Abstract
Shedding of microbial extracellular vesicles constitutes a universal mechanism for inter-kingdom and intra-kingdom communication that is conserved among prokaryotic and eukaryotic microbes. In this review we delineate fundamental aspects of bacterial extracellular vesicles (BEVs) including their biogenesis, cargo composition, and interactions with host cells. We critically examine the evidence that BEVs from the host gut microbiome can enter the circulatory system to disseminate to distant organs and tissues. The potential involvement of BEVs in carcinogenesis is evaluated and future research ideas explored. We further discuss the potential of BEVs in microbiome-based liquid biopsies for cancer diagnostics and bioengineering strategies for cancer therapy.
Similar content being viewed by others
Introduction
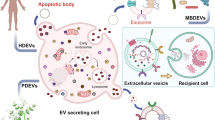
Extracellular vesicles (EVs) are released by all three domains of life—eukaryotes, bacteria, and archaea—and represent a universal, evolutionarily conserved mechanism for intercellular communication [1]. Our growing appreciation of the functional significance of the human microbiota in health and disease has triggered a marked interest in microbial-derived EVs and their functional role in intra-kingdom and inter-kingdom communication, transfer of nutrients within microbial communities, delivery of virulence factors and toxins, horizontal gene transfer, and modulation of host immunity [2,3,4,5,6,7,8,9].
In recent years, the advent of next generation sequencing technologies combined with large scale initiatives like the NIH-funded Human Microbiome Project and the EU-funded Metagenomics of the Human Intestinal Tract consortium has expanded our understanding of the human microbiome and helped shape an evolving view of the human body as a “supraorganism” that harbors trillions of bacterial and human cells in ~1:1 ratio [2, 10,11,12]. These large consortia have revealed staggering microbial gene diversity in the human microbiome as well as tremendous inter-individual variability in the microbial species inhabiting the human body [2, 13]. Interestingly, while the Human Genome Project has revealed a total number of ~20,000 genes for the human genome [14], currently accepted estimations from analyzing the bacterial communities in the gut have yielded more than 2000,000 bacterial genes vastly outnumbering the number of genes contributed by the human genome [2, 10]. A healthy human host is inhabited by more than 1000 microbial species [2]. Most of those belong to a few dominant taxonomic groups, or phyla (Actinobacteria, Bacteroidetes, Firmicutes, Proteobacteria, Cyanobacteria, Fusobacteria) that gives some level of consistency across individuals at the higher taxonomic levels; however, the relative proportions of those phyla, as well as the individual microbial species and genes can vary dramatically across individuals, even in the case of monozygotic twins [15, 16]. Individual humans may be 99.9% identical to one another in terms of their host genome (with ~0.1% of the variation being mostly SNPs and small indels) but completely different (up to 90%) in their microbiome—the collective genome of one’s microbial communities [17].
The relationship of these complex microbial communities (bacteria, fungi, viruses, and archaea) with their human host can be either symbiotic (mutually beneficial), commensal (neutral co-existence), or potentially pathogenic [18]. Accumulating evidence has revealed microbe–host interactions can critically influence host health by manipulating host immune responses, nutrient metabolism, maintenance of the intestinal barrier, and protection from pathogen colonization [9, 19,20,21]. Similarly, disruption of the gut microbiome (a term known as microbial dysbiosis) has been critically implicated in a range of human diseases including cancer, mental health, and cardiovascular and immune disorders [22,23,24].
The intersectionality of microbiome research and EVs owing to advancements in both fields has emerged as promising research endeavor. The increasing appreciation that microbiota-derived EV can enter the systemic circulation and be detected in human body fluids is likely to stimulate completely new areas of investigation in microbiome research, biomarkers and liquid biopsies, BEV-based therapeutics, onco-immunology, as well as fundamental microbial EV biology.
Bacterial extracellular vesicles (BEVs): biogenesis and cargo composition
Bacterial cells communicate with their host and other bacteria through direct contacts and secretion of soluble products, such as metabolites (e.g., short-chain fatty acids), lipoglycans, quorum sensing peptides, nucleic acids, proteins, and membrane vesicles, also known as bacterial extracellular vesicles (BEVs) [25, 26].
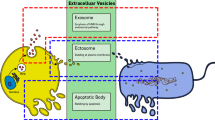
Both pathogenic and commensal bacteria secrete BEVs—spherical membrane-enveloped particles ranging in size from 20–400 nm that disseminate part of the biological content of the parent bacterium into the extracellular milieu [6, 8]. Detailed proteomic and biochemical analyses have shown that BEVs carry diverse cargo including membrane-bound and periplasmic proteins, enzymes (such as autolysins) and toxins, polysaccharides, nucleic acids (DNA and RNA), and peptidoglycan [6, 27]. However, there does not appear to be a single mechanism modulating BEV export, nor universal markers for BEV cargo [28]. Several lines of evidence suggest that BEVs are heterogeneous in their structure, size, density, and molecular cargo composition, and this heterogeneity stems from the different biogenesis routes, the unique membrane envelope structure of the parental bacterium they originate from as well as the genetic background of the producing strain and the growth conditions [8].
Mounting evidence shows BEVs can follow different formation routes, which can lead to distinct BEV subtypes with different molecular cargo and thus potentially different biological function [8, 29]. Gram-negative bacteria follow two main pathways for vesicle formation. The first formation route involves blebbing of the outer membrane of the bacterial envelope, generating outer-membrane vesicles (OMVs); and the second pathway entails explosive cell lysis forming outer-inner membrane vesicles (OIMVs) and explosive outer-membrane vesicles (EOMVs) [8, 26]. Gram-positive bacteria produce cytoplasmic membrane vesicles (CMVs) through endolysin-triggered bubbling cell death [8, 29]. Generally, OMVs are the archetypal BEVs and most heavily studied. The membrane blebbing process giving rise to OMVs generally occurs through a disruption of crosslinks between the outer membrane and the underlying peptidoglycan cell wall layer. Regardless of their biogenesis route, we collectively refer to all those vesicle subtypes as BEVs.
Furthermore, Gram-negative and Gram-positive bacteria have a distinctly different cell envelope architecture, which is reflected in the membrane composition of the BEVs they produce [8, 29]. The cell wall of Gram-negative bacteria consists of a thin layer of peptidoglycan (a polymer-like mesh made of sugars and amino acids) in the periplasmic space between two membrane bilayers; the inner (or cytoplasmic) and outer membrane. The outer membrane contains lipopolysaccharides (LPS; also known as endotoxin) on its outer leaflet and various membrane-bound proteins and channels such as porins that facilitate non-vesicle-mediated transport. In contrast, Gram-positive bacteria completely lack an outer membrane but have a much thicker peptidoglycan cell wall, which is linked to the underlying cytoplasmic membrane via lipoteichoic acids (LTA) [8, 29].
Mirroring this envelope architecture, Gram-negative BEVs consist of an outer membrane with an interior leaflet of phospholipids and an exterior leaflet of LPS, which is known to engage Toll-like receptor 4 (TLR4) [8, 26]. Gram-negative BEVs are typically enriched in various outer-membrane proteins, such as ompA and encapsulate periplasmic luminal components. However, the presence of cytoplasmic cargo (DNA, RNA, virulence factors) is debated and likely contingent on the specific biogenesis route of the three different Gram-negative BEV subtypes (OMV, OIMVs, and EOMVs). Previous reports that have found nucleic acids and cytoplasmic proteins in OMVs might not have been bona fide OMVs, formed through controlled blebbing of the outer membrane as this mechanism does not give direct access to cytoplasmic cargo. Instead, it is the biogenesis mechanism of the double bilayered OIMV and/or the single bilayered-EOMV subtypes that enables direct access to and encapsulation of cytoplasmic cargo. Indeed, endolysin-mediated degradation of the peptidoglycan cell wall (a key process in explosive cell lysis) results in cell envelope fragments that can re-circularize and enclose released chromosomal and plasmid DNA and other nucleic acids or cytoplasmic components. Gram-positive BEV, also known as CMVs as previously mentioned contain both membrane and cytoplasmic components and show LTA on their surface that can engage the Toll-like receptor 2 (TLR2) [26, 29]. A number of other environmental factors can also affect the rate of vesicle production and even bias toward certain biogenesis routes. Some of these include media composition, temperature, growth phase, iron and oxygen availability, exposure to antibiotics, and genotoxic stress [8, 28].
The localization of chromosomal DNA in BEVs from various Gram-negative pathogenic bacteria (Pseudomonas aeruoginosa, Porphyromonas gingivalis, Salmonella Typhimurim) is mostly surface-associated (or extraluminal) with smaller amounts located in the intraluminal space [30]. Sequencing of the intraluminal BEV DNA has been found to be enriched in specific regions of the bacterial chromosome involved in virulence, stress response, antibiotic resistance, and metabolism. It remains speculative at this point, whether surface-associated versus intraluminal BEV DNA serves different functions. It is not unreasonable to assume a potential role for external DNA in biofilm formation versus a role for internal BEV DNA in intercellular communication and horizontal gene transfer of antibiotic resistance or virulence genes [30]. In addition to potentially modulating the innate immune response via or more cytosolic DNA sensors, the possibility that pathogenic BEV-derived DNA can be transferred and detected in the nucleus of non-phagocytic cells (e.g. epithelial cells) [30], raises the intriguing possibility that bacterial genetic material could be transferred to human somatic cells and integrated into the host genome. Integration of bacterial DNA sequences has been in fact detected more frequently in human cancer cells versus normal cells, especially in gastrointestinal (GI)-related tumors with close proximity to the gut microbiome, suggesting a potential role of bacterial DNA in carcinogenesis [31].
Interactions between BEVs and host cells
BEVs contain numerous microbe-associated or pathogen-associated molecular patterns (MAMPs/PAMPs) including LPS, lipoproteins, peptidoglycan, and bacterial nucleic acids. The MAMP content of BEVs enables them to engage with host pattern recognition receptors (PRR) in immune cells as well as nonimmune cells (e.g., epithelial cells at mucosal surfaces) to promote host pathology, immune tolerance, or confer protective immunity [31].
The diverse immunomodulatory effects of BEVs depend largely on the specific parental bacterium and its relationship with the host. For instance, BEVs from pathogenic bacteria have the potential to exacerbate infection by dampening immune responses [32, 33], or trigger an overexaggerated immune reaction resulting in sepsis [5, 34]. In contrast, BEVs from symbiotic or commensal bacterial species in the GI tract promote maturation and immunological tolerance to confer protection from colitis or sepsis [35, 36].
Depending on the localization of PRRs and the specific route of BEV uptake, the recognition of BEV-associated MAMPs/PAMP can occur in various host cellular compartments, including the plasma membrane, endosomes, and cytoplasm [37] (Fig. 1). Cell surface members of the TLR family, namely TLR2 and TLR4, recognize extraluminal BEV ligands such as LPS and LTA molecules, peptidoglycan, and lipoarabinomannan [38,39,40,41,42]. The cytosolic receptors nucleotide-binding oligomerization domain-containing protein 1 (NOD1) and 2 (NOD2) are directly involved in sensing peptidoglycans (key component of bacterial cell wall) present in BEVs secreted from pathogenic or commensal bacteria [43,44,45,46]. NOD1/2 are key components of innate immunity and critical in host defense against bacterial infections and modulation of inflammatory responses. More recently NOD1/2 have been involved in maintaining intestinal homeostasis and microbiota balance [47, 48].
BEVs carry diverse microbe-associated molecular patterns (MAMPs) including LPS, LTA, peptidoglycan fragments, toxins, bacterial DNA and RNA that may activate extracellular or intracellular PRRs depending on the route of uptake and the nature of the bacterial ligand. Members of the Toll-like receptor (TLR) family, nucleotide-binding oligomerization domain (NOD)-like receptors, retinoic-acid-inducible gene-1 (RIG-I) receptors, and various cytosolic DNA sensors including cyclic GMP–AMP synthase (cGAS), interferon-γ-inducible protein 16 (IFI16), and absent in melanoma (AIM2). Adapted by permission from Springer Nature Ltd: Nat. Rev. Dis. Primers. Arroyo and Jalan. Acute-on-chronic liver failure in cirrhosis [87]. Copyright (2016) conveyed through Copyright Clearance Center, Inc.
Intraluminal BEV nucleic acids can be detected via DNA-sensing and RNA-sensing receptors. Following endocytosis, BEV RNA cargo can be sensed through endosomal TLRs including TLR3, TLR7, TLR8, and TLR13. Similarly, RNAs delivered into the cytoplasm following fusion of BEVs with the host cell plasma membrane can activate cytosolic RNA sensors such as RIG-I-like receptors [5]. In a similar way, BEV DNA cargo can be sensed through the endosomal TLR9 or the cytosolic DNA-sensing cyclic GMP–AMP synthase–stimulator of interferon genes pathway, although direct evidence for the latter is lacking [40, 49, 50]. Various routes of BEV endocytosis have been described in host cells including macropinocytosis, lipid-raft-dependent and lipid-raft-independent endocytosis, as well as dynamin-, caveolin-, and clarithin-dependent entry [6]. The utilization of different paths of uptake may reflect the size heterogeneity of BEVs and the size selectivity of each route of endocytosis.
In general, PRR activation triggers the activation of kinases and transcription factors, that lead to the production of cytokines and chemokines resulting in the recruitment of immune cells and upregulation of co-stimulatory molecules commonly involved in adaptive immunity. TLRs for instance, signal via the adapter proteins myeloid differentiation primary response 88 or TIR-domain-containing adapter-inducing interferon-β, leading to downstream activation and nuclear translocation of transcription factors including nuclear factor kappa-light-chain-enhancer of activated B cells, interferon-regulatory factor, and activator protein-1 to induce production of pro-inflammatory cytokines and type I interferons [5, 51].
Microbiota-derived BEVs can enter the systemic circulation and disseminate to distant organs
There exists a growing consensus that BEVs from the resident microbiota can enter the systemic circulation [26, 52,53,54,55,56,57]. BEVs released by bacteria in the gut lumen can cross the epithelial barrier to gain access into the underlying submucosa enabling them to interact with various resident immune cell populations (dendritic cells, neutrophils and macrophages) as well as potentially disseminate more widely around the body via the systemic or lymphatic circulation to reach distant tissues and organs or even the brain (Fig. 2).
Microbial dysbiosis can lead to disruption of tight junctions in the luminal epithelium leading to passive paracellular transport of BEVs into the underlying submucosa, where BEVs can interact with resident immune cells or enter the circulatory system/portal vein and lymphatics (via trans-endothelial migration) for systemic dissemination. Active transcytosis through an intact gut luminal epithelium during steady state is thought to result in a smaller number of BEVs escaping to the submucosal compartment with subsequent blood-borne dissemination.
The presence of systemic circulating BEVs was recently reported by Tulkens et al. in the plasma of patients with altered intestinal barrier function [52]. Of note, a number of communicable and noncommunicable diseases as well as lifestyle factors can trigger gut microbial dysbiosis thereby altering intestinal permeability, including obesity, diabetes, antibiotic use, diet and caloric restriction, or sleep deprivation. In the aforementioned study, patients with HIV, inflammatory bowel disease, or intestinal mucositis were found to have elevated circulating LPS-positive BEVs relative to healthy controls. The level of circulating BEVs correlated positively, but modestly, with the plasma levels of zonulin—a biomarker of epithelial barrier integrity—that phosphorylates ZO-1 proteins in epithelial and endothelial cells leading to tight junction disassembly. While these BEVs are likely to be originating by gut bacteria, the authors did not fully prove it leaving the possibility of contributions from microbial niches in other body sites. Simulating compromised tight junction integrity using an in vitro colitis model (Caco-2 epithelial monolayer challenged with DSS) also resulted in paracellular translocation of BEVs. The same group by Tulkens et al. most recently reported a detailed protocol for recovering BEVs with high specificity from human body fluids, including blood plasma and stool through the sequential implementation of size-exclusion chromatography and density-gradient ultracentrifugation [26]. The underlying physical property that distinguishes BEVs from host-derived eukaryotic EVs (EEVs) in blood plasma is their differential buoyant density. When run on a density gradient, EEVs float typically at 1.083–1.111 g/mL while BEVs are slightly heavier at 1.133–1.201 g/mL. This allows for label-free isolation of BEVs from EEVs, although subsequent biochemical characterization is typically needed. This was the first study that provided a preliminary characterization of BEVs in human body fluids with ompA and LPS being the markers for BEV identification. However, a low yield of BEV in blood plasma (~106 BEV/mL) was typically noted. Interestingly, plasma contained BEVs from both Gram-negative (TLR4 reporter assay) and Gram-positive bacteria (TLR2 reporter assay) and immunogold electron microscopy also identified the presence of both single-bilayered and double-bilayered BEVs, the latter being indicative of OIMVs, which typically contain cytoplasmic cargo and nucleic acids. The presence of chromosomal DNA in circulating OIMVs was not pursued further and 16s rRNA sequencing data are lacking. Implementation of rigorous experimental controls is imperative for samples with low microbial biomass that are inherently prone to misinterpretation due to contaminating molecules from commonly used laboratory reagents in DNA extraction kits and library preparation [58, 59].
While these studies leave the impression that entry of BEVs in the circulatory system occurs only under certain conditions of compromised gut epithelial barrier integrity, this phenomenon may be common even in the steady state of healthy individuals. Indeed, a recent study looked into the biodistribution of fluorescently labeled BEVs (derived from the major human gut commensal bacteria Bacteroides thetaiotaomicron) following oral administration in mice under normal healthy conditions [53]. While the majority of the labeled BEVs remained in the lumen of the GI tract, a small population could enter the circulatory or lymphatic systems via the GI tract. Some of the BEVs were found to accumulate in the liver, suggesting that they can transmigrate through the intestinal epithelium and enter the hepatobiliary system through the portal vein. A portion of the BEVs could also be detected in the heart and lungs suggesting BEVs can cross several host cellular barriers including epithelial barrier and the lymphatic-vascular endothelium to enter the bloodstream and disseminate systemically. Even if the gut epithelial barrier is not compromised leading to increased paracellular transport, BEVs could use other mechanisms to enter the circulatory system, such as active trans-cellular migration across the intestinal epithelium [60]. In fact, active trans-cellular migration across epithelial monolayers has been observed for eukaryotic exosomes (e.g., endocytosis, MVB formation, and exocytosis across the other side of the layer) and has even been suggested as a possible mechanism for breaching the blood–brain barrier [61]. Luminal antigens and BEVs may also be captured by dendritic cells (from the underlying lamina propria) and transported through the intestinal epithelium or via the assistance of mucus-secreting goblet cells [56, 62,63,64]. In addition, intestinal M-cells (specialized epithelial cells of the mucosa-associated lymphoid tissue) could be involved in the translocation of luminal BEVs to the submucosa and systemic circulation [65]. Macrophages infected with pathogenic bacteria are known to release exosomes with BEV-associated components that can elicit pro-inflammatory responses. The uptake, intracellular trafficking, and processing of BEV cargo by the intestinal epithelium needs to be further investigated to examine the possibility of de novo secretion of host epithelial-cell-derived exosomes carrying luminal BEV-associated cargo; this would represent a mechanism of transferring luminal antigens and BEVs directly to antigen-presenting cells in the submucosa. Circumstantial evidence for this exist from a study in which exosomes recovered from the basolateral compartment of BEV-treated epithelial cells were found to encapsulate BEV antigens as well as from a co-culture model in which exposure of dendritic cells to conditioned media from BEV-stimulated epithelial cells resulted in polarization to a mixed TH2-type and TH17-type response [6, 66,67,68].
A case for the existence of blood-derived BEVs has also been reported in a transgenic mouse model of Alzheimer’s disease [55]. Metagenomic sequencing of the blood-derived BEV DNA revealed taxonomical diversity that reflected the diversity of the intestinal microbiota as well as a distinct BEV-associated microbial landscape relative to wild-type controls. Blood-derived BEVs could represent an alternative to fecal sampling for profiling the gut microbiome and evaluating pathogenic variations in the intestinal microbiota (dysbiosis) in the context of neurodegenerative diseases. A few studies have also reported the presence of bacterial nucleic acids in the brain [69]. In view of the presence of BEVs in the bloodstream and their ability to cross boundary epithelial layers, it is interesting to speculate that a fraction of the circulating BEVs might gain access to the brain through the blood–brain barrier or alternatively be produced by brain-resident bacteria.
The gut microbiome is highly dynamic and impacted by a plethora of environmental factors such as diet, exercise, sleep habits, and medications. The presence of BEVs in systemic circulation through their translocation from GI tract or other microbial niches has challenged our notion that blood is a sterile compartment and has put BEVs in the spotlight as long-range “hormonal-like” mediators of inter-kingdom communication. Future investigations are expected to delve deeper into the cross-talk between the resident microbiota and distant organs mediated by systemically circulating BEVs, as this would further expand our understanding of how the human microbiome can regulate tissue and organ homeostasis in health and disease.
Microbial dysbiosis and BEVs: implications for oncogenesis, cancer diagnosis, and therapy
Microbial dysbiosis is a major contributing factor in oncogenesis and tumor progression for a number of GI-tract-related malignancies, including gastric, colorectal, liver, and pancreatic cancer, and might even influence the treatment response to chemotherapy and immunotherapy [33, 70,71,72,73,74,75,76,77,78,79]. The mechanisms by which bacteria affect carcinogenesis and tumor progression are largely unknown. Some of the tumor-promoting mechanisms could be direct such as by inducing genomic instability or indirect by generating a pro-inflammatory tumor microenvironment (TME) and suppression of immunosurveillance [72, 73]. Although BEVs have been implicated in the pathogenesis of inflammatory disease [6, 80], their role in cancer remains unknown. It is also uncertain whether the tumor-promoting or tumor-inhibiting effects of the inter-kingdom cross-talk between the intestinal or intra-tumoral bacteria and the host cells in the TME is mediated through secreted microbial metabolites such as SCFAs or BEVs.
It is a tantalizing possibility that the gut microbiome may be implicated in all carcinomas including those that are ostensibly remote from the GI lumen (or its drainage) through the immunomodulatory action of systemically circulating BEVs on recipient cells in distant organs, or even participating in the formation of pre-metastastic niches. Some indirect preliminary evidence toward this direction came out from a seminal retrospective pan-cancer examination of whole-genome sequencing datasets in the TCGA (33 cancer types from 10,000 treatment-naïve patients totaling 17,000 samples) for microbial reads that found unique microbial signatures in tissue and blood that could discriminate between and within most major types of cancer, including tumors distally from the GI tract [57]. The authors used various computational approaches, including independently trained machine learning models to filter, normalize, and classify microbial sequences. After stringent filtering approaches to remove potential contamination that discarded up to 92.3% of total sequencing reads, a total of 0.9% of the total reads could be mapped to sequences of microbial origin and resolved to a particular genus. The TCGA-derived blood-borne microbial DNA (mbDNA) signatures could discriminate within and between most cancer types even in low-grade tumor stages and in cancers lacking genomic alterations. Apart from the retrospective bioinformatic analysis, the group further validated the mbDNA models while benchmarking against plasma-based cell-free tumor DNA (ctDNA) assays in a separate cohort, which included a group of healthy controls and a group of individuals with advanced-stage cancer, including prostate cancer, lung cancer, and melanoma. Remarkably, plasma-based cell-free mbDNA retained strong generalizable discrimination between healthy controls and grouped patients with cancer with specificity and sensitivity exceeding 90% while also retaining high discriminatory capacity in pairwise comparisons between the three individual types of cancer and their respective healthy controls, except for melanoma.
This study raises the possibility of using microbial-based liquid biopsies for early detection of certain cancers and tumors lacking known mutational drivers. Such a microbiome-based oncology diagnostic tool might provide distinct advantages over regular ctDNA assays in predicting and stratifying patients based on differential survival and treatment response. This is because oncogenesis can proceed at variable rates in hosts with similar cancer mutational landscapes but with host microbial factors playing a much bigger role. In fact, pancreatic tumors from long-term survivors have a high quantity and quality of neoantigens [81], that exhibit homology to infectious disease-derived peptides, suggesting a neoantigen molecular mimicry with microbial epitopes, and demonstrating host microbial factors can be predictive of patient outcomes. This was corroborated with a recent study showing that the tumor microbiome in PDAC patients is predictive of long versus short-term survival irrespective of the genomic composition of the tumor [74].
It remains undetermined whether the observed microbial nucleic acids in the blood came from live or lysed bacteria or BEVs. The presence of live bacteria in blood is improbable as it would likely cause some degree of bacteremia but conclusive data could be made available through culturomics, rather than metagenomics, to identify the existence of otherwise hard-to-culture live blood-borne bacteria. The most likely scenario, given the results obtained from the plasma-derived, cell-free DNA validation cohort as well as the accumulating evidence arguing for the presence of DNA-containing circulating BEVs, that at least a significant portion of those nucleic acids is associated with BEVs. More work will be needed to determine whether this is the case, and whether the DNA-containing microbial EVs are driving cancer or are merely passengers.
To date there is no mechanistic study investigating how BEVs can impact oncogenesis and tumor progression, and their role is likely to be nuanced and context-dependent. Previous studies of BEVs in infectious diseases could provide hints for their putative role in cancer. For instance, microbial dysbiosis in cancer could trigger the systemic release of microbiota-derived BEVs that could act as tumor-promoting entities by invoking tolerogenic immune reprogramming of the TME. This could be achieved through different routes by BEVs driving suppressive cellular monocytic differentiation in a TLR-dependent manner, to indirectly elicit T-cell anergy [73]. The distal action of systemic gut-derived circulating BEVs might also be the missing link between conditions associated with persistent disturbances in gut microbiota and metastatic dissemination of pre-established tumors. BEV-associated MAMPs could interact with host cells in distant organs to initiate pro-inflammatory signaling and trigger alterations in the myeloid landscape to foster pre-metastatic niches for future colonization.
From a therapeutic standpoint one could speculate that systemic administration of commensal healthy host-derived BEVs directly to tumor-bearing hosts could represent a superior alternative to fecal microbiota transplantation that is currently being pursued in clinical trials [82]. BEVs possess several intrinsic properties that have made them appealing candidates for vaccine development against infectious pathogens. BEVs exhibit high stability to a wide range of temperatures and treatments and are non-replicative in nature and thus safe, and carry many of the same immunogenic surface- and membrane-associated components of their parental bacterium [6]. Depending on the originating species, BEVs can stimulate both humoral and cell-mediated immunity and together with their nanoparticulate nature, provide them with their own adjuvanticity, as they are able to enhance T-cell response to antigens. For instance, the clinically approved OMV-based 4CMenB vaccine containing three highly immunogenic proteins confers broad protective antibody responses against different Neisseria meningitidis (N. menigitidis) serogroup B isolates [83]. Notably, the same OMV-based vaccine that protects against N. meningitidis also confers a level of cross-protection against Neisseria gonorrhoeae likely due to the genetic and antigenic similarity shared between the two pathogens [84, 85]. The endotoxicity of BEVs can be easily manipulated through genetic engineering techniques. One could speculate that BEVs from certain commensal bacteria may have therapeutic value. In the future, we expect to see surging interest in the potential of BEVs as cancer immunotherapeutic agents to elicit durable antitumor immune responses or alternatively as personalized or universal cancer vaccines. The potential of BEVs in cancer immunotherapy was highlighted by a recent report showing that systemic intravenous administration of Gram-negative BEVs from the genetically modified Escherichia Coli (E. coli) msbB−/− strain (endotoxin-free) has a selective tropism for tumor tissue (potentially through the EPR effect) and a remarkably capability of inducing long-term antitumor immune responses through the production of cytokines CXCL10 and interferon-γ that can fully eradicate established tumors without notable adverse effects [86]. Similar antitumor effects were also observed for the Gram-positive BEVs derived from Lactobacillus Acidophilus (L. Acidophilus) and Staphylococcus Aureus (S. Aureus).
There is also an enormous potential in using genetic engineering techniques to modify bacteria and subsequently purify recombinant BEVs for use as cancer vaccines. BEV-based cancer vaccines decorated with multiple heterologous tumor antigens on their surface and/or immunostimulatory bacterial DNA (CpG motifs) for targeted delivery to antigen-presenting cells hold immense potential for eliciting a strong durable antitumor immune response potentially in conjunction to CTLA-4 and anti-PD1 immunotherapies.
References
Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367:eaau6977.
Gilbert JA, Blaser MJ, Caporaso JG, Jansson JK, Lynch SV, Knight R. Current understanding of the human microbiome. Nat Med. 2018;24:392–400.
Deatherage BL, Cookson BT. Membrane vesicle release in bacteria, eukaryotes, and archaea: a conserved yet underappreciated aspect of microbial life. Infect Immun. 2012;80:1948–57.
Ellis TN, Kuehn MJ. Virulence and immunomodulatory roles of bacterial outer membrane vesicles. Microbiol Mol Biol Rev. 2010;74:81–94.
Tsatsaronis JA, Franch-Arroyo S, Resch U, Charpentier E. Extracellular vesicle RNA: a universal mediator of microbial communication? Trends Microbiol. 2018;26:401–10.
Kaparakis-Liaskos M, Ferrero RL. Immune modulation by bacterial outer membrane vesicles. Nat Rev Immunol. 2015;15:375–87.
Schwechheimer C, Kuehn MJ. Outer-membrane vesicles from Gram-negative bacteria: biogenesis and functions. Nat Rev Microbiol. 2015;13:605–19.
Toyofuku M, Nomura N, Eberl L. Types and origins of bacterial membrane vesicles. Nat Rev Microbiol. 2019;17:13–24.
Macia L, Nanan R, Hosseini-Beheshti E, Grau GE. Host- and microbiota-derived extracellular vesicles, immune function, and disease development. Int J Mol Sci. 2019;21:1.
Human Microbiome Project C. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–14.
Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65.
Sender R, Fuchs S, Milo R. Are we really vastly outnumbered? Revisiting the ratio of bacterial to host cells in humans. Cell. 2016;164:337–40.
Tierney BT, Yang Z, Luber JM, Beaudin M, Wibowo MC, Baek C, et al. The landscape of genetic content in the gut and oral human microbiome. Cell Host Microbe. 2019;26:283–95.e8.
International Human Genome Sequencing C. Finishing the euchromatic sequence of the human genome. Nature. 2004;431:931–45.
Turnbaugh PJ, Quince C, Faith JJ, McHardy AC, Yatsunenko T, Niazi F, et al. Organismal, genetic, and transcriptional variation in the deeply sequenced gut microbiomes of identical twins. Proc Natl Acad Sci USA. 2010;107:7503–8.
Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457:480–4.
Ursell LK, Metcalf JL, Parfrey LW, Knight R. Defining the human microbiome. Nutr Rev. 2012;70:S38–44.
Group NHW, Peterson J, Garges S, Giovanni M, McInnes P, Wang L, et al. The NIH human microbiome project. Genome Res. 2009;19:2317–23.
Yang J, Kim EK, McDowell A, Kim YK. Microbe-derived extracellular vesicles as a smart drug delivery system. Transl Clin Pharmacol. 2018;26:103–10.
Young VB. The role of the microbiome in human health and disease: an introduction for clinicians. BMJ 2017;356:j831.
Takiishi T, Fenero CIM, Camara NOS. Intestinal barrier and gut microbiota: Shaping our immune responses throughout life. Tissue Barriers. 2017;5:e1373208.
Gopalakrishnan V, Helmink BA, Spencer CN, Reuben A, Wargo JA. The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell. 2018;33:570–80.
Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–71.
Zitvogel L, Ma Y, Raoult D, Kroemer G, Gajewski TF. The microbiome in cancer immunotherapy: diagnostic tools and therapeutic strategies. Science. 2018;359:1366–70.
Hughes DT, Sperandio V. Inter-kingdom signalling: communication between bacteria and their hosts. Nat Rev Microbiol. 2008;6:111–20.
Tulkens J, De Wever O, Hendrix A. Analyzing bacterial extracellular vesicles in human body fluids by orthogonal biophysical separation and biochemical characterization. Nat Protoc. 2020;15:40–67.
Lee EY, Bang JY, Park GW, Choi DS, Kang JS, Kim HJ, et al. Global proteomic profiling of native outer membrane vesicles derived from Escherichia coli. Proteomics. 2007;7:3143–53.
Orench-Rivera N, Kuehn MJ. Environmentally controlled bacterial vesicle-mediated export. Cell Microbiol. 2016;18:1525–36.
Brown L, Wolf JM, Prados-Rosales R, Casadevall A. Through the wall: extracellular vesicles in Gram-positive bacteria, mycobacteria and fungi. Nat Rev Microbiol. 2015;13:620–30.
Bitto NJ, Chapman R, Pidot S, Costin A, Lo C, Choi J, et al. Bacterial membrane vesicles transport their DNA cargo into host cells. Sci Rep. 2017;7:7072.
Riley DR, Sieber KB, Robinson KM, White JR, Ganesan A, Nourbakhsh S, et al. Bacteria-human somatic cell lateral gene transfer is enriched in cancer samples. PLoS Comput Biol. 2013;9:e1003107.
Lee HS, Boulton IC, Reddin K, Wong H, Halliwell D, Mandelboim O, et al. Neisserial outer membrane vesicles bind the coinhibitory receptor carcinoembryonic antigen-related cellular adhesion molecule 1 and suppress CD4+ T lymphocyte function. Infect Immun. 2007;75:4449–55.
Peek RM Jr., Blaser MJ. Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer. 2002;2:28–37.
Shah B, Sullivan CJ, Lonergan NE, Stanley S, Soult MC, Britt LD. Circulating bacterial membrane vesicles cause sepsis in rats. Shock. 2012;37:621–8.
Shen Y, Giardino Torchia ML, Lawson GW, Karp CL, Ashwell JD, Mazmanian SK. Outer membrane vesicles of a human commensal mediate immune regulation and disease protection. Cell Host Microbe. 2012;12:509–20.
Kang CS, Ban M, Choi EJ, Moon HG, Jeon JS, Kim DK, et al. Extracellular vesicles derived from gut microbiota, especially Akkermansia muciniphila, protect the progression of dextran sulfate sodium-induced colitis. PLoS ONE. 2013;8:e76520.
Kawai T, Akira S. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol. 2010;11:373–84.
Gu L, Meng R, Tang Y, Zhao K, Liang F, Zhang R, et al. Toll-like receptor 4 signaling licenses the cytosolic transport of lipopolysaccharide from bacterial outer membrane vesicles. Shock. 2019;51:256–65.
Zhao K, Deng X, He C, Yue B, Wu M. Pseudomonas aeruginosa outer membrane vesicles modulate host immune responses by targeting the Toll-like receptor 4 signaling pathway. Infect Immun. 2013;81:4509–18.
Cecil JD, O’Brien-Simpson NM, Lenzo JC, Holden JA, Chen YY, Singleton W, et al. Differential responses of pattern recognition receptors to outer membrane vesicles of three periodontal pathogens. PLoS ONE. 2016;11:e0151967.
Prados-Rosales R, Baena A, Martinez LR, Luque-Garcia J, Kalscheuer R, Veeraraghavan U, et al. Mycobacteria release active membrane vesicles that modulate immune responses in a TLR2-dependent manner in mice. J Clin Invest. 2011;121:1471–83.
Athman JJ, Wang Y, McDonald DJ, Boom WH, Harding CV, Wearsch PA. Bacterial membrane vesicles mediate the release of mycobacterium tuberculosis lipoglycans and lipoproteins from infected macrophages. J Immunol. 2015;195:1044–53.
Bitto NJ, Baker PJ, Dowling JK, Wray-McCann G, De Paoli A, Tran LS, et al. Membrane vesicles from Pseudomonas aeruginosa activate the noncanonical inflammasome through caspase-5 in human monocytes. Immunol Cell Biol. 2018;96:1120–30.
Canas MA, Fabrega MJ, Gimenez R, Badia J, Baldoma L. Outer membrane vesicles from probiotic and commensal Escherichia coli activate NOD1-mediated immune responses in intestinal epithelial cells. Front Microbiol. 2018;9:498.
Kaparakis M, Turnbull L, Carneiro L, Firth S, Coleman HA, Parkington HC, et al. Bacterial membrane vesicles deliver peptidoglycan to NOD1 in epithelial cells. Cell Microbiol. 2010;12:372–85.
Thay B, Damm A, Kufer TA, Wai SN, Oscarsson J. Aggregatibacter actinomycetemcomitans outer membrane vesicles are internalized in human host cells and trigger NOD1- and NOD2-dependent NF-kappaB activation. Infect Immun. 2014;82:4034–46.
Cecil JD, O’Brien-Simpson NM, Lenzo JC, Holden JA, Singleton W, Perez-Gonzalez A, et al. Outer membrane vesicles prime and activate macrophage inflammasomes and cytokine secretion in vitro and in vivo. Front Immunol. 2017;8:1017.
Chu H, Khosravi A, Kusumawardhani IP, Kwon AH, Vasconcelos AC, Cunha LD, et al. Gene-microbiota interactions contribute to the pathogenesis of inflammatory bowel disease. Science. 2016;352:1116–20.
Motwani M, Pesiridis S, Fitzgerald KA. DNA sensing by the cGAS-STING pathway in health and disease. Nat Rev Genet. 2019;20:657–74.
Vidakovics ML, Jendholm J, Morgelin M, Mansson A, Larsson C, Cardell LO, et al. B cell activation by outer membrane vesicles—a novel virulence mechanism. PLoS Pathog. 2010;6:e1000724.
Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol. 2004;4:499–511.
Tulkens J, Vergauwen G, Van Deun J, Geeurickx E, Dhondt B, Lippens L, et al. Increased levels of systemic LPS-positive bacterial extracellular vesicles in patients with intestinal barrier dysfunction. Gut. 2020;69:191–3.
Jones EJ, Booth C, Fonseca S, Parker A, Cross K, Miquel-Clopes A, et al. The uptake, trafficking, and biodistribution of bacteroides thetaiotaomicron generated outer membrane vesicles. Front Microbiol. 2020;11:57.
Stentz R, Carvalho AL, Jones EJ, Carding SR. Fantastic voyage: the journey of intestinal microbiota-derived microvesicles through the body. Biochem Soc Trans. 2018;46:1021–7.
Park JY, Choi J, Lee Y, Lee JE, Lee EH, Kwon HJ, et al. Metagenome analysis of bodily microbiota in a mouse model of alzheimer disease using bacteria-derived membrane vesicles in blood. Exp Neurobiol. 2017;26:369–79.
Castillo DJ, Rifkin RF, Cowan DA, Potgieter M. The healthy human blood microbiome: fact or fiction? Front Cell Infect Microbiol. 2019;9:148.
Poore GD, Kopylova E, Zhu Q, Carpenter C, Fraraccio S, Wandro S, et al. Microbiome analyses of blood and tissues suggest cancer diagnostic approach. Nature. 2020;579:567–74.
Lauder AP, Roche AM, Sherrill-Mix S, Bailey A, Laughlin AL, Bittinger K, et al. Comparison of placenta samples with contamination controls does not provide evidence for a distinct placenta microbiota. Microbiome. 2016;4:29.
Salter SJ, Cox MJ, Turek EM, Calus ST, Cookson WO, Moffatt MF, et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 2014;12:87.
Chen CC, Liu L, Ma F, Wong CW, Guo XE, Chacko JV, et al. Elucidation of exosome migration across the blood–brain barrier model in vitro. Cell Mol Bioeng. 2016;9:509–29.
Morad G, Carman CV, Hagedorn EJ, Perlin JR, Zon LI, Mustafaoglu N, et al. Tumor-derived extracellular vesicles breach the intact blood-brain barrier via transcytosis. ACS Nano. 2019;13:13853–65.
McDole JR, Wheeler LW, McDonald KG, Wang B, Konjufca V, Knoop KA, et al. Goblet cells deliver luminal antigen to CD103+ dendritic cells in the small intestine. Nature. 2012;483:345–9.
Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, Bonasio R, et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2:361–7.
Niess JH, Brand S, Gu X, Landsman L, Jung S, McCormick BA, et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science. 2005;307:254–8.
Lelouard H, Fallet M, de Bovis B, Meresse S, Gorvel JP. Peyer’s patch dendritic cells sample antigens by extending dendrites through M cell-specific transcellular pores. Gastroenterology. 2012;142:592–601 e3.
Giri PK, Schorey JS. Exosomes derived from M. Bovis BCG infected macrophages activate antigen-specific CD4+ and CD8+ T cells in vitro and in vivo. PLoS ONE. 2008;3:e2461.
O’Neill HC, Quah BJ. Exosomes secreted by bacterially infected macrophages are proinflammatory. Sci Signal. 2008;1:pe8.
Chatterjee D, Chaudhuri K. Vibrio cholerae O395 outer membrane vesicles modulate intestinal epithelial cells in a NOD1 protein-dependent manner and induce dendritic cell-mediated Th2/Th17 cell responses. J Biol Chem. 2013;288:4299–309.
Emery DC, Shoemark DK, Batstone TE, Waterfall CM, Coghill JA, Cerajewska TL, et al. 16S rRNA next generation sequencing analysis shows bacteria in alzheimer’s post-mortem brain. Front Aging Neurosci. 2017;9:195.
Aykut B, Pushalkar S, Chen R, Li Q, Abengozar R, Kim JI, et al. The fungal mycobiome promotes pancreatic oncogenesis via activation of MBL. Nature. 2019;574:264–7.
Mima K, Nishihara R, Qian ZR, Cao Y, Sukawa Y, Nowak JA, et al. Fusobacterium nucleatum in colorectal carcinoma tissue and patient prognosis. Gut. 2016;65:1973–80.
Pleguezuelos-Manzano C, Puschhof J, Rosendahl Huber A, van Hoeck A, Wood HM, Nomburg J, et al. Mutational signature in colorectal cancer caused by genotoxic pks(+) E. coli. Nature. 2020;580:269–73.
Pushalkar S, Hundeyin M, Daley D, Zambirinis CP, Kurz E, Mishra A, et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov. 2018;8:403–16.
Riquelme E, Zhang Y, Zhang L, Montiel M, Zoltan M, Dong W, et al. Tumor microbiome diversity and composition influence pancreatic cancer outcomes. Cell. 2019;178:795–806.e12.
Wilson MR, Jiang Y, Villalta PW, Stornetta A, Boudreau PD, Carra A, et al. The human gut bacterial genotoxin colibactin alkylates DNA. Science. 2019;363:eaar7785.
Gopalakrishnan V, Spencer CN, Nezi L, Reuben A, Andrews MC, Karpinets TV, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 2018;359:97–103.
Geller LT, Barzily-Rokni M, Danino T, Jonas OH, Shental N, Nejman D, et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science. 2017;357:1156–60.
Matson V, Fessler J, Bao R, Chongsuwat T, Zha Y, Alegre ML, et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science. 2018;359:104–8.
Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillere R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359:91–7.
Yu YJ, Wang XH, Fan GC. Versatile effects of bacterium-released membrane vesicles on mammalian cells and infectious/inflammatory diseases. Acta Pharm Sin. 2018;39:514–33.
Balachandran VP, Luksza M, Zhao JN, Makarov V, Moral JA, Remark R, et al. Identification of unique neoantigen qualities in long-term survivors of pancreatic cancer. Nature. 2017;551:512–6.
McQuade JL, Daniel CR, Helmink BA, Wargo JA. Modulating the microbiome to improve therapeutic response in cancer. Lancet Oncol. 2019;20:e77–e91.
Vesikari T, Esposito S, Prymula R, Ypma E, Kohl I, Toneatto D, et al. Immunogenicity and safety of an investigational multicomponent, recombinant, meningococcal serogroup B vaccine (4CMenB) administered concomitantly with routine infant and child vaccinations: results of two randomised trials. Lancet. 2013;381:825–35.
Petousis-Harris H, Paynter J, Morgan J, Saxton P, McArdle B, Goodyear-Smith F, et al. Effectiveness of a group B outer membrane vesicle meningococcal vaccine against gonorrhoea in New Zealand: a retrospective case-control study. Lancet. 2017;390:1603–10.
Petousis-Harris H, Radcliff FJ. Exploitation of Neisseria meningitidis Group B OMV vaccines against N. gonorrhoeae to Inform the development and deployment of effective gonorrhea vaccines. Front Immunol. 2019;10:683.
Kim OY, Park HT, Dinh NTH, Choi SJ, Lee J, Kim JH, et al. Bacterial outer membrane vesicles suppress tumor by interferon-gamma-mediated antitumor response. Nat Commun. 2017;8:626.
Arroyo V, Jalan R. Acute-on-chronic liver failure: definition, diagnosis, and clinical characteristics. Semin Liver Dis. 2016;36:109–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MD Anderson Cancer Center and RK hold patents in the area of exosome biology and are licensed to Codiak Biosciences, Inc. MD Anderson Cancer Center and RK are stock equity holders in Codiak Biosciences, Inc. RK is a consultant and scientific adviser for Codiak Biosciences, Inc.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chronopoulos, A., Kalluri, R. Emerging role of bacterial extracellular vesicles in cancer. Oncogene 39, 6951–6960 (2020). https://doi.org/10.1038/s41388-020-01509-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41388-020-01509-3
This article is cited by
-
Prokaryotic microvesicles Ortholog of eukaryotic extracellular vesicles in biomedical fields
Cell Communication and Signaling (2024)
-
Extracellular vesicles from Lactobacillus druckerii inhibit hypertrophic scar fibrosis
Journal of Nanobiotechnology (2023)
-
Both extracellular vesicles from helicobacter pylori-infected cells and helicobacter pylori outer membrane vesicles are involved in gastric/extragastric diseases
European Journal of Medical Research (2023)
-
Bacteria in cancer initiation, promotion and progression
Nature Reviews Cancer (2023)
-
Prediction of breast cancer using blood microbiome and identification of foods for breast cancer prevention
Scientific Reports (2023)