Abstract
Background
The glucocorticosteroid betamethasone is routinely administered prior to anticipated preterm birth to enhance lung maturation. While betamethasone also increases fetal pulmonary blood flow and reduces pulmonary vascular resistance (PVR), we investigated whether alterations in right ventricular (RV) function and ductal characteristic impedance (Zc) additionally contributed to rises in pulmonary flow.
Methods
Anesthetized preterm fetal lambs with (n = 10) or without (n = 8) betamethasone pretreatment were instrumented with a pulmonary trunk micromanometer and ductus arteriosus and left pulmonary artery (PA) flow probes to calculate Zc, and obtain RV output and hydraulic power.
Results
Betamethasone (1) increased systolic and pulse arterial pressures (P ≤ 0.04), heart rate (P = 0.02), and lowered PVR (P = 0.04), (2) increased mean (P = 0.008) and systolic (P = 0.004), but not diastolic PA flow or PA Zc, (3) increased ductal Zc (P < 0.05), but not ductal flow, (4) increased RV output (P = 0.03) and the proportion of PT flow distributed to the lungs (P = 0.02), and (5) increased RV power (P ≤ 0.002).
Conclusion
An increased fetal PA blood flow after betamethasone therapy was confined to the systole and underpinned not only by decreased PVR, but also greater RV power and preferential distribution of an augmented RV systolic outflow to the lungs due to higher ductal Zc.
Similar content being viewed by others
Introduction
An antenatal glucocorticosteroid, such as betamethasone, is routinely administered to women at 24–34 weeks’ gestation who are at risk of premature delivery, in order to accelerate fetal lung maturation and increase surfactant production, and thus reduce the incidence and severity of respiratory distress syndrome in preterm babies.1,2 In addition to their maturational actions on respiratory elements, however, antenatal steroids also alter pulmonary hemodynamics, as mean pulmonary artery (PA) blood flow is increased and pulmonary vascular resistance (PVR) is reduced in preterm fetal lambs,3,4 while PA resistance index is decreased on Doppler echocardiography in preterm human fetuses.5,6
Although an increase in fetal PA blood flow observed with betamethasone therapy has been attributed to the fall in PVR,3 this may not be the entire explanation for at least two reasons. First, antenatal betamethasone therapy results in maturation of cardiomyocyte growth patterns7 and can increase myocardial contractility and metabolism,8 both of which may enhance right ventricular (RV) pump function and thus contribute to an increase in PA blood flow via a rise in the RV output. Second, maintenance of ductal patency in the fetus is dependent on prostaglandins, the local production and pharmacological effects of which may be suppressed by glucocorticosteroids,9 potentially leading to increased ductal tone with a greater distribution of RV output toward the lungs.
These potential mechanisms are especially relevant in the context of recent analyses of phasic pulmonary trunk (PT), ductus arteriosus, and PA flow interactions10,11,12 that have provided greater understanding about the basis of fetal pulmonary blood flow patterns than flow data averaged over the cardiac cycle. Thus, in line with well-established data,13,14 only a minor portion (<20%) of RV output entering the PT traversed the lungs in the baseline state,10 with the rest crossing the ductus into the descending thoracic aorta.13,15,16 On the other hand, phasic analysis indicated that most (~60%) of the initial RV systolic flow passed into the PA rather than the ductus, due to characteristic impedance (Zc) of the ductus being considerably higher than PA Zc. However, PA flow then fell abruptly to near-zero in mid-systole because of high downstream PVR, effectively directing subsequent RV outflow across the ductus.10 Furthermore, ~35% of the systolic PA in flow did not pass through the lungs, but was instead transiently stored within a compliant reservoir (windkessel) formed by elastic conduit PAs, and discharged in the ensuing diastole as a backflow (i.e., negative flow) that then crossed the ductus.10,11,12,17
Moreover, increases in fetal PA blood flow were supported by a range of changes in these interactions. Thus, two-thirds of rise in PA flow occurring after a reduction in lung liquid volume arose from an increase in RV pump function which resulted in a higher RV systolic outflow that was distributed near-equally to the lungs and across the ductus, with the remaining rise in flow due to reduced PA diastolic backflow.12 By contrast, although two-thirds of an elevation in PA blood flow evident after adenosine infusion was also related to augmented RV pump function, the associated increase in RV output passed exclusively to the lungs, with the remaining increase in PA flow due to emergence of positive diastolic flow that was related to increased diastolic discharge from a central pulmonary reservoir situated in the PT region.11
Apart from the observation that mean diastolic and end-diastolic flows were less negative in preterm fetal lambs,3 however, little is known about the characteristics and relative importance of phasic interactions which contribute to rises in fetal PA blood flow after antenatal betamethasone therapy. This study therefore tested the hypothesis that this therapy, via changes in RV function, ductal tone, and pulmonary reservoir discharge, altered phasic PA flow interactions in the fetus. The aim of the study was to determine the nature of these interactions in anesthetized preterm fetal lambs by analysis of PT, ductal and PA phasic flows, ductal and PA Zc, pulmonary reservoir function, and RV pump function via calculation of hydraulic power indices.
Methods
The studies conformed to the guidelines of the National Health and Medical Council of Australia and were approved by the Murdoch Children’s Research Institute Animal Ethics Committee.
Experimental preparation
Betamethasone (Celestone Chronodose, 11.4 mg, Merck Sharp & Dohme, Australia) was administered by intramuscular injection to pregnant Border-Leicester cross ewes (n = 10) 48 and 24 h before the day of study, a regimen similar to that recommended in clinical practice for anticipated preterm birth.2 Control ewes (n = 8) received no betamethasone and were studied during the same time period as treated animals. Investigators were blinded to the treatment given to ewes, with betamethasone injections allocated and administered by senior Animal Facility staff.
On the day of the experiment at a gestation of 128 ± 1 days (mean ± SD, term = 147 days), ewes were anesthetized with intramuscular ketamine (5 mg kg−1) and xylazine (0.1 mg kg−1), followed by 4% isoflurane given by mask. After tracheal intubation, anesthesia was maintained with isoflurane (2–3%) and nitrous oxide (10–20%) delivered by ventilator in O2-enriched air supplemented by intravenous infusion of ketamine (1–1.5 mg kg−1 h−1), midazolam (0.1–0.15 mg kg−1 h−1), and fentanyl (2–2.5 mcg kg−1 h−1). Transcutaneous oxygen saturation (SpO2) was monitored continuously with a pulse-oximetric sensor applied to the ear. The right common carotid artery was cannulated for monitoring of blood pressure and regular blood gas analysis (ABL800, Radiometer, Copenhagen, Denmark), with ventilation of the ewe adjusted to maintain arterial O2 tension (Pao2) at 100–120 mmHg and CO2 tension (Paco2) at 35–40 mmHg.
Following exposure of the uterus through a midline laparotomy, the fetal head was exteriorized and placed in a saline-filled glove to prevent loss of lung liquid. Catheters were inserted into the left axillary or external jugular vein for fluid administration. Catheters were also inserted into the left axillary or common carotid artery for pressure measurement and blood sampling, and a 3.5-Fr micromanometer catheter (SPR-524, Millar Instruments, Houston, TX) was passed into the aortic trunk (AoT) to measure the high-fidelity pressure. After delivery of the left forelimb and upper thorax, a thoracotomy was performed in the third left interspace, the pericardium was incised and major vessels were carefully dissected for the placement of transit-time flow probes (Transonic Systems, Ithaca, NY) around the ductus (8 or 10 mm PAU series) and left PA (4 or 6 mm PS series). To measure pulmonary pressures, a fluid-filled catheter and a second 3.5-Fr micromanometer catheter were inserted into the PT close to its junction with the ductus and common PA via purse-string sutures. A fluid-filled catheter was also introduced through the appendage into the left atrium (LA) in all animals. Note that the thoracotomy was not surgically closed after completion of instrumentation so as to (1) allow ready access to flow probes for instillation of perivascular acoustic gel and (2) avoid the risk of compression of surrounding structures (particularly the upper lobe of the left lung) by the ductal flow probe.
Experimental protocol
Hemodynamics were allowed to stabilize for 10–15 min after the completion of the surgery. Subsequently, an aortic sample was withdrawn for blood gas analysis, and physiologic data recorded onto computer in both groups. After completion of the study protocol, animals were euthanased with intravenous sodium pentobarbitone (100 mg kg−1).
Physiological data
AoT, PT, and LA fluid-filled catheter pressures were measured with transducers referenced to LA level and calibrated against a water manometer before each study. Catheter, micromanometer, and flow probe signals were digitized at a sampling rate of 1 kHz using customized acquisition and analysis software (Spike2, Cambridge Electronic Design, Cambridge, UK), with mains electrical noise removed via a 48 Hz low-pass filter.
AoT and PT micromanometer signals were calibrated to the corresponding mean fluid-filled catheter pressures. The PT blood flow profile (i.e., RV outflow) was obtained as the sum of instantaneous ductal and main PA flows, with the latter calculated as the product of measured left PA flow and the total-to-left lung weight ratio.18 Hemodynamic analyses were performed on ensemble-averaged signals typically generated from 40 to 50 individual beats.
Phasic blood flow analysis
Fiducial time points obtained from the PT flow profile were used to define systolic and diastolic flow periods at all sites, with forward systolic flow measured from the start of the PT systolic upstroke to the point where PT flow returned to zero in late systole, and diastolic flow occupying the remainder of the cardiac cycle. Note that (1) PT and PA diastolic flow included the transient nadir occurring at pulmonary valve closure;10,12,17 (2) raw average systolic and diastolic PT, and ductal and PA flows were multiplied by the quotient of systolic or diastolic duration and heart period to yield the reported systolic and diastolic flows, whose sum was equal to mean flow;11,12,17 (3) to permit direct comparison with PT and ductal flows, reported PA flows refer to the calculated combined left and right PA flow values; (4) PVR was computed as (mean PT pressure − mean LA pressure)/(mean PA flow) and normalized to 100 g of wet lung weight.
Characteristic impedance
Using high-fidelity pulmonary pressure and the appropriate flow, PA and ductal Zc were computed as the slope of the pressure-flow relation in early systole, when reflected waves are assumed to be negligible.19
Pulmonary reservoir function
Discharge from the central pulmonary (i.e., PT) reservoir was calculated as the difference between ductal and PA flows in diastole,20 while backflow from the conduit PA reservoir was equated to the absolute value of diastolic PA flow.11,17
Right ventricular pump function
To quantify RV pump function, total RV hydraulic power was calculated as the product of instantaneous PT flow and micromanometer pressure, mean RV power as the product of mean PT flow and pressure, and oscillatory RV power as total minus mean RV power, with RV pump efficiency assessed from the oscillatory-to-total power ratio.12,21,22 To evaluate heart rate-independent changes in RV pump function, RV stroke work was calculated as total RV hydraulic power divided by heart rate.
Statistical analysis
Results were analyzed using SPSS (v24, IBM Corporation, Armonk, NY). After logarithmic transformation of any non-normally distributed data, the control and the betamethasone groups were compared with one-way analysis of variance, while characteristic impedance data within these groups were compared with repeated measures one-way analysis of variance. Data are expressed as mean ± SD and significance was set at P < 0.05.
Results
Weights and blood gases
Body weight (3.36 ± 0.46 vs 3.18 ± 0.35 kg, P = 0.35), total lung weight (108 ± 17 vs 96 ± 15 g, P = 0.15), and the lung-to-body weight ratio (32.1 ± 2.2 vs 30.2 ± 3.3 g kg−1, P = 0.18) were not different between the control and the betamethasone groups. Furthermore, apart from a slightly higher hemoglobin O2 saturation in control lambs (P = 0.01), aortic blood gas variables were similar between groups (Table 1).
Hemodynamic
Betamethasone treatment was accompanied by higher systolic and pulse arterial blood pressures (P ≤ 0.03), mean AoT blood pressure (P = 0.04), and heart rate (P = 0.02), but a lower PT–AoT mean blood pressure difference (P = 0.01) and PVR (P = 0.04, Table 2).
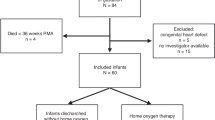
Blood flows
Mean PA flow was ∼130% higher (P = 0.008) and systolic flow ∼100% higher (P = 0.004) in the betamethasone group, but diastolic flow was not different between groups. Similarly, mean and systolic PT flows were ∼20% (P = 0.03) and ∼25% (P = 0.009) higher, but diastolic PT flow was similar between groups, with the proportion of PT blood flow distributed to the lungs rising from 16 ± 9 to 30 ± 15% after betamethasone treatment (P = 0.02). By contrast, mean systolic and diastolic ductal flows were not significantly affected by betamethasone therapy (Fig. 1 and Table 3).
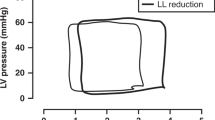
Characteristic impedance
In the control group, Zc of the ductus was double that of the PA (P < 0.01). Compared to controls, Zc in the betamethasone group was ∼70% higher in the ductus (P < 0.05), but was not different in the PA (P = 0.61, Fig. 2).
Pulmonary reservoir function
Discharge from the central pulmonary reservoir was similar in the control and the betamethasone-treated fetuses (36 ± 49 vs. 33 ± 30 ml min−1, P = 0.87), as was backflow from the conduit PA reservoir (45 ± 43 vs. 58 ± 54 ml min−1, P = 0.56).
Right ventricular function
Betamethasone treatment increased RV total, mean, and oscillatory hydraulic power by 43% (P < 0.001), 42% (P = 0.002), and 52% (P < 0.001), respectively, without a change in the RV oscillatory-to-total power ratio (P = 0.38), while RV stroke work was 24% higher (P = 0.03, Table 4).
Discussion
This study, which has examined the basis of alterations in phasic PA blood flow patterns after antenatal steroid therapy with betamethasone in preterm fetal lambs, has produced two main findings. First, betamethasone therapy resulted in an increased PA blood flow that was confined to the systole. Second, although a fall in PVR was a major contributor to this increase in PA blood flow, the latter was also underpinned by two other factors, namely (1) an increased RV hydraulic power, as evidenced by increased RV output and higher pulmonary pressures, and (2) a greater distribution of RV systolic outflow to the lungs, related to an elevation in characteristic impedance (Zc) of the ductus.
Relatively, few animal studies have measured general hemodynamic responses after administration of antenatal betamethasone to preterm fetuses in the recommended clinical practice of a course of two maternal intramuscular injections of the combined acetate and phosphate forms given 24 h apart.2 Within these studies, general hemodynamic responses to betamethasone have been quite variable, ranging from no effect on mean arterial blood pressure or heart rate,3 an increase in mean arterial blood pressure but not heart rate23,24,25 or, as in the present study, increases in both arterial blood pressure and heart rate.26 With respect to heart rate, this mirrors the wide range of patterns reported in clinical studies,27,28,29,30 with factors implicated in this varying response including (1) the degree of fetal maturity, with a change from increased to unaltered heart rate observed with advancing gestation29 and (2) temporal effects, with a fall in heart rate on the first day after the start of antenatal steroid therapy, but an increase in heart rate after the second day.30
The ∼130% increment in mean PA blood flow after betamethasone therapy in preterm fetal lambs of the present study was slightly greater than the ∼80% increase reported by Miller et al,4 but substantially less than the fourfold rise observed by Crossley et al.3 The basis of a higher fetal PA blood flow induced by betamethasone has been considered to be a fall in PVR,3 related to factors such as an augmented vasodilator response to agents such as catecholamines, prostaglandins, and nitric oxide,31,32 and increased pulmonary β-adrenoceptor density.33 However, analysis of phasic flow patterns in the present study suggested that the elevation in fetal PA blood flow after betamethasone therapy was also underpinned by two specific extra-pulmonary changes.
The first was a rise in RV output, a finding consistent with previous speculation in preterm fetal lambs of similar gestation that betamethasone administration increased cardiac output, based on the observation that a large increment in arterial blood pressure was disproportionate to a modest rise in systemic (femoral arterial) vascular resistance.24 Note that, our finding that betamethasone increased between-group RV output measured with transit-time flow probes differs from the decrease in within-group combined ventricular output obtained with colored microspheres in preterm fetal lambs without intrauterine growth retardation.4 A gestational factor may have contributed to this divergence, as control fetal lambs in the aforementioned study were 2–3 weeks younger and about half the body weight of fetuses in the present study.
An increase in fetal RV output after antenatal betamethasone was, in turn, related to an augmentation of RV pump function, as indicated by increases in total and mean RV power (Table 4), and consistent with rises in pulmonary systolic and pulse pressures (Table 2). As in near-term fetal lambs,12 the oscillatory-to-total power ratio, which represents the proportion of “wasted” RV energy used to generate the pulsatile components of pressure and flow,21 was quite low in control preterm fetal lambs (∼12%), compared to the range of 21–28% reported for the adult right ventricle.21,34,35 Taken together, these findings imply that a low oscillatory-to-total power ratio (which reflects a high level of pump efficiency) is a normal feature of fetal RV in the latter part of gestation. Moreover, the unchanged oscillatory-to-total power ratio after betamethasone therapy indicated that the increased RV pumping performance did not come at a cost of lowering pump efficiency.
At least two myocardial effects are likely to have contributed to an increase in fetal RV pump function after antenatal steroid therapy. First, a 2-day course of antenatal betamethasone results in maturation of cardiac growth patterns with increased myocyte binucleation, as well as levels of myocyte proliferation and apoptosis that are similar to those of term hearts.7 Second, antenatal glucocorticoids can enhance myocardial metabolism via effects such as higher levels of adenylate cyclase activity,36 and increased ATP production with augmented creatine kinase expression37 and glycolytic pathway activity.38 It is important to note, however, that higher heart rate also contributed to an augmented RV pump function, with comparison of increases in RV total power (43%) and stroke work (24%; Table 4), suggesting that it accounted for more than half of the rise in RV power after betamethasone therapy.
The second factor underpinning a rise in PA blood flow in betamethasone animals was a greater distribution of the increased RV systolic outflow to the lungs. We have previously shown that relative differences in PA and ductal Zc (governed by the size and stiffness of these vessels) determines the degree to which the initial RV systolic flow impulse is transmitted into the PA vs. the ductus10 with a higher ductal Zc, leading to preferential passage of the initial RV systolic flow impulse into the PA rather than the ductus. More importantly, however, an even higher ductal Zc was seen after betamethasone therapy, without a corresponding increase in PA Zc, so that the entire increase in the RV systolic flow impulse passed into the lungs without an increase in ductal systolic flow.
The effect of betamethasone on ductal Zc can be understood on the basis that (1) prostaglandins, particularly prostaglandin E2, play a key role in maintaining patency of the smooth muscle-rich ductus in the fetus by inhibiting intrinsic contractile tone and (2) glucocorticosteroids suppress prostaglandin synthesis and also reduce the sensitivity of the ductus to prostaglandin E2.9 Although constriction of the ductus after antenatal betamethasone therapy has been reported in an experimental study39 and observed clinically with Doppler ultrasonography, albeit uncommonly,40 it is unlikely that significant ductal constriction occurred in the present study, as the PT–AoT mean blood pressure difference was lower in the betamethasone group (Table 2), whereas this pressure difference is increased by ductal constriction.17 Instead, a more plausible explanation was that the increase in ductal Zc represented a stiffening of the ductus related to a disinhibition of intrinsic contractile tone, with ductal patency maintained due to the rise in pulmonary pressure.9
Contrary to the expectation based on a previous report,3 betamethasone therapy did not result in a less negative fetal PA diastolic flow in our study. Instead, the level of negative fetal PA diastolic flow, which represents retrograde discharge from the conduit PA reservoir,10 was unaffected by antenatal betamethasone, as was the degree of discharge from the central PT reservoir. The lack of a change in fetal PA (and PT) diastolic flow in our study could be explained by a smaller increase in mean PA blood flow (∼130%), compared to the fourfold rise observed after betamethasone therapy in Crossley et al.3
One potential methodological limitation of our study was that calculation of Zc was performed using a single high-fidelity micromanometer catheter located within the PT close to the junction of the ductus and main PA, rather than passage of separate catheters into the ductus and a PA, as is possible in larger near-term fetuses.10,11,12,17 However, analysis of data in a subgroup of eight randomly selected fetal lambs from these prior studies indicated that ductal Zc calculated with PT (y) and ductal (x) pressure signals were related linearly (y = 1.03x + 0.08, R2 = 0.97, P < 0.001). A similar result was obtained for PA Zc, if PT pressure was substituted for the PA pressure profile (y = 1.22x + 0.05, R2 = 0.84, P < 0.001). It is thus unlikely that our conclusions about changes in ductal and PA Zc were affected by the use of a single micromanometer to calculate these variables.
We also cannot exclude the possibility that non-closure of the thoracotomy after completion of instrumentation may have altered fetal hemodynamic variables. However, any effects of an open-chest state were likely to have been quite minor, given that, as mentioned previously,10,11,12,17,18,22 variables such as heart rate, arterial blood pressure, the morphology of ductal and PA flow profiles, as well as mean ductal and PA flows in our preparation are similar to those reported in closed-chest (and chronically instrumented) fetal preparations.
In conclusion, our study results suggest that an increase in pulmonary perfusion evident after antenatal betamethasone treatment is not simply due to reduction in PVR, but occurs in conjunction with rise in RV output and pump function, as well as preferential distribution of increased RV output to the lungs due to an augmentation of ductal characteristic impedance. In concert with our previous studies,10,11,12 these findings emphasize the important contribution of integrated changes within the lung-ductus-RV functional unit to the level of pulmonary blood flow in the fetus.
References
Roberts, D. & Dalziel, S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst. Rev. 3, CD004454 (2006).
Ballard, P. L. & Ballard, R. A. Scientific basis and therapeutic regimens for use of antenatal glucocorticoids. Am. J. Obstet. Gynecol. 173, 254–262 (1995).
Crossley, K. J. et al. Antenatal corticosteroids increase fetal, but not postnatal, pulmonary blood flow in sheep. Pediatr. Res. 66, 283–288 (2009).
Miller, S. L., Supramaniam, V. G., Jenkin, G., Walker, D. W. & Wallace, E. M. Cardiovascular responses to maternal betamethasone administration in the intrauterine growth-restricted ovine fetus. Am. J. Obstet. Gynecol. 201, 613 e611–613 e618 (2009).
Bartha, J. L., Largo-Heinrich, M., Machado, M. J., Gonzalez-Bugatto, F. & Hervias-Vivancos, B. Effects of antenatal betamethasone on human fetal branch pulmonary artery flow velocity waveforms. Fetal Diagn. Ther. 23, 46–53 (2008).
Ustunyurt, O. B. et al. The effect of maternal betamethasone administration on Doppler flow velocity parameters of the fetal branch pulmonary artery. J. Obstet. Gynaecol. 34, 489–491 (2014).
Kim, M. Y. et al. Effects of glucocorticoid exposure on growth and structural maturation of the heart of the preterm piglet. PLoS ONE 9, e93407 (2014).
Padbury, J. F., Ervin, M. G. & Polk, D. H. Extrapulmonary effects of antenatally administered steroids. J. Pediatr. 128, 167–172 (1996).
Clyman, R. I. Mechanisms regulating the ductus arteriosus. Biol. Neonate 89, 330–335 (2006).
Smolich, J. J., Mynard, J. P. & Penny, D. J. Pulmonary trunk, ductus arteriosus and pulmonary arterial phasic blood flow interactions during systole and diastole in the fetus. J. Appl. Physiol. 110, 1362–1373 (2011).
Smolich, J. J., Penny, D. J. & Mynard, J. P. Increased right ventricular output and central pulmonary reservoir function support rise in pulmonary blood flow during adenosine infusion in the ovine fetus. Am. J. Physiol. Regul. Integr. Comp. Physiol. 302, R1450–R1457 (2012).
Smolich, J. J. Enhanced ventricular pump function and decreased reservoir backflow sustain rise in pulmonary blood flow after reduction of lung liquid volume in fetal lambs. Am. J. Physiol. Regul. Integr. Comp. Physiol. 306, R273–R280 (2014).
Fineman, J. R., Soifer, S. J. & Heymann, M. A. Regulation of pulmonary vascular tone in the perinatal period. Annu. Rev. Physiol. 57, 115–134 (1995).
Rudolph, A. M. Fetal and neonatal pulmonary circulation. Annu. Rev. Physiol. 41, 383–395 (1979).
Rudolph, A. M. Distribution and regulation of blood flow in the fetal and neonatal lamb. Circ. Res. 57, 811–821 (1985).
Smolich, J. J. Ultrastructural and functional features of the developing mammalian heart: a brief overview. Reprod. Fertil. Dev. 7, 451–461 (1995).
Smolich, J. J., Penny, D. J. & Mynard, J. P. Enhanced central and conduit pulmonary arterial reservoir function offsets reduced ductal systolic outflow during constriction of the fetal ductus arteriosus. Am. J. Physiol. Regul. Integr. Comp. Physiol. 302, R175–R183 (2012).
Smolich, J. J., Kenna, K. R. & Mynard, J. P. Retrograde lower body arterial reservoir discharge underlies rapid reversal of ductus arteriosus shunting after early cord clamping at birth in preterm lambs. J. Appl. Physiol. 120, 399–407 (2016).
Dujardin, J. P. & Stone, D. N. Characteristic impedance of the proximal aorta determined in the time and frequency domain: a comparison. Med. Biol. Eng. Comput. 19, 565–568 (1981).
Smolich, J. J. & Mynard, J. P. Major contribution of central pulmonary reservoir discharge to increased pulmonary arterial diastolic blood flow after birth in near-term lambs. Am. J. Physiol. Regul. Integr. Comp. Physiol. 311, R702–R709 (2016).
Saouti, N. et al. Right ventricular oscillatory power is a constant fraction of total power irrespective of pulmonary artery pressure. Am. J. Respir. Crit. Care Med. 182, 1315–1320 (2010).
Smolich, J. J., Mynard, J. P. & Penny, D. J. Wave intensity analysis of right ventricular and pulmonary vascular contributions to higher pulmonary than aortic blood pressure in fetal lambs. Am. J. Physiol. Heart Circ. Physiol. 299, H890–H897 (2010).
Miller, S. L. et al. The effects of maternal betamethasone administration on the intrauterine growth-restricted fetus. Endocrinology 148, 1288–1295 (2007).
Derks, J. B. et al. A comparative study of cardiovascular, endocrine and behavioural effects of betamethasone and dexamethasone administration to fetal sheep. J. Physiol. 499(Pt 1), 217–226 (1997).
Segar, J. L., Bedell, K. A. & Smith, O. J. Glucocorticoid modulation of cardiovascular and autonomic function in preterm lambs: role of ANG II. Am. J. Physiol. Regul. Integr. Comp. Physiol. 280, R646–R654 (2001).
Schwab, M., Coksaygan, T. & Nathanielsz, P. W. Betamethasone effects on ovine uterine and umbilical placental perfusion at the dose used to enhance fetal lung maturation. Am. J. Obstet. Gynecol. 194, 572–579 (2006).
Rotmensch, S. et al. The effect of betamethasone and dexamethasone on fetal heart rate patterns and biophysical activities. A prospective randomized trial. Acta Obstet. Gynecol. Scand. 78, 493–500 (1999).
Lunshof, M. S. et al. Short-term (0-48 h) effects of maternal betamethasone administration on fetal heart rate and its variability. Pediatr. Res. 57, 545–549 (2005).
Mulder, E. J., Koenen, S. V., Blom, I. & Visser, G. H. The effects of antenatal betamethasone administration on fetal heart rate and behaviour depend on gestational age. Early Hum. Dev. 76, 65–77 (2004).
Subtil, D. et al. Immediate and delayed effects of antenatal corticosteroids on fetal heart rate: a randomized trial that compares betamethasone acetate and phosphate, betamethasone phosphate, and dexamethasone. Am. J. Obstet. Gynecol. 188, 524–531 (2003).
Gao, Y., Tolsa, J. F., Shen, H. & Raj, J. U. A single dose of antenatal betamethasone enhances isoprenaline and prostaglandin E2-induced relaxation of preterm ovine pulmonary arteries. Biol. Neonate 73, 182–189 (1998).
Zhou, H., Gao, Y. & Raj, J. U. Antenatal betamethasone therapy augments nitric oxide-mediated relaxation of preterm ovine pulmonary veins. J. Appl. Physiol. 80, 390–396 (1996).
Cheng, J. B., Goldfien, A., Ballard, P. L. & Roberts, J. M. Glucocorticoids increase pulmonary beta-adrenergic receptors in fetal rabbit. Endocrinology 107, 1646–1648 (1980).
Milnor, W. R., Conti, C. R., Lewis, K. B. & O’Rourke, M. F. Pulmonary arterial pulse wave velocity and impedance in man. Circ. Res. 25, 637–649 (1969).
Laskey, W. K., Ferrari, V. A., Palevsky, H. I. & Kussmaul, W. G. Ejection characteristics in primary pulmonary hypertension. Am. J. Cardiol. 71, 1111–1114 (1993).
Stein, H. M. et al. Effects of corticosteroids in preterm sheep on adaptation and sympathoadrenal mechanisms at birth. Am. J. Physiol. Endocrinol. Metab. 264, E763–E769 (1993).
Mizuno, M. et al. Antenatal glucocorticoid therapy accelerates ATP production with creatine kinase increase in the growth-enhanced fetal rat heart. Circ. J. 74, 171–180 (2010).
Tsuzuki, Y. et al. Antenatal glucocorticoid therapy increase cardiac alpha-enolase levels in fetus and neonate rats. Life Sci. 85, 609–616 (2009).
Momma, K., Nishihara, S. & Ota, Y. Constriction of the fetal ductus arteriosus by glucocorticoid hormones. Pediatr. Res. 15, 19–21 (1981).
Wasserstrum, N. et al. Betamethasone and the human fetal ductus arteriosus. Obstet. Gynecol. 74, 897–900 (1989).
Acknowledgements
We thank Magdy Sourial, Rebecca Sutton, Sara White, Amy Tilley, and Aaron Mocciaro for their assistance with experimental studies, and Dr. Kelly Kenna for assistance with experimental studies and manuscript preparation. This work was supported by Grant-in-Aid GM12M6372 from the National Heart Foundation of Australia, Project Grant 1105137 from the National Health and Medical Research Council of Australia, and the Victorian Government’s Operational Infrastructure Support Program. J.P.M. is supported by a Career Development Fellowship co-funded by the National Health and Medical Research Council of Australia (GNT1143510) and National Heart Foundation (101866).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smolich, J.J., Mynard, J.P. Increased right ventricular power and ductal characteristic impedance underpin higher pulmonary arterial blood flow after betamethasone therapy in fetal lambs. Pediatr Res 84, 558–563 (2018). https://doi.org/10.1038/s41390-018-0098-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0098-5
This article is cited by
-
Reducing lung liquid volume in fetal lambs decreases ventricular constraint
Pediatric Research (2021)