Abstract
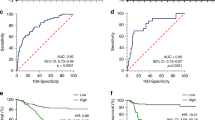
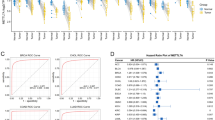
Frequent mutations of genes in the histone-lysine N-methyltransferase 2 (KMT2) family members were identified in gastric cancers (GCs). Understanding how gene mutations of KMT2 family affect cancer progression and tumor immune microenvironment may provide new treatment strategies. A total of 1245 GCs were analyzed using next-generation sequencing, whole transcriptome sequencing, immunohistochemistry (Caris Life Sciences, Phoenix, AZ). The overall mutation rate of genes in the KMT2 family was 10.6%. Compared to KMT2-wild-type GCs, genes involved in epigenetic modification, receptor tyrosine kinases/MAPK/PI3K, and DNA damage repair (DDR) pathways had higher mutation rates in KMT2-mutant GCs (p < 0.05). Significantly higher rates of high tumor mutational burden, microsatellite instability-high/mismatch-repair deficiency (dMMR), and PD-L1 positivity were observed in KMT2-mutant GCs (p < 0.01), compared to KMT2-wild-type GCs. The association between PD-L1 positivity and KMT2 mutations remained significant in the proficient-MMR and microsatellite stable subgroup. Based on transcriptome data from the TCGA, cell cycle, metabolism, and interferon-α/β response pathways were significantly upregulated in KMT2-mutant GCs than in KMT2-wild-type GCs. Patients with KMT2 mutation treated with immune checkpoint inhibitors had longer median overall survival compared to KMT2-wild-type patients with metastatic solid tumors (35 vs. 16 months, HR = 0.73, 95% CI: 0.62–0.87, p = 0.0003). In conclusion, this is the largest study to investigate the distinct molecular features between KMT2-mutant and KMT2-wild-type GCs to date. Our data indicate that GC patients with KMT2 mutations may benefit from ICIs and drugs targeting DDR, MAPK/PI3K, metabolism, and cell cycle pathways.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Selected subset of analyzed data from CARIS are available on reasonable request and through collaborative investigations. The clinical information and tumor DNA/RNA sequencing data about TCGA and MSKCC cohort are available from websites (http://www.cbioportal.org, https://tcga.xenahubs.net).
References
Feinberg AP, Koldobskiy MA, Gondor A. Epigenetic modulators, modifiers and mediators in cancer aetiology and progression. Nat Rev Genet. 2016;17:284–99.
Cristescu R, Lee J, Nebozhyn M, Kim KM, Ting JC, Wong SS, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21:449–56.
Zang ZJ, Cutcutache I, Poon SL, Zhang SL, McPherson JR, Tao J, et al. Exome sequencing of gastric adenocarcinoma identifies recurrent somatic mutations in cell adhesion and chromatin remodeling genes. Nat Genet. 2012;44:570–4.
Wang K, Yuen ST, Xu J, Lee S, Yan HHN, Shi ST, et al. Whole-genome sequencing and comprehensive molecular profiling identify new driver mutations in gastric cancer. Nat Genet. 2014;46:573–82.
Ge S, Li B, Li Y, Li Z, Liu Z, Chen Z, et al. Genomic alterations in advanced gastric cancer endoscopic biopsy samples using targeted next-generation sequencing. AM J Cancer Res. 2017;7:1540–53.
Chen K, Yang D, Li X, Sun B, Song F, Cao W, et al. Mutational landscape of gastric adenocarcinoma in Chinese: implications for prognosis and therapy. Proc Natl Acad Sci USA. 2015;112:1107–12.
Kandoth C, McLellan MD, Vandin F, Ye K, Niu B, Lu C, et al. Mutational landscape and significance across 12 major cancer types. Nature. 2013;502:333–9.
Shilatifard A. Chromatin modifications by methylation and ubiquitination: implications in the regulation of gene expression. Annu Rev Biochem. 2006;75:243–69.
Rao Rajesh C, Yali D. Hijacked in cancer: the KMT2 (MLL) family of methyltransferases. Nat Rev Cancer. 2015;15:334–46.
Kelly TK, De Carvalho DD, Jones PA. Epigenetic modifications as therapeutic targets. Nat Biotechnol. 2010;28:1069–78.
Milne TA, Briggs SD, Brock HW, Martin ME, Gibbs D, Allis CD, et al. MLL targets SET domain methyltransferase activity to Hox gene promoters. Mol Cell. 2002;10:1107–17.
Krivtsov AV, Armstrong SA. MLL translocations, histone modifications and leukaemia stem-cell development. Nat Rev Cancer. 2007;7:823–33.
Fagan Richard J, Dingwall Andrew K. COMPASS ascending: emerging clues regarding the roles of MLL3/KMT2C and MLL2/KMT2D proteins in cancer. Cancer Lett. 2019;458:56–65.
Cho S-J, Yoon C, Lee JH, Chang KK, Lin J, Young-Ho K, et al. KMT2C mutations in diffuse-type gastric adenocarcinoma promote epithelial-to-mesenchymal transition. Clin Cancer Res. 2018;24:6556–69.
Theodoros R, Dimitris K, Margaritis A, Alexander P, Antonis K, Zoi K, et al. The lysine-specific methyltransferase KMT2C/MLL3 regulates DNA repair components in cancer. EMBO Rep. 2019;20:e46821.
Je EM, Lee SH, Yoo NJ, Lee SH. Mutational and expressional analysis of MLL genes in gastric and colorectal cancers with microsatellite instability. Neoplasma. 2012;60:188–95.
Kantidakis T, Saponaro M, Mitter R, Horswell S, Kranz A, Boeing S, et al. Mutation of cancer driver MLL2 results in transcription stress and genome instability. Genes Dev. 2016;30:408–20.
Wang G, Chow RD, Zhu L, Bai Z, Ye L, Zhang F, et al. CRISPR-GEMM pooled mutagenic screening identifies KMT2D as a major modulator of immune checkpoint blockade. Cancer Discov. 2020;10:1912–33.
Jia Q, Wang J, He N, He J, Zhu B. Titin mutation associated with responsiveness to checkpoint blockades in solid tumors. JCI Insight. 2019;4:e127901.
Li X, Pasche B, Zhang W, Chen K. Association of MUC16 mutation with tumor mutation load and outcomes in patients with gastric cancer. JAMA Oncol. 2018;4:1691–8.
Chen H, Chong W, Wu Q, Yao Y, Mao M, Wang X. Association of LRP1B mutation with tumor mutation burden and outcomes in melanoma and non-small cell lung cancer patients treated with immune check-point blockades. Front Immunol. 2019;10:1113.
Okamura R, Kato S, Lee S, Jimenez RE, Sicklick JK, Kurzrock R. ARID1A alterations function as a biomarker for longer progression-free survival after anti-PD-1/PD-L1 immunotherapy. J Immunother Cancer. 2020;8:e000438.
Wang F, Wei XL, Wang FH, Xu N, Shen L, Dai GH, et al. Safety, efficacy and tumor mutational burden as a biomarker of overall survival benefit in chemo-refractory gastric cancer treated with toripalimab, a PD-1 antibody in phase Ib/II clinical trial NCT02915432. Ann Oncol. 2019;30:1479–86.
Bang YJ, Van CE, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687–97.
Italiano A, Soria JC, Toulmonde M, Michot JM, Lucchesi C, Varga A, et al. Tazemetostat, an EZH2 inhibitor, in relapsed or refractory B-cell non-Hodgkin lymphoma and advanced solid tumours: a first-in-human, open-label, phase 1 study. Lancet Oncol. 2018;19:649–59.
Wang Lu Z, Zibo O, Patrick A, Fantini D, Marshall SA, Rendleman EJ, et al. Resetting the epigenetic balance of Polycomb and COMPASS function at enhancers for cancer therapy. Nat Med. 2018;24:758–69.
Park Y, Chui MH, Suryo Rahmanto Y, Yu ZC, Shamanna RA, Bellani MA, et al. Loss of ARID1A in tumor cells renders selective vulnerability to combined ionizing radiation and PARP inhibitor therapy. Clin Cancer Res. 2019;25:5584–94.
Yang L, Yang G, Ding Y, Huang Y, Liu S, Zhou L, et al. Combined treatment with PI3K inhibitor BKM120 and PARP inhibitor olaparib is effective in inhibiting the gastric cancer cells with ARID1A deficiency. Oncol Rep. 2018;40:479–87.
Lv S, Wen H, Shan X, Li J, Wu Y, Yu X, et al. Loss of KMT2D induces prostate cancer ROS-mediated DNA damage by suppressing the enhancer activity and DNA binding of antioxidant transcription factor FOXO3. Epigenetics. 2019;14:1194–208.
Bang YJ, Xu RH, Chin K, Lee KW, Park SH, Rha SY, et al. Olaparib in combination with paclitaxel in patients with advanced gastric cancer who have progressed following first-line therapy (GOLD): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1637–51.
Mitani S, Kawakami H. Emerging targeted therapies for HER2 positive gastric cancer that can overcome trastuzumab resistance. Cancers (Basel). 2020;12:400.
Alam HT, Ming M, Mayinuer D, Shilpa S, Kumar M, Han CY, et al. KMT2D deficiency impairs super-enhancers to confer a glycolytic vulnerability in lung cancer. Cancer Cell. 2020;37:599–617.
Mardis ER. Neoantigens and genome instability: impact on immunogenomic phenotypes and immunotherapy response. Genome Med. 2019;11:71.
Witt DA, Donson AM, Amani V, Moreira DC, Sanford B, Hoffman LM, et al. Specific expression of PD-L1 in RELA-fusion supratentorial ependymoma: Implications for PD-1-targeted therapy. Pediatr Blood Cancer. 2018;65:e26960.
Tokunaga R, Xiu J, Johnston C, Goldberg RM, Philip PA, Seeber A, et al. Molecular profiling of appendiceal adenocarcinoma and comparison with right-sided and left-sided colorectal cancer. Clin Cancer Res. 2019;25:3096–103.
Marabelle A, Fakih M, Lopez J, Shah M, Shapira-Frommer R, Nakagawa K, et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 2020;21:1353–65.
Becht E, Giraldo NA, Lacroix L, Buttard B, Elarouci N, Petitprez F. et al. Estimating the population abundance of tissue-infiltrating immune and stromal cell populations using gene expression. Genome Biol. 2016;17:218.
Salem ME, Puccini A, Xiu J, Raghavan D, Lenz HJ, Korn WM, et al. Comparative molecular analyses of esophageal squamous cell carcinoma, esophageal adenocarcinoma, and gastric adenocarcinoma. Oncologist. 2018;23:1319–27.
Acknowledgements
We would like to thank the staff members of the TCGA Research Network and MSKCC and the cBioportal; as well as all the authors for making their valuable research data public.
Funding
This work was supported by the National Cancer Institute [P30CA 014089 to H-JL], Gloria Borges WunderGlo Foundation, Dhont Family Foundation, Victoria and Philip Wilson Research Fund, San Pedro Peninsula Cancer Guild, the V Foundation for Cancer Research, Eddie Money Research Fund.
Author information
Authors and Affiliations
Contributions
Conception and design: JW, JX, YB, WMK, and H-JL. Development of methodology: JW, JX, YB, WZ, and H-JL. Acquisition of data (carried out experiments, acquired, and managed patients, provided facilities, etc.): JW, JX, YB, BS, RMG, PAP, AS, JJH, AFS, JLM, IA, ACL, ZG, WMK, FB, HA, NK, SS, WZ, and H-JL. Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): JW, JX, YB, WZ, WMK, and H-JL. Writing, review, and/or revision of the manuscript: JW, JX, BS, WMK, FB, HA, NK, SS, WZ, JM, and H-JL. Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): JW, JX, and H-JL. Study supervision: H-JL.
Corresponding author
Ethics declarations
Conflict of interest
H-JL reports receiving honoraria from consultant/advisory board membership for Merck Serono, Bayer, and Genentech. JX, YB, ZG, and WMK are employees of Caris Life Sciences. AFS reports funding for research, travel, and the speakers bureau from Caris Life Sciences. All remaining authors have declared no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, J., Xiu, J., Baca, Y. et al. Large-scale analysis of KMT2 mutations defines a distinctive molecular subset with treatment implication in gastric cancer. Oncogene 40, 4894–4905 (2021). https://doi.org/10.1038/s41388-021-01840-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41388-021-01840-3
This article is cited by
-
Gastric cancer treatment: recent progress and future perspectives
Journal of Hematology & Oncology (2023)
-
SL-scan identifies synthetic lethal interactions in cancer using metabolic networks
Scientific Reports (2023)
-
Chromatin and noncoding RNA-mediated mechanisms of gastric tumorigenesis
Experimental & Molecular Medicine (2023)