Abstract
Objectives
Iron deficiency anemia in childhood is a serious public health problem worldwide. Reticulocyte hemoglobin content (Ret-He) is a novel biomarker of iron deficiency adopted for adults but there is a lack of reference intervals for Ret-He in infants. The aim of this study was to provide data from healthy infants.
Methods
Swedish infants (n = 456), born at term after normal pregnancies were included. Ret-He was measured at birth (umbilical cord sample), 48–72 h, 4 months, and 12 months. Reference intervals were calculated as ±2 standard deviations from the mean of Ret-He.
Results
Reference intervals for newborn Ret-He were 27.4 to 36.0 pg/L (N = 376) in the cord sample, 28.1–37.7 pg/L (N = 253) at 48–72 h, 25.6–33.4 pg/L (N = 341) at four months and 24.9–34.1 pg/L (N = 288) at 12 months. Ret-He was significantly lower among iron-deficient infants, at 4 months mean difference (95% CI) −4.2 pg/L (−6.1 to −2.4) and at 12 months mean difference (95% CI) −3.4 pg/L (−5.0 to −1.8).
Conclusions
This longitudinal study presents Ret-He reference intervals based on non-anemic and non-iron-deficient infants and constitutes a step towards standardizing Ret-He as a pre-anemia biomarker of iron deficiency in children.
Similar content being viewed by others
Introduction
Iron deficiency (ID) is the most common nutritional deficiency worldwide.1,2 Insufficient dietary iron, variable absorption, and rapid growth put infants at particular risk for ID. Iron plays an important role in the development of the central nervous system and is essential to neural myelination and neurotransmitter function.3,4,5 Iron deficiency anemia (IDA) during infancy is therefore associated with poor neurodevelopment. Although ID can be reversed with iron supplementation, the alteration in cognitive and behavioral performance observed in children with ID may not be fully correctable.6,7,8
Relying solely on hemoglobin (Hb) for evaluation of iron status is not recommended since it is a poor marker of mild or moderate ID and may thus delay the detection of ID in infants. An optimal biomarker of ID has proven difficult to establish.9
In clinical practice, biochemical tests are most commonly used to diagnose ID, such as serum ferritin and transferrin saturation (TS).10 However, these tests are subjected to biological variability, such as diurnal variation and fluctuation with dietary iron intake. Ferritin, which is the most commonly used biomarker, is an acute phase reactant produced in the liver, and is also altered in inflammatory states.11
In this setting, reticulocyte hemoglobin content (Ret-He) has emerged as a relatively new iron status marker. In some previous studies, it has even shown promising qualities as a biomarker of early ID.11,12 Two methods for analysis of Ret-He are available; the CHr (mean cellular Hb content of reticulocytes) parameter provided by the ADVIA 120 and 2120 (Bayer Diagnostics, Tarrytown, NY) and the Ret-He (reticulocyte Hb equivalent) available on analyzers from the Sysmex Corporation, Kobe, Japan (XE 2100, XE 5000 and the XN series), respectively, and show very good level agreement.13 Ret-He, together with mean corpuscular volume (MCV), Hb, and reticulocyte count are hematological tests that can be used to diagnose ID. The lifespan of erythrocytes among children after the neonatal period is 60–90 days;14 therefore, it takes some time to see changes in red blood cell parameters appropriate for ID. Reticulocytes exist in the circulation for only 1–2 days and may provide a more real-time view of the availability of iron in the bone marrow.15
The potential clinical utility of Ret-He for diagnosis of ID in infancy has so far been limited by the lack of reference intervals,9,16 but has been proposed to be superior to ferritin and TS in the evaluation of iron status in anemic children in chronic dialysis.17 Reference intervals have been reported for newborns within 24 h, in a population of children between 6 months and 5 years, with a median of 4 years, and for infants during their fist 90 days.18,19,20,21 A recent study compared Ret-He and soluble transferrin receptors (sTfR) for the diagnosis of iron depletion in young children aged 0.5–3 years, comparing these biomarkers with ferritin levels.22 The study showed that Ret-He was decreased at low levels of ferritin, and also that Ret-He level was significantly correlated with ferritin, MCV, and Hb. Another study concluded that CHr/Ret-He seems to be a suitable marker for latent ID in preterms at 3–4 months corrected age.23
However, earlier studies have been based on patients, that is children visiting hospitals due to a health-related reason, which may introduce bias, and since there is still a lack of age specific reference intervals for Ret-He, we decided to utilize data from a large sample of healthy infants to create reference intervals for Ret-He from birth to one year of age.
Methods
Study population
This study was performed at the Hospital of Halland, Halmstad, based on two earlier studies on hematological and iron status in relation to cord clamping during infancy. Between 16 April 2008 and 22 May 2009; 378 children were included in a randomized controlled trial investigating the effect of early versus late umbilical cord clamping at birth.24 Additional blood samples were collected between 7 June 2010 and 29 February 2012, when 78 children were included as part of a study assessing timing of umbilical cord clamping in relation to planned cesarean section.25 Thus, this study population comprises of two separate sample populations, the first with vaginal births and the second with caesarean section. All children were born at term, with normal birth weights. Their mothers were healthy, non-smokers with uneventful pregnancies.24 In the present study, blood samples from both study populations were used. The timing of blood sampling was as follows: birth (umbilical cord blood), 48–72 h (in conjunction with metabolic screening), 4 months, and 12 months. In addition to Ret-He, the blood samples were analyzed for C-reactive protein (CRP), Hb, MCV, transferrin, serum iron, ferritin, sTfR, and TS.
To define the age-related reference populations we excluded infants with anemia, ID, or inflammation. The following exclusion criteria were used: CRP level above 10 mg/L, ID, or anemia; see Table 1. ID was defined as at least two (out of four) iron store indicators, including MCV, TS, sTfR, and ferritin, outside reference interval.26
Statistical analyzes
Statistical analyzes were conducted using IBM SPSS Statistics 22.0 (SPPS, Chicago, IL). Several statistical methods are available to estimate reference intervals. The parametric approach is one of the most commonly used, where data is assumed to follow a Gaussian distribution, based on the distribution curves and the size of the population. In the present study, the reference interval is presented as the arithmetic mean ± 2 standard deviations (SD). In a single interval study, the recruitment of at least 120 healthy reference individuals is proposed to be required in order to achieve an acceptably high enough statistical confidence.27
Associations between Ret-He and more established biomarkers for ID, i.e ferritin, MCV, sTfR, and Hb were analyzed by calculation of the Pearson’s correlation coefficient. Independent samples T-test was used for the comparison between groups with continuous data, while groups with skewed distribution were analysed with Mann–Whitney U test. To assess differences between Ret-He at different time points paired samples T-test was used. Statistical significance was defined as a P-value <0.05.
Technical methods
Blood was collected in EDTA tubes (BD Vacutainer®, Plymouth, UK) for complete blood count, and in serum separator tubes (BD Vacutainer®) for iron status, bilirubin, and CRP. Blood samples were stored for a maximum of one hour in room temperature and then transported for analysis to the hospital Clinical Chemistry Laboratory where analyses were performed. Ret-He, as well as Hb and MCV, were analyzed using the automated haematology analyser Sysmex XE 2100 (Sysmex, Kobe, Japan). Iron status indicators and CRP were analysed using Cobas 6000 (Roche Diagnostics, Basel, Switzerland).
Ethical approval
The study was approved by the regional research ethics committee at Lund University (41/2008, 344/2009). Written informed consent was obtained from the parents by a midwife before the inclusion.
Results
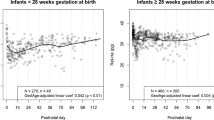
This study included a total of 456 full-term infants. Participants were included at Hospital of Halland, Halmstad between April 2009 and February 2012. The baseline and background characteristics of all the infants included in the study are presented in Table 2. Figure 1 shows the flow of study infants and the number of samples excluded.
After statistical analyzes, we found that Ret-He was approximately normally distributed (Fig. 2). We therefore decided to define reference intervals as the arithmetic mean ±2 SD. In order to establish reference intervals for healthy infants, infants with anemia, ID, inflammation or any combination of these conditions were excluded. These exclusions are detailed in Fig. 1. The number of subjects with a missing value of Ret-He at each time point is also shown in Fig. 1.
Reference intervals, the arithmetic mean ±2 SD for Ret-He are shown in Table 3. The arithmetic mean of Ret-He was 31.7 pg/L in cord blood and 32.9 pg/L at 48–72 h, while at 4 to 12 months Ret-He was 29.5 pg/L. Ret-He increased significantly between birth and at 48–72 h, average mean difference (AMD) (95 % confidence interval) 1.2 pg/L (0.9–1.6), n = 212 and decreased between 48–72 h and 4 months, AMD (95 % confidence interval) −3.6 pg/L (−4.0 to −3.2), n = 187.
Ret-He level was similar between boys and girls at birth, 48–72 h and 12 months, but was significantly lower among boys at 4 months of age, AMD (95% confidence interval) −0.8 pg/L (−1.2 to −0.4). As earlier reported, Ret-He differed between delayed and early clamped infants at 4 months; 29.6 (1.9) vs. 28.9 (2.1) pg/L, p = 0.005 but not at 2 days; 32.7 (2.6) vs 32.5 (2.4) pg/L or at 12 months of age; 29.2 (2.2) vs 29.0 (2.2) pg/L.24,28
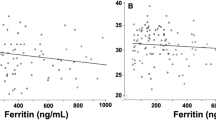
A negative correlation with sTfR was found at all time-points, whereas a Ret-He was positively correlated with ferritin at birth and at 4 months. Ret-He showed a significant correlation with Hb at 12 months. There was also a strong negative correlation with CRP at 4 and 12 months of age (Table 4)
.
Discussion
Our data provide reference data of Ret-He from birth to 12 months in a large population of healthy infants. We demonstrate that Ret-He is approximately normally distributed, as shown also in other studies,29 and therefore eligible for analyzes by parametric methods. For the calculation of reference intervals we have selected a reference subset of infants excluding conditions that may affect reticulocytes, such as anemia, ID, and inflammation.
To establish reference intervals, it is proposed to measure blood samples from subjects who are healthy.27,30,31 In children, it is often challenging, because reference intervals should reflect different phases of physiological development from birth and upwards. Therefore, defining the exclusion criteria is crucial and the excluded subjects will depend, of course, on the particular analyte evaluated. For example, to determine a reference interval for Hb or related hematological analytes, it would be wise to exclude subjects with ID or inflammation.32 The obtained values will assume a certain distribution (reference distribution) and, by analyzing it with appropriate statistical methods, reference intervals can be calculated. Our observed lower reference levels (−2 SD) at 4 and 12 months of 25.6 and 24.9 pg/L, respectively, corresponds well to the cut off level of 25 pg/L commonly used to diagnose ID in older children.33
Ret-He or its equivalent CHr has shown promise in the identification of children with ID solely on the basis of hematological parameters,11 as well as a potential predictive tool as an early indicator of ID in infants,12,13 even though its use as a single biomarker has been challenged.9 In our correlation analysis, Ret-He was strongly correlated to sTfR at all ages, while there were varying correlations to MCV, Ferritin, and TS, as well as Hb. This might reflect that these indicators describe different stages of iron metabolism. Ret-He has been suggested as superior to Ferritin for not being affected by inflammation, which has been questioned.34 Our study suggest a correlation between CRP and Ret-He at 4 and 12 months, when inflammation most likely has been in place for a longer time reducing circulating iron in the blood.
In comparison to other proposed reference intervals for Ret-He and/or CHr, it is possible to compare our results at birth and at 48–72 h with the study by Christensen et al. who analysed Ret-He from 6632 blood samples among infants in the first 90 days of life.20 A majority of the blood samples were taken during the first three days of life (N = 4950, 75%) and the first week (N = 5676, 86%). The study also included ~30% preterm (less than 37 weeks gestational age) infants. The mean Ret-He at birth was 35.9 pg/L (3.1), which is higher than in the present study, 31.7 pg/L (2.2). The Ret-He decreased to 30.1 pg/L (3.6) at day four in the study by Christensen et al., in comparison to the present study in which Ret-He rose to 32.9 pg/L (2.4) at 48–72 h in our study. The study by Christensen et al. study had a larger sample size but is limited by being based on convenience samples from clinically ordered complete blood counts, thereby most likely containing a larger sample of infants in need of hospital care, while the children in our study were healthy. Lorenz et al. reported Ret-He levels within 24 h after birth in 512 newborn including a subgroup of 216 term infants.18 Ret-He was 32.0 (3.2) pg/L in the term group, relatively similar to our results 31.7 (2.2) pg/L in umbilical blood. In parallel to the Christensen study, but in contrast to our findings, Lorenz found a decrease in Ret-He from samples taken within the first days of life compared.35 One explanation might be that Ret-He was measured from umbilical cord samples in our study, while from blood samples taken after birth in the Christensen and Lorenz studies.
Another study, by Teixeira et al., presented reference intervals for CHr, based on 100 children aged 6 months to 5 years, as 27.5–33.4 pg/L, which is higher than our proposed interval at 12 months; 24.9–34.0, based on 285 children. The median age in the study by Teixeira et al. was 4 years, which might explain this discrepancy.19
In our study, we found a significant lower Ret-He among boys compared to girls at 4 months of age. The background for this difference is not known but most likely reflects the earlier reported difference in iron status between sexes at this time point of life.24,36 Kuehn et al. have reported a lower Ret-He among blacks compared to other races among toddlers aged 12–36 months.37 We did not document race in the present study.
A limitation of this study is the varying number of infants remaining at the different time-points of blood sampling, shown in Fig. 1. This is due to loss-to-follow-up at 4 and 12 months, respectively, but also due to technical shortcomings, such as missed blood sampling at birth, and insufficient blood-sample volume at the laboratory.
By including healthy infant and not patients, this study´s results may adhere more to a “true” normal distribution of Ret-He values, further enhanced by excluding infants that were accidentally found to have ID, anemia, and/or inflammation. As Ret-He was higher in the non-ID group as compared to the excluded ID group, the suggested Ret-He intervals will allow clinicians to identify more infants with suboptimal iron stores. In the analysis of the distribution curves, there is a slight skewness to the left in the direction of the lower values of Ret-He. This may represent a subgroup of infants at risk for development of ID, which has not been identified with more established iron markers, such as ferritin.
In conclusion, this study is one the largest studies investigating reference intervals for Ret-He. The results will facilitate the use of Ret-He as a screening tool for ID in infants.
References
Domellöf, M. et al. Iron requirements of infants and toddlers. J. Pediatr. Gastroenterol. Nutr. 58, 119–129 (2014).
Global Burden of Disease C. Child and adolescent health from 1990 to 2015: findings from the global burden of diseases, injuries, and risk factors 2015 study. JAMA Pediatr. 171, 573–592 (2017).
Andersson, O. et al. Effect of delayed cord clamping on neurodevelopment at 4 years of age: a randomized clinical trial. JAMA Pediatr. 169, 631–638 (2015).
Beard, J. L. Why iron deficiency is important in infant development. J. Nutr. 138, 2534–2536 (2008).
Berglund, S. K., Westrup, B., Haraldsson, E., Engstrom, B. & Domellof, M. Effects of iron supplementation on auditory brainstem response in marginally LBW infants. Pediatr. Res. 70, 601–606 (2011).
Berglund, S. K., Westrup, B., Hägglöf, B., Hernell, O. & Domellöf, M. Effects of iron supplementation of LBW infants on cognition and behavior at 3 years. Pediatrics 131, 47–55 (2013).
Szajewska, H., Ruszczynski, M. & Chmielewska, A. Effects of iron supplementation in nonanemic pregnant women, infants, and young children on the mental performance and psychomotor development of children: a systematic review of randomized controlled trials. Am. J. Clin. Nutr. 91, 1684–1690 (2010).
Lozoff, B. & Georgieff, M. K. Iron deficiency and brain development. Semin. Pediatr. Neurol. 13, 158–165 (2006).
Baker, R. D. & Greer, F. R. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age). Pediatrics 126, 1040–1050 (2010).
Dallman, P. R., Reeves, J. D., Driggers, D. A. & Lo, E. Y. Diagnosis of iron deficiency: the limitations of laboratory tests in predicting response to iron treatment in 1-year-old infants. J. Pediatr. 99, 376–381 (1981).
Ullrich, C. et al. Screening healthy infants for iron deficiency using reticulocyte hemoglobin content. JAMA 294, 924–930 (2005).
Kiudeliene, R., Griniute, R. & Labanauskas, L. Prognostic value of reticulocyte hemoglobin content to diagnose iron deficiency in 6-24-month-old children. Med. (Kaunas.) 44, 673–677 (2008).
Brugnara, C., Schiller, B. & Moran, J. Reticulocyte hemoglobin equivalent (Ret He) and assessment of iron-deficient states. Clin. Lab. Haematol. 28, 303–308 (2006).
An, G., Widness, J. A., Mock, D. M. & Veng-Pedersen, P. A novel physiology-based mathematical model to estimate red blood cell lifespan in different human age groups. AAPS J. 18, 1182–1191 (2016).
Mast, A. E., Blinder, M. A. & Dietzen, D. J. Reticulocyte hemoglobin content. Am. J. Hematol. 83, 307–310 (2008).
Domellof, M. Iron requirements, absorption and metabolism in infancy and childhood. Curr. Opin. Clin. Nutr. Metab. Care. 10, 329–335 (2007).
Davidkova, S. et al. Comparison of reticulocyte hemoglobin equivalent with traditional markers of iron and erythropoiesis in pediatric dialysis. Pediatr. Nephrol. 31, 819–826 (2016).
Lorenz, L. et al. Reference ranges of reticulocyte haemoglobin content in preterm and term infants: a retrospective analysis. Neonatology 111, 189–194 (2017).
Teixeira, C., Barbot, J. & Freitas, M. I. Reference values for reticulocyte parameters and hypochromic RBC in healthy children. Int. J. Lab. Hematol. 37, 626–630 (2015).
Christensen, R. D., Henry, E., Bennett, S. T. & Yaish, H. M. Reference intervals for reticulocyte parameters of infants during their first 90 days after birth. J. Perinatol. 36, 61–66 (2016).
Al-Ghananim, R. T. et al. Reticulocyte hemoglobin content during the first month of life in critically ill very low birth weight neonates differs from term infants, children, and adults. J. Clin. Lab. Anal. 30, 326–334 (2016).
Uijterschout, L. et al. The value of Ret-Hb and sTfR in the diagnosis of iron depletion in healthy, young children. Eur. J. Clin. Nutr. 68, 882–886 (2014).
Lorenz, L. et al. Reticulocyte haemoglobin content as a marker of iron deficiency. Arch. Dis. Child. Fetal Neonatal Ed. 100, F198–F202 (2015).
Andersson, O., Hellström-Westas, L., Andersson, D. & Domellöf, M. Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 months: a randomised controlled trial. BMJ 343, bmj.d7157 (2011).
Andersson, O., Hellstrom-Westas, L. & Domellof, M. Elective caesarean: does delay in cord clamping for 30 s ensure sufficient iron stores at 4 months of age? A historical cohort control study. BMJ Open 6, e012995 (2016).
Domellöf, M., Dewey, K. G., Lönnerdal, B., Cohen, R. J. & Hernell, O. The diagnostic criteria for iron deficiency in infants should be re-evaluated. J. Nutr. 132, 3680–3686 (2002).
Jung, B. & Adeli, K. Clinical laboratory reference intervals in pediatrics: the CALIPER initiative. Clin. Biochem. 42, 1589–1595 (2009).
Andersson, O., Domellöf, M., Andersson, D. & Hellström-Westas, L. Effect of delayed vs early umbilical cord clamping on iron status and neurodevelopment at age 12 months: a randomized clinical trial. JAMA Pediatr. 168, 547–554 (2014).
Canals, C. et al. Clinical utility of the new Sysmex XE 2100 parameter—reticulocyte hemoglobin equivalent—in the diagnosis of anemia. Haematologica 90, 1133, 1134 (2005).
Ridefelt, P., Hellberg, D., Aldrimer, M. & Gustafsson, J. Estimating reliable paediatric reference intervals in clinical chemistry and haematology. Acta Paediatr. 103, 10–15 (2014).
Daly, C. H., Liu, X., Grey, V. L. & Hamid, J. S. A systematic review of statistical methods used in constructing pediatric reference intervals. Clin. Biochem. 46, 1220–1227 (2013).
Ceriotti, F., Hinzmann, R. & Panteghini, M. Reference intervals: the way forward. Ann. Clin. Biochem. 46, 8–17 (2009).
Mateos, M. E., De-la-Cruz, J., Lopez-Laso, E., Valdes, M. D. & Nogales, A. Reticulocyte hemoglobin content for the diagnosis of iron deficiency. J. Pediatr. Hematol. Oncol. 30, 539–542 (2008).
Syed, S. et al. Use of reticulocyte hemoglobin content in the assessment of iron deficiency in children with inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 64, 713–720 (2017).
Lorenz, L. et al. Reticulocyte haemoglobin content declines more markedly in preterm than in term infants in the first days after birth. Neonatology 112, 246–250 (2017).
Domellöf, M. et al. Sex differences in iron status during infancy. Pediatrics 110, 545–552 (2002).
Kuehn, D. et al. Reticulocyte hemoglobin content testing for iron deficiency in healthy toddlers. Mil. Med. 177, 91–95 (2012).
Acknowledgements
Funding
This study was supported by grants from the Regional Scientific Council of Halland, the Linnéa and Josef Carlsson Foundation, the Southern Healthcare Region’s common funds for development and research, H. R. H. Crown Princess Lovisa’s Society for Child Care, Uppsala University, the Little Childs foundation, Sweden, and the Swedish Research Council for Health, Working Life and Welfare.
Author information
Authors and Affiliations
Contributions
O.A. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: A.L., M.D., L.H.-W., and O.A. Acquisition of data: A.L. and O.A. Analysis and interpretation of data: A.L., M.D., L.H.-W., and O.A. Drafting of the manuscript: A.L. and O.A. Critical revision of the manuscript for important intellectual content: A.L., M.D., L.H.-W. and O.A. Statistical analysis: A.L. and O.A. Obtained funding: O.A., M.D. and L.H.-W.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Löfving, A., Domellöf, M., Hellström-Westas, L. et al. Reference intervals for reticulocyte hemoglobin content in healthy infants. Pediatr Res 84, 657–661 (2018). https://doi.org/10.1038/s41390-018-0046-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0046-4
This article is cited by
-
Serum ferritin values in neonates <29 weeks’ gestation are highly variable and do not correlate with reticulocyte hemoglobin content
Journal of Perinatology (2023)
-
Reconciling markedly discordant values of serum ferritin versus reticulocyte hemoglobin content
Journal of Perinatology (2021)
-
Urinary ferritin; a potential noninvasive way to screen NICU patients for iron deficiency
Journal of Perinatology (2021)