, G. J. et al. Lactate dehydrogenase as a biomarker of hemolysis-associated nitric oxide resistance, priapism, leg ulceration, pulmonary hypertension, and death in patients with sickle cell disease. Blood 107, 2279–2285 (2006).
Rosenzweig, E., Feinstein, J., Humpl, T. & Ivy, D. Pulmonary arterial hypertension in children: diagnostic work-up and challenges. Prog. Pediatr. Cardiol. 27, 7–11 (2009).
McLaughlin, V. V. et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on expert consensus documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J. Am. Coll. Cardiol. 53, 1573–1619 (2009).
Abman, S. H. et al. Pediatric pulmonary hypertension: guidelines from the American Heart Association and American Thoracic Society. Circulation 132, 2037–2099 (2015).
Harrington, J. K. et al. Longitudinal analysis of echocardiographic abnormalities in children with sickle cell disease. J. Pediatr. Hematol. Oncol. 39, 500–505 (2017).
Ambrusko, S. J. et al. Elevation of tricuspid regurgitant jet velocity, a marker for pulmonary hypertension in children with sickle cell disease. Pediatr. Blood Cancer 47, 907–913 (2006).
Shah, R. V. & Semigran, M. J. Pulmonary hypertension secondary to left ventricular systolic dysfunction: contemporary diagnosis and management. Curr. Heart Fail. Rep. 5, 226–232 (2008).
Johnson, M. C. et al. Left ventricular hypertrophy and diastolic dysfunction in children with sickle cell disease are related to asleep and waking oxygen desaturation. Blood 116, 16–21 (2010).
IBM Corp. IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp, Armonk, NY, 2016) (Released).
SAS Institute. Base SAS 9.4 Procedures Guide (SAS Institute, 2015). https://www.sas.com/en_us/software/sas9.html
Colombatti, R. et al. Pulmonary hypertension in sickle cell disease children under 10 years of age. Br. J. Haematol. 150, 601–609 (2010).
Halphen, I. et al. Severe nocturnal and postexercise hypoxia in children and adolescents with sickle cell disease. PLoS ONE 9, e97462 (2014).
Platt, O. S. et al. Mortality in sickle cell disease--life expectancy and risk factors for early death. New Engl. J. Med. 330, 1639–1644 (1994).
Sanner, B. M., Doberauer, C., Konermann, M., Sturm, A. & Zidek, W. Pulmonary hypertension in patients with obstructive sleep apnea syndrome. Arch. Intern. Med. 157, 2483–2487 (1997).
Kessler, R. et al. Pulmonary hypertension in the obstructive sleep apnoea syndrome: prevalence, causes and therapeutic consequences. Eur. Respir. J. 9, 787–794 (1996).
Strauss, T. et al. Upper airway lymphoid tissue size in children with sickle cell disease. Chest 142, 94–100 (2012).
Kaleyias, J. et al. Severity of obstructive sleep apnea in children with sickle cell disease. J. Pediatr. Hematol. Oncol. 30, 659–665 (2008).
Needleman, J. P. et al. Mechanisms of nocturnal oxyhemoglobin desaturation in children and adolescents with sickle cell disease. Pediatr. Pulmonol. 28, 418–422 (1999).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Mondal, P., Stefek, B., Sinharoy, A. et al. The association of nocturnal hypoxia and an echocardiographic measure of pulmonary hypertension in children with sickle cell disease. Pediatr Res 85, 506–510 (2019). https://doi.org/10.1038/s41390-018-0125-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0125-6
This article is cited by
-
Sleep disordered breathing and its relation to stroke and pulmonary hypertension in children with sickle cell disease: a single-center cross-sectional study
Annals of Hematology (2023)
-
Pulmonary Hypertension in Children with Sickle Cell Disease: a Review of the Current Literature
Current Pediatrics Reports (2019)