Abstract
Background
Maternal thyroid deficiency can increase Rho-kinase procontractile influence in arteries of 2-week-old progeny. Here we hypothesized that augmented role of Rho-kinase persists in arteries from adult progeny of hypothyroid rats.
Methods
Dams were treated with 6-propyl-2-thiouracil (PTU) in drinking water (0.0007%) during pregnancy and 2 weeks postpartum; control (CON) females received PTU-free water. At the age of 10–12-weeks, serum T3/T4 levels did not differ between PTU and CON male offspring. Cutaneous (saphenous), mesenteric, and skeletal muscle (sural) arteries were studied by wire myography, qPCR, and Western blotting.
Results
Saphenous arteries of PTU and CON groups showed similar responses to α1-adrenoceptor agonist methoxamine and were equally suppressed by Rho-kinase inhibitor Y27632. Responses of mesenteric arteries also did not differ between PTU and CON, but the effects of Y27632 were more prominent in the PTU group. Sural arteries of PTU rats compared to CON demonstrated augmented responses to methoxamine, increased RhoA mRNA contents and higher levels of MYPT1 phosphorylation at Thr855. Intergroup differences in contractile responses and phospho-MYPT1-Thr855 were eliminated by Y27632.
Conclusion
Rho-kinase contribution to contractile responses of mesenteric and especially sural arteries is augmented in adult PTU rats. Therefore, maternal thyroid deficiency may have long-term detrimental consequences for vasculature in adult offspring.
Similar content being viewed by others
Introduction
Thyroid hormones are essential for normal functioning and development of cardiovascular system.1,2 Unfortunately, thyroid dysfunction is a common endocrine disorder during pregnancy.3,4 According to the current concept, adverse alterations of maternal thyroid status lead to abnormalities in the heart and vasculature of adult progeny, indicating intrauterine programming of cardiovascular function by thyroid hormones.5 Recently it was shown that subclinical hypothyroidism during pregnancy is associated with higher blood pressure in adult offspring.6 Similar observation was made in an animal study of maternal hypothyroidism.7 On the other hand, high blood pressure does not always develop in adult progeny of hypothyroid rats.8,9 The diversity of results suggests that there are adverse circulatory alterations only in certain organs, which might be more susceptible to the developmental thyroid deficiency than others. For example, antenatal/early postnatal hypothyroidism causes increased contractility of coronary vasculature in adult rats, despite the absence of evident alterations in their thyroid function and blood pressure level.9 Further, antenatal/early postnatal hypothyroidism did not affect the responses of saphenous (cutaneous) artery but suppressed the activity of NO-pathway and increased procontractile effects of Rho-kinase in small mesenteric arteries of 2-week-old rat pups.10
Importantly, our study10 was the first to demonstrate the functional link between thyroid hormones and Rho-kinase pathway, a key regulator of smooth muscle contraction in vascular system. Rho-kinase substantially increases the sensitivity of contractile apparatus to Ca2+ downstream to activation of membrane receptors,11 e.g., α1-adrenоceptors.12 Being activated by upstream RhoA protein, Rho-kinase augments contractile responses of vascular smooth muscle through phosphorylation of a number of targets.11,13 One of the well-established Rho-kinase targets in smooth muscle is myosin light chain phosphatase regulatory subunit MYPT1 that can be phosphorylated by Rho-kinase at two sites—Thr696 and Thr855—11 the latter is considered to be the established smooth muscle marker of Rho-kinase activity.14 Rho-kinase-dependent phosphorylation decreases the myosin light chain phosphatase activity and thereby increases smooth muscle contraction. Of note, along with its physiological role in vascular functioning, Rho-kinase was shown to be involved in the pathogenesis of a wide range of cardiovascular diseases such as arterial hypertension, coronary vasospasm, aortic aneurism etc.15,16 However, the role of Rho-kinase pathway in arteries of adult rats suffered from antenatal/early postnatal hypothyroidism has not been explored yet.
Therefore, we hypothesized that the contribution of Rho-kinase to α1-adrenergic arterial contractile responses is altered in adult rats, which suffered from antenatal/early postnatal hypothyroidism. To test this hypothesis, we have compared the effects of Rho-kinase inhibitor in arteries from three different vascular regions of control and previously hypothyroid adult rats. We chose to follow up on saphenous and mesenteric arteries in adult rats, as these arteries have been already studied in 2-week-old pups.10 Additionally, we studied sural (gastrocnemius muscle) artery, since skeletal muscles and their blood supply demonstrate clear insufficiencies in hypothyroid animals17, but possible role of Rho-kinase in such alterations was not addressed in previous studies.
Methods
Animals
All experimental procedures used in this work were approved by the Biomedical Ethics Committee of the Russian Federation State Research Center - Institute for Biomedical Problems, Russian Academy of Sciences (protocol № 426), and conformed to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (Eight edition, 2011).
Adult female (230–280 g) and male (300–350 g) Wistar rats were obtained from the vivarium of the Institute of General Pathology and Pathophysiology (Moscow, Russia) and then bred in the laboratory animal unit of the Biological Faculty, Moscow State University. The animals were maintained on 12/12-h light/dark cycle and fed with normal rodent chow ad libitum.
The model of antenatal/early postnatal hypothyroidism
Detailed description of our maternal hypothyroidism model was provided recently.10 Briefly, pregnant dams were randomly divided into two groups. One group (n = 5) was treated with 6-propyl-2-thiouracil in the drinking water (PTU, 7 ppm or 0.0007%, w/v, Sigma) from the first gestational day until 14th day after delivery. Control group (n = 4) received water without PTU. One or two 2-week-old pups were taken from each litter to evaluate the effects of PTU treatment at this age (n = 6;6). The remaining offspring was grown up till the mature age of 10–12 weeks and one or two male sibs from each litter were used in further wire myography experiments. The rats were killed by decapitation under CO2 anesthesia and trunk blood was collected. The saphenous, sural (external and internal) and small mesenteric arteries (2–3-order branches of the superior mesenteric artery) were isolated from the animals and used for wire myography and qPCR experiments. Additionally, adult males (n = 7; 7) from the same litters were used to obtain the material for protein phosphorylation measurements in sural arteries.
Blood samples analysis
After blood clotting (30 min at room temperature followed by 30 min at 4 °C) the serum was separated by centrifugation for 15 min at 4300 g and kept at −20 °C till further analysis. Total T4, total T3, free T3, and free T4 levels were measured by ELISA using commercially available kits from Immunotek (Moscow, Russia). Total cholesterol serum concentration was determined using automatic biochemistry analyzer (A-25 Biosystems, Spain).
Experiments on isolated arteries
Two neighboring segments with length of 2 mm were cut from each type of artery and mounted in wire myograph system (DMT, Denmark, models 410A or 620) for isometric force recoding. The preparations were kept at 37 °C in physiological salt solution containing (in mM): 120 NaCl, 26 NaHCO3, 4.5 KCl, 1.2 NaH2PO4, 1.0 MgSO4, 1.6 CaCl2, 5.5 D-glucose, 0.025 EDTA, 5 HEPES, equilibrated with gas mixture 5% CO2 + 95% O2 to maintain pH 7.4. Transducer readings were continuously recorded at 10 Hz sampling rate using E14–140 analog-to-digital data converter (L-Card, Russia) and PowerGraph 3.3 software (DISoft, Russia). The segments were gradually stretched to 0.9 d100, where d100 is the inner diameter of fully relaxed vessel exposed to the transmural pressure of 100 mmHg.18 The arteries were activated with norepinephrine (10 µM) and then with methoxamine (MX, selective agonist of α1-adrenoceptors, 10 µM). Functional integrity of endothelium was checked by application of acetylcholine (10 µM) on top of MX-induced contraction (3 µM).
The experimental protocol used in this study consisted of two cumulative concentration-response relationships to MX (0.01 μМ–100 µM) that were performed consecutively in both segments of the same artery. First concentration-response relationships to MX were performed in order to ensure similar initial responses of two studied arterial segments. The second concentration–response relationships to MX were obtained after 20-min incubation of one preparation with Rho-kinase inhibitor Y27632 (3 µM, Calbiochem) and another one with equivalent volume of vehicle (H2O, 15 µl). The contribution of Rho-kinase was estimated by comparison of the second concentration–response relationships in preparations treated with Y27632 and vehicle.
The wire myograph experiments were analyzed as described earlier.19 All active force values were calculated by subtracting the passive force value (recorded in the preparation with fully relaxed smooth muscle) from all recorded values (before the first and at each MX concentration). Then all active force values were expressed as a percentage of the maximum active force value recorded in the first concentration–response relationship. Concentration–response relationships were fitted to a sigmoidal function with variable slope using GraphPad Prism 6.0 Software (La Jolla, CA) to calculate pD2 values (the negative logarithm of EC50). In addition, we estimated the effects of Rho-kinase inhibitor on the active force at highest MX concentration (100 µM, Fmax), for this purpose the Fmax for Y27632-treated preparations was calculated as percentage of mean Fmax in the vehicle-treated group.
Measurement of mRNA level by qPCR
mRNA content of RhoA in sural arteries was measured by qPCR as previously described.19 In brief, immediately after isolation, the arteries were fixed in RNA-later (Qiagen) and kept at −80 °C. RNA was extracted using RNeasy Mini Kit (Qiagen) and treated with DNase I (Fermentas, 1000 U/ml). cDNA was synthesized using MMLV RT reverse transcription kit (Evrogen, Russia). qPCR was run in Rotor Gene 6000 (Corbett Research, Australia) using qPCRmix-HS SYBR Master Mix (Evrogen, Moscow, Russia). Rn18s, Rplp0, and Gapdh were used as house-keeping genes. The primers were obtained from Evrogen (Moscow, Russia), their sequences are presented in Table 1. Amplification protocol included 10-min heating at 95 °C, followed by 40 cycles, consisting of three phases: 30 s at 95 °C, 30 s at 60 °C, and 60 s at 72 °C and final incubation at 72 °С for 10 min.
qPCR experiments were analyzed in Rotor Gene 6000 Software. Gene expression levels were calculated as 1/Е^CT, where Е—primer efficiency, CT—cycle number on which the curve for product accumulation is crossing the fluorescence detection threshold. The values for RhoA were normalized to the geometric mean of the three house-keeping genes in the same sample.
Western blotting
To determine protein phosphorylation, the isometrically held and stretched to 0.9 d100 arterial segments were subjected to similar protocols as in contraction experiments. Briefly, the preparations were activated with norepinephrine and MX followed by incubation with vehicle (H2O) or Y27632 (3 µM) for 20 min. Protein phosphorylation was preserved by instantly freezing the preparations in 15% trichloroacetic acid/acetone/dry ice slurry and stored for 3 h in dry ice. Then trichloroacetic acid was washed out by acetone and the samples were allowed to dry.
The arterial samples were homogenized in SDS-buffer (0.0625 mol/l Tris-HCl (pH 6.8), 2.5% SDS, 10% water-free glycerin, 2.47% dithiothreitol, 0.002% bromophenol blue) supplemented with protease and phosphatase inhibitors (aprotinin 50 mg/ml, leupeptin 100 mg/ml, pepstatin 30 mg/ml, NaF 2 mg/ml, and Na3VO4 180 mg/ml), centrifuged at 14,000 g for 2 min and heated at 99 °С for 2 min; supernatant was kept at −20 °С. Proteins were separated by SDS-PAGE and transferred to nitrocellulose membrane (Santa Cruz) using Trans-Blot Turbo transfer system (BioRad). The transfer was visualized with Ponceau S stain and the membrane was cut in two parts at the level of 70 kDa protein marker (Thermo Scientific). Both parts were blocked with 5% nonfat milk (Applichem, Germany) in TBS (20 mmol/l Tris-HCl, pH 7.6; 150 mmol/l NaCl) with 0.1% Tween 20 (TBSt). Then the lower part of the membrane was incubated overnight with antibodies against GAPDH (Abcam, mouse, 1:2000 in TBSt with 5% milk, Sigma). The upper part was incubated overnight with antibodies against Rho-kinase II (Millipore, rabbit, 1:200 in TBSt) or phospho-MYPT1-Thr855 (Upstate, mouse, 1:1000 in TBSt with 5% milk). Afterwards, all membranes were incubated with appropriate secondary antibodies: anti-mouse (Cell Signaling, 1:5000 in 5% milk) or anti-rabbit (Cell Signaling, 1:10000 in 5% milk) for 1 h and visualized with Super Signal West Dura Substrate (Thermo Scientific) using ChemiDoc (BioRad). Western blotting experiments were analyzed in ImageLab Software (BioRad). Protein of interest to GAPDH ratio was identified in each sample, and then the average ratio in vehicle control group was taken as 100%.
Statistical data analysis
Statistical analysis was performed in GraphPad Prism 6.0. The normality of the data distribution was confirmed using D’Agostino-Pearson test. Unpaired Student’s t-test or Repeated Measures ANOVA were used, as appropriate. Statistical significance was reached at P < 0.05. All data are given as mean ± S.E.M.; n represents the number of animals.
Results
Characteristics of the hypothyroidism model
Similar to our previous observations,9,10 2-week-old progeny of PTU-treated dams as compared to the progeny of control dams had unchanged body weight, reduced serum levels of thyroid hormones, and increased serum level of total cholesterol (Table 2). However, by the age of 10–12 weeks all these parameters did not differ between CON and PTU groups (Table 2). Antenatal/early postnatal hypothyroidism did not alter the diameter and maximum active force of all studied types of arteries (Table 3).
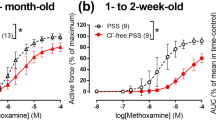
Saphenous artery
Saphenous arteries from control and PTU rats demonstrated similar concentration-response relationships and sensitivity to MX (Fig. 1a, Table 4). Rho-kinase inhibitor Y27632 significantly decreased the responses in both groups, which was evident from reduced values of pD2 and Fmax (Table 4). However, in the presence of Y27632, the responses of saphenous arteries to MX remained similar in control and PTU rats (Fig. 1b, Table 4).
Saphenous arteries from 10–12-week-old male offspring of control and PTU-treated dams demonstrate similar basal tone levels (b.t.) and responses to methoxamine after treatments with either vehicle (a) or Rho-kinase inhibitor Y27632 (3 µM) (b). Number in brackets indicates the number of animals in experimental group
Mesenteric artery
In mesenteric arteries, the concentration-response relationships to MX were similar in control and PTU rats (Fig. 2a, Table 4). Rho-kinase inhibitor Y27632 significantly decreased the sensitivity to MX in both groups, as seen from the reduced values of pD2 and Fmax (Table 4). Of note, in the presence of Y27632 the responses of mesenteric arteries to MX, as well as Fmax were weaker in PTU rats compared to control animals (Fig. 2b, Table 4).
Mesenteric arteries from 10–12-week-old male offspring of PTU-treated dams demonstrate unchanged basal tone level (b.t.) and responses to methoxamine after treatment with vehicle (a) but diminished responses to methoxamine in the presence of Rho-kinase inhibitor Y27632 (3 µM) (b). *p < 0.05 vs. respective control group (Repeated Measures ANOVA). Number in brackets indicates the number of animals in experimental group
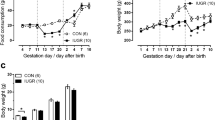
Sural artery
Unlike the two previous types of arteries, sural arteries from PTU rats showed enhanced basal tone level, contractile responses and sensitivity to MX compared to the arteries from CON group (Fig. 3a, Table 4). Rho-kinase inhibitor Y27632 significantly decreased the sensitivity to MX in both groups, as seen from reduced values of pD2 and Fmax (Table 4). Importantly, Rho-kinase inhibition eliminated the intergroup differences in MX-induced contractile responses (Fig. 3b, Table 4). These data indicate that the increase of arterial contractile responses in PTU rats was associated with higher contribution of Rho-kinase-signaling pathway.
Sural arteries from 10–12-week-old male offspring of PTU-treated dams demonstrate augmented basal tone level (b.t.) and responses to methoxamine after treatment with vehicle in comparison to Control rats (a). Basal tone level and responses to methoxamine in the presence of Rho-kinase inhibitor Y27632 (3 µM) are similar in sural arteries of Control and PTU groups (b). Relative contents of Rho-kinase II protein (RhoK, n = 7;7) (c) and RhoA mRNA, (n = 7;7) (d) in sural arteries of Control and PTU groups. e Relative levels of MYPT1 phosphorylation at Thr855 in arteries of Control and PTU groups in the presence of vehicle and Y27632 (n = 7;7;7;7). *p < 0.05 vs. respective control group (Repeated Measures ANOVA). @p < 0.05 vs. respective control group, #p < 0.05 vs. vehicle-treated arteries (unpaired t-test). Number in brackets indicates the number of animals in experimental group
To study the mechanisms of enhanced Rho-kinase pathway activity in sural arteries of PTU rats, we firstly estimated the contents of Rho-kinase protein. There was no difference in this parameter between PTU and control rats (Fig. 3c). These data suggest, that it’s the activation of Rho-kinase that must be augmented in sural arteries of PTU group. Indeed, higher mRNA expression level of RhoA, a key Rho-kinase activator, was observed in arteries of PTU group in comparison to CON (Fig. 3d).
Further, we studied the level of MYPT1 phosphorylation at Thr855, which is an established marker of Rho-kinase signaling pathway activity in smooth muscle cells.11,14 After incubation with vehicle, sural arteries of PTU rats showed significantly increased phosphorylation level of MYPT1 at Thr855 (Fig. 3e), indicating enhanced basal activity of Rho-kinase in arteries of PTU group. Incubation with Y27632 significantly decreased the phosphorylation level of MYPT1 at Thr855 in arteries of both groups (Fig. 3e), confirming the dependence of such phosphorylation on Rho-kinase activity.
Discussion
Here we report a novel finding that antenatal/early postnatal hypothyroidism is followed by augmented procontractile activity of Rho-kinase signaling pathway in intestinal and skeletal muscle arteries of adult rats with completely recovered thyroid state. We show here for the first time the programming effects of thyroid hormones during early stages of development on the activity of Rho-kinase signaling pathway in adulthood.
Thyroid state is completely restored in adult rats suffered from antenatal/early postnatal hypothyroidism
The results of the present study are consistent with our previous findings and show that treatment of dams with relatively low PTU dosage (7 ppm) causes significant reduction of thyroid hormones concentrations in their 2-week-old progeny, which, however, restores to adulthood.9,10 Of note, already at the age of 6 weeks, the progeny of PTU-treated dams demonstrated restored blood levels of thyroid hormones and TSH,20 which is consistent with other studies, where the restoration of thyroid state was observed in 4 weeks after PTU withdrawal.8 Based on the above, we can consider that the adult rats from PTU group had an euthyroid status for at least 4 weeks before their arteries were taken for in vitro studies.
Maximum contractility is not changed in adult rats, suffered from antenatal/early postnatal hypothyroidism
Noteworthy, at the age of 2 weeks the maximum active force of arteries was significantly reduced by antenatal/early postnatal hypothyroidism, along with reduced mRNA contents of smooth muscle differentiation markers, such as, smooth muscle MHC, α-actin, and SERCA2A.10 These data point to the retardation of arterial development by maternal thyroid deficiency. However, the intergroup difference in the maximum active force disappeared by the age of 10–12 weeks, suggesting unaltered contents of contractile proteins in arteries of previously hypothyroid rats. On the other hand, reduced contractility to the agonist of α1-adrenoceptors was observed previously in aorta of adult rats, which suffered from maternal hypothyroidism.21,22 Nevertheless, the dosage of PTU used in the studies above was much higher than in ours, which makes the comparison of the results rather complicated. In addition, the discrepancy of the results can be attributed to inherent regulatory differences between aorta and small arteries.
The effects of antenatal/early postnatal hypothyroidism on Rho-kinase pathway in saphenous and mesenteric arteries
Antenatal/early postnatal hypothyroidism did not alter concentration–response relationships to the agonist of α1-adrenoceptors in saphenous and mesenteric arteries of adult rats. This goes in accordance with our previous observations from 2-week-old progeny of PTU-treated dams.10 Thus, saphenous and mesenteric arteries do not change their overall adrenergic contractile responses due to antenatal/early postnatal hypothyroidism at either age of 2 weeks or in adulthood.
In this study, the contribution of Rho-kinase to α1-adrenergic contractile responses was elevated in mesenteric arteries of adult PTU rats in comparison to control group, while no CON vs. PTU differences in the effects of Rho-kinase inhibitor were observed in saphenous artery. Similarly, the effects of antenatal/early postnatal hypothyroidism on Rho-kinase were visible in mesenteric but not saphenous artery of 2-week-old rats.10
The augmented Y27632 effects in mesenteric arteries of adult previously hypothyroid rats speaks in favor of programming effects of thyroid hormones on Rho-kinase pathway activity in intestinal feed vasculature. However, the mesenteric arteries of adult PTU rats apparently redistribute the activity of Rho-kinase-dependent and independent mechanisms resulting in similar contractile responses compared to control rats. Such plasticity of smooth muscle contractile mechanisms in mesenteric arteries allows to compensate the increased procontractile activity of Rho-kinase pathway evoked by antenatal/early postnatal hypothyroidism.
The effects of antenatal/early postnatal hypothyroidism on Rho-kinase pathway in sural artery in adulthood
Unlike saphenous and mesenteric arteries, sural artery of PTU rats demonstrated increased basal tone level and α1-adrenergic contractile responses. Importantly, these differences between control and PTU rats were eliminated by Rho-kinase inhibitor, indicating the increased activity of Rho-kinase signaling pathway in PTU rats. Elevated activity of Rho-kinase signaling pathway in sural arteries of PTU rats was associated with higher expression of RhoA, a key Rho-kinase activator in vascular smooth muscle.11 Further, increased activity of Rho-kinase signaling pathway in sural arteries of PTU rats was confirmed by higher phosphorylation level of MYPT1 at Thr855. Of note, the phosphorylation level of MYPT1 at Thr855 in both control and PTU rats was Rho-kinase-dependent, indicating it to be a marker of Rho-kinase pathway activity in smooth muscle.14
In the sural artery we didn’t observe any potential redistribution between the activities of Rho-kinase-dependent and independent mechanisms, since we see that α1-adrenergic contractile responses are clearly elevated as a result of antenatal/early postnatal hypothyroidism. The reason why mesenteric, unlike sural artery, can compensate the increased activity of Rho-kinase pathway is currently not clear. In particular, it can be associated with different density of sympathetic innervation in these two types of arteries. Trophic influence of sympathetic nerves was shown to decrease the contribution of Ca2+-sensitizing mechanisms to the arterial contraction, that includes Rho-kinase-dependent mechanisms.23,24 Rat mesenteric arteries are densely innervated by sympathetic fibers,25,26 while only sparse fibers can be observed in rat sural artery wall.27 Therefore, mesenteric arteries with dense sympathetic smooth muscle innervation may more easily compensate the effects of Rho-kinase overactivity in adult rats, which suffered from antenatal/early postnatal hypothyroidism by changing Rho-kinase–independent mechanisms. However, this issue is beyond the aim of the present study and needs to be addressed in the future.
Conclusion
Taken together, our data indicate that antenatal/early postnatal hypothyroidism increases the activity of Rho-kinase pathway in arteries of adult animals despite the normalization of the thyroid hormones level. This finding points to the presence of programming effects of thyroid hormones on Rho-kinase pathway activity during early stages of development. Pathologically elevated activity of Rho-kinase pathway in adulthood can cause insufficient blood supply to certain organs, such as skeletal muscle, and represent a risk factor for the development of cardiovascular disorders.
References
Vargas, F. et al. Vascular and renal function in experimental thyroid disorders. Eur. J. Endocrinol. 154, 197–212 (2006).
Forhead, A. J. & Fowden, A. L. Thyroid hormones in fetal growth and prepartum maturation. J. Endocrinol. 221, R87–R103 (2014).
Yim, C. H. Update on the management of thyroid disease during pregnancy. Endocrinol. Metab. 31, 386 (2016).
Stagnaro-Green, A. Postpartum management of women begun on levothyroxine during pregnancy. Front. Endocrinol. (Lausanne) 6, 183 (2015).
Fowden, A. L., Giussani, D. A. & Forhead, A. J. Intrauterine programming of physiological systems: causes and consequences. Physiol. (Bethesda). 21, 29–37 (2006).
Rytter, D. et al. Maternal thyroid function in pregnancy may program offspring blood pressure, but not adiposity at 20 y of age. Pediatr. Res. 80, 7–13 (2016).
Santos, S. O. et al. Experimental gestational hypothyroidism evokes hypertension in adult offspring rats. Auton. Neurosci. 170, 36–41 (2012).
Ghanbari, M. et al. Hemodynamic properties and arterial structure in male rat offspring with fetal hypothyroidism. Gen. Physiol. Biophys. 35, 397–405 (2016).
Gaynullina, D. K. et al. NO-mediated anticontractile effect of the endothelium is abolished in coronary arteries of adult rats with antenatal/early postnatal hypothyroidism. Nitric Oxide 63, 21–28 (2017).
Sofronova, S. I. et al. Antenatal/early postnatal hypothyroidism alters arterial tone regulation in 2-week-old rats. J. Endocrinol. 235, 137–151 (2017).
Somlyo, A. P. & Somlyo, A. V. Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiol. Rev. 83, 1325–1358 (2003).
Dimopoulos, G. J., Semba, S., Kitazawa, K., Eto, M. & Kitazawa, T. Ca2+-dependent rapid Ca2+ sensitization of contraction in arterial smooth muscle. Circ. Res. 100, 121–129 (2007).
Walsh, M. P. & Cole, W. C. The role of actin filament dynamics in the myogenic response of cerebral resistance arteries. J. Cereb. Blood. Flow. Metab. 33, 1–12 (2013).
Kitazawa, T., Eto, M., Woodsome, T. P. & Khalequzzaman, M. Phosphorylation of the myosin phosphatase targeting subunit and CPI-17 during Ca2+ sensitization in rabbit smooth muscle. J. Physiol. 546, 879–889 (2003).
Shimokawa, H., Sunamura, S. & Satoh, K. RhoA/Rho-kinase in the cardiovascular system. Circ. Res. 118, 352–366 (2016).
Hartmann, S., Ridley, A. J. & Lutz, S. The Function of rho-associated kinases ROCK1 and ROCK2 in the pathogenesis of cardiovascular disease. Front. Pharmacol. 6, 276 (2015).
McAllister, R. M., Delp, M. D. & Laughlin, M. H. Thyroid status and exercise tolerance. Cardiovascular and metabolic considerations. Sports Med. 20, 189–198 (1995).
Mulvany, M. J. & Halpern, W. Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ. Res. 41, 19–26 (1977).
Sofronova, S. I., Gaynullina, D. K., Martyanov, A. A. & Tarasova, O. S. Endogenous oestrogens do not regulate endothelial nitric oxide production in early postnatal rats. Eur. J. Pharmacol. 765, 598–605 (2015).
Gaynullina, D. K. et al. Voluntary exercise training restores anticontractile effect of NO in coronary arteries of adult rats with antenatal/early postnatal hypothyroidism. Nitric Oxide 74, 10–18 (2018).
Sedaghat, K., Zahediasl, S. & Ghasemi, A. Gestational hypothyroidism-induced changes in L-type calcium channels of rat aorta smooth muscle and their impact on the responses to vasoconstrictors. Iran. J. Basic Med. Sci. 18, 172–179 (2015).
Khaksari, M., Shafiee, M., Ghasemi, A. & Asl, S. Z. Effect of orally administered propylthiouracil in pregnant and lactating rats on isolated aorta contractility of their adult male offspring. Med. Sci. Monit. 15, BR123–BR127 (2009).
Mochalov S., et al. Higher Ca2+-sensitivity of arterial contraction in the 1-week-old rats is due to a greater Rho-kinase activity. Acta Physiol. (Oxf.). e13044 (2018). doi: 10.1111/apha.13044.
Puzdrova, V. A. et al. Trophic action of sympathetic nerves reduces arterial smooth muscle Ca(2+) sensitivity during early post-natal development in rats. Acta Physiol. (Oxf.). 212, 128–141 (2014).
Li, M., Galligan, J., Wang, D. & Fink, G. The effects of celiac ganglionectomy on sympathetic innervation to the splanchnic organs in the rat. Auton. Neurosci. 154, 66–73 (2010).
Yokomizo, A., Takatori, S., Hashikawa-Hobara, N., Goda, M. & Kawasaki, H. Characterization of perivascular nerve distribution in rat mesenteric small arteries. Biol. Pharm. Bull. 38, 1757–1764 (2015).
Tarasova, O. et al. A comparative analysis of vasomotor responses and sympathetic innervation of feed arteries from locomotor and respiratory muscles in a rat. Biophys. (Oxf.). 53, 621–625 (2008).
Acknowledgements
This study was supported by the Russian Science Foundation (grant No. 14-15-00704).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gaynullina, D.K., Sofronova, S.I., Shvetsova, A.A. et al. Antenatal/early postnatal hypothyroidism increases the contribution of Rho-kinase to contractile responses of mesenteric and skeletal muscle arteries in adult rats. Pediatr Res 84, 112–117 (2018). https://doi.org/10.1038/s41390-018-0029-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0029-5